Nature–Based Interventions for Improving Health and Wellbeing: The Purpose, the People and the Outcomes
Abstract
1. Introduction
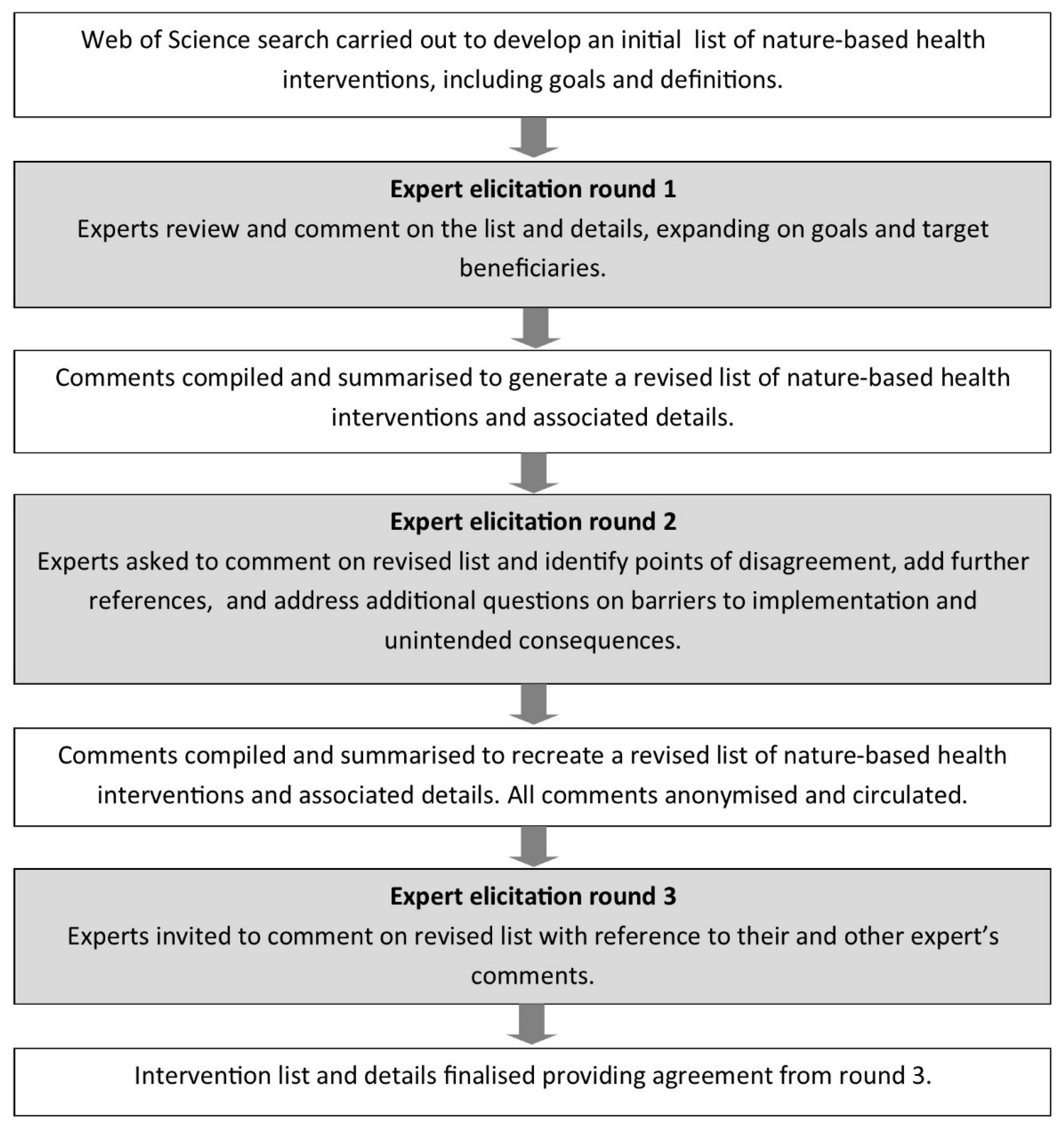
2. Materials and Methods
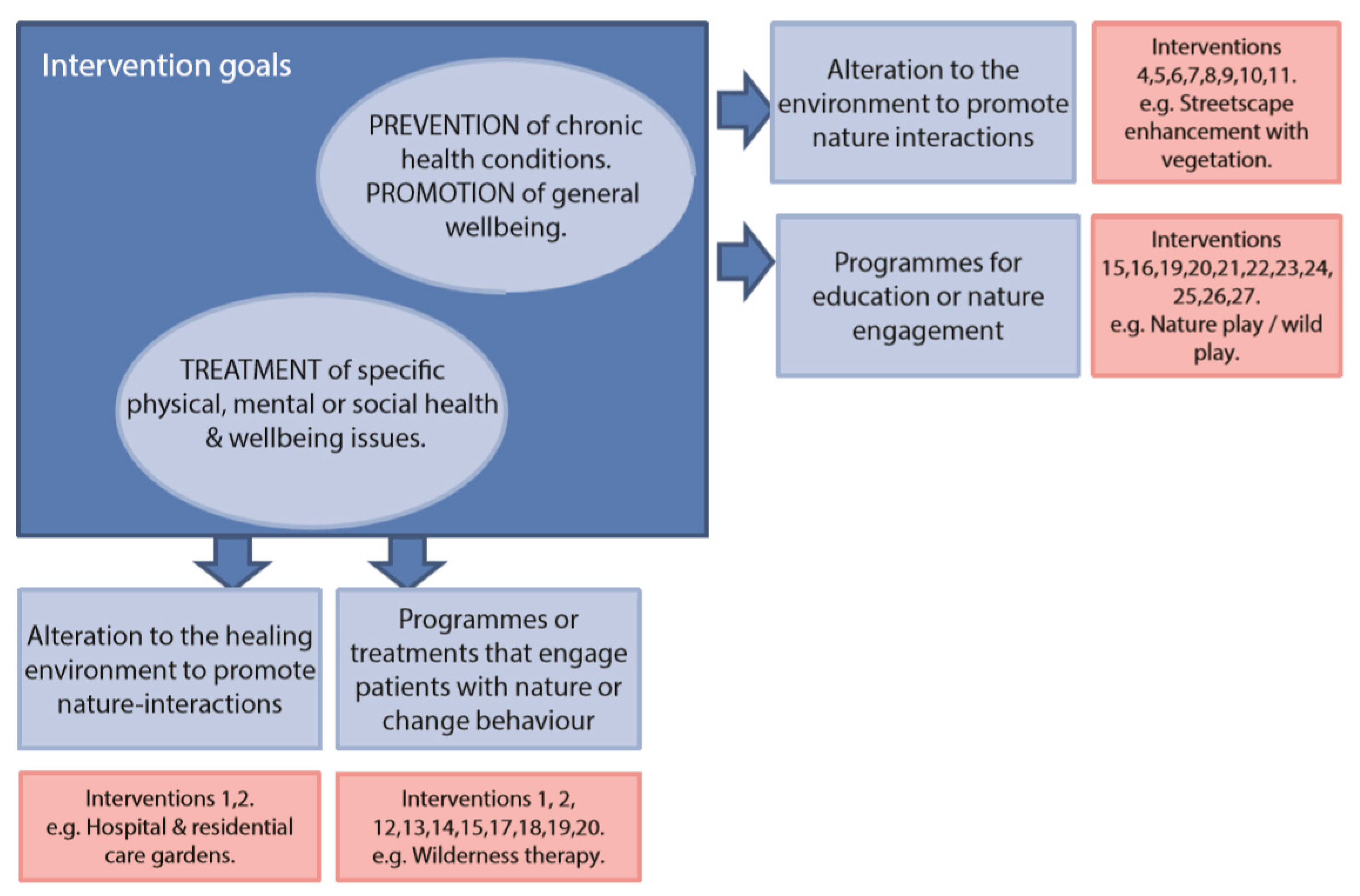
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Moore, M.; Gould, P.; Keary, B.S. Global urbanization and impact on health. Int. J. Hyg. Environ. Health 2003, 206, 269–278. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Urban Health. 2015. Available online: http://www.who.int/topics/urban_health/en/ (accessed on 14 October 2015).
- Dye, C. Health and urban living. Science 2008, 319, 766–769. [Google Scholar] [CrossRef]
- Sundquist, K.; Frank, G.; Sundquist, J. Urbanisation and incidence of psychosis and depression: Follow-up study of 4.4 million women and men in Sweden. Br. J. Psychiatry 2004, 184, 293–298. [Google Scholar] [CrossRef]
- Schneiderman, N.; Ironson, G.; Siegel, S.D. Stress and health: Psychological, behavioral, and biological determinants. Ann. Rev. Clin. Psychol. 2005, 1, 607–628. [Google Scholar] [CrossRef] [PubMed]
- Cox, D.T.C.; Hudson, H.L.; Shanahan, D.F.; Fuller, R.A.; Gaston, K.J. The rarity of direct experiences of nature in an urban population. Landsc. Urban Plan. 2017, 160, 79–84. [Google Scholar] [CrossRef]
- Donovan, G.H.; Gatziolis, D.; Longley, I.; Douwes, J. Vegetation diversity protects against childhood asthma: Results from a large New Zealand birth cohort. Nat. Plants 2018, 4, 358–364. [Google Scholar] [CrossRef]
- Shanahan, D.F.; Bush, R.; Gaston, K.J.; Lin, B.B.; Dean, J.; Barber, E.; Fuller, R.A. Health benefits from nature experiences depend on dose. Sci. Rep. 2016, 6, 28551. [Google Scholar] [CrossRef] [PubMed]
- Cohen-Cline, H.; Turkheimer, E.; Duncan, G.E. Access to green space, physical activity and mental health: A twin study. J. Epidemiol. Community Health 2015, 69, 523–529. [Google Scholar] [CrossRef]
- Cox, D.T.C.; Shanahan, D.F.; Hudson, H.L.; Fuller, R.A.; Anderson, K.; Hancock, S.; Gaston, K.J. Doses of nearby nature simultaneously associated with multiple health benefits. Int. J. Environ. Res. Public Health 2017, 14, 172. [Google Scholar] [CrossRef]
- Pretty, J.; Peacock, J.; Hine, R.; Sellens, M.; South, N.; Griffin, M. Green exercise in the UK countryside: Effects on health and psychological well-being, and implications for policy and planning. J. Environ. Plan. Manag. 2007, 50, 211–231. [Google Scholar] [CrossRef]
- Soga, M.; Gaston, K.J. Extinction of experience: The loss of human–nature interactions. Front. Ecol. Environ. 2016, 14, 94–101. [Google Scholar] [CrossRef]
- Gaston, J.K.; Ávila-Jiménez, M.L.; Edmondson, J.L. Managing urban ecosystems for goods and services. J. Appl. Ecol. 2013, 50, 830–840. [Google Scholar] [CrossRef]
- UK National Ecosystem Assessment. The UK National Ecosystem Assessment Technical Report; UNEP-WCMC: Cambridge, UK, 2011. [Google Scholar]
- Shanahan, D.F.; Lin, B.B.; Bush, R.; Gaston, K.J.; Barber, L.; Dean, J.; Fuller, R.A. Toward improved public health outcomes from urban nature. Am. J. Public Health 2015, 105, 470–477. [Google Scholar] [CrossRef] [PubMed]
- Keniger, L.E.; Gaston, K.J.; Irvine, K.N.; Fuller, R.A. What are the benefits of interacting with nature? Int. J. Environ. Res. Public Health 2013, 10, 913–935. [Google Scholar] [CrossRef]
- Hartig, T.; Mitchell, R.; de Vries, S.; Frumkin, H. Nature and Health. Annu. Rev. Public Health 2014, 35, 207–228. [Google Scholar] [CrossRef]
- Maller, C.; Townsend, M.; Pryor, A.; Brown, P.; St Leger, L. Healthy nature healthy people: ‘Contact with nature’ as an upstream health promotion intervention for populations. Health Promot. Int. 2006, 21, 45–54. [Google Scholar] [CrossRef]
- Pretty, J.; Peacock, J.; Sellens, M.; Griffin, M. The mental and physical health outcomes of green exercise. Int. J. Environ. Health Res. 2005, 15, 319–337. [Google Scholar] [CrossRef]
- Douglas, I. Urban ecology and urban ecosystems: Understanding the links to human health and well-being. Curr. Opin. Environ. Sustain. 2012, 4, 385–392. [Google Scholar] [CrossRef]
- Frumkin, H. Beyond toxicity: human health and the natural environment. Am. J. Prev. Med. 2001, 20, 234–240. [Google Scholar] [CrossRef]
- Husk, R.; Blockley, K.; Lovell, R.; Bethel, A.; Bloomfield, D.; Warber, S.L.; Pearson, M.; Lang, I.; Byng, R.; Garside, R. What approaches to social prescribing work, for whom, and in what circumstances? A protocol for a realist review. Syst. Rev. 2016, 5, 93. [Google Scholar] [CrossRef]
- Finlayson, C.M.; Horwitz, P. Wetlands as Settings for Human Health—The Benefits and the Paradox, in Wetlands and Human Health; Weinstein, P., Horwitz, P., Finlayson, C.M., Eds.; Springer: Berlin, Germany, 2015. [Google Scholar]
- Department of Health. Healthy Lives, Healthy People: Our Strategy for Public Health in England; The Stationery Office Limited: London, UK, 2010.
- The Scottish Government. National Planning Framework for Scotland 2; Scottish Government Directorate for the Built Environment: Edinburgh, Scotland, 2009.
- National Park Service Health and Wellness Executive Steering Committee. Healthy Parks Health People US Strategic Action Plan; U.S. Department of the Interior: Washington, DC, USA, 2011.
- Parks Victoria. Linking People and Spaces: A strategy for Melbourne’s Open Space Network; Victorian Government: Melbourne, Australia, 2002.
- UN-Habitat. State of the World’s Cities, 2012/2013: Prosperity of Cities; UN-Habitat: New York, NY, USA, 2013; p. 80. [Google Scholar]
- Carpenter, M. From ‘healthful exercise’ to ‘nature on prescription’: The politics of urban green spaces and walking for health. Landsc. Urban Plan. 2013, 118, 120–127. [Google Scholar] [CrossRef]
- Jepson, R.R.; Robertson, R.; Cameron, H. Green Prescription Schemes: Mapping and Current Practice; NHS Scotland: Edinburgh, Scotland, 2010. [Google Scholar]
- Johnson, M.; Wood, A. Green Prescription Patient Survey 2015 Report; Research New Zealand: Wellington, New Zealand, 2015. [Google Scholar]
- Swinburn, B.A.; Walter, L.G.; Arroll, B.; Tilyard, M.W.; Russell, D.G. The green prescription study: A randomized controlled trial of written exercise advice provided by general practitioners. Am. J. Public Health 1998, 88, 288–291. [Google Scholar] [CrossRef] [PubMed]
- Hsu, C.C.; Sandford, B.A. The Delphi technique: Making sense of concensus. Pract. Assess. Res. Eval. 2007, 12, 1–8. [Google Scholar]
- Maller, C.; Townsend, M.; St Leger, L.; Henderson-Wilson, C.; Pryor, A.; Prosser, L.; Moore, M. Health Parks, Healthy People: The Benefits of Contact with Nature in a Park Context; School of Health and Social Development, Deakin University: Melbourne, Australia, 2008. [Google Scholar]
- Play England. The Wild Network. 2015. Available online: http://www.playengland.org.uk/our-work/campaigns/the-wild-network.aspx (accessed on 10 June 2015).
- Cooper Marcus, C.; Barnes, M. Healing Gardens: Therapeutic Benefits and Design Recommendations; John Wiley & Sons: Hoboken NJ, USA, 1999. [Google Scholar]
- Cooper Marcus, C. Healing gardens in hospitals. Interdiscip. Des. Res. e-J. 2007, 1, 1–27. Available online: http://www.idrp.wsu.edu/ (accessed on 30 January 2016).
- Hartig, T.; Cooper Marcus, C. Essay: Healing gardens—Places for nature in healthcare. Lancet 2006, 368, S36–S37. [Google Scholar] [CrossRef]
- O’Brien, E. Innovative NHS Greenspace in Scotland. Forest Research; Farnham Forestry Commission: Farnham, Scotland, 2014. [Google Scholar]
- Van den Berg, A.E.; Jaspers, F.C.A.; Wagenaar, C. Health Impacts of Healing Environments; University Hospital Groningen: Groningen, The Netherlands, 2005. [Google Scholar]
- Weerasuriya, R.; Townsend, M.; Henderson-Wilson, C.; Wells, S. Exploring the health and wellbeing experiences in accessing gardens within a healthcare setting in Australia: The preliminary findings. Acta Hortic. in press.
- Whear, R.; Coon, J.T.; Bethel, A.; Abbott, R.; Stein, K.; Garside, R. What is the impact of using outdoor spaces such as gardens on the physical and mental well-being of those with dementia? A systematic review of quantitative and qualitative evidence. J. Am. Med. Dir. Assoc. 2014, 15, 697–705. [Google Scholar] [CrossRef]
- Gerlach-Spriggs, N.; Kaufman, R.E.; Warner, J.B.S. Restorative Gardens: The Healing Landscape; Yale University Press: New Haven, CT, USA, 2004. [Google Scholar]
- Ulrich, R.S.; Bogren, L.; Gardiner, S.K.; Lundin, S. Psychiatric ward design can reduce aggressive behavior. J. Environ. Psychol. 2018, 57, 53–66. [Google Scholar] [CrossRef]
- Gonzalez, M.T.; Kirkevold, M. Benefits of sensory garden and horticultural activities in dementia care: A modified scoping review. J. Clin. Nurs. 2014, 23, 2698–2715. [Google Scholar] [CrossRef]
- Irvine, K.N.; Warber, S.L. Greening healthcare: Practicing as if the natural environment really mattered. Altern. Ther. Health Med. 2002, 8, 76–83. [Google Scholar] [PubMed]
- Park, S.H.; Mattson, R.H. Effects of flowering and foliage plants in hospital rooms on patients recovering from abdominal surgery. Horttechnology 2008, 18, 563–568. [Google Scholar] [CrossRef]
- Park, S.H.; Mattson, R.H. Therapeutic influences of plants in hospital rooms on surgical recovery. Hortscience 2009, 44, 102–105. [Google Scholar] [CrossRef]
- Raanaas, R.K.; Patil, G.G.; Hartig, T. Health benefits of a view of nature through the window: A quasi-experimental study of patients in a residential rehabilitation center. Clin. Rehabil. 2012, 26, 21–32. [Google Scholar] [CrossRef] [PubMed]
- Ulrich, R.S. View through a window may influence recovery from surgery. Science 1984, 224, 420–421. [Google Scholar] [CrossRef] [PubMed]
- Yeo, N.L.; Elliott, L.R.; Bethel, A.; White, M.P.; Dean, S.G.; Garside, R. Indoor nature interventions for health and wellbeing of older adults in residential settings: A systematic review. The Gerontologist 2019. [Google Scholar] [CrossRef] [PubMed]
- Bringslimark, T.; Hartig, T.; Patil, G.G. Psychological benefits of indoor plants in workplaces: Putting experimental results into context. HortScience 2007, 42, 581–587. [Google Scholar] [CrossRef]
- Shibata, S.; Suzuki, N. Effects of an indoor plant on creative task performance and mood. Scand. J. Psychol. 2004, 45, 373–381. [Google Scholar] [CrossRef] [PubMed]
- Dela Cruz, M.; Christensen, J.H.; Thomsen, J.D.; Muller, R. Can ornamental potted plants remove volatile organic compounds from indoor air? A review. Environ. Sci. Pollut. Res. Int. 2014, 21, 13909–13928. [Google Scholar] [CrossRef] [PubMed]
- De Sousa, C.A. Unearthing the benefits of brownfield to green space projects: An examination of project use and quality of life impacts. Local Environ. 2006, 11, 577–600. [Google Scholar] [CrossRef]
- Hoehner, C.M.; Brownson, R.C.; Allen, D.; Gramann, J.; Behrens, T.K.; Floyd, M.F.; Leahy, J.; Liddle, J.B.; Smaldone, D.; Spain, D.D.; et al. Parks promoting physical activity: synthesis of findings from interventions in seven national parks. J. Phys. Act. Health 2010, 7, S67–S81. [Google Scholar] [CrossRef]
- Nordh, H.; Alalouch, C.; Hartig, T. Assessing restorative components of small urban parks using conjoint methodology. Urban For. Urban Green. 2011, 10, 95–103. [Google Scholar] [CrossRef]
- Nordh, H.; Hartig, T.; Hägerhäll, C.; Fry, G. Components of small urban parks that predict the possibility for restoration. Urban For. Urban Green. 2009, 8, 225–235. [Google Scholar] [CrossRef]
- Giles-Corti, B.; Broomhall, M.H.; Knuiman, M.; Collins, C.; Douglas, K.; Ng, K.; Lange, A.; Donovan, R.J. Increasing walking—How important is distance to, attractiveness, and size of public open space? Am. J. Prev. Med. 2005, 28, 169–176. [Google Scholar] [CrossRef] [PubMed]
- Thomsen, J.M.; Powell, R.B.; Allen, D. designing parks for human health benefits park health resources: Benefits, values, and implications. Park Sci. 2013, 30, 30–36. [Google Scholar]
- Veitch, J.; Ball, K.; Crawford, D.; Abbott, G.R.; Salmon, J. Park improvements and park activity: a natural experiment. Am. J. Prev. Med. 2012, 42, 616–619. [Google Scholar] [CrossRef] [PubMed]
- Roemmich, J.N.; Beeler, J.E.; Johnson, L. A microenvironment approach to reducing sedentary time and increasing physical activity of children and adults at a playground. Prev. Med. 2014, 62, 108–112. [Google Scholar] [CrossRef] [PubMed]
- Dallimer, M.; Irvine, K.N.; Skinner, A.M.J.; Davies, Z.G.; Rouquette, J.R.; Maltby, L.L.; Warren, P.H.; Armsworth, P.R.; Gaston, K.J. Biodiversity and the feel-good factor: understanding associations between self-reported human well-being and species richness. Bio. Science 2012, 62, 47–55. [Google Scholar] [CrossRef]
- Fuller, R.A.; Irvine, K.N.; Devine-Wright, P.; Warren, P.H.; Gaston, K.J. Psychological benefits of greenspace increase with biodiversity. Biol. Lett. 2007, 3, 390–394. [Google Scholar] [CrossRef] [PubMed]
- Badland, H.; Knuiman, M.; Hooper, P.; Giles-Corti, B. Socio-ecological predictors of the uptake of cycling for recreation and transport in adults: Results from the RESIDE study. Prev. Med. 2013, 57, 396–399. [Google Scholar] [CrossRef]
- Bauman, A.E.; Reis, R.S.; Sallis, J.F.; Wells, J.C.; Loos, R.J.F.; Martin, B.W. Correlates of physical activity: why are some people physically active and others not? Lancet 2012, 380, 258–270. [Google Scholar] [CrossRef]
- Evenson, R.K.; Herring, A.H.; Huston, S.L. Evaluating change in physical activity with the building of a multi-use trail. Am. J. Prev. Med. 2005, 28, 177–185. [Google Scholar] [CrossRef]
- Fraser, S.D.S.; Lock, K. Cycling for transport and public health: A systematic review of the effect of the environment on cycling. Eur. J. Public Health 2011, 21, 738–743. [Google Scholar] [CrossRef] [PubMed]
- Giles-Corti, B.; Bull, F.; Knuiman, M.; McCormack, G.; Van Niel, K.; Timperio, A.; Christian, H.; Foster, S.; Divitini, M.; Middleton, N.; et al. The influence of urban design on neighbourhood walking following residential relocation: Longitudinal results from the RESIDE study. Soc. Sci. Med. 2013, 77, 20–30. [Google Scholar] [CrossRef] [PubMed]
- Gomez-Feliciano, L.; McCreary, L.L.; Sadowsky, R.; Peterson, S.; Hernandez, A.; McElmurry, B.J.; Park, C.G. Active Living Logan Square: Joining together to create opportunities for physical activity. Am. J. Prev. Med. 2009, 37, S361–S367. [Google Scholar] [CrossRef] [PubMed]
- Jia, Y.N.; Fu, H. Associations between perceived and observational physical environmental factors and the use of walking paths: a cross-sectional study. BMC Public Health 2014, 14, 11. [Google Scholar] [CrossRef]
- Morris, J.; O’Brien, E. Encouraging healthy outdoor activity amongst under-represented groups: An evaluation of the Active England woodland projects. Urban For. Urban Green. 2011, 10, 323–333. [Google Scholar] [CrossRef]
- Mosquera, J.; Parra, D.C.; Gomez, L.F.; Sarmiento, O.; Schmid, T.; Jacoby, E. An inside look at active transportation in Bogota: A qualitative study. J. Phys. Act. Health 2012, 9, 776–785. [Google Scholar] [CrossRef]
- Sallis, J.E.; Cervero, R.B.; Ascher, W.; Henderson, K.A.; Kraft, M.K.; Kerr, J. An ecological approach to creating active living communities. Ann. Rev. Publ. Health 2006, 27, 297–322. [Google Scholar] [CrossRef]
- Shafer, C.S.; Bong Koo, L.; Turner, S. A tale of three greenway trails: User perceptions related to quality of life. Landsc. Urban Plan. 2000, 49, 163. [Google Scholar] [CrossRef]
- Lindal, P.J.; Hartig, T. Effects of urban street vegetation on judgments of restoration likelihood. Urban For. Urban Green. 2015, 14, 200–209. [Google Scholar] [CrossRef]
- Lovasi, G.S.; O’Neil-Dunne, J.P.M.; Lu, J.W.T.; Sheehan, D.; Perzanowski, M.S.; MacFaden, S.W.; King, K.L.; Matte, T.; Miller, R.L.; Hoepner, L.A.; et al. Urban tree canopy and asthma, wheeze, rhinitis, and allergic sensitization to tree pollen in a New York City birth cohort. Environ. Health Perspect. 2013, 121, 494–500. [Google Scholar] [CrossRef]
- Kardan, O.; Gozdyra, P.; Misic, B.; Moola, F.; Palmer, L.J.; Paus, T.; Berman, M.G. Neighborhood greenspace and health in a large urban center. Sci. Rep. 2015, 5. [Google Scholar] [CrossRef] [PubMed]
- Okvat, H.A.; Zautra, A.J. Community gardening: A parsimonious path to individual, community, and environmental resilience. Am. J. Community Psychol. 2011, 47, 374–387. [Google Scholar] [CrossRef] [PubMed]
- George, D.R. Harvesting the biopsychosocial benefits of community gardens. Am. J. Public Health 2013, 103, E6. [Google Scholar] [CrossRef] [PubMed]
- Hatchett, L.; Brown, L.; Hopkins, J.; Larsen, K.; Fournier, E. “Something good can grow here”: Chicago urban agriculture food projects. J. Prev. Interv. Community 2015, 43, 2. [Google Scholar] [CrossRef] [PubMed]
- Laaksoharju, T.; Rappe, E.; Kaivola, T. Garden affordances for social learning, play, and for building nature-child relationship. Urban For. Urban Green. 2012, 11, 195–203. [Google Scholar] [CrossRef]
- Gonzalez, M.T.; Hartig, T.; Patil, G.G.; Martinsen, E.W.; Kirkevold, M. Therapeutic horticulture in clinical depression: A prospective study of active components. J. Adv. Nurs. 2010, 66, 2002–2013. [Google Scholar] [CrossRef]
- Blair, D.; Giesecke, C.C.; Sherman, S. A dietary, social and economic evaluation of the Philadelphia urban gardening project. J. Nutr. Educ. 1991, 23, 161–167. [Google Scholar] [CrossRef]
- Kingsley, J.; Townsend, M. ‘Dig in’ to social capital: Community gardens as mechanisms for growing urban social connectedness. Urban Policy Res. 2006, 24, 525–537. [Google Scholar] [CrossRef]
- Kingsley, J.; Townsend, M.; Henderson-Wilson, C. Cultivating health and wellbeing: members’ perceptions of the health benefits of a Port Melbourne community garden. Leis. Stud. 2009, 28, 207–219. [Google Scholar] [CrossRef]
- Fjørtoft, I.; Kristoffersen, B.; Sageie, J. Children in schoolyards: Tracking movement patterns and physical activity in schoolyards using global positioning system and heart rate monitoring. Landsc. Urban Plan. 2009, 93, 210–217. [Google Scholar]
- Dyment, J.E.; Bell, A.C.; Lucas, A.J. The relationship between school ground design and intensity of physical activity. Child. Geogr. 2009, 7, 261–276. [Google Scholar] [CrossRef]
- Dowdell, K.; Gray, T.; Malone, K. Nature and its influence on children’s outdoor play. Aust. J. Outdoor Educ. 2011, 15, 24–35. [Google Scholar] [CrossRef]
- Dadvand, P.; Nieuwenhuijsen, M.J.; Esnaola, M.; Forns, J.; Basagana, X.; Alvarez-Pedrerol, M.; Rivas, I.; Lopez-Vicente, M.; Pascual, M.D.; Su, J.; et al. Green spaces and cognitive development in primary schoolchildren. Proc. Natl. Acad. Sci. USA 2015, 112, 7937–7942. [Google Scholar] [CrossRef] [PubMed]
- Cranney, L.; Phongsavan, P.; Kariuki, M.; Stride, V.; Scott, A.; Hua, M.; Bauman, A. Impact of an outdoor gym on park users’ physical activity: A natural experiment. Health Place 2016, 37, 26–34. [Google Scholar] [CrossRef]
- Neville, L.; Scott, A. The Impact of Outdoor Gyms on Park Use and Physical Activity; NSW Government: Sydney, Australia, 2013.
- Thompson, W.C.; Roe, J.; Aspinall, P. Woodland improvements in deprived urban communities: What impact do they have on people’s activities and quality of life? Landsc. Urban Plan. 2013, 118, 79–89. [Google Scholar] [CrossRef]
- Owen, R. An Evaluation of Cydcoed; Forestry Commission Wales: Cardiff, UK, 2009. [Google Scholar]
- Park, B.J.; Tsunetsugu, Y.; Ishii, H.; Furuhashi, S.; Hirano, H.; Kagawa, T.; Miyazaki, Y. Physiological effects of Shinrin-yoku (taking in the atmosphere of the forest) in a mixed forest in Shinano Town, Japan. Scand. J. For. Res. 2008, 23, 278–283. [Google Scholar] [CrossRef]
- Tsunetsugu, Y.; Park, J.B.; Miyazaki, Y. Trends in research realted to “Shinrin-yoku” (taking in the forest atmosphere of forest bathing) in Japan. Environ. Health Prev. Med. 2010, 15, 27–37. [Google Scholar] [CrossRef] [PubMed]
- Patel, A.; Schofield, G.M.; Kolt, G.S.; Keogh, J.W.L. General practitioners’ views and experiences of counselling for physical activity through the New Zealand Green Prescription program. BMC Fam. Pract. 2011, 12, 8. [Google Scholar] [CrossRef] [PubMed]
- Barton, J.; Pretty, J. What is the best dose of nature and green exercise for improving mental health? A multi-study analysis. Environ. Sci. Technol. 2010, 44, 3947–3955. [Google Scholar] [CrossRef] [PubMed]
- Cimprich, B.; Ronis, D.L. An environmental intervention to restore attention in women with newly diagnosed breast cancer. Cancer Nurs. 2003, 26, 284–292. [Google Scholar] [CrossRef] [PubMed]
- Mao, G.X.; Cao, Y.B.; Lan, X.G.; He, Z.H.; Chen, Z.M.; Wang, Y.Z.; Hu, X.L.; Lv, Y.D.; Wang, G.F.; Yan, J. Therapeutic effect of forest bathing on human hypertension in the elderly. J. Cardiol. 2012, 60, 495–502. [Google Scholar] [CrossRef] [PubMed]
- Laumann, K.; Garling, T.; Stormark, K.M. Selective attention and heart rate responses to natural and urban environments. J. Environ. Psychol. 2003, 23, 125–134. [Google Scholar] [CrossRef]
- Grinde, B.; Patil, G.G. Biophilia: Does visual contact with nature impact on health and well-being? Int. J. Environ. Res. Public Health 2009, 6, 2332–2343. [Google Scholar] [CrossRef] [PubMed]
- The Appalachian Mountain Club. Appalachian Mountain Club and MassGeneral Hospital for Children Team Up with WGBH on Outdoors Rx Expansion. 2014. Available online: http://www.outdoors.org/about/newsroom/press/2014/outdoorsrx-chelsea-revere.cfm (accessed on 22 May 2015).
- Marselle, M.R.; Warber, S.L.; Irvine, K.N. Growing resilience through interaction with nature: Can group walks in nature buffer the effects of stressful life events on mental health? Int. J. Environ. Res. Public Health 2019, 16, 986. [Google Scholar] [CrossRef] [PubMed]
- Hine, R.; Peackock, J.; Pretty, J. Care farming in the UK: Contexts, benefits and links with therapeutic communities. Int. J. Ther. Communities 2008, 29, 245–260. [Google Scholar]
- De Bruin, S.R.; Oosting, S.J.; Tobi, H.; Blauw, Y.H.; Schols, J.M.G.A.; De Groot, C.P.G.M. Day care at green care farms: a novel way to stimulate dietary intake of community-dwelling older people with dementia? J. Nutr. Health Aging 2010, 14, 352–357. [Google Scholar] [CrossRef]
- Hine, R. Care farming: Bringing together agriculture and health. ECOS A Rev. Conserv. 2008, 29, 42–51. [Google Scholar]
- Brown, K.H.; Jameton, A.L. Public Health Implications of Urban Agriculture. J. Public Health Policy 2000, 21, 30–39. [Google Scholar] [CrossRef]
- Berget, B.; Braastad, B.O. Animal-assisted therapy with farm animals for persons with psychiatric disorders. Annali Dell Instituto Superiore Di Sanita 2011, 47, 384–390. [Google Scholar]
- Haugan, L.; Nyland, R.; Fjeldavli, E.; Meistad, T.; Braastad, B.O. Green Care in Norway—Farms as a Resource for the educational, health and social sector. In Farming for Health: Green-Care Farming Across Europe and the United States of America; Hassink, J., VanDijk, M., Eds.; Springer: Berlin, Germany, 2006; Volume 13, pp. 109–126. [Google Scholar]
- Annerstedt, M.; Wahrborg, P. Nature-assisted therapy: Systematic review of controlled and observational studies. Scand. J. Public Health 2011, 39, 371–388. [Google Scholar] [CrossRef]
- Gonzalez, M.T.; Hartig, T.; Patil, G.G.; Martinsen, E.W.; Kirkevold, M. Therapeutic horticulture in clinical depression: A prospective study. Res. Theory Nurs. Pract. 2009, 23, 312–328. [Google Scholar] [CrossRef] [PubMed]
- Kamioka, H.; Tsutani, K.; Yamada, M.; Park, H.; Okuizumi, H.; Honda, T.; Okada, S.; Park, S.J.; Kitayuguchi, J.; Abe, T.; et al. Effectiveness of horticultural therapy: A systematic review of randomized controlled trials. Complement. Ther. Med. 2014, 22, 930–943. [Google Scholar] [CrossRef] [PubMed]
- Clatworthy, J.; Hinds, J.; Camic, P.M. Gardening as a mental health intervention: A review. Ment. Health Rev. J. 2013, 18, 214–225. [Google Scholar] [CrossRef]
- Warber, S.L.; Ingerman, S.; Moura, V.L.; Wunder, J.; Northrop, A.; Gillespie, B.W.; Durda, K.; Smith, K.; Rhodes, K.S.; Rubenfire, M. Healing the heart: A randomized pilot study of a spiritual retreat for depression in acute coronary syndrome patients. Explor. J. Sci. Heal. 2011, 7, 222–233. [Google Scholar] [CrossRef] [PubMed]
- Carter, C.; West, D. Policy into Practice: Employment for Ex-Offenders—An Innovative Approach; Forest Research: Farnham, UK, 2008. [Google Scholar]
- South, N.; Brisman, A. Routledge International Handbook of Green Criminology; Routledge International Handbooks: Oxford, UK, 2013. [Google Scholar]
- Morris, J.; Marzano, M.; Dandy, N.; O’Brien, L. Lessons Learned from Interventions and Evaluations, in Forestry, Sustainable Behabiours and Behaviour Change: Interventions; Forest Research: Bristol, UK, 2012; pp. 1–13. [Google Scholar]
- Easley, T.A.; Passineau, J.F.; Driver, B.L. The Use of Wilderness for Personal Growth, Therapy, and Education (USDA Forest Service General Technical Report RM-193); USDA Forest Service Rocky Mountain Forest and Range Experiment Station: Fort Collins, CO, USA, 1990. [Google Scholar]
- Garg, R.; Couture, R.T.; Ogryzlo, T.; Schinke, R. Perceived psychosocial benefits associated with perceived restorative potential of wilderness river-rafting trips. Psychol. Rep. 2010, 107, 213–226. [Google Scholar] [CrossRef] [PubMed]
- Stuhlmiller, C.M. Breaking down the stigma of mental illness through an adventure camp: A collaborative education initiative. Aust. e-J. Adv. Ment. Health 2003, 2, 1–9. [Google Scholar] [CrossRef]
- Thomas, M. The potential unlimited programme: An outdoor experiential education and group work approach that facilitates adjustment to brain injury. Brain Inj. 2004, 18, 1271–1286. [Google Scholar] [CrossRef]
- Pryor, A.; Carpenter, C.; Townsend, M. Outdoor Education and Bush Adventure Therapy: A Socio-ecological approach to Health and Wellbeing. Aust. J. Outdoor Educ. 2005, 9, 3–13. [Google Scholar] [CrossRef]
- Levitt, L. What is the therapeutic value of camping for emotionally disturbed girls? Women Ther. 1994, 15, 129–137. [Google Scholar] [CrossRef]
- Shanahan, L.; McAllister, L.; Curtin, M. Wilderness adventure therapy and cognitive rehabilitation: Joining forces for youth with TBI. Brain Inj. 2009, 23, 1054–1064. [Google Scholar] [CrossRef]
- Drebing, C.E.; Cabot Willis, S.; Genet, B. Anxiety and the Outward Bound process. J. Exp. Educ. 1987, 10, 17–21. [Google Scholar] [CrossRef]
- Warber, S.L.; DeHudy, A.A.; Bialko, M.F.; Marselle, M.R.; Irvine, K.N. Addressing (nature-deficit disorder): A mixed methods pilot study of young adults attending a wilderness camp. Evid. Based Complement. Altern. Med. 2015, 2015, 651827. [Google Scholar] [CrossRef] [PubMed]
- Tzoulas, K.; Greening, K. Urban ecology and human health. In Urban Ecology: Patterns, Processes, and Application; Niemelä, J., Breuste, J.H., Guntenspergen, G., McIntyre, N.E., Elmqvist, T., James, P., Eds.; Oxford University Press: Oxford, UK, 2011; pp. 263–271. [Google Scholar]
- Mind. Ecotherapy: The Green Agenda for Mental Health; Mind: London, UK, 2007. [Google Scholar]
- Buzzell, L.; Chalquist, C. Ecotherapy: Healing with Nature in Mind; Sierra Club Books: San Francisco, CA, USA, 2009. [Google Scholar]
- Chalquist, C. A look at the ecotherapy research evidence. Ecophysiology 2009, 1, 64–74. [Google Scholar] [CrossRef]
- Cherniack, E.P.; Cherniack, A.R. The benefit of pets and animal-assisted therapy to the health of older individuals. Curr. Gerontol. Geriatr. Res. 2014, 2014, e623203. [Google Scholar] [CrossRef] [PubMed]
- Richeson, N.E. Effects of animal-assisted therapy on agitated behaviours and social interactions of older adults with dementia. Am. J. Alzheimers Dis. Other Dement. 2003, 18, 353–358. [Google Scholar] [CrossRef] [PubMed]
- Banks, M.R.; Banks, W.A. The effects of animal-assited therapy on lonelilness in an elderly population in long-term care facilities. J. Gerontol. Ser. A Biol. Sci. Med. Sci. 2002, 57, M428–M432. [Google Scholar] [CrossRef]
- Lee, J.; Park, B.J.; Tsunetsugu, Y.; Ohira, T.; Kagawa, T.; Miyazaki, Y. Effect of forest bathing on physiological and psychological responses in young Japanese male subjects. Public Health 2011, 125, 93–100. [Google Scholar] [CrossRef]
- Mao, G.X.; Lan, X.G.; Cao, Y.B.; Chen, Z.M.; He, Z.H.; Lv, Y.D.; Wang, Y.Z.; Hu, X.L.; Wang, G.F.; Yan, J. Effects of short-term forest bathing on human health in a broad-leaved evergreen forest in Zhejiang Province, China. Biomed. Environ. Sci. 2012, 25, 317–324. [Google Scholar]
- Yerrell, P. National Evaluation of BTCV’s Green Gym; School of Health and Social Care, Oxford Brookes University: Oxford, UK, 2008. [Google Scholar]
- O’Brien, L.; Burls, A.; Townsend, M.; Ebden, M. Volunteering in nature as a way of enabling people to re-integrate into society. Perspect. Public Health 2010, 131, 71–81. [Google Scholar] [CrossRef]
- Birch, M. Cultivating wildness: Three conservation volunteers’ experiences of participation in the Green Gym scheme. Br. J. Occup. Ther. 2005, 68, 244–252. [Google Scholar] [CrossRef]
- O’Brien, L.; Townsend, M.; Ebden, M. Doing something positive’: Volunteers’ experiences of the well-being benefits derived from practical conservation activities in nature. Voluntas 2010, 21, 525–545. [Google Scholar] [CrossRef]
- Townsend, M. Feel blue? Touch green! Participation in forest/woodland management as a treatment for depression. Urban For. Urban Green. 2006, 5, 111–120. [Google Scholar] [CrossRef]
- Blaschke, P. Health and wellbeing benefits of conservation in New Zealand. In Science for Conservation; New Zealand Department of Conservation: Wellington, New Zealand, 2013. [Google Scholar]
- Cowie, C. The Geographies of Community-Based Ecological Restoration Groups in the Wellington Region; Victoria University: Wellington, New Zealand, 2010. [Google Scholar]
- Pillemer, K.; Fuller-Rowell, T.E.; Reid, M.C.; Wells, N.M. Environmental volunteering and health outcomes over a 20-year period. Gerontologist 2010, 50, 594–602. [Google Scholar] [CrossRef] [PubMed]
- ulz, A.J.; Israel, B.A.; Mentz, G.B.; Bernal, C.; Caver, D.; DeMajo, R.; Diaz, G.; Gamboa, C.; Gaines, C.; Hoston, B.; et al. Effectiveness of a Walking Group Intervention to Promote Physical Activity and Cardiovascular Health in Predominantly Non-Hispanic Black and Hispanic Urban Neighborhoods: Findings from the Walk Your Heart to Health Intervention. Health Educ. Behav. 2015, 42, 380–392. [Google Scholar]
- Hanson, S.R.; Jones, A.P. Is there evidence that walking groups have health benefits? A systematic review and meta-analysis. Br. J. Sports Med. 2015, 49, 710–715. [Google Scholar] [CrossRef] [PubMed]
- Mitchell, T.L.; Yakiwchuk, C.V.; Griffin, K.L.; Gray, R.E.; Fitch, M.I. Survivor dragon boating: A vehicle to reclaim and enhance life after treatment for breast cancer. Health Care Women Int. 2007, 28, 133. [Google Scholar] [CrossRef]
- Lane, K.; Jespersen, D.; McKenzie, D.C. The effect of a whole body exercise pro-gramme and dragon boat training on arm volume and arm circumference in women treated for breast cancer. Eur. J. Cancer Care 2005, 14, 353. [Google Scholar] [CrossRef] [PubMed]
- Marselle, M.R.; Irvine, K.N.; Warber, S.L. Examining group walks in nature and multiple aspects of well-being: A large-scale study. Ecophysiology 2014, 6, 134–147. [Google Scholar]
- Hanson, S.J.; Guell, C.; Jones, A.P. Walking groups in socioeconomically deprived communities: A qualitative study using photo elicitation. Health Place 2016, 39, 26–33. [Google Scholar] [CrossRef] [PubMed]
- Children & Nature Network and IUCN. Children and Nature Worldwide: An Exploration of Children’s Experiences of the Outdoors and Nature with Associated Risks and Benefits; Children & Nature Network: Minneapolis, ME, USA, 2012. [Google Scholar]
- Staempfli, M.B. Reintroducing adventure into children’s outdoor play environments. Environ. Behav. 2008, 41, 268–280. [Google Scholar] [CrossRef]
- Arbogast, K.L.; Kane, B.C.P.; Kirwan, J.L.; Hertel, B.R. Vegetation and outdoor recess time at elementary schools: What are the connections? J. Environ. Psychol. 2009, 29, 450–456. [Google Scholar] [CrossRef]
- Donovan, T. Natural play areas for London children. Child. Young People Now 2008, 2, 2. [Google Scholar]
- Herrington, S.; Studtmann, K. Landscape interventions: New directions for the design of children’s outdoor play environments. Landsc. Urban Plan. 1998, 42, 191. [Google Scholar] [CrossRef]
- Fjortoft, I. The natural environment as a playground for children: The impact of outdoor play activities in pre-primary school children. Early Child. Educ. J. 2001, 29, 111–117. [Google Scholar] [CrossRef]
- Maller, C.J.; Townsend, M. Children’s mental health & wellbeing and hands-on contact with nature: perceptions of principals and teachers. Int. J. Learn. 2006, 12, 359–372. [Google Scholar]
- kson, M.; Dillon, J.; Teamey, K.; Morris, M.; Young Choi, M.; Sanders, D.; Benefield, P. A Review of Research on Outdoor Learning; National Foundation for Educational Research: Slough, UK, 2004. [Google Scholar]
- Eastwood, G.; Mitchell, H. An Evaluation of the First Three Years of the Oxfordshire Forest School Project; Oxfordshire County Council: Oxford, UK, 2003. [Google Scholar]
- Murray, R. Forest Schools Project Evaluation: A Study in Wales London; New Economics Foundation: London, UK, 2004; pp. 1–68. [Google Scholar]
- O’Brien, L. Learning outdoors: The Forest School approach. Education 2009, 37, 45–60. [Google Scholar] [CrossRef]
- Block, K.; Gibbs, L.; Staiger, P.K.; Gold, L.; Johnson, B.; Macfarlane, S.; Long, C.; Townsend, M. Growing community: The Impact of the Stephanie Alexander Kitchen Garden Program on the social and learning environment in primary schools. Health Educ. Behav. 2012, 39, 419–432. [Google Scholar] [CrossRef] [PubMed]
- Gibbs, L.; Staiger, P.K.; Johnson, B.; Block, K.; Macfarlane, S.; Gold, L.; Kulas, J.; Townsend, M.; Long, C.; Ukoumunne, O. Expanding children’s food experiences: The impact of a school-based kitchen garden program. J. Nutr. Educ. Behav. 2013, 45, 137–146. [Google Scholar] [CrossRef]
- Christian, M.S.; El Evans, C.; Nykjaer, C.; Hancock, N.; Cade, J.E. Evaluation of the impact of a school gardening intervention on children’s fruit and vegetable intake: a randomised controlled trial. Int. J. Nutr. Phys. Activ. 2014, 11, 99. [Google Scholar] [CrossRef]
- Davis, J.N.; Ventura, E.E.; Cook, L.T.; Gyllenhammer, L.E.; Gatto, N.M. LA Sprouts: A gardening, nutrition, and cooking intervention for Latino youth improves diet and reduces obesity. J. Am. Diet. Assoc. 2011, 111, 1224–1230. [Google Scholar] [CrossRef]
- Gatto, N.M.; Martinez, L.C.; Spruijt-Metz, D.; Davis, J.N. LA sprouts randomized controlled nutrition and gardening program reduces obesity and metabolic risk in latino youth. Obesity 2015, 23, 1244–1251. [Google Scholar] [CrossRef] [PubMed]
- Gatto, N.M.; Ventura, E.E.; Cook, L.T.; Gyllenhammer, L.E.; Davis, J.N. LA Sprouts: A garden-based nutrition intervention pilot program influences motivation and preferences for fruits and vegetables in Latino youth. J. Acad. Nutr. Diet. 2012, 112, 913–920. [Google Scholar] [CrossRef] [PubMed]
- Hutchinson, J.; Christian, M.S.; Evans, C.E.L.; Nykjaer, C.; Hancock, N.; Cade, J.E. Evaluation of the impact of school gardening interventions on children’s knowledge of and attitudes towards fruit and vegetables. A cluster randomised controlled trial. Appetite 2015, 91, 405–414. [Google Scholar] [CrossRef] [PubMed]
- Keys, E.B.; Lindsey, P.; Bradley, L.K.; Werner, D.; Driscoll, E. Residential children’s landscapes: Connecting with nature in the backyard. In III International Conference on Landscape and Urban Horticulture, Nanjing, China, 29 June–3 July 2011; Wuzhong, Z.Z., Groening, G., Drew, R.A., Eds.; International Society for Horticultural Science: Leuven, Belgium, 2013; pp. 81–87. [Google Scholar]
- McAleese, J.D.; Rankin, L.L. Garden-based nutrition education affects fruit and vegetable consumption in sixth-grade adolescents. J. Am. Diet. Assoc. 2007, 107, 662–665. [Google Scholar] [CrossRef] [PubMed]
- Wells, N.M.; Myers, B.M.; Henderson, C.R. School gardens and physical activity: A randomized controlled trial of low-income elementary schools. Prev. Med. 2014, 69, S27–S33. [Google Scholar] [CrossRef] [PubMed]
- Mitchell, R.; Shaw, R. Health Impacts of the John Muir Award; University of Glasgow: Glasgow, Scotland, 2015. [Google Scholar]
- De Kievit, J. Healthy Parks, Healthy People—A Natural Link; Parks and Leisure Australia: Melbourne, Australia, 2001; pp. 20–21. [Google Scholar]
- Caddick, N.; Smith, B.; Phoenix, C. The effects of surfing and the natural environment on the well-being of combat veterans. Qual. Health Res. 2015, 25, 76–86. [Google Scholar] [CrossRef] [PubMed]
- Frieden, T.R. A framework for public health action: The health impact pyramid. Am. J. Public Health 2010, 100, 590–595. [Google Scholar] [CrossRef] [PubMed]
- Irvine, K.N.; Warber, S.L.; Devine-Wright, P.; Gaston, K.J. Understanding urban green space as a health resource: A qualitative comparison of visit motivation and derived effects among park users in Sheffield, UK. Int. J. Environ. Res. Public Health 2013, 10, 417–442. [Google Scholar] [CrossRef]
- Davids, K.; Araujo, D.; Brymer, E. Designing affordances for physical activity: An ecological dynamics perspective. Sports Med, In press.
- Pretty, J.; Barton, J.; Perves Bharucha, Z.; Bragg, R.; Pencheon, D.; Wood, C.; Depledge, M. Improving health and well-being independently of GDP: Dividends of greener and prosocial economies. Int. J. Environ. Health Res. 2015, 11, 1–26. [Google Scholar] [CrossRef]
- Pikora, T.; Giles-Corti, B.; Bull, F.; Jamrozik, K.; Donovan, R. Developing a framework for assessment of the environmental determinants of walking and cycling. Soc. Sci. Med. 2003, 56, 1693–1703. [Google Scholar] [CrossRef]
- Owen, N.; Humpel, N.; Leslie, E.; Bauman, A.; Sallis, J.F. Understanding environmental influences on walking—Review and research agenda. Am. J. Prev. Med. 2004, 27, 67–76. [Google Scholar] [CrossRef] [PubMed]
- Richardson, E.A.; Pearce, J.; Mitchell, R.; Kingham, S. Role of physical activity in the relationship between urban green space and health. Public Health 2013, 127, 318–324. [Google Scholar] [CrossRef] [PubMed]
- Lee, C.; Ory, M.G.; Yoon, J.; Forjuoh, S.N. Neighborhood walking among overweight and obese adults: Age variations in barriers and motivators. J. Community Health 2013, 38, 12–22. [Google Scholar] [CrossRef] [PubMed]
- Timperio, A.; Giles-Corti, B.; Crawford, D.; Andrianopoulos, N.; Ball, K.; Salmon, J.; Hume, C. Features of public open spaces and physical activity among children: findings from the CLAN study. Prev. Med. 2008, 47, 514–518. [Google Scholar] [CrossRef] [PubMed]
- Roemmich, J.N.; Epstein, L.H.; Raja, S.; Yin, L.; Robinson, J.; Winiewicz, D. Association of access to parks and recreational facilities with the physical activity of young children. Prev. Med. 2006, 43, 437–441. [Google Scholar] [CrossRef]
- Astell-Burt, T.; Feng, X.; Kolt, G.S. Greener neighborhoods, slimmer people? Evidence from 246,920 Australians. Int. J. Obes. 2014, 38, 156–159. [Google Scholar] [CrossRef] [PubMed]
- Iverson, L.R.; Cook, E.A. Urban forest cover of the Chicago region and its relation to household density and income. Urban Ecosyst. 2000, 4, 105–124. [Google Scholar] [CrossRef]
- Shanahan, D.F.; Lin, B.B.; Gaston, K.; Bush, R.; Fuller, R.A. Socio-economic inequalities in access to nature on public and private lands: A case study from Brisbane, Australia. Landsc. Urban Plan. 2014, 130, 14–23. [Google Scholar] [CrossRef]
- Landry, S.M.; Chakraborty, J. Street trees and equity: Evaluating the spatial distribution of an urban amenity. Environ. Plan. A 2009, 41, 2651–2670. [Google Scholar] [CrossRef]
- Pham, T.-T.-H.; Apparicio, P.; Landry, S.; Seguin, A.-M.; Gagnon, M. Predictors of the distribution of street and backyard vegetation in Montreal, Canada. Urban For. Urban Green. 2013, 12, 18–27. [Google Scholar] [CrossRef]
- Cohen, D.A.; Han, B.; Derose, K.P.; Williamson, S.; Marsh, T.; Rudick, J.; McKenzie, T.L. Neighborhood poverty, park use, and park-based physical activity in a Southern California city. Soc. Sci. Med. 2012, 75, 2317–2325. [Google Scholar] [CrossRef] [PubMed]
- Cohen, D.A.; Lapham, S.; Evenson, K.R.; Williamson, S.; Golinelli, D.; Ward, P.; Hillier, A.; McKenzie, T.L. Use of neighbourhood parks: Does socio-economic status matter? A four-city study. Public Health 2013, 127, 325–332. [Google Scholar] [CrossRef] [PubMed]
- Cohen, D.A.; Marsh, T.; Williamson, S.; Derose, K.P.; Martinez, H.; Setodji, C.; McKenzie, T.L. Parks and physical activity: why are some parks used more than others? Prev. Med. 2010, 50, S9–S12. [Google Scholar] [CrossRef]
- Seaman, P.J.; Jones, R.; Ellaway, A. It’s not just about the park, it’s about integration too: Why people choose to use or not use urban greenspaces. Int. J. Behav. Nutr. Phys. Activ. 2010, 7, 78. [Google Scholar] [CrossRef]
- Carter, M.; Horwitz, P. Beyond proximity: The importance of green space useability to self-reported health. Ecohealth 2014, 11, 322–332. [Google Scholar] [CrossRef] [PubMed]
- Van den Berg, A.E.; Jorgensen, A.; Wilson, E.R. Evaluating restoration in urban green spaces: Does setting type make a difference? Landsc. Urban Plan. 2014, 127, 173–181. [Google Scholar] [CrossRef]
- Poulsen, D.V.; Stigsdotter, U.K.; Djernis, D.; Sidenius, U. ‘Everything just seems much more right in nature’: How veterans with post-traumatic stress disorder experience nature-based activities in a forest therapy garden. Health Psychol. Open 2016, 3, 2055102916637090. [Google Scholar] [CrossRef]
- Lymeus, F.; Lindberg, P.; Hartig, T. Building mindfulness bottom-up: Meditation in natural settings supports open monitoring and attention restoration. Conscious. Cognit. 2018, 59, 40–56. [Google Scholar] [CrossRef]
- Lymeus, F.; Lundgren, T.; Hartig, T. Attentional effort of beginning mindfulness training is offset with practice directed toward images of natural scenery. Environ. Behav. 2017, 49, 536–559. [Google Scholar] [CrossRef]
| Intervention | Description | T/P | Intervention Goals, and Intended Health or Wellbeing Outcome | Target Beneficiaries | Example References |
|---|---|---|---|---|---|
| 1. Provision of gardens in hospitals or residential care homes (sometimes referred to as healing gardens). | The provision of gardens that can either be viewed from hospital rooms or accessed by patients and families (can include green walls). | T | Reduce pain and stress, potentially leading to improved healing time and mental health, quality of life, wellbeing, reduced agitation for patients with dementia. | Hospital or residential care patients, their families and friends, staff. Can have targeted groups in some circumstances, e.g., hospitals for patients living with dementia. | [36,37,38,39,40,41,42,43,44] |
| 2. Provision of nature within rooms in healing environments. | The provision of nature that can be viewed or experienced from a person’s room and/or in shared areas (e.g., the view from a window, or indoor plants, flowers, garden, green walls). | T | Reduce pain and stress, potentially leading to improved healing time and mental health, social contacts, quality of life, wellbeing. | Hospital or residential care patients, their families and friends, staff. | [40,41,42,45,46,47,48,49,50,51] |
| 3. Indoor plants in workplaces or other non–healing indoor environments such as shopping centres. | Organisations shape policies and make provisions for indoor plants. | P | Enhance creativity, improve productivity, reduce absenteeism at work, improve mental wellbeing, improve air quality. | Those using indoor environments. | [52,53,54] |
| 4. Increased provision of public urban parks and gardens. | Additional new parks are provided. | P | Parks are provided to encourage outdoor leisure, engagement with nature, increase neighbourhood walkability and physical activity, with some of the cited health benefits including the physical benefits from exercise, enhanced social cohesion, mental wellbeing and quality of life outcomes. | Neighborhoods or entire towns. | [18,26,34,55,56,57,58] |
| 5. Improvement of urban public parks and gardens. | Improvement could include: (i) better public access to existing parks, including public transport provision and accessibility for those with disabilities, and improved equality in access across socioeconomic gradients; (ii) better street lighting and passive surveillance to reduce fear of crime; (iii) traffic reduction measures to reduce pollution and noise; (iv) enhancement of biodiversity within parks. | P | Improvement of parks to enhance community engagement with under–utilised parks and improve biodiversity to enhance the restorative benefits received. Some of the cited health benefits of parks include exercise, enhanced social cohesion and mental wellbeing and quality of life outcomes. | Neighborhoods or entire towns. | [59,60,61,62,63,64] |
| 6. Provision of walking or bike paths, or other shared use paths/trails. | Areas designed specifically for walking or biking. Includes paths through parks or natural areas that facilitate active travel. | P | Provide a facility that encourages physical activity, delivers the associated benefits, and improves general wellbeing. | General population in an area. | [65,66,67,68,69,70,71,72,73,74,75] |
| 7. Streetscape enhancement/green corridors along streets. | Councils plant vegetation along streets and support the efforts of residents to plant vegetation in their private or community gardens (includes both native and non–native species). | P | Enhance the environment for attention restoration, in part by improving the view from people’s homes. Indirect health benefits include better air quality, reduced heat island effects. | Neighborhoods or entire towns. | [76,77,78] |
| 8. Community gardens/allotments. | Gardens in accessible locations for community members to encourage engagement in growing one’s own food and to provide food education involving fruit and vegetables. | P | Improve nutrition, social connections and psychological benefits (e.g., confidence, psychological restoration). | Neighbourhoods or entire towns, sometimes with specific intended beneficiaries (e.g., age groups). | [79,80,81,82,83,84,85,86] |
| 9. Greening childcare or school grounds. | Increase amount and quality of natural elements, including around classrooms and play areas. | P | Increase physical activity, increase imaginative play, development of positive relationships, place of learning, attention restoration, overall improvement in health. | Children using the facility. | [87,88,89,90] |
| 10. Outdoor gym equipment. | Provide alternative exercise facilities, specifically outdoor versions of traditional gym equipment. | P | Encourage physical activity and promote the associated benefits and increased wellbeing in those reluctant to use traditional gyms or more motivated by being outdoors. | Neighbourhoods or entire towns, those reluctant to go to indoor gyms. | [91,92] |
| 11. Provision of accessible natural environments. | Location and spatial planning of accessible natural environments, with paths. Infrastructure created or improved in local woodlands, and a programme of social engagement. | P | Increase use of natural environments for health, recreation, leisure, etc. to facilitate health and wellbeing outcomes such as reduced stress, improvements in mood. | Local residents and wider populations. | [93,94,95,96] |
| Intervention | Description | T/P | Intervention Goals (i.e. Health Outcome) | Target Beneficiaries | Barriers to Implementation, Unintended Negative Impacts | Example References |
|---|---|---|---|---|---|---|
| 12. Green/nature/park/garden prescriptions. | Doctors (or other professionals) ‘prescribe’ or refer patients/clients to outdoor activities (often walks). | P/T | Increase exercise and the associated benefits, stress reduction, reduce blood pressure, improve healing times, reduce depression, increase resilience and other mental health benefits. Some are targeted towards children for purposes such as prevention or treatment of obesity, cancer and diabetes. Some also target quality of life, wellbeing and social support. | Individual patients or groups with a range of conditions. | Individual-level barriers: Geographic accessibility and availability of facilities (e.g., green spaces), affordability of the activity, social acceptability, physical and cognitive capability of individuals, perceived issues such as danger. Organisation-level barriers: Acceptability by and lack of knowledge of medical professionals, difficulty in changing behaviours of medical professionals. Potential unintended impacts: Could present risks for people with some conditions. | [31,32,97,98,99,100,101,102,103,104] |
| 13. Care–farming or farm therapy, including horticulture and animal–assisted therapy. | Therapeutic use of commercial farms and agricultural landscapes as a base for promoting mental and physical health, through normal farming activity or horticulture. | T | Mental health promotion and to reduce distress in people with dementia. Reduce social isolation. | Youth at risk; youth with special needs (e.g., autism); cancer survivors; mental disorders; people with lost functionality; people recovering from serious illness. | Not assessed in this study. | [83,105,106,107,108,109,110,111,112,113,114] |
| 14. Residential retreats. | Multi–modal therapies delivered in a removed natural setting. | T | Holistic wellbeing: physical, but primarily psychological (coping), social, spiritual. | Patients with chronic conditions such as cancer or cardiovascular disease. | Not assessed in this study. | [115] |
| 15. Wilderness therapy. | Structured nature–based activities and programmes in ‘wilder’ environments for ‘at risk’ groups or those recuperating or in recovery | P / T | Address social and psychological issues through a range of pathways, including by facilitating positive human–nature interactions, building self–esteem and fostering social connections. | People with severe mental health issues; youth at risk of involvement in crime; individuals who are imprisoned or on probation from crime; ex–offenders; victims of crime; children with ADHD; those living with or recovering from a range of mental and physical conditions; people with post–traumatic stress disorder. | Individual-level barriers: Geographic accessibility and availability of facilities (e.g., green spaces), affordability of the activity, social acceptability, some people may not appreciate the group context, physical ability, time (several days often required). Organisational level barriers: Poor system support, lack of financial resources to support the activities. Potential unintended impacts: Mental distress and physical injury in poorly managed activities, poor follow–on care. Often offered as a once–in–a–lifetime developmental boost, and they may be required more often. | [111,116,117,118,119,120,121,122,123,124,125] |
| 16. Wilderness programmes. | Programmes designed to challenge participants in natural environments. | P | Personal growth, social skills. | Often youth, but also targeting any interested people and groups. | Not assessed in this study. | [126,127] |
| 17. Ecotherapy. | Treatment modalities that include the natural world in relationships of mutual healing and growth, and as such are a form of applied ecopsychology. | T | Positive effects on psychological wellbeing, fitness and self–reported health. | People with symptoms of stress, or other mental health and wellbeing issues. | Not assessed in this study. | [128,129,130,131] |
| 18. Pet therapy, or pet–assisted therapy. | Use of pets, especially in hospitals to benefit patients. | T | Psychological wellbeing; social wellbeing. | Hospital inpatients; other vulnerable groups. | Not assessed in this study. | [132,133,134] |
| 19. Forest bathing. | Practice of spending time in forest settings, often with emphasis on attention to breathing and other meditative techniques | P / T | Improved physical and mental wellbeing. | People referred to the program or voluntary participation. | Not assessed in this study. | [95,96,100,135,136] |
| 20. Green gyms or environmental volunteering. | Active work in an outdoor environment, often with a focused conservation outcome. | P/T | Provide diverse benefits including physical activity, mental wellbeing, social connection/(re)integration. | People referred to the program or voluntary participation. | Individual-level barriers: Geographic accessibility (including transport) and availability of facilities (e.g., green spaces), affordability of the activity, social acceptability, availability of the programmes. Organisation-level barriers: Lack of financial resources, acceptability by and lack of knowledge of health professionals, difficulty in changing behaviours of health professionals. Potential unintended impacts: Chance of injuries and risk of other negative impacts of nature (e.g., insect bites, allergic responses), conflict in management of green spaces. Limited knowledge by host organisations of how to supervise people with physical or mental impairment. | [137,138,139,140,141,142,143,144] |
| 21. Outdoor exercise groups. | Groups with the specific aim of exercising in nature (most commonly walking) for health benefits. | P/T | Improve physical, psychological, social and spiritual wellbeing, including better cardio–vascular health, psychological wellbeing. | Local interested residents, or people referred to the program with a specific health condition, or voluntary participation. | Individual-level barriers: Geographic accessibility and availability of facilities (e.g., green spaces), affordability of the activity, social acceptability, concerns about, e.g., getting muddy or other issues, unfamiliarity with using non–urban environments, personality (e.g., introverts may elect out), mobility issues. Organisational-level barriers: Lack of financial resources or certainty, communication preferences for older individuals (e.g., social media). Potential unintended impacts: Chance of physical injury, group setting may engender negative feelings and interactions. | [72,128,145,146,147,148,149,150] |
| 22. Nature play/wild play. | Structured programmes designed to facilitate children’s play in natural environments. | P | Enhance child health and development through provision of social programmes and physical environments that promote varied play opportunities, improved attention and learning, physical activity, mental health. | Children (general). | Not assessed in this study. | [151,152,153,154,155,156,157] |
| 23. Forest Schools/outdoor classrooms/learning environment. | Programme of education in the outdoors (rather than about the outdoors). Typically children spend a period of their schooling (ranging from a couple of hours a week to all their time) undertaking outdoor activities. Forest school is both a pedagogy and a physical entity, with the use often being interchanged. | P | Provide alternative (and sometimes improved) learning environment, increase physical activity and the associated benefits. | Typically children, but has been used with adults and people with special needs. | Not assessed in this study. | [158,159,160,161] |
| 24. Children’s kitchen gardens. | Gardens in schools and kindergartens to encourage engagement in growing one’s own food and to increase access to fruit and vegetables | P | Improve nutrition, social connections and psychological benefits (e.g., confidence, team work skills), physical activity, educational outcomes, school–based quality of life. | Children in childcare, nurseries and schools. | Not assessed in this study. | [162,163,164,165,166,167,168,169,170,171] |
| 25. Outdoor education schemes. | Schemes designed to introduce children/adults to nature with the purpose of altering their knowledge about, attitudes toward and contact with nature. | P | Increase confidence to use natural environments for physical activity and recreation and promote the health and wellbeing benefits associated with this and increased nature exposure. | Largely children, but also aimed at adults from vulnerable groups (e.g., rehabilitation) and others. | Not assessed in this study. | [172] |
| 26. Promotion and facilitation campaigns. | Promotional campaigns (e.g., via media) to highlight and encourage engagement with natural environments and potential health benefits. | P | Increase awareness, engagement, use and experience of natural environments. | General population, but often targeted at specific groups such as different age groups. | Not assessed in this study. | [128,173] |
| 27. Blue gym. | Water– or shoreline–based activities. | P | Improve mental wellbeing. | General population. | Not assessed in this study. | [174] |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Shanahan, D.F.; Astell–Burt, T.; Barber, E.A.; Brymer, E.; Cox, D.T.C.; Dean, J.; Depledge, M.; Fuller, R.A.; Hartig, T.; Irvine, K.N.; et al. Nature–Based Interventions for Improving Health and Wellbeing: The Purpose, the People and the Outcomes. Sports 2019, 7, 141. https://doi.org/10.3390/sports7060141
Shanahan DF, Astell–Burt T, Barber EA, Brymer E, Cox DTC, Dean J, Depledge M, Fuller RA, Hartig T, Irvine KN, et al. Nature–Based Interventions for Improving Health and Wellbeing: The Purpose, the People and the Outcomes. Sports. 2019; 7(6):141. https://doi.org/10.3390/sports7060141
Chicago/Turabian StyleShanahan, Danielle F., Thomas Astell–Burt, Elizabeth A. Barber, Eric Brymer, Daniel T.C. Cox, Julie Dean, Michael Depledge, Richard A. Fuller, Terry Hartig, Katherine N. Irvine, and et al. 2019. "Nature–Based Interventions for Improving Health and Wellbeing: The Purpose, the People and the Outcomes" Sports 7, no. 6: 141. https://doi.org/10.3390/sports7060141
APA StyleShanahan, D. F., Astell–Burt, T., Barber, E. A., Brymer, E., Cox, D. T. C., Dean, J., Depledge, M., Fuller, R. A., Hartig, T., Irvine, K. N., Jones, A., Kikillus, H., Lovell, R., Mitchell, R., Niemelä, J., Nieuwenhuijsen, M., Pretty, J., Townsend, M., van Heezik, Y., ... Gaston, K. J. (2019). Nature–Based Interventions for Improving Health and Wellbeing: The Purpose, the People and the Outcomes. Sports, 7(6), 141. https://doi.org/10.3390/sports7060141







