Oral Health Conditions and Physical Performance in Two Different Professional Team Sports in Germany: A Cross-Sectional Study
Abstract
1. Introduction
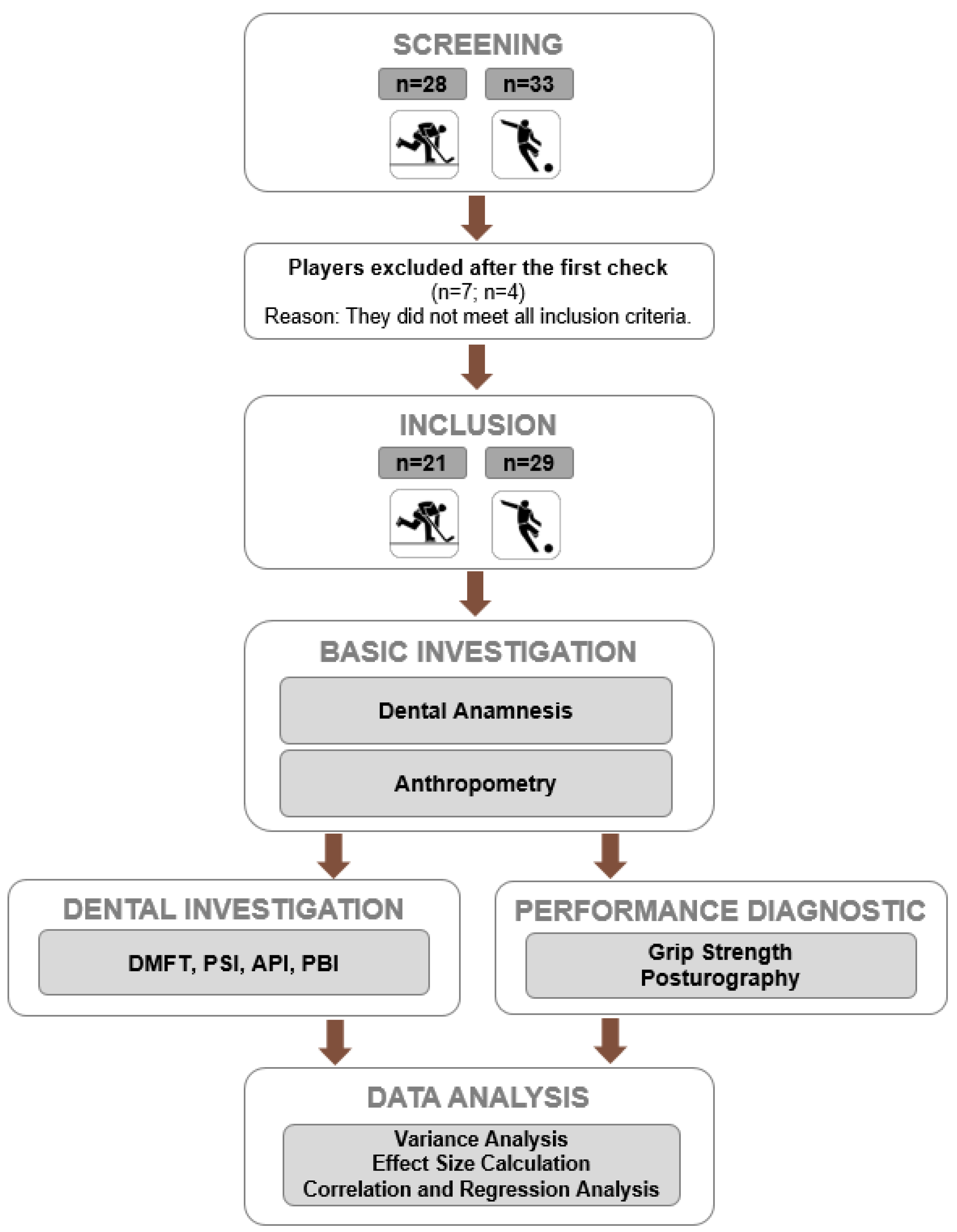
2. Materials and Methods
2.1. General Study Design
2.2. Participants
2.3. Testing Procedures
2.3.1. Questionnaire for Oral Health
- Did you have any injuries in the past two years?
- Did you ever have any surgery?
- Did you have any traumatic injuries related to sport activities inside your oral cavity?
- Do you have toothache?
- Do you suffer from tensions around your jaw joint/shoulder/neck?
- Do you use any additional oral care products?
2.3.2. Dental Indices and Scores
2.3.3. Dynamometry-Grip Strength
- -
- Participant seated in an upright posture with both hips and knees in 90° flexion with feet flat on the floor
- -
- The extremity itself has no contact with the body
- -
- The elbow is flexed at 90°, forearm in neutral position, wrist slightly extended (0° to 30°), and ulnar deviation ranging from 0° to 15°.
- -
- The non-dominant extremity should be relaxed at the side simultaneously.
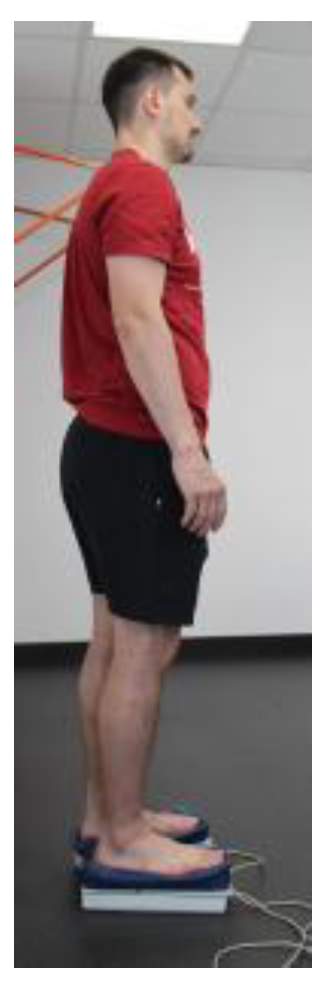
2.3.4. Dynamometry-Posturography (Posture Stability and Regulation)
2.4. Statistical Analysis
3. Results
3.1. Characteristics of the Included Participants
3.2. Normal Distribution
3.3. Results of the Dental Examination
- previous illnesses (5% vs. 11%, p = 0.480),
- medication intake (5% vs. 4%, p = 0.807),
- number of sick days (3.5 ± 2.1 vs. 3.3 ± 3.9, p = 0.797),
- number of injuries (80% vs. 68%, p = 0.351),
- past operations (70% vs. 50%, p = 0.166),
- traumatic injuries in the mouth (30% vs. 21%, p = 0.499),
- tooth pain (10% vs. 7%, p = 0.724),
- bleeding gums (30% vs. 18%, p = 0.327),
- grinding teeth (0% vs. 14%, p = 0.077),
- tension of the temporomandibular joint (35% vs. 4%, p = 0.004),
- previously treated orthodontically (35% vs. 46%, p = 0.428),
- regular check-ups (40% vs. 4%, p < 0.001),
- number of times teeth brushed per day (two times daily: 85% vs. 93%, p = 0.227),
- additional oral hygiene procedures (35% vs. 64%, p = 0.045),
- satisfaction with oral hygiene (80% vs. 89%, p = 0.369),
- changes in teeth (40% vs. 43%, p = 0.843),
- impact on competitive sport (5% vs. 14%, p = 0.299).
3.4. Comparison Ice Hockey vs. Soccer and Comparison Based on Specific Reference Data
3.5. Associations Between Oral Health and Performance Parameters
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| API | Approximal Plaque Index |
| BH | Body Height |
| BM | Body Mass |
| BMI | Body Mass Index |
| CI | Confidence Interval |
| DMFT | Decayed, Missing, Filled Teeth |
| IBS | Interactive Balance System |
| IDR | Interdecile Range |
| OR | Odds Ratio |
| PBI | Periodontal Bleeding Index |
| PSI | Periodontal Screening Index |
| SD | Standard Deviation |
| Synch | Synchronization |
References
- Spanemberg, J.C.; Cardoso, J.A.; Slob, E.M.G.B.; Lopez-Lopez, J. Quality of life related to oral health and its impact in adults. J. Stomatol. Oral Maxillofac. Surg. 2019, 120, 234–239. [Google Scholar] [CrossRef] [PubMed]
- Natarajan, P.; Madanian, S.; Marshall, S. Investigating the link between oral health conditions and systemic diseases: A cross-sectional analysis. Sci. Rep. 2025, 15, 10476. [Google Scholar] [CrossRef] [PubMed]
- Magalhaes, F.C.O.; Marques da Silva, C.E.; Springer, C.R.; Carteri, R.B.; Luiz Lopez, A.; Costa Teixeira, B.; Capitanio de Souza, B. Survey on Oral Health and History of Muscle Injury in Professional Athletes of Brazilian Women’s Soccer: A Cross-Sectional Self-Reported Study. Curr. Res. Dent. 2022, 13, 1–10. [Google Scholar] [CrossRef]
- Ashley, P.; Di Iorio, A.; Cole, E.; Tanday, A.; Needleman, I. Oral health of elite athletes and association with performance: A systematic review. Br. J. Sports Med. 2015, 49, 14–19. [Google Scholar] [CrossRef]
- Niszezak, C.M.; Sonza, A.; Santos, G.M. Pain, dynamic postural control, mental health and impact of oral health in individuals with temporomandibular disorder: A cross-sectional study. J. Bodyw. Mov. Ther. 2024, 40, 1231–1237. [Google Scholar] [CrossRef]
- Niszezak, C.M.; Sonza, A.; Garrett, A.; Santos, G.M. Muscle oxygenation and pain in different types of temporomandibular disorders: A cross-sectional study. Clin. Oral Investig. 2024, 28, 410. [Google Scholar] [CrossRef]
- Moriya, S.; Muramatsu, T.; Tei, K.; Nakamura, K.; Muramatsu, M.; Notani, K.; Inoue, N. Relationships between oral conditions and physical performance in a rural elderly population in Japan. Int. Dent. J. 2009, 59, 369–375. [Google Scholar]
- Hansen, P.; Nygaard, H.; Schultz, M.; Dela, F.; Aagaard, P.; Ryg, J.; Suetta, C. Frailty is associated with a history of falls among mobility-limited older adults-cross-sectional multivariate analysis from the BIOFRAIL study. Eur. Geriatr. Med. 2025. Online ahead of print. [Google Scholar] [CrossRef]
- Schulze, A.; Busse, M. Sports Diet and Oral Health in Athletes: A Comprehensive Review. Medicina 2024, 60, 319. [Google Scholar] [CrossRef]
- Mielle, B.; Judice, A.; Proenca, L.; Machado, V.; Vieira, A.M.; Mendes, J.J.; Manso, C.; Rozan, C.; Botelho, J. Dental Caries, Tooth Erosion and Nutritional Habits in a Cohort of Athletes: A Cross-Sectional Study. Nutrients 2025, 17, 543. [Google Scholar] [CrossRef]
- Rattai, J.; Levin, L. Oral injuries related to Ice Hockey in the province of Alberta, Canada: Trends over the last 15 years. Dent. Traumatol. 2018, 34, 107–113. [Google Scholar] [CrossRef] [PubMed]
- Needleman, I.; Ashley, P.; Petrie, A.; Fortune, F.; Turner, W.; Jones, J.; Niggli, J.; Engebretsen, L.; Budgett, R.; Donos, N.; et al. Oral health and impact on performance of athletes participating in the London 2012 Olympic Games: A cross-sectional study. Br. J. Sports Med. 2013, 47, 54–1058. [Google Scholar] [CrossRef] [PubMed]
- Gallagher, J.; Ashley, P.; Aviva, P.; Needleman, I. Oral health and performance impacts in elite and professional athletes. Community Dent. Oral Epidemiol. 2018, 46, 563–568. [Google Scholar] [CrossRef] [PubMed]
- Opazo-García, C.; Moya-Salazar, J.; Chicoma-Flores, K.; Contreras-Pulache, H. Oral health problems in high-performance athletes at 2019 Pan American Games in Lima: A descriptive study. BDJ. Open 2021, 7, 21. [Google Scholar] [CrossRef]
- Kragt, L.; Moen, M.; Van Den Hoogenband, C.; Wolvius, E. Oral health among Dutch elite athletes prior to Rio 2016. Phys. Sportsmed. 2019, 47, 182–188. [Google Scholar] [CrossRef]
- Konviser, S.N.; Nurek, M.; Needleman, I. Disadvantage starts early: Academy football has high levels of oral disease. BMJ Open 2025, 11, e02245. [Google Scholar] [CrossRef]
- Sevindik, B.; Sengül, F.; Kiyici, F. Evaluation of Oral and Dental Health Results and Competition Stress Levels of Adolescent Athletes in Different Winter Sports Branches. Eurasian J. Med. 2024, 56, 114–120. [Google Scholar] [CrossRef]
- Needleman, I.; Ashley, P.; Fine, P.; Haddad, F.; Loosemore, M.; de Medici, A.; Donos, N.; Newton, T.; van Someren, K.; Moazzez, R.; et al. Consensus statement: Oral health and elite sport performance. Br. Dent. J. 2014, 217, 587–590. [Google Scholar] [CrossRef]
- Mattila, V.M.; Raisamo, S.; Pihlajamäki, H.; Mäntysaari, M.; Rimpelä, A. Sports activity and the use of cigarettes and snus among young males in Finland in 1999–2010. BMC Public Health 2012, 12, 230. [Google Scholar] [CrossRef]
- Zandonai, T.; Botré, F.; Abate, M.G.; Peiro, A.M.; Müdel, T. Should We be Concerned with Nicotine in Sport? Analysis from 60,802 Doping Control Tests in Italy. Sports Med. 2023, 53, 1273–1279. [Google Scholar] [CrossRef]
- Tripodi, D.; Cosi, A.; Fulco, D.; DÈrcole, S. The Impact of Sport Training on Oral Health in Athletes. Dent. J. 2021, 9, 51. [Google Scholar] [CrossRef] [PubMed]
- Katz, J.; Rotstein, I. Prevalence of Periapical Abscesses in Patients with Hypertension: A Cross-sectional Study of a Large Hospital Population. J. Endod. 2021, 47, 1070–1074. [Google Scholar] [CrossRef] [PubMed]
- Abraham, D.; Gupta, A.; Duraisamy, A.K.; Mrinalini, M. The influence of chronic periodontitis and type 2 diabetes mellitus on resistin levels of gingival crevicular fluid—A systematic review and meta-analysis. J. Oral Biol. Craniofac. Res. 2025, 15, 612–623. [Google Scholar] [CrossRef]
- Ferraz, D.C.; Dotto, M.E.P.; Vieira, W.A.; Paranhos, L.R.; Moura, C.C.G. Apical Periodontitis and Systemic Health: A Bibliometric Analysis of the Top 100 Most-cited Publications. J. Endod. 2025, 51, 268–278. [Google Scholar] [CrossRef]
- Fu, D.; Shu, X.; Zhou, G.; Ji, M.; Liao, G.; Zou, L. Connection between oral health and chronic diseases. MedComm (2020) 2025, 6, e70052. [Google Scholar] [CrossRef]
- Lopez, L.Z.; Taques Neto, L.; Arcaro, G.; da Rosa, F.G.; Cruz, K.T.; Pochapski, M.T.; Santos, F.A.D. Periodontal condition and quality of life in patients with controlled chronic systemic diseases: A cross-sectional study. Dent. Med. Probl. 2025, 62, 237–245. [Google Scholar] [CrossRef]
- Öcbe, M.; Celebi, E.; Öcbe, C.B. An overlooked connection: Oral health status in patients with chronic diseases. BMC Oral Health 2025, 25, 314. [Google Scholar] [CrossRef]
- Holmlund, A.; Holm, G.; Lind, L. Number of teeth as a predictor of cardiovascular mortality in a cohort of 7674 subjects followed for 12 years. J. Periodontol. 2010, 81, 870–876. [Google Scholar] [CrossRef]
- Larvin, H.; Kang, J.; Aggarwal, V.R.; Pavitt, S.; Wu, J. Risk of incident cardiovascular disease in people with periodontal disease: A systematic review and meta-analysis. Clin. Exp. Dent. Res. 2021, 7, 109–122. [Google Scholar] [CrossRef]
- Schulze, Z.J.; Schubert, F.; Gernhardt, C.R.; Krayl, N.; Peters, A.; Unverzagt, S.; Wagner, K.; Wienke, A.; Führer, A. Area-Level Factors of Dental Caries in Children and Adolescents in European Neighborhoods—A Systematic Review. J. Urban Health 2025, 102, 125–138. [Google Scholar] [CrossRef]
- Abnet, C.C.; Qiao, Y.L.; Dawsey, S.M.; Dong, Z.W.; Taylor, P.R.; Mark, S.D. Tooth loss is associated with increased risk of total death and death from upper gastrointestinal cancer, heart disease, and stroke in a Chinese population-based cohort. Int. J. Epidemiol. 2005, 34, 467–474. [Google Scholar] [CrossRef] [PubMed]
- Zhang, J.S.; Chu, C.H.; Yu, O.Y. Oral Microbiome and Dental Caries Development. Dent. J. 2022, 10, 184. [Google Scholar] [CrossRef] [PubMed]
- Lu, Y.; Li, Z.; Peng, X. Regulatory effects of oral microbe on intestinal microbiota and the illness. Front. Cell. Infect. Microbiol. 2023, 13, 1093967. [Google Scholar] [CrossRef]
- AlShammari, A.; AlSaleh, S.; AlKandari, A.; AlSaqabi, S.; AlJalahmah, D.; AlSulimanni, W.; AlDosari, M.; AlHazmi, H.; AlQaderi, H. The association between dental caries and serum crp in the us adult population: Evidence from NHANES 2015–2018. BMC Public Health 2024, 24, 2210. [Google Scholar] [CrossRef]
- Liu, R.; Liu, Y.; Yi, J.; Fang, Y.; Guo, Q.; Cheng, L.; He, J.; Li, M. Imbalance of oral microbiome homeostasis: The relationship between microbiota and the occurrence of dental caries. BMC Microbiol. 2025, 25, 46. [Google Scholar] [CrossRef]
- Millum, J.; Wendler, D.; Emanuel, E.J. The 50th Anniversary of the Declaration of Helsinki. JAMA 2013, 310, 2143. [Google Scholar] [CrossRef]
- Robertson, M.D.; Schwendicke, F.; Pinheiro de Auraujo, M.; Radford, J.R.; Harris, J.C.; McGregor, S.; Innes, N.P.T. Dental caries experience, care index and restorative index in children with learning disabilities and children without learning disabilities; a systematic review and meta-analysis. BMC Oral Health 2019, 19, 146. [Google Scholar] [CrossRef]
- Merle, C.L.; Richter, L.; Challakh, N.; Haak, R.; Schmalz, G.; Needleman, I.; Wolfarth, B.; Ziebholz, D.; Wüstenfeld, J. Orofacial conditions and oral health behavior of young athletes: A comparison of amateur and competitive sports. Scand. J. Med. Sci. Sports 2022, 32, 903–912. [Google Scholar] [CrossRef]
- Ferreira, M.K.M.; Ferreira, R.O.; Castro, M.M.L.; Almeida, A.P.C.P.C.; Fagundes, N.C.F.; Maia, L.C.; Lima, R.R. Is there an association between asthma and periodontal disease among adults? Systematic review and meta-analysis. Life Sci. 2019, 223, 74–87. [Google Scholar] [CrossRef]
- MacDermid, J.; Solomon, G.; Valdes, K. Clinical Assessment Recommendations; American Society of Hand Therapists: Mount Laurel, NJ, USA, 2015. [Google Scholar]
- Ringhof, S.; Stein, T.; Potthast, W.; Schindler, H.J.; Hellmann, D. Force-controlled biting alters postural control in bipedal and unipedal stance. J. Oral Rehabil. 2015, 42, 173–184. [Google Scholar] [CrossRef]
- Julia-Sanchez, S.; Alvarez-Herms, J.; Burtscher, M. Dental occlusion and body balance: A question of environmental constraints? J. Oral Rehabil. 2019, 46, 388–397. [Google Scholar] [CrossRef] [PubMed]
- Quinney, H.A.; Dewart, R.; Game, A.; Snydmiller, G.; Warburton, D.; Bell, G. A 26 year physiological description of a National Hockey League team. Appl. Physiol. Nutr. Metab. 2008, 33, 753–760. [Google Scholar] [CrossRef] [PubMed]
- Friedrich, M.; Grein, H.J.; Wicher, C.; Schuetze, J.; Müller, A.; Lauenroth, A.; Hottenrott, K.; Schwesig, R. Influence of pathologic and simulated visual dysfunctions on the postural system. Exp. Brain Res. 2008, 186, 305–314. [Google Scholar] [CrossRef]
- Schwesig, R.; Goldich, Y.; Hahn, A.; Müller, A.; Kohen-Raz, R.; Kluttig, A.; Morad, Y. Postural control in subjects with visual impairment. Eur. J. Ophthalmol. 2011, 21, 303–309. [Google Scholar] [CrossRef]
- Zeh, A.; Stier, J.; Meyer, L.; Wohlrab, D.; Gutteck, N.; Schulze, S.; Panian, M.; Delank, K.S.; Laudner, K.G.; Schwesig, R. No clinical relevant differences in early clinical outcomes, patient satisfaction and objective gait and posture analysis between a custom versus off-the-shelf total knee arthroplasty: A prospective controlled study. Arch. Orthop. Trauma Surg. 2025, 145, 245. [Google Scholar] [CrossRef]
- Reinhardt, L.; Heilmann, F.; Teicher, M.; Wollny, R.; Lauenroth, A.; Delank, K.S.; Schwesig, R.; Kurz, E. Comparison of posturographic outcomes between two different devices. J. Biomech. 2019, 86, 218–224. [Google Scholar] [CrossRef]
- Schwesig, R.; Becker, S.; Fischer, D. Intraobserver reliability of posturography in healthy subjects. Somatosens. Mot. Res. 2014, 31, 16–22. [Google Scholar] [CrossRef]
- Schwesig, R.; Fischer, D.; Kluttig, A. Are there changes in postural regulation across the life span? Somatosens. Mot. Res. 2013, 30, 167–174. [Google Scholar] [CrossRef]
- Richardson, J.T.E. Eta squared and partial eta squared as measures of effect size in educational research. Educ. Res. Rev. 2011, 6, 135–147. [Google Scholar] [CrossRef]
- Hartmann, A.; Herzog, T.; Drinkmann, A. Psychotherapy of bulimia nervosa: What is effective? A meta-analysis. J. Psychosom. Res. 1992, 36, 159–167. [Google Scholar] [CrossRef]
- Cohen, J. Statistical Power Analysis for the Behavioural Sciences; Lawrence Earlbaum Associates: Hillside, NJ, USA, 1988; pp. 77–83+278–280. [Google Scholar]
- Noether, G.E. Sample size determination for some common nonparametric tests. J. Am. Stat. Assoc. 1987, 82, 645–647. [Google Scholar] [CrossRef]
- Gay-Escoda, C.; Vieira-Duarte-Pereira, D.; Ardèvol, J.; Pruna, R.; Fernandez, J.; Valmaseda-Castellón, N. Study of the effect of oral health on physical condition of professional soccer players of Football Club Barcelona. Med. Oral Patol. Oral Cir. Bucal. 2011, 16, e436–e439. [Google Scholar] [CrossRef] [PubMed]
- Chantaramanee, A.; Siangruangsaeng, K.; Chittaputta, P.; Daroonpan, P.; Jaichum, P.; Jommoon, P.; Laohachaiaroon, P.; Champeecharoensuk, S.-A.; Sitthirat, T.; Samnieng, P. Oral health status of the professional soccer players in Thailand. J. Dent. Ind. 2016, 23, 1–4. [Google Scholar] [CrossRef]
- Needleman, I.; Ashley, P.; Meehan, L.; Petrie, A.; Weiler, R.; McNally, S.; Ayer, C.; Hanna, R.; Hunt, I.; Kell, S.; et al. Poor oral health including active caries in 187 UK professional male football players: Clinical dental examination performed by dentists. Br. J. Sports Med. 2016, 50, 41–44. [Google Scholar] [CrossRef]
- Needleman, I.; Ashley, P.; Weiler, R.; McNally, S. Oral health screening should be a routine in professional football: A call to action for sports and exercise medicine (SEM) clinicans. Br. J. Sports Med. 2016, 50, 1295–1296. [Google Scholar] [CrossRef]
- Toong, T.; Wilson, K.E.; Urban, K.; Paniccia, M.; Hunt, A.W.; Keightley, M.; Reed, N. Grip Strength in Youth Ice Hockey Players: Normative Values and Predictors of Performance. J. Strength Cond. Res. 2018, 32, 3494–3502. [Google Scholar] [CrossRef]
- Gouveia, J.N.; Franca, C.; Martins, F.; Henriques, R.; de Maio Nascimento, M.; Ihle, A.; Sarmento, H.; Przednowek, K.; Martinho, D.; Gouveia, E.R. Characterization of static strength, vertical jumping, and isokinetic strength in soccer players according to age, competitive level, and field position. Int. J. Environ. Res. Public Health 2023, 20, 1799. [Google Scholar] [CrossRef]
- Huemer, M.T.; Kluttig, A.; Fischer, B.; Ahrens, W.; Castell, S.; Ebert, N.; Gastell, S.; Jöckel, K.H.; Kaaks, R.; Karch, A.; et al. Grip strength values and cut-off points based on over 200,000 adults of the German National Cohort—A comparison to the EWGSOP2 cut-off points. Age Aging 2023, 52, afac324. [Google Scholar] [CrossRef]
- Schulze, S.; Laudner, K.G.; Delank, K.S.; Bartels, T.; Marshall, R.P.; Schwesig, R. Position-specific reference data for an ice hockey-specific complex test—An up-date and practical recommendations. Appl. Sci. 2024, 14, 7648. [Google Scholar] [CrossRef]

| Soccer | Ice Hockey | Variance Analysis | ||
|---|---|---|---|---|
| p | ηp2 | |||
| Age [years] | 24.3 ± 4.13 | 27.7 ± 3.55 | 0.004 | 0.16 |
| Height [m] | 1.83 ± 0.06 | 1.82 ± 0.07 | 0.555 | 0.01 |
| Body mass [kg] | 80.3 ± 7.59 | 86.5 ± 9.10 | 0.011 | 0.13 |
| BMI [kg/m2] | 24.0 ± 1.78 | 26.1 ± 1.82 | <0.001 | 0.27 |
| Sick days [d] | 3.25 ± 3.93 | 3.50 ± 2.09 | 0.797 | 0 |
| Parameter | Soccer (n = 28) | Ice Hockey (n = 20) | Mann–Whitney U Test (p) |
|---|---|---|---|
| DMFT | 3.5 (0–9.2) | 5.5 (0.2–13.0) | 0.062 |
| DT | 0 (0–1.1) | 0 (0–2.0) | 0.969 |
| MT | 0 (0–2.0) | 0 (0–2.0) | 0.105 |
| FT | 3.0 (0–7.2) | 4.0 (0.1–11.0) | 0.152 |
| PSI | 1.0 (0.9–2.1) | 2.0 (2.0–3.0) | <0.001 |
| API (%) | 28.5 (9.4–54.3) | 47.5 (22.3–72.7) | 0.001 |
| PBI (%) | 14.0 (0–39.3) | 41.5 (11.3–67.3) | <0.001 |
| Parameter | Soccer (n = 29) | Ice Hockey (n = 21) | Variance Analysis | ||
|---|---|---|---|---|---|
| p | ηp2 | d | |||
| Combined grip strength in physiological rest position of the mandibula | |||||
| absolute (kg) | 101 ± 11.3 (96.2–105) | 106 ± 13.0 (100–111) | 0.151 | 0.04 | 0.41 |
| relative (kg/kg BM) | 1.26 ± 0.16 (1.20–1.33) | 1.23 ± 0.17 (1.16–1.30) | 0.493 | 0.01 | 0.42 |
| Combined grip strength in maximal intercuspal position of the mandibula | |||||
| absolute (kg) | 106 ± 13.4 (101–112) | 110 ± 13.4 (104–116) | 0.383 | 0.02 | 0.30 |
| relative (kg/kg BM) | 1.33 ± 0.17 (1.26–1.39) | 1.28 ± 0.17 (1.20–1.35) | 0.313 | 0.02 | 0.29 |
| Parameter | Soccer (n = 27) | Ice Hockey (n = 21) | Reference Data | |
|---|---|---|---|---|
| Mean (SD) | 95% CI | |||
| F1 | 19.3 ± 6.09 (16.9–21.7) | 17.5 ± 6.17 (14.8–20.1) | 14.6 (4.23) | 14.1–15.2 |
| p/ηp2/d | 0.319/0.02/0.29 | |||
| F2–4 | 8.76 ± 1.95 (8.03–9.50) | 8.68 ± 1.81 (7.85–9.51) | 8.15 (1.94) | 7.87–8.43 |
| p/ηp2/d | 0.884/0/0.04 | |||
| F5–6 | 3.55 ± 0.82 (3.22–3.89) | 3.69 ± 0.94 (3.31–4.07) | 3.58 (0.90) | 3.45–3.70 |
| p/ηp2/d | 0.587/0.01/0.16 | |||
| F7–8 | 0.70 ± 0.17 (0.63–0.78) | 0.71 ± 0.22 (0.62–0.79) | 0.66 (0.19) | 0.64–0.69 |
| p/ηp2/d | 0.935/0/0.05 | |||
| ST | 20.1 ± 4.98 (17.9–22.3) | 20.9 ± 6.36 (18.4–23.3) | 16.7 (3.86) | 16.2–17.3 |
| p/ηp2/d | 0.637/0.01/0.14 | |||
| WDI | 6.59 ± 2.74 (5.73–7.45) | 4.27 ± 1.25 (3.29–5.24) | 5.21 (2.17) | 4.95–5.47 |
| p/ηp2/d | <0.001/0.22/1.16 | |||
| Heel (%) | 42.0 ± 9.43 (38.8–45.1) | 49.6 ± 6.04 (46.1–53.2) | 46.6 (8.07) | 45.6–47.6 |
| p/ηp2/d | 0.002/0.19/0.98 | |||
| Left (%) | 50.6 ± 2.84 (49.3–51.8) | 49.7 ± 3.78 (48.3–51.1) | 50.1 (3.29) | 49.7–50.5 |
| p/ηp2/d | 0.370/0.02/0.27 | |||
| Synchronization | 603 ± 133 (549–657) | 670 ± 149 (608–731) | 625 (119) | 608–642 |
| p/ηp2/d | 0.108/0.06/0.48 | |||
| Dependent Variables | Independent Posturographic Variables | ||||
|---|---|---|---|---|---|
| r2 | Parameter | OR | 95% CI | p | |
| general injuries | 0.10 | - | |||
| general surgeries | 0.11 | - | |||
| traumatic mouth injury | 0.53 | F 1 | 0.75 | 0.60–0.93 | 0.01 |
| F 2–4 | 3.88 | 1.33–11.4 | 0.01 | ||
| Synch. | 1.01 | 1.00–1.02 | 0.02 | ||
| tooth pain | 0.05 | - | |||
| tension of the temporomandibular joint | 0.39 | - | |||
| Dependent Variables | Independent Posturographic Variables | ||||
|---|---|---|---|---|---|
| r2 | Parameter | OR | 95% CI | p | |
| general injuries | 0.20 | - | |||
| general surgeries | 0.37 | - | |||
| traumatic mouth injury | 0.58 | F 1 | 0.75 | 0.59–0.95 | 0.02 |
| F 2–4 | 4.59 | 1.28–16.5 | 0.02 | ||
| Synch. | 1.01 | 1.00–1.02 | 0.03 | ||
| tooth pain | 0.10 | - | |||
| tension of the temporomandibular joint | 0.52 | WDI | 0.28 | 0.09–0.95 | 0.04 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Schwesig, R.; Born, P.; Kurz, E.; Schulze, S.; Panian, M.; Marshall, R.P.; Bartels, T.; Wienke, A.; Gernhardt, C.R. Oral Health Conditions and Physical Performance in Two Different Professional Team Sports in Germany: A Cross-Sectional Study. Sports 2025, 13, 206. https://doi.org/10.3390/sports13070206
Schwesig R, Born P, Kurz E, Schulze S, Panian M, Marshall RP, Bartels T, Wienke A, Gernhardt CR. Oral Health Conditions and Physical Performance in Two Different Professional Team Sports in Germany: A Cross-Sectional Study. Sports. 2025; 13(7):206. https://doi.org/10.3390/sports13070206
Chicago/Turabian StyleSchwesig, René, Paulina Born, Eduard Kurz, Stephan Schulze, Matti Panian, Robert Percy Marshall, Thomas Bartels, Andreas Wienke, and Christian Ralf Gernhardt. 2025. "Oral Health Conditions and Physical Performance in Two Different Professional Team Sports in Germany: A Cross-Sectional Study" Sports 13, no. 7: 206. https://doi.org/10.3390/sports13070206
APA StyleSchwesig, R., Born, P., Kurz, E., Schulze, S., Panian, M., Marshall, R. P., Bartels, T., Wienke, A., & Gernhardt, C. R. (2025). Oral Health Conditions and Physical Performance in Two Different Professional Team Sports in Germany: A Cross-Sectional Study. Sports, 13(7), 206. https://doi.org/10.3390/sports13070206









