Abstract
Background: Infrared thermography and acute muscle fatigue are often correlated in sports medicine for assessing muscle health during and after exercise, but there are no known studies describing the response throughout exercise; therefore, this study aims to observe the variation in skin temperature (Tsk) during the execution of a maximal muscle fatigue protocol using concentric exercises in the triceps suralis. Methods: An open cross-sectional descriptive observational study of the posterior region of the leg (triceps suralis) was performed using 98 healthy subjects. Volunteers were subjected to a maximal fatigue protocol, with thermographic images analyzed at 25%, 50%, 75%, and 100% cumulative maximal fatigue. Results: Results showed a significant difference in time (p = 0.039; η2p = 0.026) and side (p =≤ 0.001; η2p = 0.120). Tukey’s post hoc analysis detected a significant difference in Tsk B between the R and L side (R, 30.3 ± 1.39 °C; L, 30.2 ± 1.39 °C), in Tsk at 25% (R, 30.2 ± 1. 27 °C; L; 30.1 ± 1.27 °C), in Tsk at 50% (R, 30.2 ± 1.29 °C; L, 30.1 ± 1.29 °C), and in Tsk at 75% (R, 30.3 ± 1.33 °C; L, 30.2 ± 1.33 °C). Conclusions: The results observed in this study show that infrared thermography is a valid tool for the measurement, analysis, and quantification of the tissue metabolic response of the muscular system, pre, during, and after exercise. Therefore, we believe that, for future studies, it would be interesting to find relationships between Tsk variations and other performance and metabolic variables. The focus on a single muscle and not directly measuring muscle activity are two limitations of this study.
1. Introduction
Infrared thermography (IRT) and acute muscle fatigue (until exhaustion) are correlated in the context of sports medicine in order to assess muscle health and monitor the body’s response to intense physical exertion by detecting thermal signatures associated with underlying physiological processes [1]. It is known that during the contractile process leading to muscle fatigue, biochemical, metabolic, and physiological changes are experienced in the muscle, such as increased lactate production [2], reduced energy levels (e.g., ATP) [3], and accumulation of metabolic by-products. These processes, in turn, generate alterations in vascular dynamics which can modulate peripheral blood flow and consequently, surface skin temperature [4].
In this context, according to some authors, IRT has been suggested in the last decade as a very efficient tool for monitoring the metabolic responses associated with muscle contraction, since this technique makes it possible to determine, from superficial skin analysis, changes in blood flow and physiological activity in deep tissues quickly and non-invasively, without contact [5,6]. IRT enables the identification of both hypothermic and hyperthermic patterns suggestive of persistent physiological stress, since cutaneous temperature reflects thermoregulatory adjustments connected to cellular activity in deeper layers [7].
In the neurological field, IRT is being used with very promising results in the quantification of trophic tissue in relation to functional muscle activity [8]. In the oncological field, the study of cancerous processes through thermography has advanced greatly over the last decade, providing information on the metabolic activity of tumor masses [9], and in the field of diagnostic medicine, there are numerous studies in which its reliability and validity have been proven in relation to different pathologies [10].
In the current landscape of sports medicine, this tool is being widely used, not only to detect early and late changes in muscle responses in relation to fatigue [11], but also to generate new knowledge through the assessment by thermograms of muscle overload and the prevention of injury or recovery from it in the medium to long term, especially in the lower extremities [12]. However, despite the new knowledge generated, there is still no single consensus on the specific thermoregulatory response obtained according to the type of exercise performed, the duration of the test, and the patient profile measured.
Some authors have advanced the hypothesis that in aerobic exercise, skin temperature (Tsk) tends to decrease in the exercised regions [13,14], while in strength training, a hyperthermic response is generated in the requested muscle groups [15,16]; however, there is a lack of studies confirming these results, and the literature often offers contrasting data [17,18]. This could be because current studies, on the one hand, have not reached a consensus on an exhaustive explanation from the thermographic point of view in relation to metabolic processes, and on the other, the samples are usually small and difficult to compare. Previous research examining thermographic responses to exercise was often limited by small sample sizes and the exclusive use of pre- and post-exercise measurements, without continuous monitoring throughout the exercise session. For example, Fink et al. [19] assessed changes in skin temperature before and after exercise, which limited their ability to capture dynamic thermoregulatory adjustments during the development of muscle fatigue.
Few studies have conducted continuous monitoring during exercise, a limitation that has made it difficult to understand dynamic thermoregulatory adjustments in real time. By contrast, our study incorporated continuous thermographic monitoring during the exercise protocol, allowing for real-time assessment of temperature fluctuations at different intensity stages (25%, 50%, 75%, and 100% of total effort). This methodological approach provides a more comprehensive understanding of thermal behavior during progressive fatigue, overcoming the limitations of previous studies that focused solely on static pre- and post-comparisons. Therefore, the present study aimed to investigate skin temperature variations during the execution of a maximal muscle fatigue protocol, using concentric exercises targeting the triceps suralis. The analysis also considered the participants’ genders and any potential distinctions between the left and right sides. We postulated that the protocol’s increasing metabolic demands would cause detectable temperature changes in the exercised area, indicating the degree of physiological stress.
2. Materials and Methods
2.1. Study Design
This open cross-sectional descriptive observational study of the posterior leg region (triceps suralis) in healthy subjects was performed in two laboratory views. The first familiarization session was performed 3 days before the development of the stress test and was used to confirm that the volunteer was suitable to participate in the study and to record data regarding age, sex, and BMI. From the familiarization day until the test days, participants were not allowed to do any type of exercise. In addition, in this session, the volunteers were familiarized with the thermographic evaluation position and the development of the maximal gastrocnemius fatigue protocol. During this phase, all volunteers were notified about exercise habits throughout the data-gathering timeframe. Considering the sensitivity and ongoing utilization of the calf muscles, it was recommended to decrease walking frequency and to refrain from standing for extended durations. The protocol used during the test is described in Section 2.4. The second session was used for measurement and stress testing. The study was conducted based on the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) guidelines [20]. As it enables the description and analysis of physiological and thermographic variables in a particular population under carefully monitored experimental conditions—without modifying any independent variables—this design was selected. The study’s goal of describing the skin temperature response during an exercise regimen until exhaustion is in line with the open cross-sectional descriptive observational approach.
All participants received an information sheet and signed the informed consent form at the first visit. The study was carried out in accordance with the Declaration of Helsinki for Research on Human Subjects [21] and was approved by the ethics committee of the Universidad Católica San Antonio de Murcia with code (CE032402).
2.2. Participants
None of the participants received economic incentives to participate in the study. A total of 100 healthy young subjects were recruited through an open advertisement (by email) at the Universidad Católica San Antonio de Murcia. Subjects who were of legal age, without gender or race limits, who were not semi-professional, professional or elite athletes, were included; subjects who had contraindications to muscle fatigue or who presented any issue that influenced the IT results, according to the investigators, were excluded. Participants were recreationally active, defined as individuals who engaged in planned, structured physical activity of moderate to vigorous intensity, including aerobic and strength training exercises, at least three times per week for a minimum of 30 min per session. Subjects in a febrile state, i.e., subjects with muscle or joint pain in the posterior region of the leg, were excluded from the study. Finally, 2 participants were excluded due to non-specific knee pain, so that a total of 98 subjects were considered eligible to participate in the study. The sample size was calculated using G*Power (version 3.1) for a repeated measures ANOVA (within–between contrast), considering the time × sex interaction. The following assumptions were considered: effect size f = 0.10 (small effect), α = 0.05, power = 0.90, number of groups = two (gender), number of measures = 10 (time levels were multiplied by 2 to incorporate the left/right factor), correlation between repeated measures = 0.60, and non-sphericity correction ε = 1. With these parameters, the required sample size was N = 12, correlation between repeated measures = 0.60, and non-sphericity correction ε = 1. With these parameters, the required sample size was N = 82 subjects (≈41 per group). To compensate for possible dropouts, additional recruitment (15%) was planned, resulting in a total sample of 95 subjects.
2.3. Equipment and Thermographic Protocols
The Flir E75 thermal camara (Wilsonville, OR, USA) was used, setting the emissivity at 0.98 [22]. BMI data were obtained using Tanita BC-545 Innerscan Segmental Body Composition Monitor (Tanita Corporation, Itabashi-ku, Tokyo, Japan). Volunteers underwent thermal acclimatization for 15 min in the room (25 m2) maintained at a constant temperature between 23 °C ± 1 °C, wearing shorts and short-sleeved T-shirts. The humidity never exceeded 40 ± 0.8%, and the atmospheric pressure was maintained at 1 ATM. The temperature and humidity in the room were monitored and recorded using a digital hygrometer and controlled using the air conditioning units located in the room. There were no electronic devices or sources of artificial light and heat near the measurement point that could influence the volunteers’ body temperatures. The thermographic device was turned on 1 h before the first recording and was located 1 m from the patient. The camera was positioned in front of the volunteers’ legs at an angle of 10°. To obtain a continuous thermographic follow-up during the test, photos were captured every five complete repetitions performed (ankle flexion–extension, full ROM). Once the total number of repetitions had been obtained, the images were subdivided into four quartiles, thus obtaining a baseline image (pre-protocol), one at 25% of maximum effort, another at 50% of maximum effort, another at 75% of maximum effort, and a final image at the end of the protocol (Figure 1). For example, if a volunteer performed 100 repetitions, since an image was recorded every 5 repetitions, the basal image, (T0) 0 repetitions; image 5 (T1), 25 repetitions; image 10 (T2), 50 repetitions; image 15 (T3), 75 repetitions; and image 20 (T4), 100 repetitions, were analyzed at the end of the protocol. In the case of patients who performed an odd number of repetitions, the image closest to the corresponding quartile was used. Image processing was performed in a blinded fashion by two investigators using Flir ResearchIR 4 software (Teledyne FLIR LLC, Wilsonville, OR, USA), as described by previous authors.
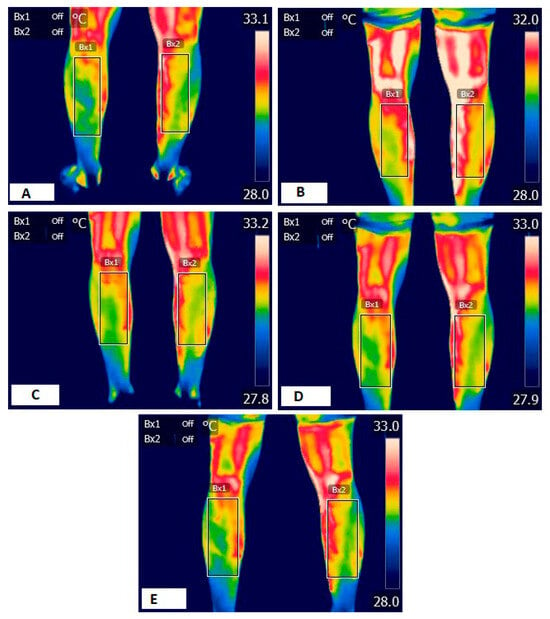
Figure 1.
Thermographic sequence. (A) Basal thermography, (B) thermography 25%, (C) thermography 50%, (D) thermography 75%, and (E) final thermography, BX1: left leg; BX2: right leg.
2.4. Maximum Fatigue Protocol
In the maximal gastrocnemius fatigue assessment, participants stood on a 25 cm elevated step with their knees extended, ensuring that the front part of their forefoot (head of the goal) contacted with the step. The midfoot and rearfoot were unencumbered to enhance maximum dorsiflexion and plantarflexion movement (ankle ROM). The patient was able to grip the stair rail with both hands to maintain balance, but not to lessen weight or move himself forward. Patients were required to maintain a constant speed of execution, (one second of the eccentric phase, dorsiflexion; and one second of the concentric phase, plantar flexion, was calculated using a digital stopwatch and verbally indicated by one of the researchers), performing the full range of motion of ankle dorsiflexion. If these requirements were not met, the test was terminated. A stress testing specialist observed that the range of motion and support were executed as described and assessed during the introductory session. The overall count of repetitions executed by each participant was recorded from the beginning of the test until the final possible repetition completed by the patients. The test was deemed complete when the volunteer was unable to execute further movements, the joint ranges were not adhered to, or the arms were utilized to aid the dorsiflexion phase. The area of the gastrocnemius was selected due to the extensive research previously completed in thermography linked to physical activity, along with the straightforwardness of conducting and evaluating both the physical and thermographic assessments. The participants completed the tests between 8:00 and 11:30 in the morning to minimize the effects of circadian rhythms on body temperature. Previous studies have demonstrated significant circadian rhythmicity in regards to skin temperature [23,24].
2.5. Statistical Analysis
IBM Social Sciences software (SPSS, v.21.0, Chicago, IL, USA) was used for statistical analysis. Data are presented as mean ± SD. The homogeneity and normality of the data were tested using the Levene and Shapiro–Wilk tests, respectively. To analyze intragroup and intergroup differences, a two-way repeated measures ANOVA was performed for Tsk, with a time factor (B vs. 25% vs. 50% vs. 75% vs. 100%) and a side factor (right (R) and left (L)), and sex, age, ethnicity, and dominant side as a factor between subjects, with BMI and number of total repetitions as covariates. A Tukey’s post hoc analysis was performed if significance was found in the ANOVA models. Partial eta squared (η2p) was also calculated as the effect size for the interaction of all variables in the ANOVA analysis. The following partial eta squared thresholds were used: <0.01, irrelevant; ≥0.01, small; ≥0.059, moderate; ≥0.138, large. The significance level was set at p ≤ 0.05.
3. Results
3.1. General Sample Description
Table 1 shows information about the general description of the sample. In comparison to the female participants (n = 50; 21.0 ± 2.47 years), the male participants (n = 48) were marginally older (22.7 ± 3.22 years). Additionally, the men’s body mass index (BMI) was higher (24.9 ± 4.02) than the women’s (22.7 ± 2.80).

Table 1.
Data for age, body mass, height, BMI, and calf temperature during exercise protocol until exhaustion; mean (standard deviation).
The men’s baseline skin temperature values (right and left calf) were consistently higher than the women’s (29.5 ± 1.19 °C, right; 29.4 ± 1.16 °C, left) (31.2 ± 1.05 °C, right; 31.1 ± 1.05 °C, left, respectively). Throughout the various protocol intensities (25%, 50%, 75%, and 100% of total effort), this sex-related difference of roughly 1.5–1.7 °C remained constant. Women displayed somewhat lower values of ~29.3–29.5 °C throughout all stages, whereas men maintained constant values of about 31.0–31.1 °C.
Since both men and women maintained relatively stable Tsk values from 25% to 100% of exhaustion, indicating minimal acute thermal changes despite increased workload, no significant intra-sex variations were observed when taking intensity progression into account.
Lastly, although both groups showed high variability, men completed more repetitions until exhaustion (83.8 ± 49.4) than did women (76.3 ± 64.0).
3.2. Temperature
After performing two-way repeated measures ANOVA, at the calf Tsk level, a significant difference was found in time (p = 0.039; η2p = 0.026) and side (p =≤ 0.001; η2p = 0.120), along with a trend in the interaction of time x side (p = 0.068; η2p = 0.022).
Post hoc Tukey analysis revealed that the right side (R) consistently exhibited slightly higher temperatures than did the left side (L) throughout the test. Post hoc analysis detected a significant difference in Tsk B between the R and L side (R, 30.3 ± 1.39 °C (IC 95% (30.1–30.6)); L, 30.2 ± 1.39 °C (IC 95% (30.0–30.5)); p = 0.016), in Tsk at 25% (R, 30.2 °C ± 1.27 °C (IC 95% (30.0–30.4)); L, 30.1 °C ± 1.27 °C (IC 95% (29.9–30.3)); p = 0.009), in Tsk at 50% (R, 30.2 °C ± 1.29 °C (IC 95% (30.0–30.5)); L, 30.1 °C ±1.29 °C (IC 95% (30.0–30.4)); p = 0.034), and in Tsk at 75% (R, 30.3 °C ± 1.33 °C (IC 95% (30.1–30.5)); L, 30.2 °C ± 1.33 °C (IC 95% (30.0–30.4)); p = 0.017) (Figure 2).
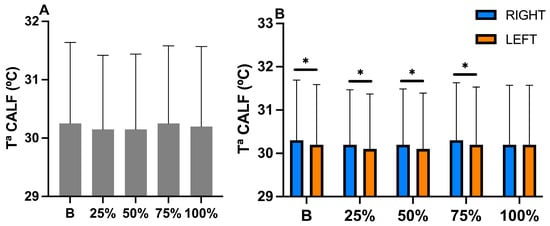
Figure 2.
(A) Changes in calf temperature considering only time data during exercise until exhaustion. (B) Changes in calf temperature considering the interaction of time x side during exercise until exhaustion. * = significant differences between right and left side ≤ p = 0.05. Ta = temperature.
The ANOVA model detected no significant difference in the interaction time x sex (p = 0.110; η2p = 0.020), side x sex (p = 0.095; η2p = 0.029), and time x side x sex (p = 0.641; η2p = 0.007) (Figure 3), indicating that sex did not influence the temporal or lateral thermoregulatory responses under the present testing conditions.
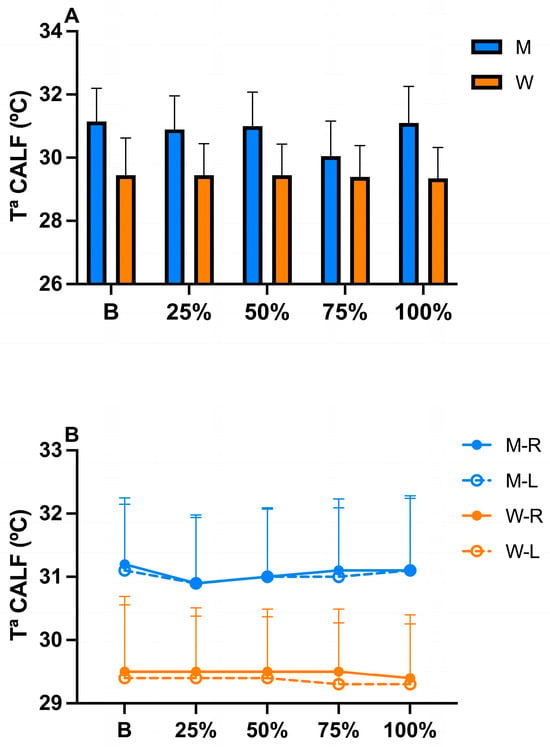
Figure 3.
(A) Changes in calf temperature considering the time x sex interaction during exercise until exhaustion. (B) Changes in calf temperature considering time x side x sex interaction during exercise until exhaustion. M = men; W = women; R = right; L = left; Ta = temperature.
4. Discussion
The aim of this study was to observe the variation in skin temperature during the execution of a maximal muscle fatigue protocol using concentric exercises on the triceps suralis. The results showed a significant difference in time (p = 0.039) and side (p =≤ 0.001). Tukey’s post hoc analysis detected a significant difference in Tsk B between the R and L side (R, 30.3 °C ± 1.39 °C; L, 30.2 °C ± 1.39 °C), in Tsk al 25% (R, 30.2 °C ± 1. 27 °C; L, 30.1 °C ± 1.27 °C), in Tsk al 50% (R, 30.2 °C ± 1.29 °C; L, 30.1 °C ± 1.29 °C), and in Tsk al 75% (R, 30.3 °C ± 1.33 °C; L, 30.2 °C ± 1.33 °C). The ANOVA model detected no significant differences in the interaction time × sex (p = 0.110), side × sex (p = 0.095), and time × side × sex (p = 0.641).
In relation to Tsk in basal conditions, despite showing significant differences between sides (p =≤ 0.001), it has been shown by other authors that only when such differences exceeded 0.6 °C between contralateral regions in the same anatomical region could they be considered as indicators of overload or pathological conditions, either superficial or deep [25,26]. Within this framework, our results are in agreement with those of previous studies in which, in healthy patients, in both other anatomical regions, as well as in twins, the temperature difference (ΔT) between extremities was never higher than 0.5 °C [8,27], representing a state of physiological normality of the tissues, ΔT ≤ 0.1 °C. Since these were healthy patients, factors that could influence these thermal asymmetries, such as inflammatory processes, vascular changes, or clinical situations, were therefore controlled and correctly ruled out.
Although descriptive analysis revealed minimal side-to-side differences (≤0.1 °C) in both sexes, the comparison between men and women showed a greater mean ΔT of approximately 0.7 °C (Figure 3B).
These findings confirm previous research in which it was observed that factors such as sex, age, training level, and BMI influence both the basal thermal response and the thermoregulatory response to fatigue [28,29,30]. As in our study, other authors showed that women tend to show different basal hypothermic patterns with respect to those of men [31] due to the concentration of muscle mass or fat tissue in certain areas, differences in the production of certain hormones, and distal vascular activity [32,33]. On the one hand, men exhibit a greater muscle mass, which generates more metabolic activity [31], and on the other, they carry less subcutaneous fat, which generates less thermal insulation, allowing greater heat transfer to the skin surface [34], and in addition, they display a lower tendency to peripheral vasoconstriction, which increases blood perfusion at distal structures [35]; thus, there is a certain consensus that men display higher skin temperatures than those of women, observable by IRT. Regarding the implication of body fat distribution, the higher percentage of fat in women and estrogen-mediated vasoconstrictive responses may limit heat transfer to the periphery [36]. In addition, gender differences have been observed in skin vascular conductance and autonomic control of thermoregulation during exercise and recovery [37], supporting the idea that thermographic patterns reflect underlying physiological differences between men and women.
The fact that men and women thermoregulate differently is of extreme importance in the clinical setting; in fact, for those physiotherapists who intend to design personalized thermal interventions and therapies on the basis of physical agents such as cold or heat, infrared thermography could be of great help to adjust treatment strategies and protocols according to individual thermal responses, improving, among others, the effects of the therapy. Future lines of research could explore the timing and delivery protocols of physical therapeutic agents aimed at increasing or decreasing muscle temperature as a function of gender.
In relation to Tsk throughout the protocol, a significant difference in time (p = 0.039) and side (p =≤ 0.001) of Tsk was described in this study. From a descriptive point of view, we can observe that, at 25% of the protocol, in men, a decrease in surface temperature of ΔT ≥ 0.2 °C is generated with respect to the basal temperature, while in women, the Tsk remains constant at ΔT ≥ 0.0 °C. These results could be evidence of a possible peripheral vasoconstriction that redirects blood flow toward more active muscles, as suggested by other authors [38,39,40], temporarily generating a reduction in vascular perfusion at the cutaneous level, which translates into a decrease in Tsk during exercise. However, unlike in the study by Ludwig et al. [38], in our study, it was only possible to observe this phenomenon in the male population, which leads us to believe that the thermoregulatory response in men does not follow the same dynamics as those in women. However, it should be noted that there are no known previous studies in which Tsk has been assessed during protocols according to sex, since most thermographic studies provide data from pre- and post-exertion. This opens a new window regarding the knowledge of the tissue metabolic response during exercise as a function of gender, of great interesting for personalizing program training sessions according to the physiological characteristics of each athlete.
At 50% of the protocol, in men, there was an increase in skin temperature that remained progressive and constant at 75% and until the end of the protocol, while in women the Tsk remained constant practically until the end of the protocol, where a decrease in temperature of 0.1 °C could be observed immediately after the end of the exercise. We know from other authors that, during exercise, due to the increase in muscle metabolism, an increase in heat release is generated and that part of this heat can be projected to the skin through the convection process, increasing the Tsk, which could explain the results obtained in this phase [41,42]. However, other authors showed that after intense sessions, a decrease in skin surface temperature has been observed due to the reduction in blood flow at the superficial level by migration to the deep level [5,43]. However, it should be noted that variations in Tsk depend mainly on the intensity, duration, and type of exercise, in combination with the characteristics of the anatomical region and the profile of the patient analyzed [44]. As in our work, some authors [45]) have observed increased Tsk in anaerobic training sessions, while others [46]) have observed hypothermic patterns after aerobic training; however, there are no known studies with a sample as large as ours in which this has been observed, analyzed, and described (using these parameters) throughout the protocol as a function of sex. Future studies could better clarify these novel findings found in our work.
Regarding the thermal variations found in our study pre-, during, and post-protocol, it should be noted that they are minimal compared to those observed in other works [41,42]. These differences could depend on the fact that the posterior region of the leg is a region too small to generate large thermoregulatory responses and that the type of exercise performed did not generate increased sweating or systemic response when compared to those noted in other studies in which larger anatomical regions that usually generated more robust metabolic changes were analyzed [47]. The small changes obtained in this study suggest that the exercise session did not promote acute injuries or important asymmetries, results consistent with an expected physiological response; in fact, the temperature differences between legs during and post-protocol were never higher than 0.2 °C. This study then presents some limitations, such as the anatomical region studied; a larger number of ROIs would have provided greater robustness to the results. However, it is worth mentioning that this study is the first work that analyzes the tissue metabolic response in such a large sample via IRT pre-, during, and post-exercise. In addition, since the sample size is substantial relative to those used in other research, our findings offer a clearer insight into the fundamental processes of skin temperature variations during physical activity.
Future research could expand the use of infrared thermography (IRT) by exploring other muscle groups and different types of exercise to better characterize thermal regulation patterns and their relationship to specific fatigue. IRT could also be evaluated as a non-invasive tool for monitoring the onset of fatigue and recovery in athletes, contributing to the individualization of training programs and injury prevention. Finally, combining IRT with other physiological measures, such as electromyography, blood lactate levels, or heart rate, would provide a more comprehensive view of muscle function and fatigue, improving the interpretation of thermographic changes and their practical relevance to athletic performance.
Limitations and Strengths
This study has several limitations. First, the analysis was limited to the leg’s posterior region; adding more regions of interest (ROI) would have strengthened the conclusions. Second, IRT does not directly measure deeper muscle activity, even though it is very sensitive to surface temperature changes. This could be addressed by combining other measurements, like electromyography or near-infrared spectroscopy.
Despite these limitations, the current work offers some notable strengths. It is among the first studies to analyze sex-specific responses in a sizable sample while continuously monitoring Tsk during a maximal fatigue protocol. Given that female populations are frequently underrepresented in exercise physiology and thermography research, the inclusion of both men and women is a significant contribution. This study offers new evidence to better understand thermoregulatory processes during exercise by analyzing bilateral differences and incorporating sex-specific analysis. This knowledge could have applications in sports performance, injury prevention, and customized rehabilitation strategies.
5. Conclusions
The results observed in this study evidence that infrared thermography is a valid tool for the measurement, analysis, and quantification of the tissue metabolic response of the muscular system before, during, and after exercise, showing the changes in skin temperature throughout the maximum muscle fatigue protocol. However, due to the study design, it was not possible to compare these thermal changes with serum values or biomarkers. Therefore, we believe that for future studies, it would be interesting to find relationships between Tsk variations and other performance and metabolic variables. However, it should be noted that this technology does not directly measure deep muscle activity.
Author Contributions
Conceptualization, A.C., A.Z. and F.J.M.-N.; methodology, A.C., A.Z. and F.J.M.-N.; software, A.C. and A.Z.; formal analysis, A.C. and F.J.M.-N.; investigation, A.C. and A.Z.; writing—original draft, A.C.; writing—review and editing, A.C., A.Z. and F.J.M.-N. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki and was approved by the Ethics Committee of the Universidad Católica de Murcia (approval number: CE032402; approval date: 21 March 2024).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The data presented in this study are available on request from the corresponding author due to privacy or ethical restrictions.
Acknowledgments
We would like to thank Roberto Mevi, a student at the Catholic University of San Antonio in Murcia, for his help in developing this project.
Conflicts of Interest
The authors declare no conflicts of interest.
Abbreviations
| ATM | Atmosphere |
| BMI | Body Mass Index |
| ΔT | Difference in Temperature |
| IRT | Infrared Thermography |
| ROI | Region of Interest |
| TSK | Skin Temperature |
| STARD | Standards for the Reporting of Diagnostic Accuracy Studies |
| TISEM | Thermographic Imaging in Sports and Exercise Medicine |
References
- Côrte, A.C.; Pedrinelli, A.; Marttos, A.; Souza, I.F.G.; Grava, J.; José Hernandez, A. Infrared thermography study as a complementary method of screening and prevention of muscle injuries: Pilot study. BMJ Open Sport Exerc. Med. 2019, 5, e000431. [Google Scholar] [CrossRef]
- Gladden, L.B. Muscle as a consumer of lactate. Med. Sci. Sports Exerc. 2000, 32, 764–771. [Google Scholar] [CrossRef]
- Foster, A.D.; Straight, C.R.; Woods, P.C.; Lee, C.; Kent, J.A.; Chipkin, S.R.; Debold, E.P.; Miller, M.S. Cellular and molecular contractile function in aged human skeletal muscle is altered by phosphate and acidosis and partially reversed with an ATP analog. Am. J. Physiol. Cell Physiol. 2025, 328, C1220–C1233. [Google Scholar] [CrossRef]
- Alburquerque Santana, P.V.; Alvarez, P.D.; Felipe da Costa Sena, A.; Serpa, T.K.; de Assis, M.G.; Pimenta, E.M.; Costa, H.A.; Sevilio de Oliveira Junior, M.N.; Torres Cabido, C.E.; Veneroso, C.E. Relationship between infrared thermography and muscle damage markers in physically active men after plyometric exercise. J. Therm. Biol. 2022, 104, 103187. [Google Scholar] [CrossRef] [PubMed]
- Martínez-Noguera, F.J.; Cabizosu, A.; Marín-Pagán, C.; Alcaraz, P.E. Body surface profile in ambient and hot temperatures during a rectangular test in race walker champions of the World Cup in Oman 2022. J. Therm. Biol. 2023, 114, 103548. [Google Scholar] [CrossRef]
- Priego Quesada, J.I.; Martinez, N.; Salvador-Palmer, R.; Psikuta, A.; Annaheim, S.; Rossi, R.; Corberan, J.; Cibrian, R.; Perez-Soriano, P. Effects of the cycling workload on core and local skin temperatures. Exp. Therm. Fluid Sci. 2016, 77, 91–99. [Google Scholar] [CrossRef]
- Cabizosu, A.; Carboni, N.; Martinez-Almagro Andreo, A.; Vegara-Meseguer, J.M.; Marziliano, N.; Gea Carrasco, G.; Casu, G. Theoretical basis for a new approach of studying Emery-Dreifuss muscular dystrophy by means of thermography. Med. Hypotheses 2018, 118, 103–106. [Google Scholar] [CrossRef]
- Cabizosu, A.; López-López, A.; Grotto, D.; Vegara-Meseguer, J.M. Relationship Between Infrared Thermography and Functional Parameters in the Lower Limbs of Hemiplegic Patients. Life 2025, 15, 542. [Google Scholar] [CrossRef] [PubMed]
- Verstockt, J.; Verspeek, S.; Thiessen, F.; Tjalma, W.A.; Brochez, L.; Steenackers, G. Skin Cancer Detection Using Infrared Thermography: Measurement Setup, Procedure and Equipment. Sensors 2022, 22, 3327. [Google Scholar] [CrossRef]
- Carrière, M.E.; de Haas, L.E.M.; Pijpe, A.; Meij-de Vries, A.; Gardien, K.L.M.; van Zuijlen, P.P.M.; Jaspers, M.E.H. Validity of thermography for measuring burn wound healing potential. Wound Repair Regen. 2020, 28, 347–354. [Google Scholar] [CrossRef] [PubMed]
- Dindorf, C.; Bartaguiz, E.; Janowicz, E.; Fröhlich, M.; Ludwig, O. Effects of Unilateral Muscle Fatigue on Thermographic Skin Surface Temperature of Back and Abdominal Muscles-A Pilot Study. Sports 2022, 10, 41. [Google Scholar] [CrossRef]
- Escamilla-Galindo, V.-L.; Luis Felipe, J.; Alonso-Callejo, A.; Van-der-Horst, R.; de la Torre-Combarros, A.; Minafra, P.; Fernández-Muñoz, D.; Fernández-Cuevas, I. Return-to-play criteria based on infrared thermography during anterior cruciate ligament rehabilitation in football players. Biol. Sport 2025, 42, 161–167. [Google Scholar] [CrossRef]
- De Andrade Fernandes, A.; dos Santos Amorim, P.R.; Brito, C.J.; Sillero-Quintana, M.; Bouzas Marins, J.C. Regional Skin Temperature Response to Moderate Aerobic Exercise Measured by Infrared Thermography. Asian J. Sports Med. 2016, 7, e29243. [Google Scholar] [CrossRef]
- Cabizosu, A.; Marín-Pagán, C.; Martínez-Serrano, A.; Alcaraz, P.E.; Martínez-Noguera, F.J. Myotendinous Thermoregulation in National Level Sprinters After a Unilateral Fatigue Acute Bout-A Descriptive Study. Sensors 2023, 23, 9330. [Google Scholar] [CrossRef]
- Priego Quesada, J.I.; Lucas-Cuevas, A.G.; Gil-Calvo, M.; Giménez, J.V.; Aparicio, I.; Cibrián Ortiz de Anda, R.M.; Salvador Palmer, R.; Llana-Belloch, S.; Pérez-Soriano, P. Effects of graduated compression stockings on skin temperature after running. J. Therm. Biol. 2015, 52, 130–136. [Google Scholar] [CrossRef]
- Fernández Cuevas, I.; Torres-Márquez, G.; Quintana, M.; Navandar, A. Thermographic assessment of skin response to strength training in young participants. J. Therm. Anal. Calorim. 2023, 148, 3407–3415. [Google Scholar] [CrossRef]
- Luo, Y.; Tong, Y.J.; Hu, Y.Y. Thermal Increasing Information for Foot Surface during Jogging. J. Biomim. Biomater. Biomed. Eng. 2015, 24, 70–76. [Google Scholar] [CrossRef]
- Robles Dorado, V. Variaciones termométricas en la planta del pie y piernas valorada en corredores antes y después de correr 30 km. Rev. Int. Cienc. Podol. Internet 2016, 10, 31–40. [Google Scholar] [CrossRef]
- Fink, N.; Bogomilsky, S.; Raz, A.; Hoffer, O.; Scheinowitz, M. Thermographic Changes following Short-Term High-Intensity Anaerobic Exercise. Life 2023, 13, 2175. [Google Scholar] [CrossRef]
- Cuschieri, S. The STROBE guidelines. Saudi J. Anaesth. 2019, 13 (Suppl. S1), S31–S34. [Google Scholar] [CrossRef]
- World Medical Association. World Medical Association Declaration of Helsinki: Ethical principles for medical research involving human subjects. JAMA 2013, 310, 2191–2194. [Google Scholar] [CrossRef]
- Bernard, V.; Staffa, E.; Mornstein, V.; Bourek, A. Infrared camera assessment of skin surface temperature—Effect of emissivity. Phys. Medica Eur. J. Med. Phys. 2013, 29, 583–591. [Google Scholar] [CrossRef]
- Yosipovitch, G.; Xiong, G.L.; Haus, E.; Sackett-Lundeen, L.; Ashkenazi, I.; Maibach, H.I. Time-Dependent Variations of the Skin Barrier Function in Humans: Transepidermal Water Loss, Stratum Corneum Hydration, Skin Surface pH, and Skin Temperature. J. Investig. Dermatol. 1998, 110, 20–23. [Google Scholar] [CrossRef]
- Cuesta, M.; Boudreau, P.; Cermakian, N.; Boivin, D.B. Skin Temperature Rhythms in Humans Respond to Changes in the Timing of Sleep and Light. J. Biol. Rhythms 2017, 32, 257–273. [Google Scholar] [CrossRef]
- Feldman, F.; Nickoloff, E.L. Normal thermographic standards for the cervical spine and upper extremities. Skelet. Radiol. 1984, 12, 235–249. [Google Scholar] [CrossRef]
- Son, S.; Yoo, B.R.; Zhang, H.Y. Reference Standards for Digital Infrared Thermography Measuring Surface Temperature of the Upper Limbs. Bioengineering 2023, 10, 671. [Google Scholar] [CrossRef]
- Zhang, H.Y.; Son, S.; Yoo, B.R.; Youk, T.-M. Reference Standard for Digital Infrared Thermography of the Surface Temperature of the Lower Limbs. Bioengineering 2023, 10, 283. [Google Scholar] [CrossRef]
- Reis, H.H.T.; Brito, C.J.; Sillero-Quintana, M.; da Silva, A.G.; Fernández-Cuevas, I.; Cerqueira, M.S.; Werneck, F.Z.; Marins, J.C.B. Can the body mass index influence the skin temperature of adolescents assessed by infrared thermography? J. Therm. Biol. 2023, 111, 103424. [Google Scholar] [CrossRef]
- Chudecka, M.; Lubkowska, A. Thermal maps of young women and men. Infrared Phys. Technol. 2015, 69, 81–87. [Google Scholar] [CrossRef]
- Lahiri, B.B.; Bagavathiappan, S.; Nishanthi, K.; Mohanalakshmi, K.; Veni, L.; Saumya; Yacin, S.M.; Philip, J. Infrared thermography based studies on the effect of age on localized cold stress induced thermoregulation in human. Infrared Phys. Technol. 2016, 76, 592–602. [Google Scholar] [CrossRef]
- Binek, M.; Drzazga, Z.; Teresa, S.; Pokora, I. (PDF) Do Exist Gender Differences in Skin Temperature of Lower Limbs Following Exercise Test in Male and Female Cross-Country Skiers? Available online: https://www.researchgate.net/publication/354682574_Do_exist_gender_differences_in_skin_temperature_of_lower_limbs_following_exercise_test_in_male_and_female_cross-country_skiers (accessed on 18 May 2023).
- Christensen, J.; Vaeth, M.; Wenzel, A. Thermographic imaging of facial skin—Gender differences and temperature changes over time in healthy subjects. Dentomaxillofacial Radiol. 2012, 41, 662–667. [Google Scholar] [CrossRef]
- Marins, J.C.B.; Formenti, D.; Costa, C.M.A.; de Andrade Fernandes, A.; Sillero-Quintana, M. Circadian and gender differences in skin temperature in militaries by thermography. Infrared Phys. Technol. 2015, 71, 322–328. [Google Scholar] [CrossRef]
- Canda, A. Study of differences in subcutaneous fat distribution based on ethnicity and sex in high-level competitive athletes. Anthropol. Anz. Ber. Uber Biol. Anthropol. Lit. 2025, 82, 147–159. [Google Scholar] [CrossRef]
- Cignarella, A.; Bolego, C.; Barton, M. Sex and sex steroids as determinants of cardiovascular risk. Steroids 2024, 206, 109423. [Google Scholar] [CrossRef]
- Gagnon, D.; Kenny, G.P. Sex differences in thermoeffector responses during exercise at fixed requirements for heat loss. J. Appl. Physiol. (1985) 2012, 113, 746–757. [Google Scholar] [CrossRef]
- Keatisuwan, W.; Ohnaka, T.; Tochihara, Y. Physiological responses of men and women during exercise in hot environments with equivalent WBGT. Appl. Hum. Sci. J. Physiol. Anthropol. 1996, 15, 249–258. [Google Scholar] [CrossRef]
- Ludwig, N.; Trecroci, A.; Gargano, M.; Formenti, D.; Bosio, A.; Rampinini, E.; Alberti, G. Thermography for skin temperature evaluation during dynamic exercise: A case study on an incremental maximal test in elite male cyclists. Appl. Opt. 2016, 55, D126–D130. [Google Scholar] [CrossRef]
- Drzazga, Z.; Binek, M.; Pokora, I.; Sadowska-Krępa, E. A preliminary study on infrared thermal imaging of cross-country skiers and swimmers subjected to endurance exercise. J. Therm. Anal. Calorim. 2018, 134, 701–710. [Google Scholar] [CrossRef]
- Akimov, E.B.; Son’kin, V.D. Skin temperature and lactate threshold during muscle work in athletes. Hum. Physiol. 2011, 37, 621–628. [Google Scholar] [CrossRef]
- Novotny, J.; Rybarova, S.; Zacha, D.; Bernacikova, M.; Ramadan, W.A. The influence of breast-stroke swimming on the muscle activity of young men in thermographic imaging. Acta Bioeng. Biomech. 2015, 17, 022015. [Google Scholar]
- Barboza, J.A.M.; de Almeida Ferreira, J.J.; Cerqueira, M.S.; Maciel, D.G.; de Barros, A.C.M.; Leite, E.C.; Matias, M.G.; Lemos, T.M.; Nonato, R.D.; de Brito Vieira, W.H. Can Skin Temperature Be Altered After Different Magnitudes of Eccentric Exercise-Induced Muscle Damage? Res. Q. Exerc. Sport 2022, 93, 702–709. [Google Scholar] [CrossRef]
- Tanda, G. Total body skin temperature of runners during treadmill exercise. J. Therm. Anal. Calorim. 2018, 131, 1967–1977. [Google Scholar] [CrossRef]
- Crenna, F.; Tanda, G. Design of an experiment for the biomechanical and thermal analysis of athletes during prolonged running exercise. J. Hum. Sport Exerc. 2021, 16, 773–794. [Google Scholar] [CrossRef]
- Cholewka, A.; Kasprzyk, T.; Stanek, A.; Sieroń-Stołtny, K.; Drzazga, Z. May thermal imaging be useful in cyclist endurance tests? J. Therm. Anal. Calorim. 2016, 123, 1973–1979. [Google Scholar] [CrossRef]
- da Silva, W.; Machado, Á.S.; Lemos, A.L.; de Andrade, C.F.; Priego-Quesada, J.I.; Carpes, F.P. Relationship between exercise-induced muscle soreness, pain thresholds, and skin temperature in men and women. J. Therm. Biol. 2021, 100, 103051. [Google Scholar] [CrossRef] [PubMed]
- Merla, A.; Mattei, P.A.; Di Donato, L.; Romani, G.L. Thermal imaging of cutaneous temperature modifications in runners during graded exercise. Ann. Biomed. Eng. 2010, 38, 158–163. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).