Characteristics and Clinical Assessment of Elbow Pain in Youth Baseball Players
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants
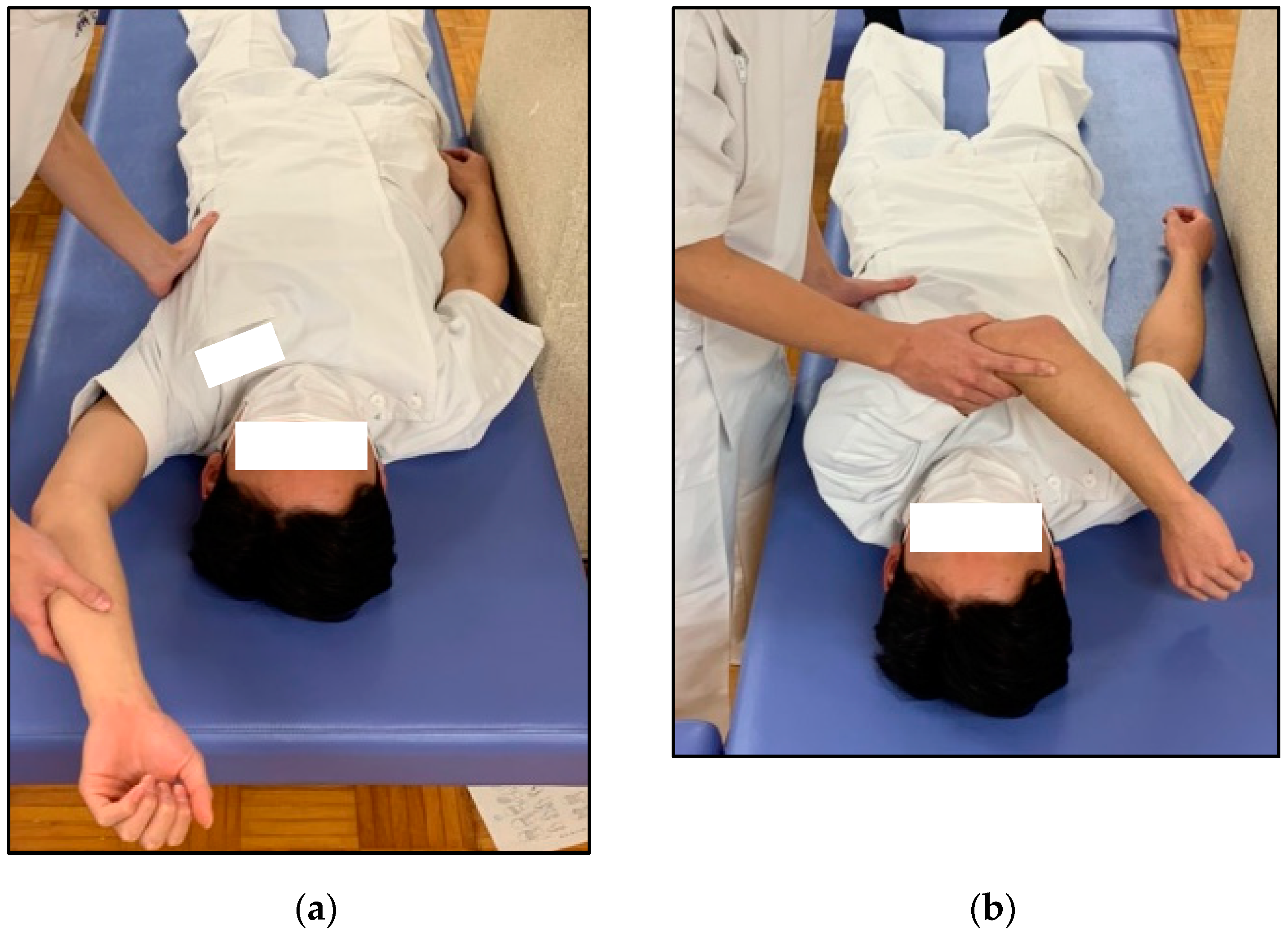
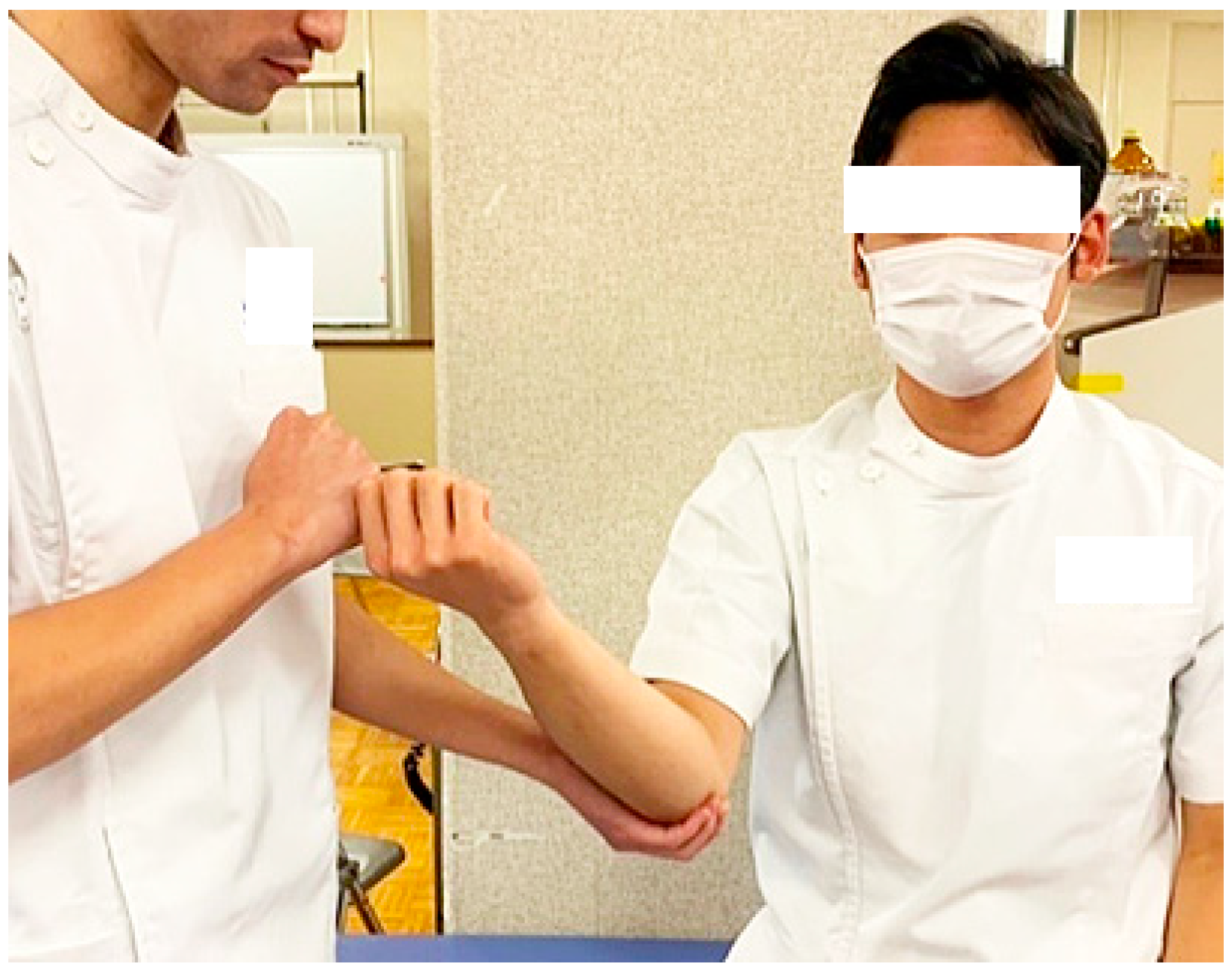
2.2. Physical Examination
2.3. Clinical Assessment
2.4. Ultrasonography
2.5. Statistical Analyses
2.6. Ethical Consideration
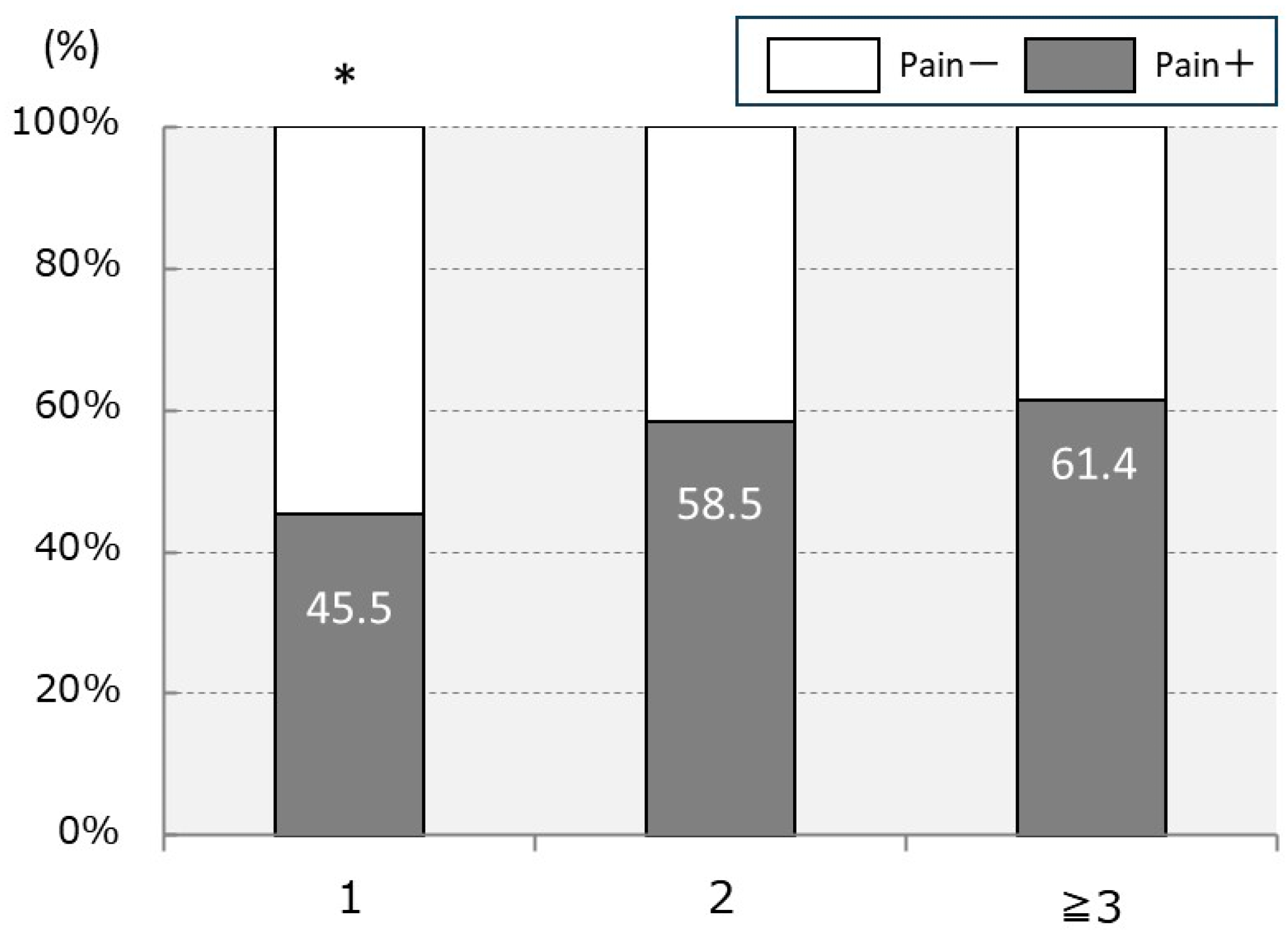
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
References
- Lawson, B.R.; Comstock, R.D.; Smith, G.A. Baseball-related injuries to children treated in hospital emergency departments in the United States, 1994–2006. Pediatrics 2009, 123, e1028–e1034. [Google Scholar] [CrossRef] [PubMed]
- E-Stat: Portal Site of Official Statistics of Japan. 2011 Survey on Time. Use and Leisure Activities. Available online: http://www.e-stat.go.jp/SG1/estat/ListE.do?bid=000001039118&cycode=0 (accessed on 29 February 2024).
- Matsuura, T.; Suzue, N.; Iwame, T.; Arisawa, K.; Fukuta, S.; Sairyo, K. Epidemiology of shoulder and elbow pain in youth baseball players. Phys. Sportsmed. 2016, 44, 97–100. [Google Scholar] [CrossRef] [PubMed]
- Shanley, E.; Rauh, M.J.; Michener, L.A.; Ellenbecker, T.S.; Garrison, J.C.; Thigpen, C.A. Shoulder range of motion measures as risk factors for shoulder and elbow injuries in high school softball and baseball players. Am. J. Sports Med. 2011, 39, 1997–2006. [Google Scholar] [CrossRef] [PubMed]
- Collins, C.L.; Comstock, R.D. Epidemiological features of high school baseball injuries in the United States, 2005–2007. Pediatrics 2008, 121, 1181–1187. [Google Scholar] [CrossRef] [PubMed]
- Valovich McLeod, T.C.; Decoster, L.C.; Loud, K.J.; Micheli, L.J.; Parker, J.T.; Sandrey, M.A.; White, C. National Athletic Trainers’ Association position statement: Prevention of pediatric overuse injuries. J. Athl. Train. 2011, 46, 206–220. [Google Scholar] [CrossRef] [PubMed]
- Gugenheim, J.J., Jr.; Stanley, R.F.; Woods, G.W.; Tullos, H.S. Little League survey: The Houston study. Am. J. Sports Med. 1976, 4, 189–200. [Google Scholar] [CrossRef] [PubMed]
- Larson, R.L.; Singer, K.M.; Bergstrom, R.; Thomas, S. Little League survey: The Eugene study. Am. J. Sports Med. 1976, 4, 201–209. [Google Scholar] [CrossRef] [PubMed]
- Adams, J.E. Injury to the throwing arm. A study of traumatic changes in the elbow joints of boy baseball players. Calif. Med. 1965, 102, 127–132. [Google Scholar] [PubMed]
- Lyman, S.; Fleisig, G.S.; Andrews, J.R.; Osinski, E.D. Effect of pitch type, pitch count, and pitching mechanics on risk of elbow and shoulder pain in youth baseball pitchers. Am. J. Sports Med. 2002, 30, 463–468. [Google Scholar] [CrossRef]
- Matsuura, T.; Suzue, N.; Kashiwaguchi, S.; Arisawa, K.; Yasui, N. Elbow injuries in youth baseball players without prior elbow pain: A 1-year prospective study. Orthop. J. Sports Med. 2013, 1, 2325967113509948. [Google Scholar] [CrossRef]
- Takagishi, K.; Matsuura, T.; Masatomi, T.; Chosa, E.; Tajika, T.; Watanabe, M.; Iwama, T.; Otani, T.; Inagaki, K.; Ikegami, H.; et al. Shoulder and elbow pain in elementary school baseball players: The results from a nation-wide survey in Japan. J. Orthop. Sci. 2017, 22, 682–686. [Google Scholar] [CrossRef] [PubMed]
- Sakata, J.; Nakamura, E.; Suzukawa, M.; Akaike, A.; Shimizu, K. Physical risk factors for a medial elbow injury in junior baseball players: A prospective cohort study of 353 players. Am. J. Sports Med. 2017, 45, 135–143. [Google Scholar] [CrossRef]
- Klingele, K.E.; Kocher, M.S. Little league elbow: Valgus overload injury in the paediatric athlete. Sports Med. 2002, 32, 1005–1015. [Google Scholar] [CrossRef] [PubMed]
- Shanley, E.; Thigpen, C. Throwing injuries in the adolescent athlete. Int. J. Sports Phys. Ther. 2013, 8, 630–640. [Google Scholar]
- Olsen, S.J.; Fleisig, G.S.; Dun, S.; Loftice, J.; Andrews, J.R. Risk factors for shoulder and elbow injuries in adolescent baseball pitchers. Am. J. Sports Med. 2006, 34, 905–912. [Google Scholar] [CrossRef] [PubMed]
- Endo, Y.; Sakamoto, M. Relationship between lower extremity tightness and star excursion balance test performance in junior high school baseball players. J. Phys. Ther. Sci. 2014, 26, 661–663. [Google Scholar] [CrossRef] [PubMed]
- Harada, M.; Takahara, M.; Mura, N.; Sasaki, J.; Ito, T.; Ogino, T. Risk factors for elbow injuries among young baseball players. J. Shoulder Elbow Surg. 2010, 19, 502–507. [Google Scholar] [CrossRef]
- Lyman, S.; Fleisig, G.S.; Waterbor, J.W.; Funkhouser, E.M.; Pulley, L.; Andrews, J.R.; Osinski, E.D.; Roseman, J.M. Longitudinal study of elbow and shoulder pain in youth baseball pitchers. Med. Sci. Sports Exerc. 2001, 33, 1803–1810. [Google Scholar] [CrossRef]
- Yang, J.; Mann, B.J.; Guettler, J.H.; Dugas, J.R.; Irrgang, J.J.; Fleisig, G.S.; Albright, J.P. Risk-prone pitching activities and injuries in youth baseball: Findings from a national sample. Am. J. Sports Med. 2014, 42, 1456–1463. [Google Scholar] [CrossRef]
- Fleisig, G.S.; Andrews, J.R. Prevention of elbow injuries in youth baseball pitchers. Sports Health 2012, 4, 419–424. [Google Scholar] [CrossRef]
- Matsuura, T.; Iwame, T.; Suzue, N.; Arisawa, K.; Sairyo, K. Risk factors for shoulder and elbow pain in youth baseball players. Phys. Sportsmed. 2017, 45, 140–144. [Google Scholar] [CrossRef] [PubMed]
- USA Baseball Medical and Safety Advisory Committee. Position Statement for Youth Baseball Pitchers; American Sports Medicine Institute: Birmingham, AL, USA, 2013. [Google Scholar]
- Shitara, H.; Kobayashi, T.; Yamamoto, A.; Shimoyama, D.; Ichinose, T.; Tajika, T.; Osawa, T.; Iizuka, H.; Takagishi, K. Prospective multifactorial analysis of preseason risk factors for shoulder and elbow injuries in high school baseball pitchers. Knee Surg. Sports Traumatol. Arthrosc. 2017, 25, 3303–3310. [Google Scholar] [CrossRef] [PubMed]
- Horii, M.; Kimura, S.; Akagi, R.; Watanabe, S.; Yamaguchi, S.; Ohtori, S.; Sasho, T. Referential values for lower limb flexibility in healthy children and adolescents in Japan: A five-year cross-sectional study. J. Orthop. Sci. 2024, 29, 891–896. [Google Scholar] [CrossRef] [PubMed]
- Perret, C.; Poiraudeau, S.; Fermanian, J.; Colau, M.M.L.; Benhamou, M.A.M.; Revel, M. Validity, reliability, and responsiveness of the fingertip-to-floor test. Arch. Phys. Med. Rehabil. 2001, 82, 1566–1570. [Google Scholar] [CrossRef] [PubMed]
- Saito, M.; Kenmoku, T.; Kameyama, K.; Murata, R.; Yusa, T.; Ochiai, N.; Kijima, T.; Takahira, N.; Fukushima, K.; Ishige, N.; et al. Relationship between tightness of the hip joint and elbow pain in adolescent baseball players. Orthop. J. Sports Med. 2014, 2, 2325967114532424. [Google Scholar] [CrossRef] [PubMed]
- Ichinose, T.; Shitara, H.; Tajika, T.; Kuboi, T.; Shimoyama, D.; Sasaki, T.; Hamano, N.; Kamiyama, M.; Yamamoto, A.; Kobayashi, T.; et al. Reciprocal inhibition improves posterior shoulder tightness and shoulder range of motion in youth baseball players. JSES Int. 2021, 5, 978–982. [Google Scholar] [CrossRef]
- Wilk, K.E.; Macrina, L.C.; Fleisig, G.S.; Aune, K.T.; Porterfield, R.A.; Harker, P.; Evans, T.J.; Andrews, J.R. Deficits in glenohumeral passive range of motion increase risk of elbow injury in professional baseball pitchers: A prospective study. Am. J. Sports Med. 2014, 42, 2075–2081. [Google Scholar] [CrossRef] [PubMed]
- Tennent, T.D.; Beach, W.R.; Meyers, J.F. A review of the special tests associated with shoulder examination: Part I: The rotator cuff tests. Am. J. Sports Med. 2003, 31, 154–160. [Google Scholar] [CrossRef] [PubMed]
- Kotoshiba, S.; Maeda, N.; Urabe, Y.; Sasadai, J.; Aramaki, K.; Sumida, R.; Yanase, K.; Hara, M. Effect of short-term intervention on infraspinatus muscle activity during throwing motion and physical examination in baseball players with throwing disorder. Isokinet. Exerc. Sci. 2020, 28, 91–99. [Google Scholar] [CrossRef]
- O’Driscoll, S.W.; Lawton, R.L.; Smith, A.M. The “moving valgus stress test” for medial collateral ligament tears of the elbow. Am. J. Sports Med. 2005, 33, 231–239. [Google Scholar] [CrossRef]
- Harada, M.; Takahara, M.; Sasaki, J.; Mura, N.; Ito, T.; Ogino, T. Using sonography for the early detection of elbow injuries among young baseball players. AJR Am. J. Roentgenol. 2006, 187, 1436–1441. [Google Scholar] [CrossRef] [PubMed]
- Wilk, K.E.; Macrina, L.C.; Fleisig, G.S.; Porterfield, R.; Simpson, C.D.; Harker, P.; Paparesta, N.; Andrews, J.R. Correlation of glenohumeral internal rotation deficit and total rotational motion to shoulder injuries in professional baseball pitchers. Am. J. Sports Med. 2011, 39, 329–335. [Google Scholar] [CrossRef] [PubMed]
- Frush, T.J.; Lindenfeld, T.N. Peri-epiphyseal and overuse injuries in adolescent athletes. Sports Health 2009, 1, 201–211. [Google Scholar] [CrossRef] [PubMed]
- Hang, D.W.; Chao, C.M.; Hang, Y.-S. A Clinical and roentgenographic study of little league elbow. Am. J. Sports Med. 2004, 32, 79–84. [Google Scholar] [CrossRef] [PubMed]
- Hattori, H.; Akasaka, K.; Otsudo, T.; Takei, K.; Yamamoto, M. The effects of elbow bracing on medial elbow joint space gapping associated with repetitive throwing in high school baseball players. Orthop. J. Sports Med. 2017, 5, 2325967117702361. [Google Scholar] [CrossRef] [PubMed]
- Greenberg, E.M.; Lawrence, J.T.R.; Fernandez-Fernandez, A.; Shah, K.; McKenna, C.; Rowan, M.L.; Kim, J.; McClure, P. Physical and functional differences in youth baseball players with and without throwing-related pain. Orthop. J. Sports Med. 2017, 5, 2325967117737731. [Google Scholar] [CrossRef] [PubMed]
- Davis, J.T.; Limpisvasti, O.; Fluhme, D.; Mohr, K.J.; Yocum, L.A.; ElAttrache, N.S.; Jobe, F.W. The effect of pitching biomechanics on the upper extremity in youth and adolescent baseball pitchers. Am. J. Sports Med. 2009, 37, 1484–1491. [Google Scholar] [CrossRef] [PubMed]
- Yachi, K.Y.T.; Murase, T.; Tada, K. Analysis of cause of low teenager’ baseball elbow. J. Jpn. Elbow Soc. 2001, 8, 117–118. (In Japanese) [Google Scholar]
- Cain, E.L., Jr.; Dugas, J.R.; Wolf, R.S.; Andrews, J.R. Elbow injuries in throwing athletes: A current concepts review. Am. J. Sports Med. 2003, 31, 621–635. [Google Scholar] [CrossRef]
- Matsel, K.A.; Butler, R.J.; Malone, T.R.; Hoch, M.C.; Westgate, P.M.; Uhl, T.L. Current concepts in arm care exercise programs and injury risk reduction in adolescent baseball players: A clinical review. Sports Health 2021, 13, 245–250. [Google Scholar] [CrossRef]
- Matsuura, T.; Suzue, N.; Iwame, T.; Nishio, S.; Sairyo, K. Prevalence of osteochondritis dissecans of the capitellum in young baseball players: Results based on ultrasonographic findings. Orthop. J. Sports Med. 2014, 2, 2325967114545298. [Google Scholar] [CrossRef] [PubMed]
- Jones, K.J.; Osbahr, D.C.; Schrumpf, M.A.; Dines, J.S.; Altchek, D.W. Ulnar collateral ligament reconstruction in throwing athletes: A review of current concepts. AAOS exhibit selection. J. Bone Jt. Surg. Am. 2012, 94, e49. [Google Scholar] [CrossRef] [PubMed]
| Mean ± SD | ||
|---|---|---|
| Age, years | 11.6 ± 1.4 | |
| Height, cm | 147.0 ± 11.0 | |
| Weight, kg | 39.7 ± 9.4 | |
| BMI, kg/m2 | 18.2 ± 2.4 | |
| Age at the start of baseball practice, years | 8.5 ± 1.4 | |
| Length of experience, years | 3.0 ± 1.5 | |
| Daily practice time, hours | 4.2 ± 1.8 | |
| Practice days per week, days | 4.2 ± 1.5 | |
| FFD, cm | 4.6 ± 3.3 | |
| N | ||
| Pitching side (right/left) | 190/26 | |
| Position † | Pitcher | 98 |
| Catcher | 50 | |
| Infielder | 148 | |
| Outfielder | 105 | |
| US (N = 213) | N (%) | |
| Lateral side | Normal | 207 (97.2%) |
| Mild | 2 (0.9%) | |
| Severe | 4 (1.9%) | |
| Medial side | Normal | 133 (62.4%) |
| Mild | 41 (19.2%) | |
| Severe | 39 (18.3%) | |
| Median (IQR) | Dominant | Non-Dominant | p-Value | |
|---|---|---|---|---|
| SLR, deg | 60.0 (60.0–70.0) | 60.0 (60.0–70.0) | 0.742 | |
| HBD, cm | 5.0 (0–9.0) | 6.0 (0–9.8) | 0.667 | |
| Shoulder | Second IR, deg | 45.0 (35.0–60.0) * | 60.0 (50.0–70.0) | <0.001 |
| Second ER, deg | 117.5 (110.0–130.0) * | 110.0 (100.0–130.0) | <0.001 | |
| Third IR, deg | 30.0 (20.0–40.0) * | 35.0 (30.0–45.0) | <0.001 | |
| Elbow | Flex, deg | 145.0 (140.0–150.0) * | 145.0 (140.0–150.0) | <0.001 |
| Ext, deg | 0 (0–5.0) * | 5.0 (0–5.0) | <0.001 | |
| Hip | IR, deg | 40.0 (30.0–45.0) | 40.0 (31.3–50.0) | 0.089 |
| ER, deg | 45.0 (45.0–60.0) | 50.0 (45.0–60.0) | 0.949 | |
| CAT +/− | N (%) | 87/160 (54.4) * | 34/160 (21.3) | <0.01 |
| HFT +/− | N (%) | 62/160 (38.8) * | 20/160 (12.5) | <0.01 |
| MVST +/− | N (%) | 36/215 (16.7) * | 2/212 (0.9) | <0.01 |
| Median (IQR) | Pain-Free Group | Elbow Pain Group | p-Value | |
|---|---|---|---|---|
| Age, years | 11.0 (10.0–12.0) * | 12.0 (11.0–13.0) | <0.01 | |
| Height, cm | 143.0 (136.0–151.3) * | 148.0 (142.0–157.0) | <0.01 | |
| Weight, kg | 36.0 (31.3–41.0) * | 40.0 (34.0–49.5) | <0.01 | |
| BMI, kg/m2 | 17.4 (16.0–19.2) | 18.1 (16.7–19.8) | 0.069 | |
| Age at the start of baseball practice, years | 8.0 (7.0–9.0) | 8.0 (8.0–9.0) | 0.733 | |
| Length of experience, years | 2.0 (1.0–4.0)* | 3.0 (2.0–4.0) | <0.01 | |
| Daily practice time, hours | 3.9 (3.0–4.7) | 3.7 (2.9–4.7) | 0.469 | |
| Practice days per week, days | 4.0 (3.0–5.0) | 4.0 (3.0–5.0) | 0.827 | |
| FFD, cm | 3.3 (2.3–4.6) | 4.3 (1.9–7.8) | 0.494 | |
| SLR (dominant), deg | 60 (60–70) | 60 (60–70) | 0.695 | |
| HBD (dominant), cm | 6.5 (2.5–10.0) * | 4.0 (0.0–8.0) | 0.038 | |
| Shoulder (dominant) | Second IR, deg | 50 (40–60) | 45 (30–51) | 0.076 |
| Second ER, deg | 120 (110–138) | 115 (109–130) | 0.670 | |
| Third IR, deg | 30 (20–40) | 30 (20–40) | 0.406 | |
| Elbow (dominant) | Flex, deg | 145 (140–150) | 145 (140–148) | 0.235 |
| Ext, deg | 5 (0–5) | 0 (0–5) | 0.231 | |
| Hip (dominant) | IR, deg | 40 (35–50) | 40 (30–45) | 0.179 |
| ER, deg | 50 (45–57.5) | 45 (45–60) | 0.380 | |
| CAT +/− | N (%) | 38/75 (50.7) | 49/85 (57.6) | 0.376 |
| HFT +/− | N (%) | 22/75 (29.3) * | 40/85 (47.1) | <0.05 |
| MVST +/− | N (%) | 7/98 (7.1) * | 29/117 (24.8) | <0.01 |
| Pain-Free Group | Elbow Pain Group | p-Value | ||
|---|---|---|---|---|
| Lateral side N (%) (N = 213) | Normal | 97 (99.0%) | 110 (95.7%) | 0.290 |
| Mild | 0 (0.0%) | 2 (1.7%) | ||
| Severe | 1 (1.0%) | 3 (2.6%) | ||
| Medial side N (%) (N = 213) | Normal | 70 (71.4%) | 63 (54.8%) | 0.022 * |
| Mild | 17 (17.3%) | 24 (20.9%) | ||
| Severe | 11 (11.2%) | 28 (24.3%) |
| Coefficient | p-Value | Odds Ratio | 95% CI | Deviance | |
|---|---|---|---|---|---|
| Age | −0.134 | 0.619 | 0.875 | 0.517–1.482 | 0.247 |
| Height | 0.045 | 0.222 | 1.046 | 0.973–1.123 | 1.494 |
| Weight | −0.003 | 0.933 | 0.997 | 0.933–1.066 | 0.007 * |
| Length of experience | 0.110 | 0.448 | 1.116 | 0.841–1.481 | 0.576 |
| HFT | 0.664 | 0.076 | 1.943 | 0.933–4.046 | 3.154 |
| MVST | 1.373 | 0.025 | 3.948 | 1.192–13.079 | 5.049 |
| Constant | −5.566 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Koseki, H.; Kajiyama, S.; Shida, T.; Tomonaga, I.; Nishiyama, Y.; Yoshida, D.; Mizukami, S.; Yamaguchi, K.; Imai, C. Characteristics and Clinical Assessment of Elbow Pain in Youth Baseball Players. Sports 2024, 12, 161. https://doi.org/10.3390/sports12060161
Koseki H, Kajiyama S, Shida T, Tomonaga I, Nishiyama Y, Yoshida D, Mizukami S, Yamaguchi K, Imai C. Characteristics and Clinical Assessment of Elbow Pain in Youth Baseball Players. Sports. 2024; 12(6):161. https://doi.org/10.3390/sports12060161
Chicago/Turabian StyleKoseki, Hironobu, Shiro Kajiyama, Takayuki Shida, Iku Tomonaga, Yuta Nishiyama, Daisuke Yoshida, Satoshi Mizukami, Kazuhiro Yamaguchi, and Chieko Imai. 2024. "Characteristics and Clinical Assessment of Elbow Pain in Youth Baseball Players" Sports 12, no. 6: 161. https://doi.org/10.3390/sports12060161
APA StyleKoseki, H., Kajiyama, S., Shida, T., Tomonaga, I., Nishiyama, Y., Yoshida, D., Mizukami, S., Yamaguchi, K., & Imai, C. (2024). Characteristics and Clinical Assessment of Elbow Pain in Youth Baseball Players. Sports, 12(6), 161. https://doi.org/10.3390/sports12060161






