Acute Oxygen Consumption Response to Fast Start High-Intensity Intermittent Exercise
Abstract
1. Introduction
2. Materials and Methods
2.1. Visit 1
2.2. Visit 2
Calculating Critical Power (CP) and W Prime (W’)
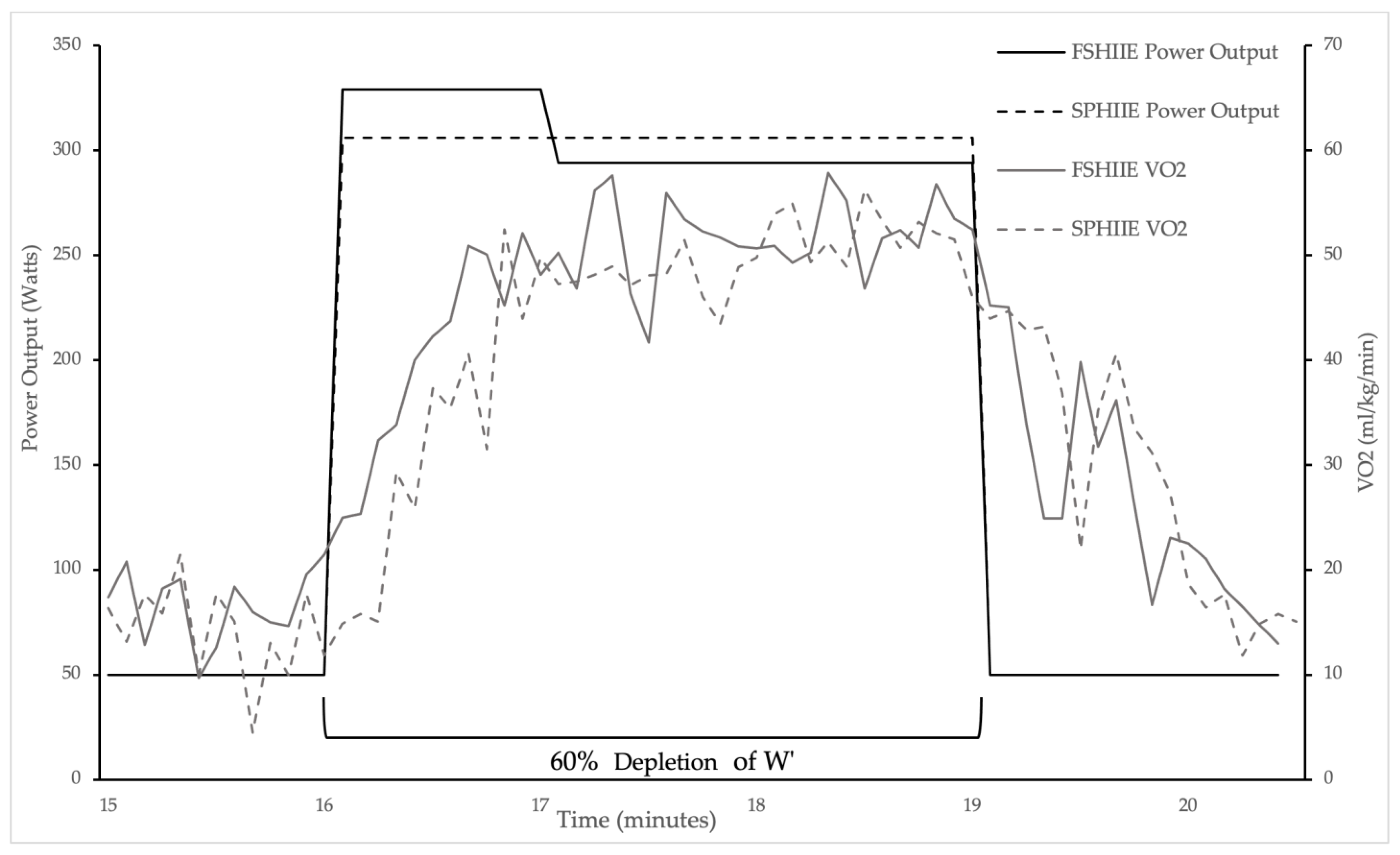
2.3. Visits 3 and 4
2.4. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Atakan, M.M.; Li, Y.; Koşar, Ş.N.; Turnagöl, H.H.; Yan, X. Evidence-Based Effects of High-Intensity Interval Training on Exercise Capacity and Health: A Review with Historical Perspective. Int. J. Environ. Res. Public Health 2021, 18, 7201. [Google Scholar] [CrossRef]
- Buchheit, M.; Laursen, P.B. High-Intensity Interval Training, Solutions to the Programming Puzzle: Part I: Cardiopulmonary Emphasis. Sports Med. 2013, 43, 313–338. [Google Scholar] [CrossRef] [PubMed]
- Lundby, C.; Jacobs, R.A. Adaptations of Skeletal Muscle Mitochondria to Exercise Training. Exp. Physiol. 2016, 101, 17–22. [Google Scholar] [CrossRef] [PubMed]
- MacInnis, M.J.; Gibala, M.J. Physiological Adaptations to Interval Training and the Role of Exercise Intensity. J. Physiol. 2017, 595, 2915–2930. [Google Scholar] [CrossRef] [PubMed]
- Huang, G.; Wang, R.; Chen, P.; Huang, S.C.; Donnelly, J.E.; Mehlferber, J.P. Dose–Response Relationship of Cardiorespiratory Fitness Adaptation to Controlled Endurance Training in Sedentary Older Adults. Eur. J. Prev. Cardiol. 2016, 23, 518–529. [Google Scholar] [CrossRef] [PubMed]
- Hawley, J.A.; Hargreaves, M.; Joyner, M.J.; Zierath, J.R. Integrative Biology of Exercise. Cell 2014, 159, 738–749. [Google Scholar] [CrossRef] [PubMed]
- Ma, X.; Cao, Z.; Zhu, Z.; Chen, X.; Wen, D.; Cao, Z. VO2max (VO2peak) in Elite Athletes under High-Intensity Interval Training: A Meta-Analysis. Heliyon 2023, 9, e16663. [Google Scholar] [CrossRef]
- Saltin, B.; Calbet, J.A.L. Point: In Health and in a Normoxic Environment, VO2max Is Limited Primarily by Cardiac Output and Locomotor Muscle Blood Flow. J. Appl. Physiol. 2006, 100, 744–748. [Google Scholar] [CrossRef]
- Hellsten, Y.; Nyberg, M. Cardiovascular Adaptations to Exercise Training. In Comprehensive Physiology; Prakash, Y.S., Ed.; Wiley: Hoboken, NJ, USA, 2015; pp. 1–32. ISBN 978-0-470-65071-4. [Google Scholar]
- Buchheit, M.; Laursen, P.B. High-Intensity Interval Training, Solutions to the Programming Puzzle: Part II: Anaerobic Energy, Neuromuscular Load and Practical Applications. Sports Med. 2013, 43, 927–954. [Google Scholar] [CrossRef]
- Jamnick, N.A.; Pettitt, R.W.; Granata, C.; Pyne, D.B.; Bishop, D.J. An Examination and Critique of Current Methods to Determine Exercise Intensity. Sports Med. 2020, 50, 1729–1756. [Google Scholar] [CrossRef]
- Gildea, N.; McDermott, A.; Rocha, J.; Crognale, D.; Nevin, A.; O’Shea, D.; Green, S.; Egaña, M. Low-Volume HIIT and MICT Speed VO2 Kinetics during High-Intensity “Work-to-Work” Cycling with a Similar Time-Course in Type 2 Diabetes. J. Appl. Physiol. 2022, 133, 273–287. [Google Scholar] [CrossRef] [PubMed]
- Jones, A.M.; Vanhatalo, A. The ‘Critical Power’ Concept: Applications to Sports Performance with a Focus on Intermittent High-Intensity Exercise. Sports Med. 2017, 47, 65–78. [Google Scholar] [CrossRef] [PubMed]
- Bailey, S.J.; Vanhatalo, A.; Dimenna, F.J.; Wilkerson, D.P.; Jones, A.M. Fast-Start Strategy Improves VO2 Kinetics and High-Intensity Exercise Performance. Med. Sci. Sports Exerc. 2011, 43, 457–467. [Google Scholar] [CrossRef] [PubMed]
- Burnley, M.; Doust, J.H.; Vanhatalo, A. A 3-Min All-Out Test to Determine Peak Oxygen Uptake and the Maximal Steady State. Med. Sci. Sports Exerc. 2006, 38, 1995–2003. [Google Scholar] [CrossRef] [PubMed]
- Brickley, G.; Doust, J.; Williams, C. Physiological Responses during Exercise to Exhaustion at Critical Power. Eur. J. Appl. Physiol. 2002, 88, 146–151. [Google Scholar] [CrossRef] [PubMed]
- Coats, E.M.; Rossiter, H.B.; Day, J.R.; Miura, A.; Fukuba, Y.; Whipp, B.J. Intensity-Dependent Tolerance to Exercise after Attaining VO2max in Humans. J. Appl. Physiol. 2003, 95, 483–490. [Google Scholar] [CrossRef] [PubMed]
- Moritani, T.; Nagata, A.; Devries, H.A.; Muro, M. Critical Power as a Measure of Physical Work Capacity and Anaerobic Threshold. Ergonomics 1981, 24, 339–350. [Google Scholar] [CrossRef]
- Rønnestad, B.R.; Bakken, T.A.; Thyli, V.; Hansen, J.; Ellefsen, S.; Hammarstrøm, D. Increasing Oxygen Uptake in Cross-Country Skiers by Speed Variation in Work Intervals. Int. J. Sports Physiol. Perform. 2022, 17, 384–390. [Google Scholar] [CrossRef]
- Warburton, D.E.R.; Gledhill, N.; Jamnik, V.K.; Bredin, S.S.D.; McKenzie, D.C.; Stone, J.; Charlesworth, S.; Shephard, R.J. Evidence-Based Risk Assessment and Recommendations for Physical Activity Clearance: Consensus Document 2011. Appl. Physiol. Nutr. Metab. 2011, 36, S266–S298. [Google Scholar] [CrossRef]
- Zadow, E.; Gordon, N.; Abbiss, C.; Peiffer, J. Pacing, the Missing Piece of the Puzzle to High-Intensity Interval Training. Int. J. Sports Med. 2014, 36, 215–219. [Google Scholar] [CrossRef][Green Version]
- Lisbôa, F.D.; Salvador, A.F.; Raimundo, J.A.G.; Pereira, K.L.; De Aguiar, R.A.; Caputo, F. Decreasing Power Output Increases Aerobic Contribution during Low-Volume Severe-Intensity Intermittent Exercise. J. Strength Cond. Res. 2015, 29, 2434–2440. [Google Scholar] [CrossRef] [PubMed]
- De Aguiar, R.A.; Turnes, T.; De Oliveira Cruz, R.S.; Caputo, F. Fast-Start Strategy Increases the Time Spent above 95% VO2max during Severe-Intensity Intermittent Running Exercise. Eur. J. Appl. Physiol. 2013, 113, 941–949. [Google Scholar] [CrossRef] [PubMed]
- Lisbôa, F.D.; Raimundo, J.A.G.; Salvador, A.F.; Pereira, K.L.; Turnes, T.; Diefenthaeler, F.; de Oliveira, M.F.M.; Caputo, F. Acute Cardiopulmonary, Metabolic, and Neuromuscular Responses to Severe-Intensity Intermittent Exercises. J. Strength Cond. Res. 2019, 33, 408–416. [Google Scholar] [CrossRef] [PubMed]
- Rønnestad, B.R.; Rømer, T.; Hansen, J. Increasing Oxygen Uptake in Well-Trained Cross-Country Skiers During Work Intervals with a Fast Start. Int. J. Sports Physiol. Perform. 2020, 15, 383–389. [Google Scholar] [CrossRef] [PubMed]
- Kirkeberg, J.M.; Dalleck, L.C.; Kamphoff, C.S.; Pettitt, R.W. Validity of 3 Protocols for Verifying VO2max. Int. J. Sports Med. 2011, 32, 266–270. [Google Scholar] [CrossRef] [PubMed]
- Jamnick, N.A.; By, S.; Pettitt, C.D.; Pettitt, R.W. Comparison of the YMCA and a Custom Submaximal Exercise Test for Determining VO2max. Med. Sci. Sports Exerc. 2016, 48, 254–259. [Google Scholar] [CrossRef] [PubMed]
- Beaver, W.L.; Wasserman, K.; Whipp, B.J. A New Method for Detecting Anaerobic Threshold by Gas Exchange. J. Appl. Physiol. 1986, 60, 2020–2027. [Google Scholar] [CrossRef] [PubMed]
- Hill, D.W.; Poole, D.C.; Smith, J.C. The Relationship between Power and the Time to Achieve VO2max. Med. Sci. Sports Exerc. 2002, 34, 709–714. [Google Scholar] [CrossRef]
- Jones, A.M.; Berger, N.J.A.; Wilkerson, D.P.; Roberts, C.L. Effects of “Priming” Exercise on Pulmonary O2 Uptake and Muscle Deoxygenation Kinetics during Heavy-Intensity Cycle Exercise in the Supine and Upright Positions. J. Appl. Physiol. 2006, 101, 1432–1441. [Google Scholar] [CrossRef]
- Rossiter, H.B.; Kowalchuk, J.M.; Whipp, B.J. A Test to Establish Maximum O2 Uptake despite No Plateau in the O2 Uptake Response to Ramp Incremental Exercise. J. Appl. Physiol. 2006, 100, 764–770. [Google Scholar] [CrossRef]
- Whipp, B.J.; Davis, J.A.; Torres, F.; Wasserman, K. A Test to Determine Parameters of Aerobic Function during Exercise. J. Appl. Physiol. 1981, 50, 217–221. [Google Scholar] [CrossRef] [PubMed]
- Beltz, N.M.; Gibson, A.L.; Janot, J.M.; Kravitz, L.; Mermier, C.M.; Dalleck, L.C. Graded Exercise Testing Protocols for the Determination of VO2max: Historical Perspectives, Progress, and Future Considerations. J. Sports Med. 2016, 2016, 3968393. [Google Scholar] [CrossRef] [PubMed]
- Foster, C.; Kuffel, E.; Bradley, N.; Battista, R.A.; Wright, G.; Porcari, J.P.; Lucia, A.; de Koning, J.J. VO2max during Successive Maximal Efforts. Eur. J. Appl. Physiol. 2007, 102, 67–72. [Google Scholar] [CrossRef] [PubMed]
- Midgley, A.W.; McNaughton, L.R.; Carroll, S. Verification Phase as a Useful Tool in the Determination of the Maximal Oxygen Uptake of Distance Runners. Appl. Physiol. Nutr. Metab. 2006, 31, 541–548. [Google Scholar] [CrossRef] [PubMed]
- Bergstrom, H.C.; Housh, T.J.; Zuniga, J.M.; Traylor, D.A.; Lewis, R.W.; Camic, C.L.; Schmidt, R.J.; Johnson, G.O. Differences among Estimates of Critical Power and Anaerobic Work Capacity Derived from Five Mathematical Models and the Three-Minute All-Out Test. J. Strength Cond. Res. 2014, 28, 592–600. [Google Scholar] [CrossRef]
- Hill, D.W.; Smith, J.C. Determination of Critical Power by Pulmonary Gas Exchange. Can. J. Appl. Physiol. 1999, 24, 74–86. [Google Scholar] [CrossRef]
- Pettitt, R.W. Using Scatterplots to Teach the Critical Power Concept. Adv. Physiol. Educ. 2012, 36, 172–175. [Google Scholar] [CrossRef][Green Version]
- Dicks, N.D.; Jamnick, N.A.; Murray, S.R.; Pettitt, R.W. Load Determination for the 3-Minute All-Out Exercise Test for Cycle Ergometry. Int. J. Sports Physiol. Perform. 2016, 11, 197–203. [Google Scholar] [CrossRef]
- Black, M.I.; Durant, J.; Jones, A.M.; Vanhatalo, A. Critical Power Derived from a 3-Min All-out Test Predicts 16.1-Km Road Time-Trial Performance. Eur. J. Sport Sci. 2014, 14, 217–223. [Google Scholar] [CrossRef]
- Clark, I.E.; West, B.M.; Reynolds, S.K.; Murray, S.R.; Pettitt, R.W. Applying the Critical Velocity Model for an Off-Season Interval Training Program. J. Strength Cond. Res. 2013, 27, 3335–3341. [Google Scholar] [CrossRef]
- Vanhatalo, A.; Doust, J.H.; Burnley, M. Determination of Critical Power Using a 3-Min All-out Cycling Test. Med. Sci. Sports Exerc. 2007, 39, 548–555. [Google Scholar] [CrossRef] [PubMed]
- Poole, D.C.; Burnley, M.; Vanhatalo, A.; Rossiter, H.B.; Jones, A.M. Critical Power: An Important Fatigue Threshold in Exercise Physiology. Med. Sci. Sports Exerc. 2016, 48, 2320–2334. [Google Scholar] [CrossRef] [PubMed]
- Chidnok, W.; DiMenna, F.J.; Fulford, J.; Bailey, S.J.; Skiba, P.F.; Vanhatalo, A.; Jones, A.M. Muscle Metabolic Responses during High-Intensity Intermittent Exercise Measured by 31 P-MRS: Relationship to the Critical Power Concept. Am. J. Physiol.-Regul. Integr. Comp. Physiol. 2013, 305, R1085–R1092. [Google Scholar] [CrossRef] [PubMed]
- Murgatroyd, S.R.; Ferguson, C.; Ward, S.A.; Whipp, B.J.; Rossiter, H.B. Pulmonary O2 Uptake Kinetics as a Determinant of High-Intensity Exercise Tolerance in Humans. J. Appl. Physiol. 2011, 110, 1598–1606. [Google Scholar] [CrossRef] [PubMed]
- Laursen, P.B.; Jenkins, D.G. The Scientific Basis for High-Intensity Interval Training: Optimising Training Programmes and Maximising Performance in Highly Trained Endurance Athletes. Sports Med. 2002, 32, 53–73. [Google Scholar] [CrossRef]
- Billat, V.; Slawinksi, J.; Bocquet, V.; Chassaing, P.; Demarle, A.; Koralsztein, J. Very Short (15 s–15 s) Interval-Training Around the Critical Velocity Allows Middle-Aged Runners to Maintain VO2max for 14 Minutes. Int. J. Sports Med. 2001, 22, 201–208. [Google Scholar] [CrossRef] [PubMed]
- Chorley, A.; Lamb, K.L. Effect of Varying Recovery Intensities on Power Outputs during Severe Intensity Intervals in Trained Cyclists during the Covid-19 Pandemic. Sport Sci. Health 2023, 19, 1199–1207. [Google Scholar] [CrossRef] [PubMed]
- Caen, K.; Bourgois, J.G.; Bourgois, G.; Van Der Stede, T.; Vermeire, K.; Boone, J. The Reconstitution of W′ Depends on Both Work and Recovery Characteristics. Med. Sci. Sports Exerc. 2019, 51, 1745–1751. [Google Scholar] [CrossRef]
- Ferguson, C.; Rossiter, H.B.; Whipp, B.J.; Cathcart, A.J.; Murgatroyd, S.R.; Ward, S.A. Effect of Recovery Duration from Prior Exhaustive Exercise on the Parameters of the Power-Duration Relationship. J. Appl. Physiol. 2010, 108, 866–874. [Google Scholar] [CrossRef]
- Skiba, P.F.; Chidnok, W.; Vanhatalo, A.; Jones, A.M. Modeling the Expenditure and Reconstitution of Work Capacity above Critical Power. Med. Sci. Sports Exerc. 2012, 44, 1526–1532. [Google Scholar] [CrossRef]
- Skiba, P.F.; Jackman, S.; Clarke, D.; Vanhatalo, A.; Jones, A.M. Effect of Work and Recovery Durations on W′ Reconstitution during Intermittent Exercise. Med. Sci. Sports Exerc. 2014, 46, 1433–1440. [Google Scholar] [CrossRef]
- Williams, N. The Borg Rating of Perceived Exertion (RPE) Scale. Occup. Med. 2017, 67, 404–405. [Google Scholar] [CrossRef]
- Pauw, K.D.; Roelands, B.; Cheung, S.S.; De Geus, B.; Rietjens, G.; Meeusen, R. Guidelines to Classify Subject Groups in Sport-Science Research. Int. J. Sports Physiol. Perform. 2013, 8, 111–122. [Google Scholar] [CrossRef] [PubMed]
- Meyler, S.; Bottoms, L.; Wellsted, D.; Muniz-Pumares, D. Variability in Exercise Tolerance and Physiological Responses to Exercise Prescribed Relative to Physiological Thresholds and to Maximum Oxygen Uptake. Exp. Physiol. 2023, 108, 581–594. [Google Scholar] [CrossRef] [PubMed]
- Nixon, R.J.; Kranen, S.H.; Vanhatalo, A.; Jones, A.M. Steady-State VO2 above MLSS: Evidence That Critical Speed Better Represents Maximal Metabolic Steady State in Well-Trained Runners. Eur. J. Appl. Physiol. 2021, 121, 3133–3144. [Google Scholar] [CrossRef] [PubMed]
- Jones, A.M.; Burnley, M.; Black, M.I.; Poole, D.C.; Vanhatalo, A. The Maximal Metabolic Steady State: Redefining the ‘Gold Standard’. Physiol. Rep. 2019, 7, e14098. [Google Scholar] [CrossRef] [PubMed]
- Collins, J.; Leach, O.; Dorff, A.; Linde, J.; Kofoed, J.; Sherman, M.; Proffit, M.; Gifford, J.R. Critical Power and Work-Prime Account for Variability in Endurance Training Adaptations Not Captured by VO2max. J. Appl. Physiol. 2022, 133, 986–1000. [Google Scholar] [CrossRef]
- Jones, A.M.; Grassi, B.; Christensen, P.M.; Krustrup, P.; Bangsbo, J.; Poole, D.C. Slow Component of VO2 Kinetics: Mechanistic Bases and Practical Applications. Med. Sci. Sports Exerc. 2011, 43, 2046–2062. [Google Scholar] [CrossRef]
- Koppo, K.; Bouckaert, J.; Jones, A.M. Effects of Training Status and Exercise Intensity on Phase II VO2 Kinetics. Med. Sci. Sports Exerc. 2004, 36, 225–232. [Google Scholar] [CrossRef]
- Lucia, A.; Hoyos, J.; Santalla, A.; Perez, M.; Chicharro, L. Kinetics of VO2 in Professional Cyclists. Med. Sci. Sports Exerc. 2002, 34, 320–325. [Google Scholar] [CrossRef]
- Murias, J.M.; Kowalchuk, J.M.; Paterson, D.H. Speeding of VO2 Kinetics with Endurance Training in Old and Young Men Is Associated with Improved Matching of Local O2 Delivery to Muscle O2 Utilization. J. Appl. Physiol. 2010, 108, 913–922. [Google Scholar] [CrossRef] [PubMed]
- Murias, J.M.; Spencer, M.D.; DeLorey, D.S.; Gurd, B.J.; Kowalchuk, J.M.; Paterson, D.H. Speeding of VO2 Kinetics during Moderate-Intensity Exercise Subsequent to Heavy-Intensity Exercise Is Associated with Improved Local O2 Distribution. J. Appl. Physiol. 2011, 111, 1410–1415. [Google Scholar] [CrossRef] [PubMed]
- Spencer, M.D.; Murias, J.M.; Grey, T.M.; Paterson, D.H. Regulation of VO2 Kinetics by O2 Delivery: Insights from Acute Hypoxia and Heavy-Intensity Priming Exercise in Young Men. J. Appl. Physiol. 2012, 112, 1023–1032. [Google Scholar] [CrossRef] [PubMed]
- Vanhatalo, A.; Fulford, J.; DiMenna, F.J.; Jones, A.M. Influence of Hyperoxia on Muscle Metabolic Responses and the Power-Duration Relationship during Severe-Intensity Exercise in Humans: A 31P Magnetic Resonance Spectroscopy Study: Hyperoxia and the Power-Duration Relationship. Exp. Physiol. 2010, 95, 528–540. [Google Scholar] [CrossRef] [PubMed]
- Jones, A.M.; Wilkerson, D.P.; DiMenna, F.; Fulford, J.; Poole, D.C. Muscle Metabolic Responses to Exercise above and below the “Critical Power” Assessed Using 31P-MRS. Am. J. Physiol.-Regul. Integr. Comp. Physiol. 2008, 294, R585–R593. [Google Scholar] [CrossRef] [PubMed]
- Krustrup, P.; Söderlund, K.; Mohr, M.; Bangsbo, J. The Slow Component of Oxygen Uptake during Intense, Sub-Maximal Exercise in Man Is Associated with Additional Fibre Recruitment. Pflüg. Arch. Eur. J. Physiol. 2004, 447, 855–866. [Google Scholar] [CrossRef]
- Bergstrom, H.C.; Housh, T.J.; Cochrane-Snyman, K.C.; Jenkins, N.D.M.; Byrd, M.T.; Switalla, J.R.; Schmidt, R.J.; Johnson, G.O. A Model for Identifying Intensity Zones Above Critical Velocity. J. Strength Cond. Res. 2017, 31, 3260–3265. [Google Scholar] [CrossRef]
- Bergstrom, H.C.; Housh, T.J.; Dinyer, T.K.; Byrd, T.M.; Jenkins, N.D.M.; Cochrane-Snyman, K.C.; Succi, P.J.; Schmidt, R.J.; Johnson, G.O.; Zuniga, J.M. Neuromuscular Responses of the Superficial Quadriceps Femoris Muscles: Muscle Specific Fatigue and Inter-Individual Variability during Severe Intensity Treadmill Running. J. Musculoskelet. Neuronal Interact. 2020, 20, 77–87. [Google Scholar]
- Hill, D.W.; Stevens, E.C. VO2 Response Profiles in Severe Intensity Exercise. J. Sports Med. Phys. Fit. 2005, 45, 239–247. [Google Scholar]
- Midgley, A.W.; Mc Naughton, L.R. Time at or near VO2max during Continuous and Intermittent Running. A Review with Special Reference to Considerations for the Optimisation of Training Protocols to Elicit the Longest Time at or near VO2max. J. Sports Med. Phys. Fit. 2006, 46, 1–14. [Google Scholar]
| Participant | Sex | Age (years) | Height (cm) | Body Mass (kg) | VO2max (mL∙kg−1∙min−1) | CP (W) | W’ (Kj) |
|---|---|---|---|---|---|---|---|
| 1 | M | 19 | 173 | 65.70 | 66.30 | 304.50 | 11.26 |
| 2 | M | 31 | 176 | 76.00 | 55.50 | 291.85 | 10.92 |
| 3 | M | 20 | 166 | 60.00 | 64.60 | 289.81 | 13.55 |
| 4 | M | 27 | 173 | 94.90 | 45.30 | 289.27 | 10.15 |
| 5 | M | 29 | 174 | 68.10 | 55.00 | 259.29 | 14.05 |
| 6 | M | 28 | 179 | 77.50 | 59.60 | 339.72 | 19.06 |
| 7 | F | 36 | 158 | 58.20 | 55.20 | 242.89 | 10.98 |
| 8 | M | 24 | 183 | 102.80 | 53.50 | 341.39 | 12.68 |
| Conditions | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| SPHIIE | FSHIIE | Main Effect Condition | Main Effect Time | Condition X Time Interaction | ||||||||
| Time (Minutes) | Time (Minutes) | |||||||||||
| Variable | 1 | 2 | 3 | 1 | 2 | 3 | p | η2 | p | η2 | p | η2 |
| Average VO2 (mL∙kg−1∙min−1) | 31.39 (4.28) | 51.59 (5.77) | 53.96 (5.36) | 29.96 (5.37) | 47.84 (11.94) | 50.07 (11.66) | 0.237 | 0.192 | 0.000 * | 0.879 | 0.628 | 0.064 |
| Average Peak VO2 (mL∙kg−1∙min−1) | 42.45 (5.59) | 53.64 (6.00) | 55.01 (5.47) | 41.61 (7.63) | 52.88 (8.38) | 54.68 (7.33) | 0.636 | 0.034 | 0.000 * | 0.917 | 0.912 | 0.013 |
| Variable | FSHIIE | SPHIIE |
|---|---|---|
| % of Total Training Time Above 90% VO2max | 25.20 ± 8.77 | 26.07 ± 11.84 |
| Peak Lactate | 14.77 ± 3.43 | 16.02 ± 2.39 |
| Average Lactate | 12.98 ± 2.28 | 13.61 ± 1.55 |
| Peak RPE | 19.00 ± 1.30 | 18.50 ± 1.69 |
| Average RPE | 17.21 ± 1.26 | 17.06 ± 1.74 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Miller, P.; Perez, N.; Farrell, J.W., III. Acute Oxygen Consumption Response to Fast Start High-Intensity Intermittent Exercise. Sports 2023, 11, 238. https://doi.org/10.3390/sports11120238
Miller P, Perez N, Farrell JW III. Acute Oxygen Consumption Response to Fast Start High-Intensity Intermittent Exercise. Sports. 2023; 11(12):238. https://doi.org/10.3390/sports11120238
Chicago/Turabian StyleMiller, Payton, Noah Perez, and John W. Farrell, III. 2023. "Acute Oxygen Consumption Response to Fast Start High-Intensity Intermittent Exercise" Sports 11, no. 12: 238. https://doi.org/10.3390/sports11120238
APA StyleMiller, P., Perez, N., & Farrell, J. W., III. (2023). Acute Oxygen Consumption Response to Fast Start High-Intensity Intermittent Exercise. Sports, 11(12), 238. https://doi.org/10.3390/sports11120238






