Bodyweight and Combined Training Reduce Chronic Low-Grade Inflammation and Improve Functional Fitness of Postmenopausal Women
Abstract
1. Introduction
2. Materials and Methods
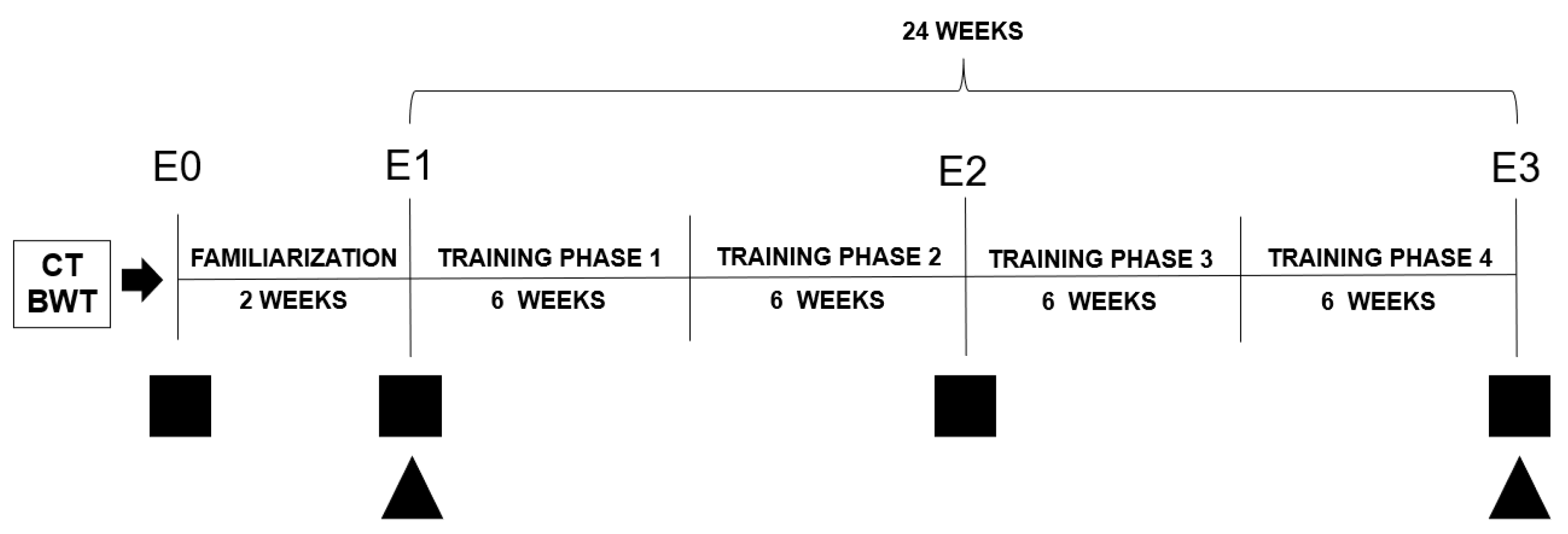
2.1. Experimental Design
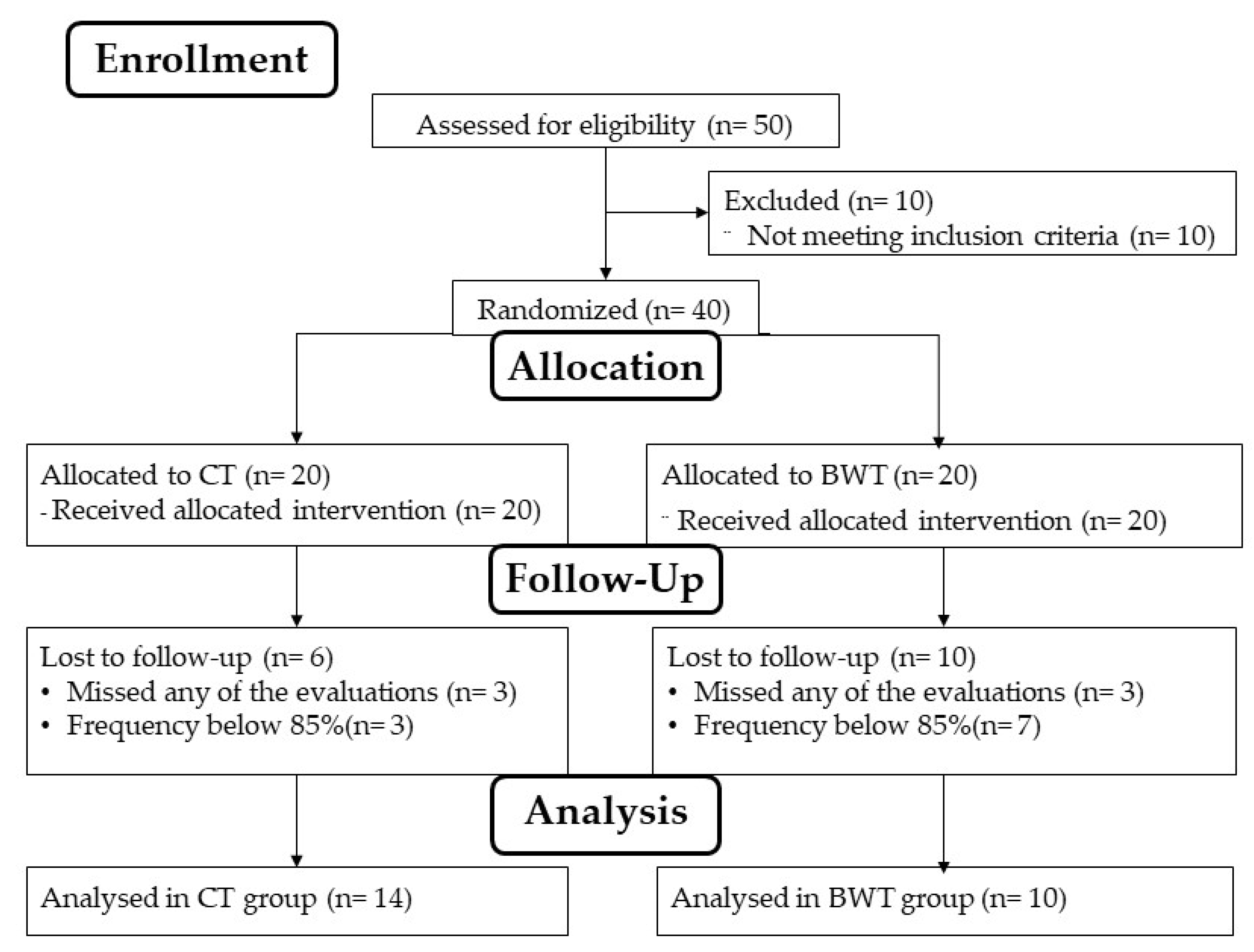
2.2. Subjects
2.3. Intervention
2.4. Data Collection
2.4.1. Cytokines
2.4.2. Hand Grip Test
2.4.3. Five Times Sit to Stand Test
2.4.4. Stand-Up and Walk around the House
2.4.5. Rise from Prone Position
2.4.6. Dressing on and Taking off a T-Shirt
2.4.7. Gallon-Jug Shelf-Transfer
2.4.8. Test of 400-Meter Walk
2.5. Statistical Analysis
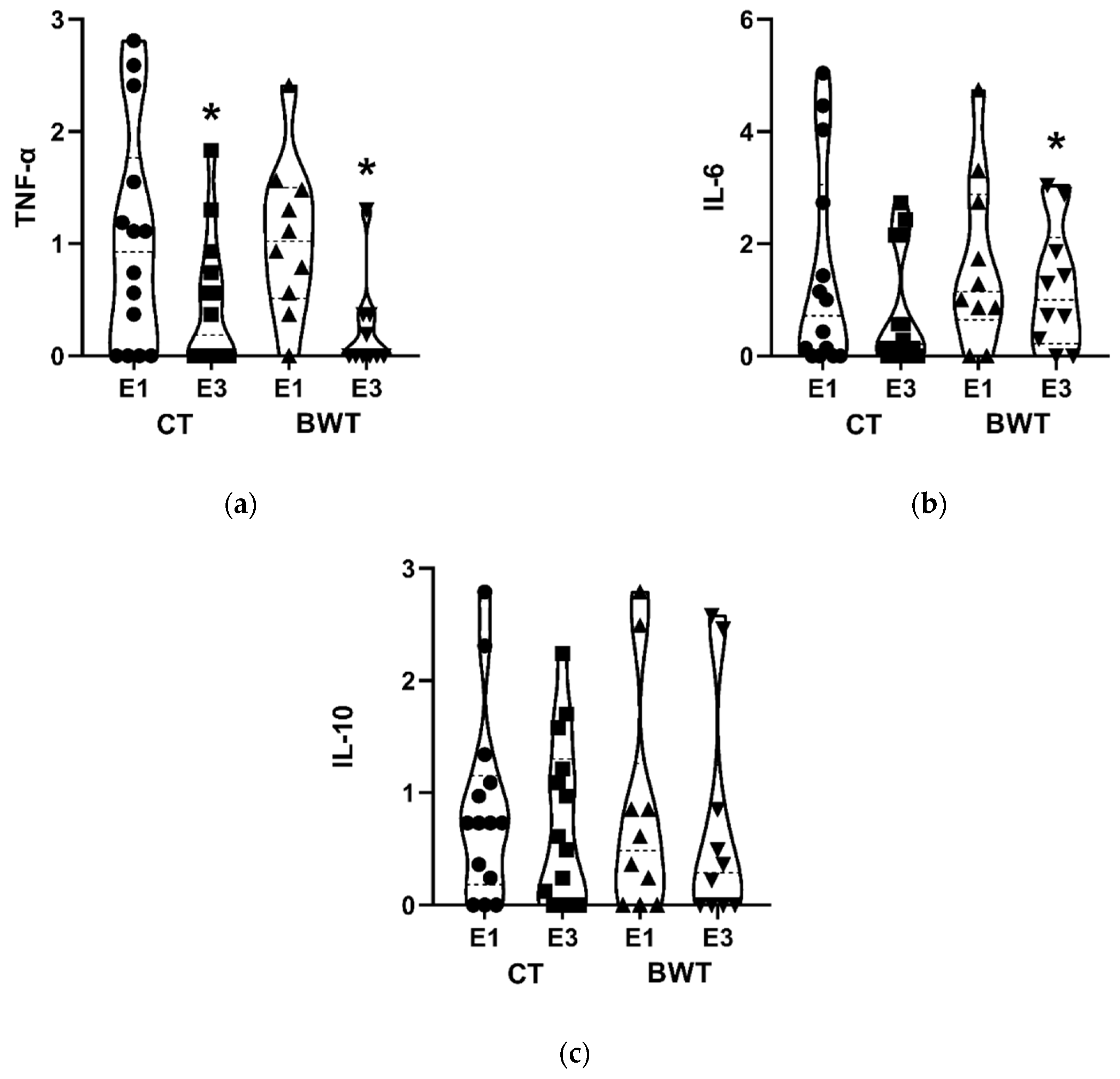
3. Results
4. Discussion
5. Conclusions and Practical Application
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Fragala, M.S.; Cadore, E.L.; Dorgo, S.; Izquierdo, M.; Kraemer, W.J.; Peterson, M.D.; Ryan, E.D. Resistance Training for Older Adults: Position Statement from the National Strength and Conditioning Association. J. Strength Cond. Res. 2019, 33, 2019–2052. [Google Scholar] [CrossRef] [PubMed]
- Duggal, N.A.; Niemiro, G.; Harridge, S.D.R.; Simpson, R.J.; Lord, J.M. Can Physical Activity Ameliorate Immunosenescence and Thereby Reduce Age-Related Multi-Morbidity? Nat. Rev. Immunol. 2019, 19, 563–572. [Google Scholar] [CrossRef] [PubMed]
- Izquierdo, M.; Merchant, R.A.; Morley, J.E.; Anker, S.D.; Aprahamian, I.; Arai, H.; Aubertin-Leheudre, M.; Bernabei, R.; Cadore, E.L.; Cesari, M.; et al. International Exercise Recommendations in Older Adults (ICFSR): Expert Consensus Guidelines. J. Nutr. Health Aging 2021, 25, 824–853. [Google Scholar] [CrossRef] [PubMed]
- Cadore, E.; Pinto, R.S.; Bottaro, M.; Izquierdo, M. Strength and Endurance Training Prescription in Healthy and Frail Elderly. Aging Dis. 2014, 5, 183–195. [Google Scholar] [CrossRef]
- Stuenkel, C.A.; Davis, S.R.; Gompel, A.; Lumsden, M.A.; Murad, M.H.; Pinkerton, J.V.; Santen, R.J. Treatment of Symptoms of the Menopause: An Endocrine Society Clinical Practice Guideline. J. Clin. Endocrinol. Metab. 2015, 100, 3975–4011. [Google Scholar] [CrossRef]
- Flynn, M.G.; Markofski, M.M.; Carrillo, A.E. Elevated Inflammatory Status and Increased Risk of Chronic Disease in Chronological Aging: Inflamm-Aging or Inflamm-Inactivity? Aging Dis. 2019, 10, 147–156. [Google Scholar] [CrossRef]
- Methenitis, S. A Brief Review on Concurrent Training: From Laboratory to the Field. Sports 2018, 6, 127. [Google Scholar] [CrossRef]
- Resende-Neto, A.G.; Oliveira Andrade, B.C.; Cyrino, E.S.; Behm, D.G.; DeSantana, J.M.; Da Silva-Grigoletto, M.E. Effects of Functional and Traditional Training in Body Composition and Muscle Strength Components in Older Women: A Randomized Controlled Trial. Arch. Gerontol. Geriatr. 2019, 84, 103902. [Google Scholar] [CrossRef]
- de Resende-Neto, A.G.; Aragão-Santos, J.C.; Oliveira-Andrade, B.C.; Silva Vasconcelos, A.B.; De Sá, C.A.; Aidar, F.J.; DeSantana, J.M.; Cadore, E.L.; Da Silva-Grigoletto, M.E. The Efficacy of Functional and Traditional Exercise on the Body Composition and Determinants of Physical Fitness of Older Women: A Randomized Crossover Trial. J. Aging Res. 2019, 2019, 5315376. [Google Scholar] [CrossRef]
- Vasconcelos, A.B.S.; de Resende-Neto, A.G.; Nogueira, A.C.; Aragão-Santos, J.C.; Monteiro, M.R.P.; Morais Junior, G.S.; Avelar, G.G.; Camargo, E.A.; de Toledo Nóbrega, O.; Da Silva-Grigoletto, M.E. Functional and Traditional Training Improve Muscle Power and Reduce Proinflammatory Cytokines in Older Women: A Randomized Controlled Trial. Exp. Gerontol. 2020, 135, 110920. [Google Scholar] [CrossRef]
- Chaves, L.M.D.S.; Santos, G.V.; Teixeira, C.L.S.; Da Silva-Grigoletto, M.E. Calisthenics and bodyweight exercises: Different concepts or scientific synonyms? Rev. Bras. Fisiol. Exerc. 2020, 19, 13–15. [Google Scholar] [CrossRef]
- Santos, G.V.; De Resende Neto, A.G.; Chaves, L.M.D.S.; De Jesus, L.C.; Vasconcelos, A.B.S.; Barranco-Ruiz, Y.; Monteiro, M.R.P.; Bocalini, D.S.; Teixeira, C.V.L.S.; Da Silva-Grigoletto, M.E. Effects of Bodyweight and Traditional Resistance Training on the Functionality of Elderly People: A Randomized Clinical Trial. Rev. Bras. Fisiol. Exerc. 2020, 19, 180–191. [Google Scholar] [CrossRef]
- Osuka, Y.; Suzuki, T.; Kim, M.; Kojima, N.; Fujino, K.; Yoshida, Y.; Hirano, H.; Kim, H. Association between Exercise Type and the Decline in Instrumental Activities of Daily Living in Community-Dwelling Older Women: A 4-Year Prospective Study. Prev. Med. 2018, 112, 23–30. [Google Scholar] [CrossRef] [PubMed]
- Watanabe, Y.; Tanimoto, M.; Oba, N.; Sanada, K.; Miyachi, M.; Ishii, N. Effect of Resistance Training Using Bodyweight in the Elderly: Comparison of Resistance Exercise Movement between Slow and Normal Speed Movement: Exercise Training Using Bodyweight in Elderly. Geriatr. Gerontol. Int. 2015, 15, 1270–1277. [Google Scholar] [CrossRef]
- Kaya, D.O.; Duzgun, I.; Baltaci, G.; Karacan, S.; Colakoglu, F. Effects of Calisthenics and Pilates Exercises on Coordination and Proprioception in Adult Women: A Randomized Controlled Trial. Hum. Kinet. 2012, 21, 235–243. [Google Scholar] [CrossRef]
- James, E.G.; Leveille, S.G.; Hausdorff, J.M.; Barton, B.; Cote, S.; Karabulut, M.; Conatser, P.; Kennedy, D.N.; Tucker, K.L.; Al Snih, S.; et al. Coordination Impairments Are Associated with Falling among Older Adults. Exp. Aging Res. 2017, 43, 430–439. [Google Scholar] [CrossRef]
- Cleland, C.; Ferguson, S.; Ellis, G.; Hunter, R.F. Validity of the International Physical Activity Questionnaire (IPAQ) for Assessing Moderate-to-Vigorous Physical Activity and Sedentary Behaviour of Older Adults in the United Kingdom. BMC Med. Res. Methodol. 2018, 18, 176. [Google Scholar] [CrossRef]
- Haff, G.; Triplett, N.T. Essentials of Strength Training and Conditioning, 4th ed.; Human Kinectis: Champaign, United States of America, 2015; ISBN 978-1-71821-086-8. [Google Scholar]
- La Scala Teixeira, C.V.; Evangelista, A.L.; Pereira, P.E.D.A.; Da Silva-Grigoletto, M.E.; Bocalini, D.S.; Behm, D.G. Complexity: A Novel Load Progression Strategy in Strength Training. Front. Physiol. 2019, 10, 839. [Google Scholar] [CrossRef]
- Da Silva-Grigoletto, M.E. Validación de la escala de valoración subjetiva del esfuerzo OMNI-GSE para el control de la intensidad global en sesiones de objetivos múltiples en personas mayores. Kronos Act. Física Salud 2013, 12, 32–40. [Google Scholar]
- Kiss, M.A.P. Avaliação em Educação Física: Aspectos Biológicos e Educacionais; Manole: São Paulo, Brazil, 1987. [Google Scholar]
- Guralnik, J.M.; Simonsick, E.M.; Ferrucci, L.; Glynn, R.J.; Berkman, L.F.; Blazer, D.G.; Scherr, P.A.; Wallace, R.B. A Short Physical Performance Battery Assessing Lower Extremity Function: Association with Self-Reported Disability and Prediction of Mortality and Nursing Home Admission. J. Gerontol. 1994, 49, M85–M94. [Google Scholar] [CrossRef]
- Andreotti, R.A.; Okuma, S.S. Validating a Test Battery of Activities of Daily Living for Physically Independent Elderly. Rev. Paul. Educ. Física 1999, 13, 46–66. [Google Scholar] [CrossRef]
- Martin Dantas, E.H.; Gomes de Souza Vale, R. Protocolo GDLAM de avaliação da autonomia funcional. Fit. Perform. J. 2004, 3, 175–183. [Google Scholar] [CrossRef][Green Version]
- Signorile, J.F.; Sandler, D.; Ma, F.; Bamel, S.; Stanziano, D.; Smith, W.; Roos, B.A.; Sandals, L. The Gallon-Jug Shelf-Transfer Test: An Instrument to Evaluate Deteriorating Function in Older Adults. J. Aging Phys. Act. 2007, 15, 56–74. [Google Scholar] [CrossRef] [PubMed]
- Vestergaard, S.; Patel, K.V.; Bandinelli, S.; Ferrucci, L.; Guralnik, J.M. Characteristics of 400-Meter Walk Test Performance and Subsequent Mortality in Older Adults. Rejuvenation Res. 2009, 12, 177–184. [Google Scholar] [CrossRef]
- Cohen, J. Statistical Power Analysis for the Behavioral Sciences, 2nd ed.; L. Erlbaum Associates: Hillsdale, NJ, USA, 1988; ISBN 978-0-8058-0283-2. [Google Scholar]
- Şahin, M.; Aybek, E. Jamovi: An Easy to Use Statistical Software for the Social Scientists. Int. J. Assess. Tools Educ. 2019, 6, 670–692. [Google Scholar] [CrossRef]
- Sardeli, A.V.; Tomeleri, C.M.; Cyrino, E.S.; Fernhall, B.; Cavaglieri, C.R.; Chacon-Mikahil, M.P.T. Effect of Resistance Training on Inflammatory Markers of Older Adults: A Meta-Analysis. Exp. Gerontol. 2018, 111, 188–196. [Google Scholar] [CrossRef]
- Campo, R.A.; Light, K.C.; O’Connor, K.; Nakamura, Y.; Lipschitz, D.; LaStayo, P.C.; Pappas, L.M.; Boucher, K.M.; Irwin, M.R.; Hill, H.R.; et al. Blood Pressure, Salivary Cortisol, and Inflammatory Cytokine Outcomes in Senior Female Cancer Survivors Enrolled in a Tai Chi Chih Randomized Controlled Trial. J. Cancer Surviv. 2015, 9, 115–125. [Google Scholar] [CrossRef]
- Ferrucci, L.; Fabbri, E. Inflammageing: Chronic Inflammation in Ageing, Cardiovascular Disease, and Frailty. Nat. Rev. Cardiol. 2018, 15, 505–522. [Google Scholar] [CrossRef]
- Bohannon, R.W. Hand-Grip Dynamometry Predicts Future Outcomes in Aging Adults. J. Geriatr. Phys. Ther. 2008, 31, 3–10. [Google Scholar] [CrossRef]
- Resende-Neto, A.G.; da Silva Resende, M.; Oliveira-Andrade, B.C.; da Silva Chaves, L.M.; Brandão, L.H.A.; Nogueira, A.C.; Mota, M.M.; DeSantana, J.M.; Da Silva-Grigoletto, M.E. Functional Training in Comparison to Traditional Training on Physical Fitness and Quality of Movement in Older Women. Sport Sci. Health 2021, 17, 213–222. [Google Scholar] [CrossRef]
- Aragão-Santos, J.C.; Vasconcelos, A.B.S.; de Resende-Neto, A.G.; Rodrigues, L.S.; de Lima Silva, N.; Da Silva, D.N.; Schimieguel, D.M.; Correa, C.B.; Da Silva-Grigoletto, M.E. Functional and Concurrent Training Do Not Impair Immune Function and Improve Functional Fitness in Postmenopausal Women: A Randomized Controlled Trial. Exp. Gerontol. 2021, 153, 111504. [Google Scholar] [CrossRef] [PubMed]
- Cadore, E.L.; Izquierdo, M. Muscle Power Training: A Hallmark for Muscle Function Retaining in Frail Clinical Setting. J. Am. Med. Dir. Assoc. 2018, 19, 190–192. [Google Scholar] [CrossRef] [PubMed]
- Resende-Neto, A.G.; Da Silva-Grigoletto, M.E. Prescription of the Functional Strength Training for Older People: A Brief Review. J. Aging Sci. 2019, 7, 210. [Google Scholar] [CrossRef]
- Ribeiro, A.; Carneiro, N.; Nascimento, M.; Gobbo, L.; Schoenfeld, B.J.; Achour Júnior, A.; Gobbi, S.; Oliveira, A.; Cyrino, E. Effects of Different Resistance Training Frequencies on Flexibility in Older Women. Clin. Interv. Aging 2015, 10, 531. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Byrne, C.; Faure, C.; Keene, D.J.; Lamb, S.E. Ageing, Muscle Power and Physical Function: A Systematic Review and Implications for Pragmatic Training Interventions. Sports Med. 2016, 46, 1311–1332. [Google Scholar] [CrossRef]
- Resende-Neto, A.G.; Do Nascimento, M.A.; de Sá, C.A.; Ribeiro, A.S.; DeSantana, J.M.; Da Silva-Grigoletto, M.E. Comparison between Functional and Traditional Training Exercises on Joint Mobility, Determinants of Walking and Muscle Strength in Older Women. J. Sports Med. Phys. Fit. 2019, 59, 1659–1668. [Google Scholar] [CrossRef]
- Marin, L.; Salerno, A.P.; Variani, F. Efeito Do Exercício Calistênico Na Dor e Capacidade Cardiorrespiratória de Idosos Com Doença Arterial Obstrutiva Periférica. Rev. FisiSenectus 2016, 3, 47–58. [Google Scholar] [CrossRef]
- McRae, G.; Payne, A.; Zelt, J.G.E.; Scribbans, T.D.; Jung, M.E.; Little, J.P.; Gurd, B.J. Extremely Low Volume, Whole-Body Aerobic–Resistance Training Improves Aerobic Fitness and Muscular Endurance in Females. Appl. Physiol. Nutr. Metab. 2012, 37, 1124–1131. [Google Scholar] [CrossRef]
- Khalafi, M.; Malandish, A.; Rosenkranz, S.K. The Impact of Exercise Training on Inflammatory Markers in Postmenopausal Women: A Systemic Review and Meta-Analysis. Exp. Gerontol. 2021, 150, 111398. [Google Scholar] [CrossRef]
- Hurst, C.; Weston, K.L.; McLaren, S.J.; Weston, M. The Effects of Same-Session Combined Exercise Training on Cardiorespiratory and Functional Fitness in Older Adults: A Systematic Review and Meta-Analysis. Aging Clin. Exp. Res. 2019, 31, 1701–1717. [Google Scholar] [CrossRef]
| Characteristics | CT (n = 14) | BWT (n = 10) | p Interaction |
|---|---|---|---|
| Anthropometry (mean and standard deviation) | |||
| Age (years) | 64.43 ± 3.13 | 65.10 ± 4.86 | 0.685 |
| Body mass (kg) | 71.95 ± 8.36 | 67.92 ± 10.14 | 0.298 |
| Height (m) | 1.57 ± 0.06 | 1.54 ± 0.06 | 0.258 |
| BMI (kg/m²) | 29.56 ± 4.80 | 28.76 ± 4.26 | 0.680 |
| WHR | 0.86 ± 0.10 | 0.88 ± 0.10 | 0.763 |
| Medical History (relative and absolute frequency) | |||
| Hypertension | 35.7 (5) | 50.0 (5) | 0.484 |
| Diabetes | 7.1 (1) | 10.0 (1) | 0.803 |
| Dyslipidemia | 42.9 (6) | 50.0 (5) | 0.729 |
| Osteoarthritis | 28.6 (4) | 20.0 (2) | 0.633 |
| Arthritis | 21.4 (3) | 40.0 (4) | 0.324 |
| Depression | 7.1 (1) | 40.0 (4) | 0.051 |
| E1 | E2 | E3 | Analysis | |
|---|---|---|---|---|
| HGT (kg/F) | ||||
| CT | 22.46 ± 4.24 | 23.96 ± 3.81 (∆ = 6.67%; d = 0.372; CI = [−3.108; 0.108]) | 24.21 ± 3.82 * (∆ = 7.79%; d = 0.434; CI = [−3.242; −0.258]) | p time < 0.001 p interaction = 0.064 η² parcial = 0.118 |
| BWT | 21.80 ± 4.72 | 22.35 ± 3.91 (∆ = 2.52%; d = 0.127; CI = [−2.448; 1.358]) | 24.70 ± 4.08 *⸸ (∆ = 13.30%; d = 0.657; CI = [4.660; −1.330]) | |
| 5XSTS (s) | ||||
| CT | 7.75 ± 1.54 | 6.57 ± 1.61 * (∆ = −15.23%; d = 0.749; CI = [0.494; 1.858]) | 5.83 ± 1.32 *⸸ (∆ = −24.77%; d = 1.339; CI = [1.335; 2.487]) | p time < 0.001 p interaction = 0.998 η² parcial = 0.000 |
| BWT | 7.77 ± 1.36 | 6.59 ± 1.49 * (∆ = −15.18%; d = 0.827; CI = [0.368; 1.982]) | 5.88 ± 1.30 * (∆ = −24.19%; d = 1.421; CI = [1.210; 2.574]) | |
| SUWAH (s) | ||||
| CT | 33.68 ± 3.41 | 31.72 ± 2.99 * (∆ = −5.82%; d = 0.611; CI = [0.009; 3.911]) | 30.59 ± 3.77 * (∆ = −9.17%; d = 0.860; CI = [0.802; 5.380]) | p time < 0.001 p interaction = 0.732 η² parcial = 0.009 |
| BWT | 34.19 ± 3.11 | 32.78 ± 1.88 (∆ = −4.12%; d = 0.549; CI = [−0.798; 3.818]) | 30.84 ± 2.32 *⸸ (∆ = −9.79%; d = 1.221; CI = [0.645; 6.061]) | |
| RPP (s) | ||||
| CT | 2.56 ± 1.00 | 2.50 ± 0.95 (∆ = −2.34%; d = 0.062; CI = [−0.222; 0.349]) | 2.42 ± 0.88 (∆ = −5.49 %; d = 0.149; CI = [−0.209; 0.506]) | p time < 0.001 p interaction = 0.034 η² parcial = 0.143 |
| BWT | 2.87 ± 1.21 | 2.60 ± 1.02 (∆ = −9.40%; d = 0.241; CI = [−0.072; 0.604]) | 2.22 ± 0.97 *⸸ (∆ = −22.64% d = 0.593; CI = [0.227; 1.073]) | |
| DTOT (s) | ||||
| CT | 13.70 ± 2.59 | 12.39 ± 2.10 * (∆ = −9.56%; d = 0.556; CI = [0.022; 2.611]) | 12.08 ± 2.08 * (∆ = −11.82%; d = 0.690; CI = [0.218; 3.028]) | p time < 0.001 p interaction = 0.728 η² parcial = 0.011 |
| BWT | 14.10 ± 2.11 | 12.86 ± 1.43 (∆ = −8.79%; d = 0.688; CI = [−0.291; 2.773]) | 12.08 ± 2.06 * (∆ = −14.32%; d = 0.969; CI = [0.361; 3.685]) | |
| GJST (s) | ||||
| CT | 10.68 ± 0.80 | 10.41 ± 1.09 (∆ = −2.53%; d = 0.282; CI = [−0.265; 0.808]) | 9.93 ± 0.74 *⸸ (∆ = −7.02%; d = 0.973; CI = [0.330; 1.166]) | p time < 0.001 p interaction = 0.631 η² parcial = 0.021 |
| BWT | 11.11 ± 0.92 | 10.80 ± 0.76 (∆ = −2.79%; d = 0.367; CI = [−0.323; 0.947]) | 10.12 ± 0.84 *⸸ (∆ = −8.91%; d = 1.124; CI = [0.495; 1.485]) | |
| 400 MW (s) | ||||
| CT | 242.92 ± 28.82 | 222.57 ± 38.88 (∆ = −8.38%; d = 0.595; CI = [2.040; 38.670]) | 229.78 ± 31.55 (∆ = −5.41%; d = 0.435; CI = [−5.175; 31.460]) | p time = 0.003 p interaction = 0.283 η² parcial = 0.056 |
| BWT | 239.70 ± 23.02 | 222.40 ± 23.32 (∆ = −7.22%; d = 0.747; CI = [−4.374; 38.971]) | 212.40 ± 21.70 * (∆ = −11.38%; d = 1.220; CI = [5.626; 31.672]) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Monteiro, M.R.P.; Aragão-Santos, J.C.; Vasconcelos, A.B.S.; Resende-Neto, A.G.d.; Chaves, L.M.d.S.; Cardoso, A.P.; Nogueira, A.C.; Carnero-Diaz, A.; Marcos-Pardo, P.J.; Corrêa, C.B.; et al. Bodyweight and Combined Training Reduce Chronic Low-Grade Inflammation and Improve Functional Fitness of Postmenopausal Women. Sports 2022, 10, 143. https://doi.org/10.3390/sports10100143
Monteiro MRP, Aragão-Santos JC, Vasconcelos ABS, Resende-Neto AGd, Chaves LMdS, Cardoso AP, Nogueira AC, Carnero-Diaz A, Marcos-Pardo PJ, Corrêa CB, et al. Bodyweight and Combined Training Reduce Chronic Low-Grade Inflammation and Improve Functional Fitness of Postmenopausal Women. Sports. 2022; 10(10):143. https://doi.org/10.3390/sports10100143
Chicago/Turabian StyleMonteiro, Marcos Raphael Pereira, José Carlos Aragão-Santos, Alan Bruno Silva Vasconcelos, Antônio Gomes de Resende-Neto, Leury Max da Silva Chaves, Alan Pantoja Cardoso, Albernon Costa Nogueira, Angel Carnero-Diaz, Pablo Jorge Marcos-Pardo, Cristiane Bani Corrêa, and et al. 2022. "Bodyweight and Combined Training Reduce Chronic Low-Grade Inflammation and Improve Functional Fitness of Postmenopausal Women" Sports 10, no. 10: 143. https://doi.org/10.3390/sports10100143
APA StyleMonteiro, M. R. P., Aragão-Santos, J. C., Vasconcelos, A. B. S., Resende-Neto, A. G. d., Chaves, L. M. d. S., Cardoso, A. P., Nogueira, A. C., Carnero-Diaz, A., Marcos-Pardo, P. J., Corrêa, C. B., Moura, T. R. d., & Da Silva-Grigoletto, M. E. (2022). Bodyweight and Combined Training Reduce Chronic Low-Grade Inflammation and Improve Functional Fitness of Postmenopausal Women. Sports, 10(10), 143. https://doi.org/10.3390/sports10100143







