Experimental Evaluation of the Tribological Properties of Rigid Gas-Permeable Contact Lens Under Different Lubricants
Abstract
1. Introduction
2. Materials and Methods
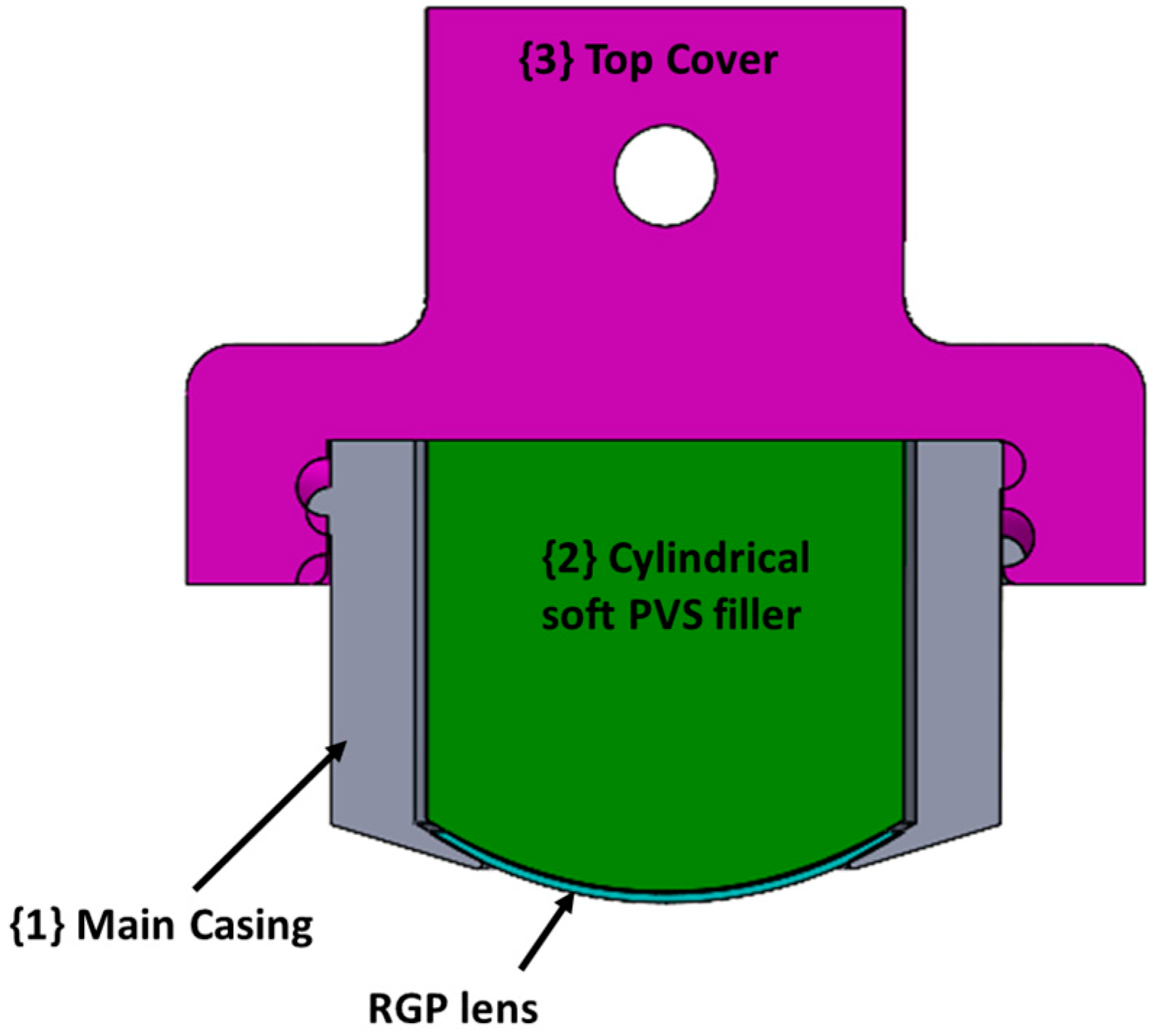
2.1. Rigid Gas-Permeable (RGP) Contact Lens Samples
2.2. Counter Surface
2.3. Lubricants
- Artificial tear solution contains lipids, salts, and proteins. In general, a complex of salt solution was made, containing 5.26 mg/mL of sodium chloride, 1.19 mg/mL of potassium chloride, 0.44 mg/mL of sodium citrate, 0.036 mg/mL of glucose, 0.072 mg/mL of urea, 0.07 mg/mL of calcium chloride, 1.27 mg/mL of sodium carbonate, 0.3 mg/mL of potassium hydrogen carbonate, 3.41 mg/mL of sodium phosphate dibasic, 0.94 mg/mL of hydrochloric acid, and 200 μl of ProClin 300 per one liter of solution. Then, a stock lipid solution including 3.6 mg/mL of oleic acid, 24.0 mg/mL of oleic acid methyl ester, 32.0 mg/mL of triolein, 3.6 mg/mL of cholesterol, 48.0 mg/mL if cholesteryl oleate, and 1.0 mg/mL of phosphatidylcholine was dissolved in a solution of 1 hexane: 1 ether. The detailed preparation of lipid–salt mixed solution has been previously published [21,29]. We added 2 mg/ml of lysozyme and 0.2 mg/ml of albumin into the mixed solution for further experiments. The tear film proteins in healthy human eyes contain on average 1.9 mg/mL of lysozyme, 0.2 mg/mL of albumin, 0.15 mg/mL of mucin, 1.8 mg/mL of lactoferrin, and 0.02 mg/mL of immunoglobulin G [30]. Since lysozyme is the most abundant tear film protein, and the concentration of albumin is similar when eyes are closed or wearing ortho-k lenses [31,32], only these two proteins were added into the artificial tear solution. All the chemicals were purchased from Sigma-Aldrich (St. Louis, MO, USA).
- Polysaccharides containing care solution included 0.45 g of alginate acid (AA, Sigma-Aldrich), 0.45 g of lambda-carrageenan (CRG, Sigma-Aldrich), 0.75 g of poloxamer-407 (Wei Ming Pharmaceutical Mfg. Co., Ltd., Taipei, Taiwan), 0.2 g of ethylenediaminetetraacetic acid (Sigma-Aldrich), 0.015 g of calcium chloride (Sigma-Aldrich), 0.15 g of potassium chloride (Sigma-Aldrich), 0.45 g of sodium chloride (Sigma-Aldrich), 0.4 g of sodium phosphate dibasic (Sigma-Aldrich), and double distilled water in a final volume of 100 mL and pH of 7.4.
- Normal saline solution contained 0.9 g of sodium chloride in 100 mL of double distilled water (Taiwan Biotech Co., Ltd., Taoyuan, Taiwan).
- The commercial care solution used was Menicon Care Plus multipurpose solution for all rigid gas-permeable lenses (Menicon, Nagoya, Japan). The main ingredients are 0.5% poloxamer, 0.0005% polyhexamethylene biguanide, and 0.275% hypromellose, according to manufacturer’s manual. The reason for selecting this commercial care solution was the presence of hypromellose, which is also a kind of polysaccharide.
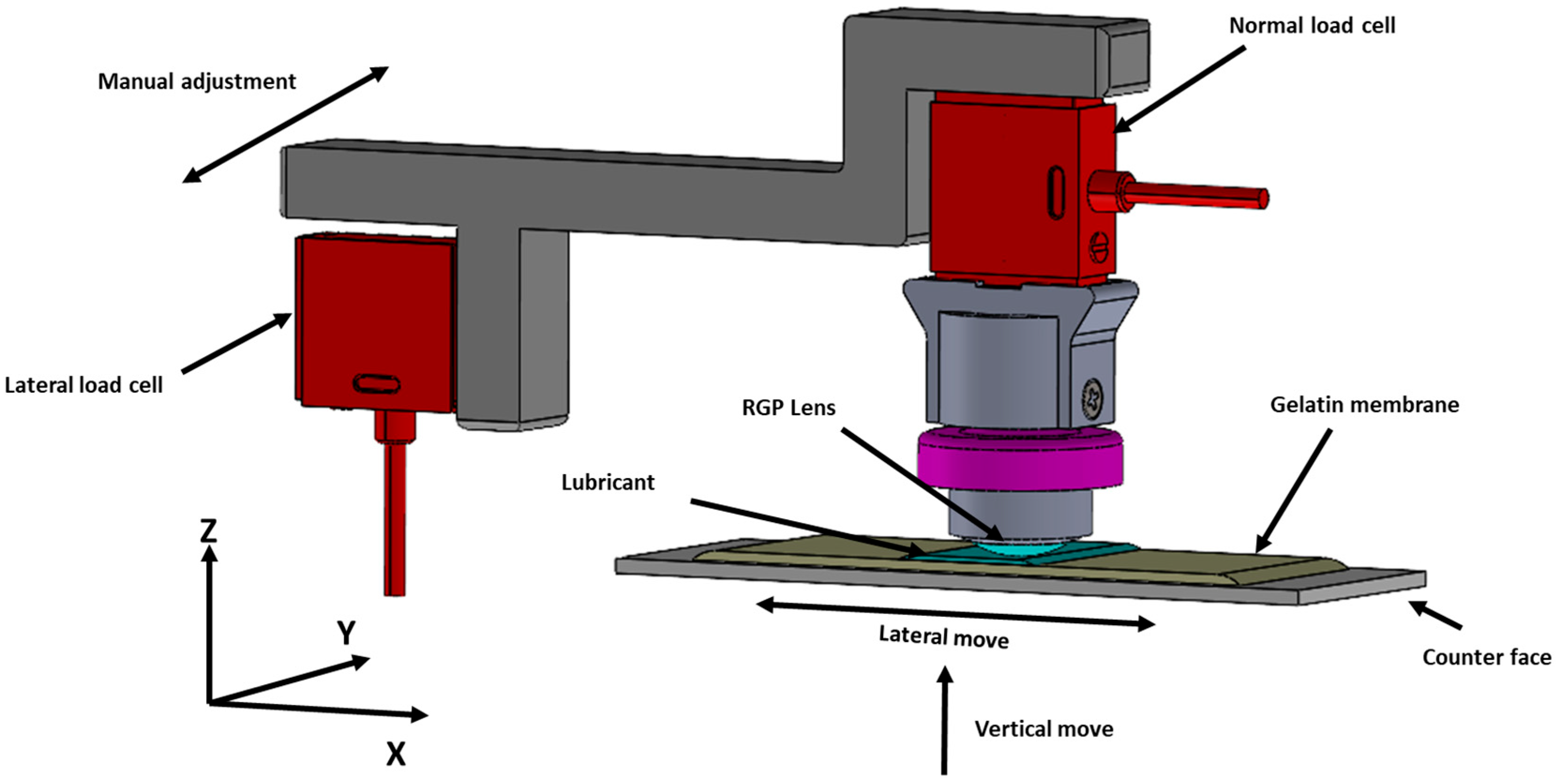
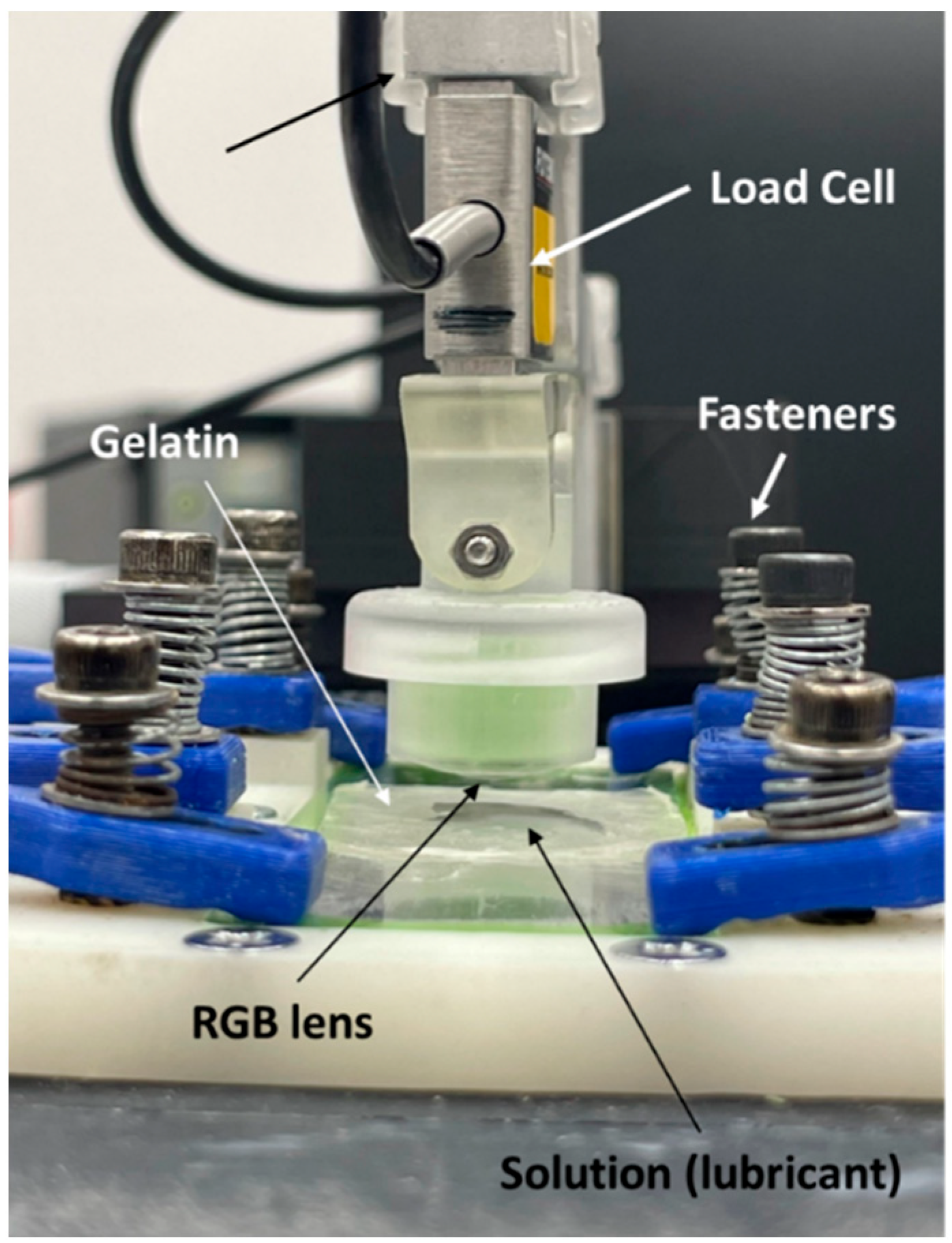
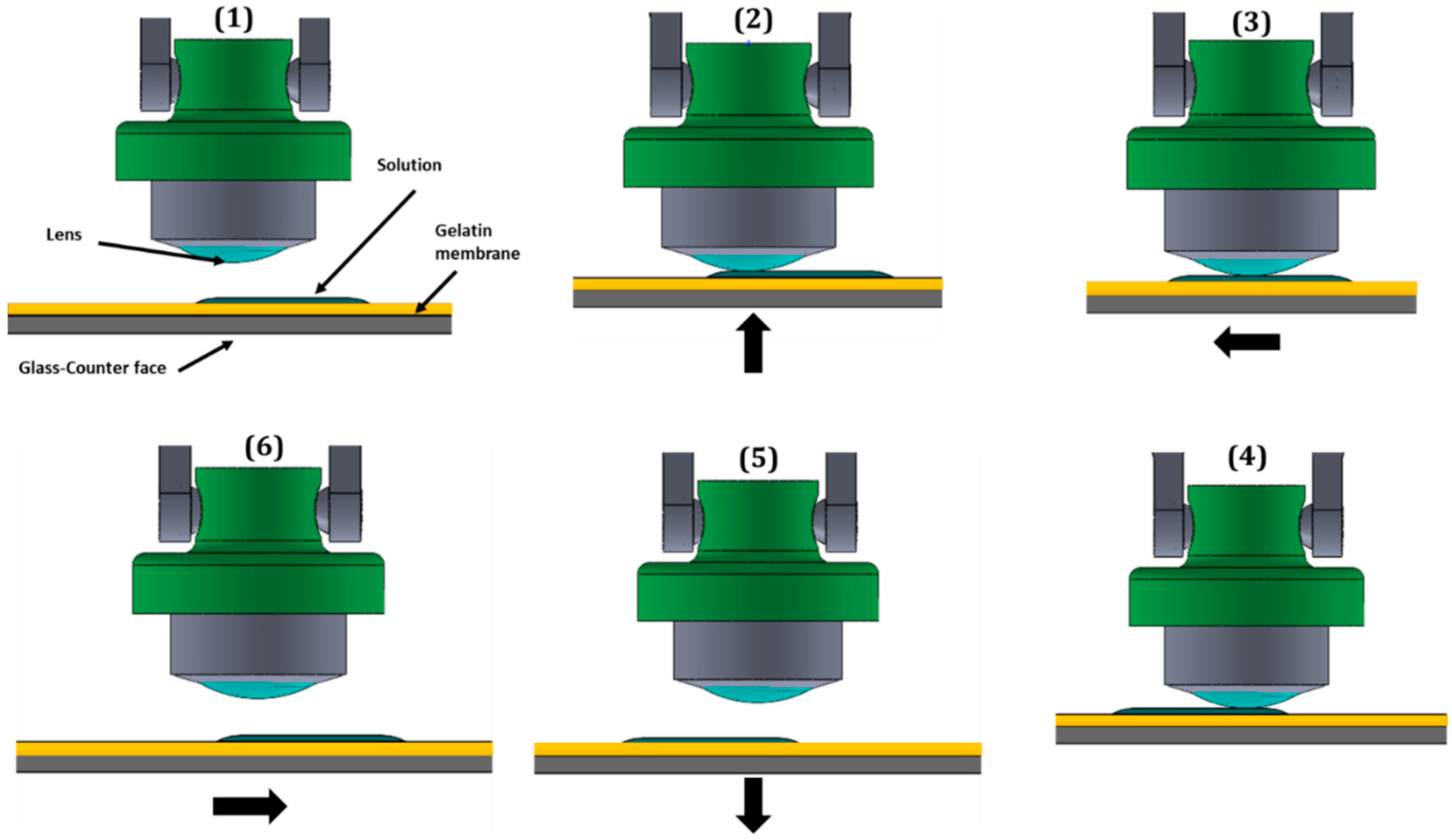
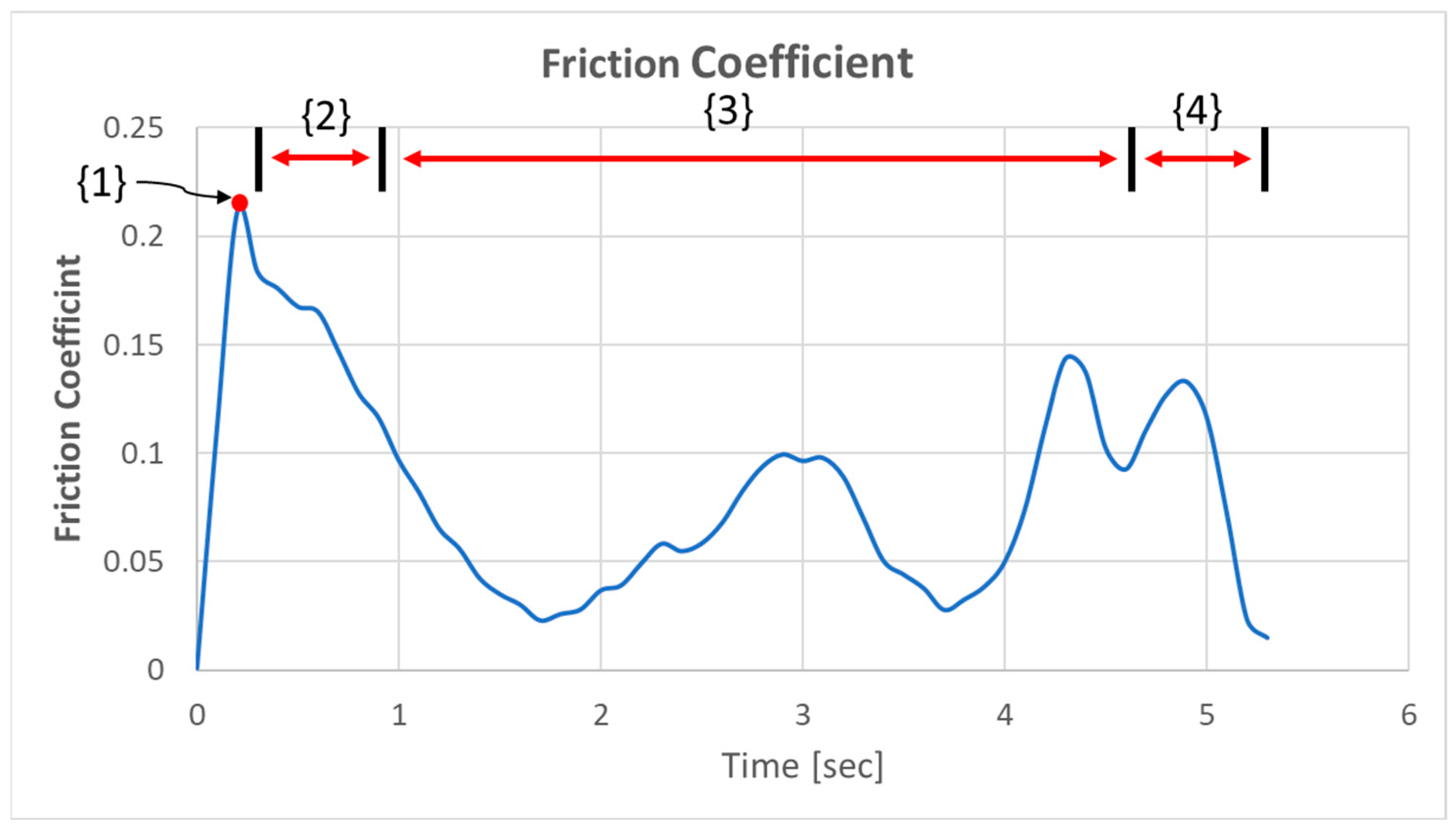
2.4. Experimental Setup for Measuring Tribological Property of RGP Lenses
2.5. Tribological Experiment Procedure
2.6. Analysis of Physical–Chemical Properties of Different Lubricants
3. Results and Discussion
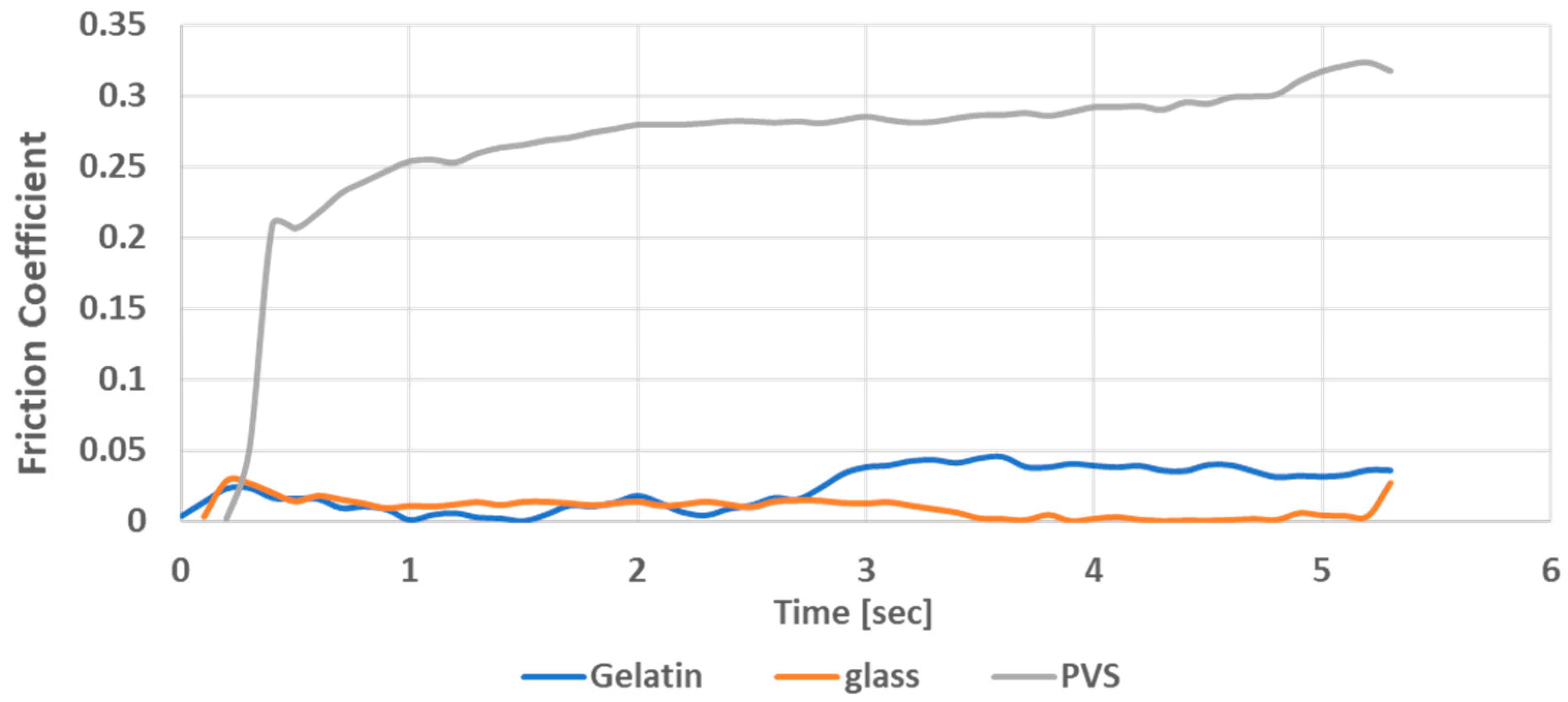
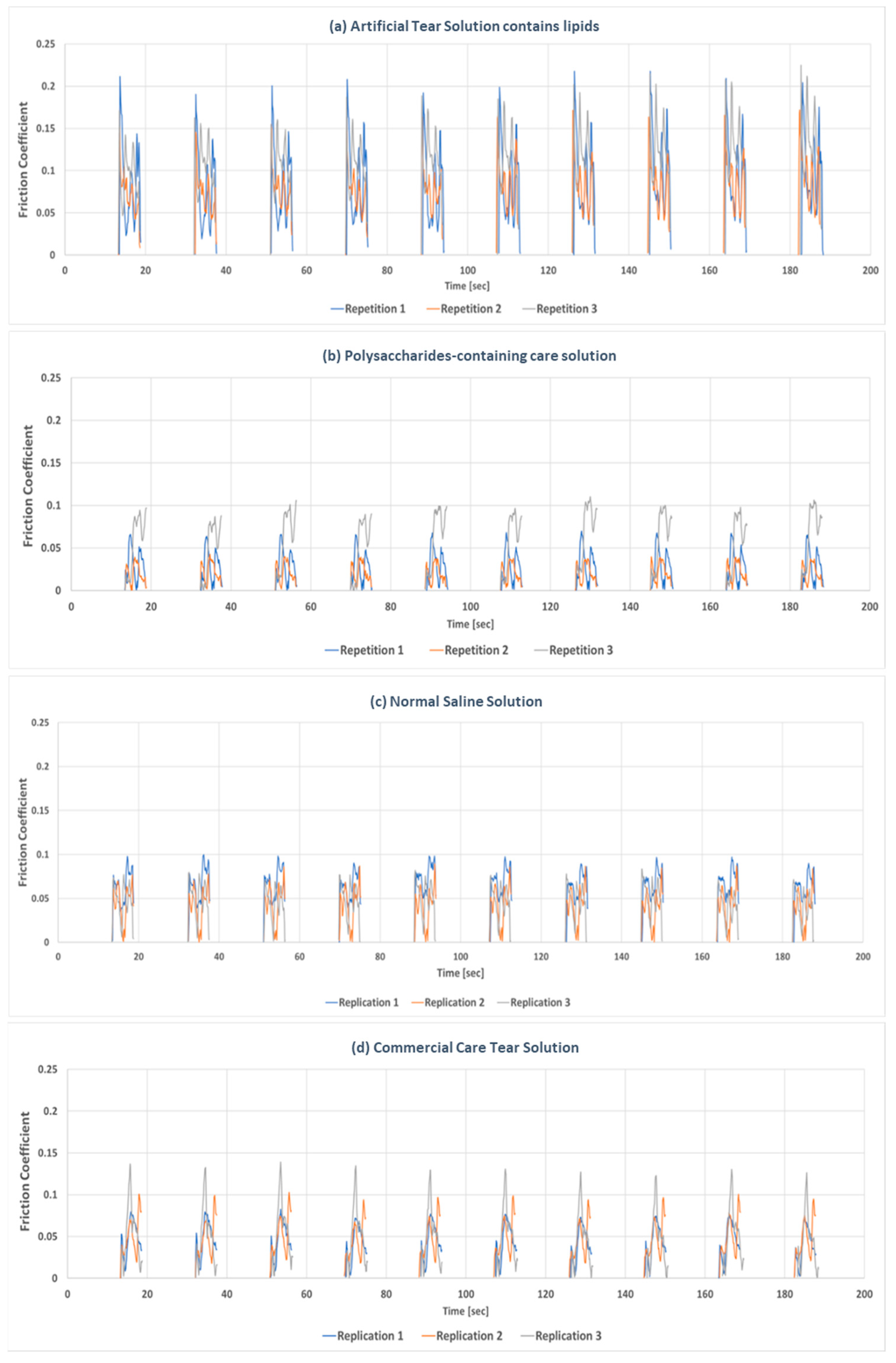
3.1. Comparison of Tribological Properties of Each Lubricant During Whole Friction Cycles
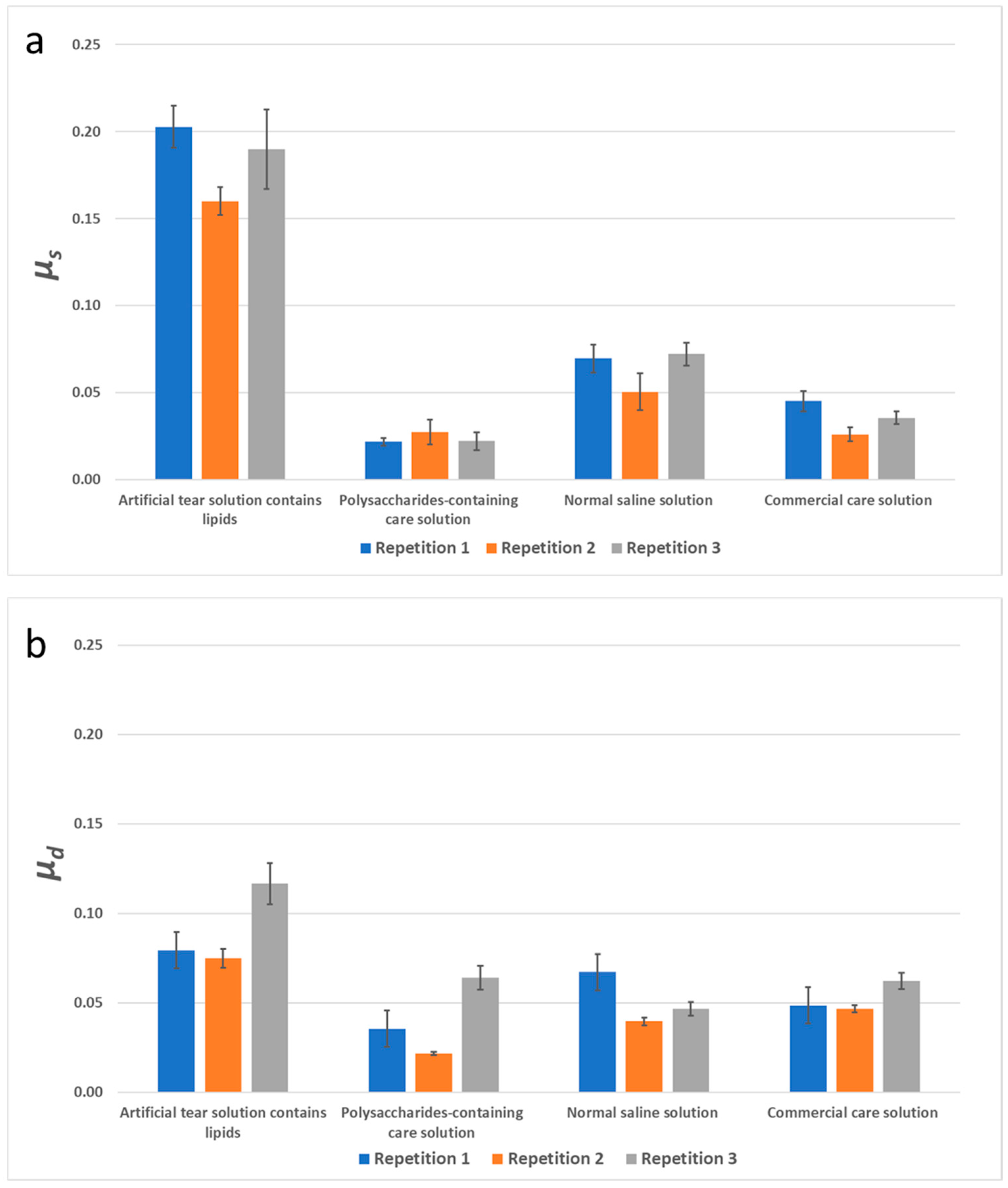
3.2. The Static and Dynamic Friction of Different Solutions
4. Conclusions
- Among the three counterface materials (gelatin, glass, and PVS), gelatin was the best candidate to simulate mechanical and tribological properties of biological tissues such as the cornea and eyelid.
- A very good reproducibility of frictional behavior was obtained with successive friction cycle repetitions when the tests were conducted with a given lubricant under the same operational conditions and on the same location on the gelatin counterface.
- The slight difference in frictional behavior at the different gelatin counterface locations is likely due to the different topography; such variations are expected between one given location and another on a gelatin surface.
- The adopted experimental methodology based on biaxial tribometer testing was suitable for the evaluation and comparison of lubrication capacity of lubricant used in contact lenses.
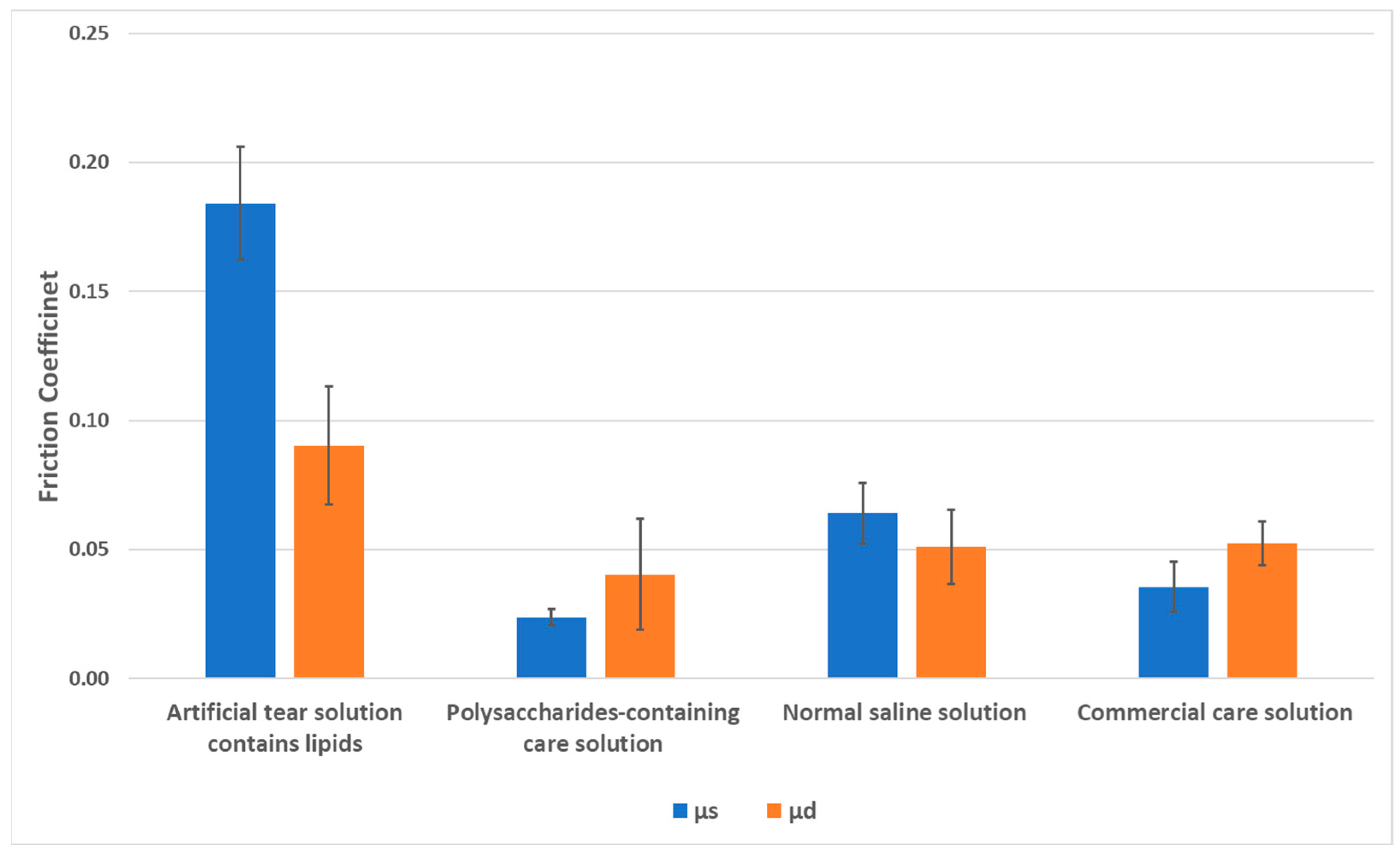
- Distinct outcomes were observed for the solutions. Higher static and dynamic coefficients of friction were obtained with the artificial tear solution, and the averaged static friction coefficient of artificial tear solution was twice as high as its averaged dynamic friction coefficient.
- Lower friction values were obtained with the polysaccharide-containing care solution, but the averaged static friction coefficient was lower than its averaged dynamic friction coefficient, which might result from its high hydrophilicity and lubricating properties.
Author Contributions
Funding
Data Availability Statement
Conflicts of Interest
References
- Sankaridurg, P.; Tahhan, N.; Kandel, H.; Naduvilath, T.; Zou, H.; Frick, K.D.; Marmamula, S.; Friedman, D.S.; Lamoureux, E.; Keeffe, J.; et al. Imi impact of myopia. Investig. Ophthalmol. Vis. Sci. 2021, 62, 2. [Google Scholar] [CrossRef] [PubMed]
- Holden, B.A.; Fricke, T.R.; Wilson, D.A.; Jong, M.; Naidoo, K.S.; Sankaridurg, P.; Wong, T.Y.; Naduvilath, T.J.; Resnikoff, S. Global prevalence of myopia and high myopia and temporal trends from 2000 through 2050. Ophthalmology 2016, 123, 1036–1042. [Google Scholar] [CrossRef]
- Gwiazda, J. Treatment options for myopia. Optom. Vis. Sci. 2009, 86, 624–628. [Google Scholar] [CrossRef]
- Ezinne, N.E.; Bhattarai, D.; Ekemiri, K.K.; Harbajan, G.N.; Crooks, A.C.; Mashige, K.P.; Ilechie, A.A.; Zeried, F.M.; Osuagwu, U.L. Demographic profiles of contact lens wearers and their association with lens wear characteristics in trinidad and tobago: A retrospective study. PLoS ONE 2022, 17, e0264659. [Google Scholar] [CrossRef]
- Bullimore, M.A.; Johnson, L.A. Overnight orthokeratology. Contact Lens Anterior Eye 2020, 43, 322–332. [Google Scholar] [CrossRef]
- Jones, L.; Brennan, N.A.; Gonzalez-Meijome, J.; Lally, J.; Maldonado-Codina, C.; Schmidt, T.A.; Subbaraman, L.; Young, G.; Nichols, J.J. The tfos international workshop on contact lens discomfort: Report of the contact lens materials, design, and care subcommittee. Investig. Ophthalmol. Vis. Sci. 2013, 54, TFOS37-70. [Google Scholar] [CrossRef] [PubMed]
- Roba, M.; Duncan, E.G.; Hill, G.A.; Spencer, N.D.; Tosatti, S.G.P. Friction measurements on contact lenses in their operating environment. Tribol. Lett. 2011, 44, 387–397. [Google Scholar] [CrossRef]
- Pult, H.; Tosatti, S.G.; Spencer, N.D.; Asfour, J.M.; Ebenhoch, M.; Murphy, P.J. Spontaneous blinking from a tribological viewpoint. Ocul. Surf. 2015, 13, 236–249. [Google Scholar] [CrossRef]
- Sterner, O.; Aeschlimann, R.; Zurcher, S.; Osborn Lorenz, K.; Kakkassery, J.; Spencer, N.D.; Tosatti, S.G. Friction measurements on contact lenses in a physiologically relevant environment: Effect of testing conditions on friction. Investig. Ophthalmol. Vis. Sci. 2016, 57, 5383–5392. [Google Scholar] [CrossRef]
- Su, C.Y.; Lai, C.C.; Yeh, L.K.; Li, K.Y.; Shih, B.W.; Tseng, C.L.; Fang, H.W. The characteristics of a preservative-free contact lens care solution on lysozyme adsorption and interfacial friction behavior. Colloids Surf. B Biointerfaces 2018, 171, 538–543. [Google Scholar] [CrossRef]
- Su, C.Y.; Yeh, L.K.; Fan, T.W.; Lai, C.C.; Fang, H.W. Albumin acts as a lubricant on the surface of hydrogel and silicone hydrogel contact lenses. Polymers 2021, 13, 2051. [Google Scholar] [CrossRef] [PubMed]
- Chirila, T.V.; Constable, I.J.; Crawford, G.J.; Vijayasekaran, S.; Thompson, D.E.; Chen, Y.C.; Fletcher, W.A.; Griffin, B.J. Poly(2-hydroxyethyl methacrylate) sponges as implant materials: In vivo and in vitro evaluation of cellular invasion. Biomaterials 1993, 14, 26–38. [Google Scholar] [CrossRef] [PubMed]
- Garrett, Q.; Laycock, B.; Garrett, R.W. Hydrogel lens monomer constituents modulate protein sorption. Investig. Ophthalmol. Vis. Sci. 2000, 41, 1687–1695. [Google Scholar]
- Luensmann, D.; Jones, L. Albumin adsorption to contact lens materials: A review. Contact Lens Anterior Eye 2008, 31, 179–187. [Google Scholar] [CrossRef]
- Vadgama, P. Surfaces and Interfaces for Biomaterials; CRC Press/Woodhead: Boca Ration, FL, USA, 2005. [Google Scholar]
- Chang, Y.C.; Su, C.Y.; Chang, C.H.; Fang, H.W.; Wei, Y. Correlation between tribological properties and the quantified structural changes of lysozyme on poly (2-hydroxyethyl methacrylate) contact lens. Polymers 2020, 12, 1639. [Google Scholar] [CrossRef]
- Efron, N.; Morgan, P.B. Soft contact lens care regimens in the uk. Contact Lens Anterior Eye 2008, 31, 283–284. [Google Scholar] [CrossRef]
- Fahmy, M.; Long, B.; Giles, T.; Wang, C.H. Comfort-enhanced daily disposable contact lens reduces symptoms among weekly/monthly wear patients. Eye Contact Lens 2010, 36, 215–219. [Google Scholar] [CrossRef]
- Hoteling, A.J.; Nichols, W.F.; Harmon, P.S.; Conlon, S.M.; Nunez, I.M.; Hoff, J.W.; Cabarcos, O.M.; Steffen, R.B.; Hook, D.J. Characterization and quantitation of pvp content in a silicone hydrogel contact lens produced by dual-phase polymerization processing. J. Biomed. Mater. Res. B Appl. Biomater. 2018, 106, 1064–1072. [Google Scholar] [CrossRef] [PubMed]
- Bontempo, A.R.; Rapp, J. Protein-lipid interaction on the surface of a rigid gas-permeable contact lens in vitro. Curr. Eye Res. 1997, 16, 1258–1262. [Google Scholar] [CrossRef]
- Su, C.Y.; Yeh, L.K.; Tsao, Y.F.; Lin, W.P.; Hou, C.H.; Huang, H.F.; Lai, C.C.; Fang, H.W. The effect of different cleaning methods on protein deposition and optical characteristics of orthokeratology lenses. Polymers 2021, 13, 4318. [Google Scholar] [CrossRef]
- Sindt, C.W. Hydra-peg: A novel custom contact lens coating technology designed to improve patient comfort and satisfaction. In Whitepaper; Tangible Science LLC: Redwood City, CA, USA, 2016. [Google Scholar]
- Wu, L.Y.; Lin, W.P.; Wu, R.; White, L.; Abass, A. Fea-based stress-strain barometers as forecasters for corneal refractive power change in orthokeratology. Bioengineering 2024, 11, 166. [Google Scholar] [CrossRef] [PubMed]
- Ngai, V.; Medley, J.; Jones, L.; Forrest, J.; Teichroeb, J. Friction of Contact Lenses: Silicone Hydrogel Versus Conventional Hydrogel; Elsevier: Amsterdam, The Netherlands, 2005; Volume 48, pp. 371–379. [Google Scholar]
- Rennie, A.C.; Dickrell, P.L.; Sawyer, W.G. Friction coefficient of soft contact lenses: Measurements and modeling. Tribol. Lett. 2005, 18, 499–504. [Google Scholar] [CrossRef]
- Amornvit, P.; Rokaya, D.; Shrestha, B.; Srithavaj, T. Prosthetic rehabilitation of an ocular defect with post-enucleation socket syndrome: A case report. Saudi Dent. J. 2014, 26, 29–32. [Google Scholar] [CrossRef]
- Rose, J.B.; Pacelli, S.; Haj, A.J.E.; Dua, H.S.; Hopkinson, A.; White, L.J.; Rose, F. Gelatin-based materials in ocular tissue engineering. Materials 2014, 7, 3106–3135. [Google Scholar] [CrossRef] [PubMed]
- Baumberger, T.; Caroli, C.; Ronsin, O. Self-healing slip pulses and the friction of gelatin gels. Eur. Phys. J. E Soft Matter 2003, 11, 85–93. [Google Scholar] [CrossRef]
- Omali, N.B.; Subbaraman, L.N.; Heynen, M.; Ng, A.; Coles-Brennan, C.; Fadli, Z.; Jones, L. Surface versus bulk activity of lysozyme deposited on hydrogel contact lens materials in vitro. Contact Lens Anterior Eye 2018, 41, 329–334. [Google Scholar] [CrossRef] [PubMed]
- Lorentz, H.; Heynen, M.; Kay, L.M.; Dominici, C.Y.; Khan, W.; Ng, W.W.; Jones, L. Contact lens physical properties and lipid deposition in a novel characterized artificial tear solution. Mol. Vis. 2011, 17, 3392–3405. [Google Scholar]
- Choy, C.K.; Cho, P.; Benzie, I.F.; Ng, V. Effect of one overnight wear of orthokeratology lenses on tear composition. Optom. Vis. Sci. 2004, 81, 414–420. [Google Scholar] [CrossRef]
- Sack, R.A.; Tan, K.O.; Tan, A. Diurnal tear cycle: Evidence for a nocturnal inflammatory constitutive tear fluid. Investig. Ophthalmol. Vis. Sci. 1992, 33, 626–640. [Google Scholar]
- Brdler, D.; Goltsberg, R.; Ammar, A.A.; Kasem, H. Experimental study of adhesion, friction, and peeling of biomimetic combined micro-mushroom and micro-spatulae textures. Tribol. Int. 2023, 186, 108609. [Google Scholar] [CrossRef]
- Tiffany, J.M. The viscosity of human tears. Int. Ophthalmol. 1991, 15, 371–376. [Google Scholar] [CrossRef] [PubMed]
- Robinson, J.W.; Zhou, Y.; Bhattacharya, P.; Erck, R.; Qu, J.; Bays, J.T.; Cosimbescu, L. Probing the molecular design of hyper-branched aryl polyesters towards lubricant applications. Sci. Rep. 2016, 6, 18624. [Google Scholar] [CrossRef] [PubMed]
- Rhein-Knudsen, N.; Ale, M.T.; Meyer, A.S. Seaweed hydrocolloid production: An update on enzyme assisted extraction and modification technologies. Mar. Drugs 2015, 13, 3340–3359. [Google Scholar] [CrossRef]
- Ko, N.Y.; Lee, K.M.; Lee, H.M. The effect of wettability and protein adsorption of contact lens by alginic acid. J. Korean Chem. Soc. 2017, 61, 352–388. [Google Scholar]
- Park, H.J.; Lee, H.M. Effect of temperature on physical properties in the manufacture of porous contact lenses using natural polysaccharides. J. Korean Ophthalmic Opt. Soc. 2022, 27, 15–21. [Google Scholar] [CrossRef]
- Kozbial, A.; Li, L. Study on the friction of kappa-carrageenan hydrogels in air and aqueous environments. Mater. Sci. Eng. C Mater. Biol. Appl. 2014, 36, 173–179. [Google Scholar] [CrossRef]
- Kruk, K.; Szekalska, M.; Basa, A.; Winnicka, K. The impact of hypromellose on pharmaceutical properties of alginate microparticles as novel drug carriers for posaconazole. Int. J. Mol. Sci. 2023, 24, 10793. [Google Scholar] [CrossRef]
- Garrett, Q.; Garrett, R.W.; Milthorpe, B.K. Lysozyme sorption in hydrogel contact lenses. Investig. Ophthalmol. Vis. Sci. 1999, 40, 897–903. [Google Scholar]
- Garrett, Q.; Griesser, H.J.; Milthorpe, B.K.; Garrett, R.W. Irreversible adsorption of human serum albumin to hydrogel contact lenses: A study using electron spin resonance spectroscopy. Biomaterials 1999, 20, 1345–1356. [Google Scholar] [CrossRef]
- Su, C.Y.; Yeh, L.K.; Huang, P.H.; Lin, W.P.; Huang, H.F.; Lai, C.C.; Fang, H.W. Long-term effects of tear film component deposition on the surface and optical properties of two different orthokeratology lenses. Contact Lens Anterior Eye 2023, 46, 101852. [Google Scholar] [CrossRef]
- Morrison, S.; Sullivan, D.A.; Sullivan, B.D.; Sheardown, H.; Schmidt, T.A. Dose-dependent and synergistic effects of proteoglycan 4 on boundary lubrication at a human cornea-polydimethylsiloxane biointerface. Eye Contact Lens 2012, 38, 27–35. [Google Scholar] [CrossRef] [PubMed]
- Dunn, A.C.; Tichy, J.A.; Uruena, J.M.; Sawyer, W.G. Lubrication regimes in contact lens wear during a blink. Tribol. Int. 2013, 63, 45–50. [Google Scholar] [CrossRef]
| Group | Artificial Tear Solution | Polysaccharide-Containing Care Solution | Normal Saline Solution | Commercial Care Solution |
|---|---|---|---|---|
| Viscosity (mPa·s) at 19.2 1/s | 0.97 ± 0.00 | 2.26 ± 1.12 | 0.97 ± 0.00 | 1.29 ± 0.56 |
| Viscosity (mPa·s) at 76.8 1/s | 0.89 ± 0.28 ** | 2.26 ± 0.37 | 0.24 ± 0.00 ** | 2.51 ± 0.37 |
| Viscosity (mPa·s) at 192 1/s | 1.15 ± 0.16 *** | 2.91 ± 0.00 *** | 1.26 ± 0.06 *** | 7.08 ± 0.09 |
| pH value | 7.40 ± 0.02 | 7.40 ± 0.01 | 5.82 ± 0.26 ** | 7.03 ± 0.21 |
| Surface tension (mN/m) | 43.23 ± 0.55 * | 41.71 ± 0.45 ** | 73.00 ± 1.00 *** | 44.47 ± 0.22 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Su, C.-Y.; Fang, H.-W.; Nimatallah, M.; Qatmera, Z.; Kasem, H. Experimental Evaluation of the Tribological Properties of Rigid Gas-Permeable Contact Lens Under Different Lubricants. Lubricants 2025, 13, 256. https://doi.org/10.3390/lubricants13060256
Su C-Y, Fang H-W, Nimatallah M, Qatmera Z, Kasem H. Experimental Evaluation of the Tribological Properties of Rigid Gas-Permeable Contact Lens Under Different Lubricants. Lubricants. 2025; 13(6):256. https://doi.org/10.3390/lubricants13060256
Chicago/Turabian StyleSu, Chen-Ying, Hsu-Wei Fang, Mousa Nimatallah, Zain Qatmera, and Haytam Kasem. 2025. "Experimental Evaluation of the Tribological Properties of Rigid Gas-Permeable Contact Lens Under Different Lubricants" Lubricants 13, no. 6: 256. https://doi.org/10.3390/lubricants13060256
APA StyleSu, C.-Y., Fang, H.-W., Nimatallah, M., Qatmera, Z., & Kasem, H. (2025). Experimental Evaluation of the Tribological Properties of Rigid Gas-Permeable Contact Lens Under Different Lubricants. Lubricants, 13(6), 256. https://doi.org/10.3390/lubricants13060256






