Assessment of Oral Health-Related Quality of Life in Children with Leukemia and Gingival Inflammation
Abstract
1. Introduction
2. Materials and Methods
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| OHRQoL | Oral health-related quality of life |
| ECOHIS | Early Childhood Oral Health Impact Scale |
| COHIP | Child Oral Health Impact Profile |
| CPQ | Child Perceptions Questionnaire |
| POQL | Pediatric Oral Health-related Quality of Life Questionnaire |
| Child-OIDP | Child—Oral Impact on Daily Performance |
| OHI-S | Oral Hygiene Index—Simplified |
| GI | Gingival Index |
References
- Sischo, L.; Broder, H. Oral Health-related Quality of Life. What, Why, How, and Future Implications. J. Dent. Res. 2011, 90, 1264–1270. [Google Scholar] [CrossRef] [PubMed]
- Locker, D.; Jokovic, A.; Tompson, B. Health-related quality of life of children aged 11 to 14 years with orofacial conditions. Cleft Palate Craniofac. J. 2005, 42, 260–266. [Google Scholar] [CrossRef]
- Alwattban, R.R.; Alkhudhayr, L.S.; Al-Haj Ali, S.N.; Farah, R.I. Oral Health-Related Quality-of-Life According to Dental Caries Severity, Body Mass Index and Sociodemographic Indicators in Children with Special Health Care Needs. J. Clin. Med. 2021, 10, 4811. [Google Scholar] [CrossRef]
- João, P.; Canta, A.C.; Mendes, S. Oral Health-Related Quality of Life, Behaviours and Oral Manifestations in a Paediatric Population with Type I Diabetes Mellitus: A Comparative Cross-Sectional Study. Dent. J. 2025, 13, 425. [Google Scholar] [CrossRef]
- Gavrila, L.M.; Savin, C.; Sirghe, A.; Serban, V.; Mihalas, E.; Adumitroaie, A.; Gamen, A.; Vacariu, S.; Toma, V. Assessing the effects of dental caries on children’s daily activities from the parents’ perspective. Rom. J. Oral Rehabil. 2025, 17, 427–433. [Google Scholar] [CrossRef]
- Mihalaş, E.; Bălan, A.; Marciuc, D.; Gavrilă, L.; Petcu, A.; Savin, C. Child oral health-related quality of life: Cross-cultural adaptation of Child Perception Questionnaire (CPQ8-10) in Romania. Int. J. Med. Dent. 2018, 22, 368–376. [Google Scholar]
- Culler, C.S.; Gunarajasingam, D.; Henshaw, M.M. Preschool oral health-related quality of life: A practical guide to measurement tools. J. Public Health Dent. 2021, 81, 29–41. [Google Scholar] [CrossRef]
- Curto, A.; Egido, B.; Gómez-Polo, C.; Restrepo-Colorado, K.V.; Garcovich, D.; Franco-Varas, V.; Flores-Fraile, J. Relationship Between the Oral Health-Related Quality of Life (OHRQoL) of Mothers and That of Their Adolescent Children: A Retrospective Pilot Study. Children 2025, 12, 1691. [Google Scholar] [CrossRef]
- Genderson, M.; Sischo, L.; Markowitz, K.; Fine, D.; Broder, H. An overview of children’s oral health-related quality of life assessment: From scale development to measuring outcomes. Caries Res. 2013, 47, 13–21. [Google Scholar] [CrossRef]
- Chai, H.H.; Gao, S.S.; Chen, K.J.; Lo, E.C.M.; Duangthip, D.; Chu, C.H. Tools Evaluating Child Oral Health–Related Quality of Life. Int. Dent. J. 2024, 74, 15–24. [Google Scholar] [CrossRef] [PubMed]
- Buldur, B.; Güvendi, O. Conceptual modelling of the factors affecting oral health-related quality of life in children: A path analysis. Int. J. Paediatr. Dent. 2020, 30, 181–192. [Google Scholar] [CrossRef] [PubMed]
- Silva, B.; Campos, L.; Marôco, J.; Campos, J. The Early Childhood Oral Health Impact Scale (ECOHIS): Psychometric properties and application on preschoolers. PeerJ 2023, 11, e16035. [Google Scholar] [CrossRef] [PubMed]
- Lembacher, S.; Hofer, V.; Bekes, K. The Impact of Dental Pain on the Oral Health-Related Quality of Life (OHRQoL) of Preschool Children in Austria. J. Clin. Med. 2023, 12, 5906. [Google Scholar] [CrossRef] [PubMed]
- Alvarez-Azaustre, M.P.; Greco, R.; Llena, C. Oral Health-Related Quality of Life in Adolescents as Measured with the Child-OIDP Questionnaire: A Systematic Review. Int. J. Environ. Res. Public Health 2021, 18, 12995. [Google Scholar] [CrossRef]
- Dhawan, P.; Singh, A.; Agarwal, A.; Aeran, H. Psychometric properties of Hindi version of child oral impact on daily performances (C-OIDP) index amongst school children in North India. J. Oral Biol. Craniofacial Res. 2019, 9, 10–13. [Google Scholar] [CrossRef]
- Ribas-Perez, D.; Muñoz-Viveros, C.; Formoso-Veloso, A.; Carrillo-Sanchez, F.; El Khoury-Moreno, L.; Torrejon-Martinez, J.; Castaño-Seiquer, A. Oral Health-Related Quality of Life in a Paediatric Population in the Dominican Republic. J. Clin. Med. 2024, 13, 2449. [Google Scholar] [CrossRef]
- Huntington, N.; Spetter, D.; Jones, J.; Rich, S.; Garcia, R.; Spiro, A. Development and validation of a measure of pediatric oral health-related quality of life: The POQL. J. Public Health Dent. 2011, 71, 185–193. [Google Scholar] [CrossRef]
- Braun, P.A.; Lind, K.E.; Henderson, W.G.; Brega, A.G.; Quissell, D.O.; Albino, J. Validation of a pediatric oral health-related quality of life scale in Navajo children. Qual. Life Res. 2015, 24, 231–239. [Google Scholar] [CrossRef]
- Angst, P.; Maier, J.; Dos Santos Nogueira, R.; Manso, I.; Tedesco, T. Oral health status of patients with leukemia: A systematic review with meta-analysis. Arch. Oral Biol. 2020, 120, 104948. [Google Scholar] [CrossRef]
- Ripardo, A.C.G.; Queiroz, A.C.D.; Herkrath, A.P.C.d.Q.; Herkrath, F.J.; Rebelo Vieira, J.M.; Pereira, J.V.; Rebelo, M.A.B.; Vettore, M.V. The Association Between Periodontal Status, Oral Health-Related Quality of Life and Self-Rated Oral Health in Socially Underprivileged Adolescents. Community Dent. Oral Epidemiol. 2025, 53, 278–285. [Google Scholar] [CrossRef]
- Moral de la Rubia, J.; Franco, N. Validation of the Oral Health Impact Profile applied to patients with periodontal disease. Rev. Fac. Odontol. Univ. Nac. 2017, 29, 148–172. [Google Scholar] [CrossRef]
- He, S.; Wang, J.; Wei, S.; Ji, P. Development and validation of a condition-specific measure for chronic periodontitis: Oral Health Impact Profile for chronic periodontitis. J. Clin. Periodontol. 2017, 44, 591–600. [Google Scholar] [CrossRef]
- Quiroz, V.; Reinero, D.; Hernandez, P.; Contreras, J.; Vernal, R.; Carvajal, P. Development of a self-report questionnaire designed for population based surveillance of gingivitis in adolescents: Assessment of content validity and reliability. J. Appl. Oral. Sci. 2017, 25, 404–411. [Google Scholar] [CrossRef][Green Version]
- Broomhead, T.; Gibson, B.; Parkinson, C.; Robinson, P.; Vettore, M.; Baker, S. Development and psychometric validation of the gum health experience questionnaire. J. Clin. Periodontol. 2023, 51, 33–42. [Google Scholar] [CrossRef]
- Slowik, J.; Panasiuk, A.; Kaczor, M.; Wnuk, M. Oral health-related quality of life in patients with periodontitis: A systematic review and meta-analysis. Front. Oral Health 2025, 6, 1503829. [Google Scholar] [CrossRef]
- Agnese, C.C.D.; Schöffer, C.; Kantorski, K.Z.; Zanatta, F.B.; Susin, C.; Antoniazzi, R.P. Periodontitis and Oral Health-Related Quality of Life: A Systematic Review and Meta-Analysis. J. Clin. Periodontol. 2025, 52, 408–420. [Google Scholar] [CrossRef] [PubMed]
- Taştan Eroğlu, Z.; Yıldız, K.; Uçan Yarkaç, F.; Özkan Şen, D.; Babayiğit, O. Assessment of self-reported symptoms and oral health-related quality of life in patients requiring periodontal treatment. Int. Dent. Res. 2024, 14, 36–44. [Google Scholar] [CrossRef]
- Lazureanu, P.C.; Popescu, F.G.; Stef, L.; Focsa, M.; Vaida, M.A.; Mihaila, R. The Influence of Periodontal Disease on Oral Health Quality of Life in Patients with Cardiovascular Disease: A Cross-Sectional Observational Single-Center Study. Medicina 2022, 58, 584. [Google Scholar] [CrossRef] [PubMed]
- Fuller, J.; Donos, N.; Suvan, J.; Tsakos, G.; Nibali, L. Association of oral health-related quality of life measures with aggressive and chronic periodontitis. J. Periodontal Res. 2020, 55, 574–580. [Google Scholar] [CrossRef]
- Al-Bitar, K.; Garcia, J.; Han, S.; Guentsch, A. Association between periodontal health status and quality of life: A cross-sectional study. Front. Oral Health 2024, 5, 1346814. [Google Scholar] [CrossRef]
- Greeshma Sivadas, T.; Bindu, R. Assessment of oral health related quality of life (OHRQL) in patients with periodontitis: A cross sectional survey. IP Int. J. Periodontol. Implantol. 2021, 6, 212–221. [Google Scholar] [CrossRef]
- Collins, J.; Elias, A.; Brache, M.; Veras, K.; Ogando, G.; Toro, M.; Rivas-Tumanyan, S.; Rajendra, A. Association between gingival parameters and Oral health–related quality of life in Caribbean adults: A population-based cross-sectional study. BMC Oral Health 2019, 19, 234. [Google Scholar] [CrossRef]
- Al-Sharqi, A.J.B.; Abdulkareem, A.A.; Gul, S.; Rawlinson, A. Impact of Nonsurgical Periodontal Treatment of Periodontitis Stages 2 and 3 on Oral Health-Related Quality of Life. Healthcare 2024, 12, 1430. [Google Scholar] [CrossRef]
- Theodoridis, C.; Violesti, A.; Nikiforidou, M.; Menexes, G.C.; Vouros, I.D. Short-Term Impact of Non-Surgical and Surgical Periodontal Therapy on Oral Health-Related Quality of Life in a Greek Population—A Prospective Cohort Study. Dent. J. 2020, 8, 54. [Google Scholar] [CrossRef]
- Vivek, B.; Ramesh, K.; Gautami, P.; Sruthima, G.; Dwarakanath, C.; Anudeep, M. Effect of periodontal treatment on oral health-related quality of life—A randomised controlled trial. J. Taibah Univ. Med. Sci. 2021, 16, 856–863. [Google Scholar] [CrossRef]
- Dumitrache, M.; Comes, C.; Teodorescu, E.; Dumitrașcu, L.; Cuculescu, M.; Ionescu, E. Calitatea vieții asociată cu sănătatea orală la elevii din București. Rev. Română Bioetică 2009, 7, 68–77. [Google Scholar]
- Singh, O.; Reddy, V.; Sharma, L.; Pradhan, D.; Srivastava, R. Association of gingivitis with children oral health-related quality of life in Lucknow: A cross-sectional study. J. Fam. Med. Prim. Care 2020, 9, 1177–1181. [Google Scholar]
- Ortiz, F.; Sfreddo, C.; Coradini, A.; Fagundes, M.; Ardenghi, T. Gingivitis influences oral health-related quality of life in adolescents: Findings from a cohort study. Rev. Bras. Epidemiol. 2020, 23, e200051. [Google Scholar] [CrossRef] [PubMed]
- Kaewkamnerdpong, I.; Urwannachotima, N.; Prasertsom, P.; Charoenruk, N.; Krisdapong, S. Impact of oral diseases on 12- and 15-year-old children’s quality of life: Condition-specific oral health related quality of life analysis. BMC Oral Health 2023, 23, 722. [Google Scholar] [CrossRef] [PubMed]
- Saber, F.; Al Sayed, M.; Omar, O. Correlation between Gingival Redness and Oral Health Related Quality of Life in A Group of Egyptian Children at New Giza University. Future Dent. J. 2024, 9, 133–137. [Google Scholar] [CrossRef]
- Farsi, N.; El-Housseiny, A.; Farsi, D.; Farsi, N. Validation of the Arabic version of the Early Childhood Oral Health Impact Scale (ECOHIS). BMC Oral Health 2017, 17, 60. [Google Scholar] [CrossRef]
- Nasu, D.; Uematsu, A.; Nakamura, S.; Ishiyama, M.; Shirakawa, T.; Hasegawa, T.; Nasu, Y.; Kaneko, T.; Hoshi, J.; Horie, N. Oral hygiene and oral status of institutionalized children with motor and intellectual disabilities. J. Oral Sci. 2020, 62, 89–92. [Google Scholar] [CrossRef]
- da Silva, P.; Barbosa, T.; Amato, J.; Montes, A.; Gavião, M. Gingivitis, Psychological Factors and Quality of Life in Children. Oral Health Prev. Dent. 2015, 13, 227–235. [Google Scholar]
- Balseca-Ibarra, M.; Medina Vega, M.; Souto, M.; Romito, G.; Frias, A.; Raggio, D.; Crosato, E.; Mendes, F.; Pannuti, C. Impact of gingivitis on oral health-related quality of life in 12-year-old schoolchildren of Quito, Ecuador. Eur. Arch. Paediatr. Dent. 2023, 24, 211–218. [Google Scholar] [CrossRef] [PubMed]
- Cammarata-Scalisi, F.; Girardi, K.; Strocchio, L.; Merli, P.; Bernardin, A.G.; Galeotti, A.; Magliarditi, F.; Inserra, A.; Callea, M. Oral Manifestations and Complications in Childhood Acute Myeloid Leukemia. Cancers 2020, 12, 1634. [Google Scholar] [CrossRef] [PubMed]
- Mathur, V.; Dhillon, J.; Kalra, G. Oral health in children with leukemia. Indian J. Palliat. Care 2012, 18, 12–18. [Google Scholar] [CrossRef] [PubMed]
- Angst, P.; Dutra, D.; Manso, I.; Moreira, C.; Kantorski, K. Association between oral health-related quality of life and periodontal status in patients with leukemia. Int. Dent. J. 2020, 70, 381–387. [Google Scholar] [CrossRef]
- Stolze, J.; Raber-Durlacher, J.E.; Loonen, J.J.; Teepen, J.C.; Ronckers, C.M.; Tissing, W.J.E.; de Vries, A.C.H.; Neggers, S.J.C.M.M.; Dulmen-den Broeder, E.; Heuvel-Eibrink, M.M.; et al. Self-reported outcomes on oral health and oral health-related quality of life in long-term childhood cancer survivors-A DCCSS-LATER 2 Study. Support. Care Cancer 2023, 31, 344. [Google Scholar] [CrossRef]
- Bensouda, S.; Elgasmi, F.E.; Al Jalil, Z.; Khoubila, N.; Iourdane, H.; Hamza, M.; El Arabi, S. Assessment of oral health-related quality of life among children with acute leukemia. Stomatol. Dis. Sci. 2020, 4, 1. [Google Scholar] [CrossRef]
- Pedrosa, B.R.V.; Martins, W.L.L.; Almeida, H.C.R.; Kozmhinsky, V.M.R.; Sabino, M.F.P.A.; Oliveira, K.M.M. Parents’ knowledge about the oral health care of oncological children. RGO Rev. Gaúch Odontol. 2019, 67, e2019008. [Google Scholar] [CrossRef]
- Alkhuwaiter, S.S. Parents’ Awareness and Oral Health Care Measures of Pediatric Patients Receiving Chemotherapy. J. Pediatr. Dent. 2021, 7, 1–8. [Google Scholar] [CrossRef]
- Alshmaa, Z.M.; Alwaheb, A.M. Impact of Gingivitis on the Quality of Life of Primary School Children 8–10 Year Age Group in Al-Najaf City. Ann. Rom. Soc. Cell Biol. 2021, 25, 319–327. [Google Scholar]
- Hegde, A.M.; Joshi, S.; Rai, K.; Shetty, S. Evaluation of oral hygiene status, salivary characteristics and dental caries experience in acute lymphoblastic leukemic (ALL) children. J. Clin. Pediatr. Dent. 2011, 35, 319–323. [Google Scholar] [CrossRef]
- Velten, D.B.; Zandonade, E.; Monteiro de Barros Miotto, M.H. Prevalence of oral manifestations in children and adolescents with cancer submitted to chemotherapy. BMC Oral Health 2017, 17, 49. [Google Scholar] [CrossRef] [PubMed]
- Kapoor, G.; Goswami, M.; Sharma, S.; Mehta, A.; Dhillon, J.K. Assessment of oral health status of children with Leukemia: A cross-sectional study. Spec. Care Dent. 2019, 39, 564–571. [Google Scholar] [CrossRef] [PubMed]
- Laheij, A.; Dillen, L.M.; Nur, E.; Raber-Durlacher, J.E. Self-perceived oral health in hemato-oncological patients and the relation to quality of life. Support. Care Cancer 2024, 32, 643. [Google Scholar] [CrossRef]
- Pels, E.; Mielnik-Błaszczak, M. Oral hygiene in children suffering from acute lymphoblastic leukemia living in rural and urban regions. Ann. Agric. Environ. Med. 2012, 19, 529–533. [Google Scholar] [PubMed]
- Mogensen, H.; Modig, K.; Tettamanti, G.; Erdmann, F.; Heyman, M.; Feychting, M. Survival after childhood cancer–social inequalities in high-income countries. Front. Oncol. 2018, 8, 485. [Google Scholar] [CrossRef]
- Ali, M.; Nurelhuda, N. Oral health status and its determinants in children with leukaemia at the Radiation and Isotope Center Khartoum, Khartoum State, Sudan. Sudan. J. Paediatr. 2019, 19, 93–100. [Google Scholar] [CrossRef]
- Azher, U.; Shiggaon, N. Oral health status of children with acute lymphoblastic leukemia undergoing chemotherapy. Indian J. Dent. Res. 2013, 24, 523. [Google Scholar] [CrossRef]
- Gupta, A.; Marwaha, M.; Bansal, K.; Sachdeva, A.; Gupta, A. Dental Awareness among Parents and Oral Health of Paediatric Cancer Patients Receiving Chemotherapy. J. Clin. Diagn. Res. JCDR 2016, 10, ZC92–ZC95. [Google Scholar] [CrossRef]
- Mishra, R.; Mathur, V.; Bakhshi, S.; Priya, H.; Ganguly, S.; Bansal, K.; Rahul, M.; Tewari, N.; Sharawat, N. Barriers and facilitators in oral hygiene maintenance in children undergoing chemotherapy for acute lymphoblastic leukemia: A qualitative investigation. Eur. Arch. Paediatr. Dent. 2025. [Google Scholar] [CrossRef] [PubMed]
- Ribeiro, I.; Limeira, R.; Dias de Castro, R.; Ferreti Bonan, P.; Valença, A. Oral mucositis in pediatric patients in treatment for acute lymphoblastic leukemia. Int. J. Environ. Res. Public Health 2017, 14, 1468. [Google Scholar] [CrossRef]
- Galbiati, G.; Giannini, L.; del Rosso, D.; Cagetti, M.G.; Maspero, C. Operative Preventive Oral Hygiene Protocols in Pediatric Patients with Leukemia: A Non-Randomized Clinical Trial. Dent. J. 2025, 13, 164. [Google Scholar] [CrossRef]
- Devi, K.; Allenidekania, A. The Relationship of Oral Care Practice at Home with Mucositis Incidence in Children with Acute Lymphoblastic Leukemia. Compr. Child Adolesc. Nurs. 2019, 42, 56–64. [Google Scholar] [CrossRef]
- Xavier, A.; Hegde, A. Preventive protocols and oral management in childhood leukemia—The pediatric specialist’s role. Asian Pac. J. Cancer Prev. APJCP 2010, 11, 39–43. [Google Scholar]
- American Academy of Pediatric Dentistry Review Council. Guideline on Dental Management of Pediatric Patients Receiving Chemotherapy, Hematopoietic Cell Transplantation, and/or Radiation Therapy. Pediatr. Dent. 2016, 38, 334–342. [Google Scholar]
- Ponce-Torres, E.; Ruíz-Rodríguez, M.D.S.; Alejo-González, F.; Hernández-Sierra, J.F.; Pozos-Guillén, A.J. Oral manifestations in pediatric patients receiving chemotherapy for acute lymphoblastic leukemia. J. Clin. Pediatr. Dent. 2010, 34, 275–279. [Google Scholar] [CrossRef]
- Spielberger, R.; Stiff, P.; Bensinger, W.; Gentile, T.; Weisdorf, D.; Kewalramani, T.; Shea, T.; Yanovich, S.; Hansen, K.; Noga, S.; et al. Palifermin for oral mucositis after intensive therapy for hematologic cancers. N. Engl. J. Med. 2004, 351, 2590–2598. [Google Scholar] [CrossRef] [PubMed]
- Nemes, J.; Jenei, Á.; Márton, I. Oral mucositis as the most common complication of childhood cancer therapy. Review of literature. Orvosi Hetil. 2018, 159, 495–502. [Google Scholar] [CrossRef] [PubMed]
| Subject | Inclusion Criteria | Exclusion Criteria |
|---|---|---|
| Study group | Age < 18 years old Any form of leukemia Any cancer treatment stage No periodontal treatment 6 months prior to the examination | Age > 18 years old Any periodontal treatment 6 months prior to the examination |
| Control group | Age < 18 years old No inflammatory systemic condition No periodontal treatment 6 months prior to the examination |
| Variable | χ2 (df) | p-Value | Control Group n (%) | Study Group n (%) |
|---|---|---|---|---|
| Smile complaints | 17.785 (3) | 0.000 | Never: 29 (58.0) Rarely: 8 (16.0) Quite often: 7 (14.0) Often: 6 (12.0) | Never: 45 (91.8) Rarely: 4 (8.2) Quite often: 0 (0.0) Often: 0 (0.0) |
| Peer difficulties | 5.835 (1) | 0.016 | Never: 42 (84.0) Rarely: 8 (16.0) | Never: 48 (98.0) Rarely: 1 (2.0) |
| Pain | 10.775 (3) | 0.013 | Never: 15 (30.0) Rarely: 23 (46.0) Quite often: 6 (12.0) Often: 6 (12.0) | Never: 25 (51.0) Rarely: 15 (30.6) Quite often: 9 (18.4) Often: 0 (0.0) |
| Sleep disturbances | 26.478 (3) | 0.000 | Never: 24 (48.0) Rarely: 11 (22.0) Quite often: 8 (16.0) Often: 7 (14.0) | Never: 46 (93.9) Rarely: 3 (6.1) Quite often: 0 (0.0) Often: 0 (0.0) |
| Concentration difficulties | 27.720 (3) | 0.000 | Never: 28 (56.0) Rarely: 7 (14.0) Quite often: 7 (14.0) Often: 8 (16.0) | Never: 49 (100.0) Rarely: 0 (0.0) Quite often: 0 (0.0) Often: 0 (0.0) |
| School absenteeism | 27.720 (3) | 0.000 | Never: 28 (56.0) Rarely: 11 (22.0) Quite often: 5 (10.0) Often: 6 (12.0) | Never: 49 (100.0) Rarely: 0 (0.0) Quite often: 0 (0.0) Often: 0 (0.0) |
| Burning sensation | 7.004 (3) | 0.072 * | Never: 25 (50.0) Rarely: 14 (28.0) Quite often: 5 (10.0) Often: 6 (12.0) | Never: 32 (65.3) Rarely: 12 (24.5) Quite often: 5 (10.2) Often: 0 (0.0) |
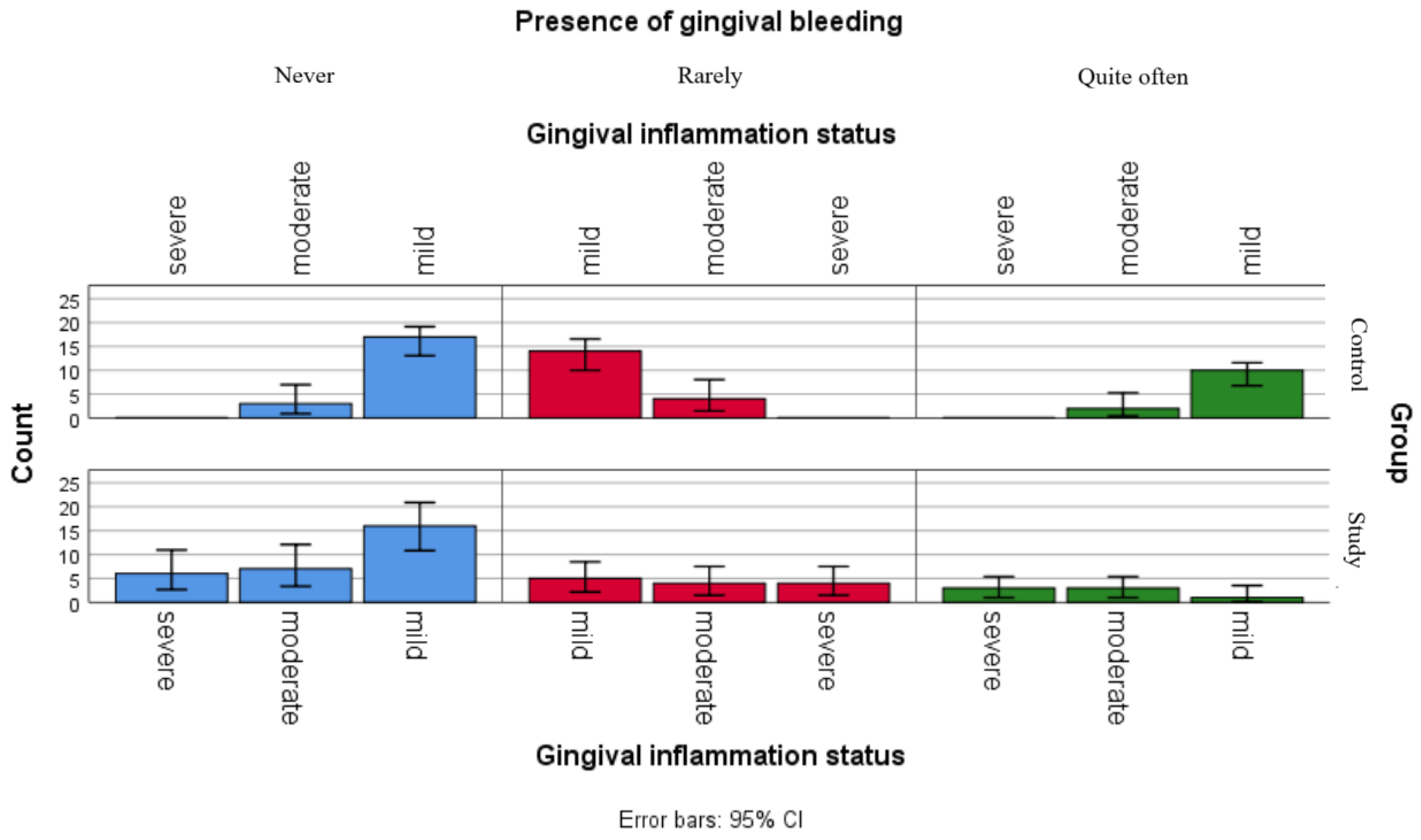
| Gingival bleeding | 3.766 (2) | 0.152 | Never: 20 (40.0) Rarely: 18 (36.0) Quite often: 12 (24.0) | Never: 29 (59.2) Rarely: 13 (26.5) Quite often: 7 (14.3) |
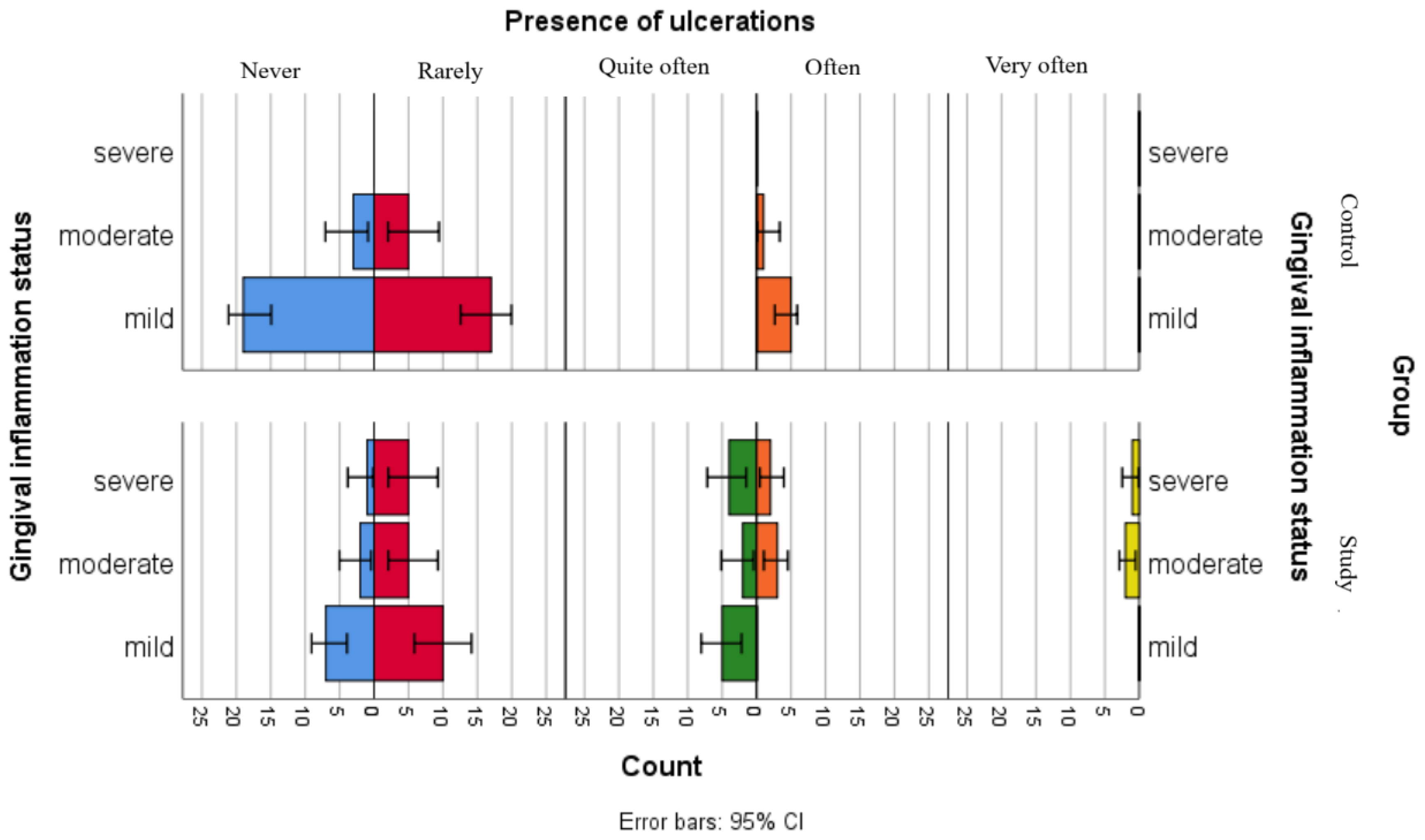
| Ulcerations | 18.678 (4) | 0.001 | Never: 22 (44.0) Rarely: 22 (44.0) Quite often: 0 (0.0) Often: 6 (12.0) Very often: 0 (0.0) | Never: 10 (20.4) Rarely: 20 (40.8) Quite often: 11 (22.5) Often: 5 (10.2) Very often: 3 (6.1) |
| Dry mouth | 5.395 (2) | 0.067 * | Never: 17 (34.0) Rarely: 21 (42.0) Quite often: 12 (24.0) | Never: 28 (57.1) Rarely: 14 (28.6) Quite often: 7 (14.3) |
| Variable | χ2 (df) | p-Value | Category | Control Group n (%) | Study Group n (%) |
|---|---|---|---|---|---|
| Brushing frequency | 0.046 (2) | 0.831 | Never brushes | 6 (12.0) | 5 (11.3) |
| 1/day | 23 (46.0) | 24 (48.9) | |||
| 2/day | 21 (42.0) | 20 (40.8) | |||
| Total valid | 44 (100) | 44 (100) | |||
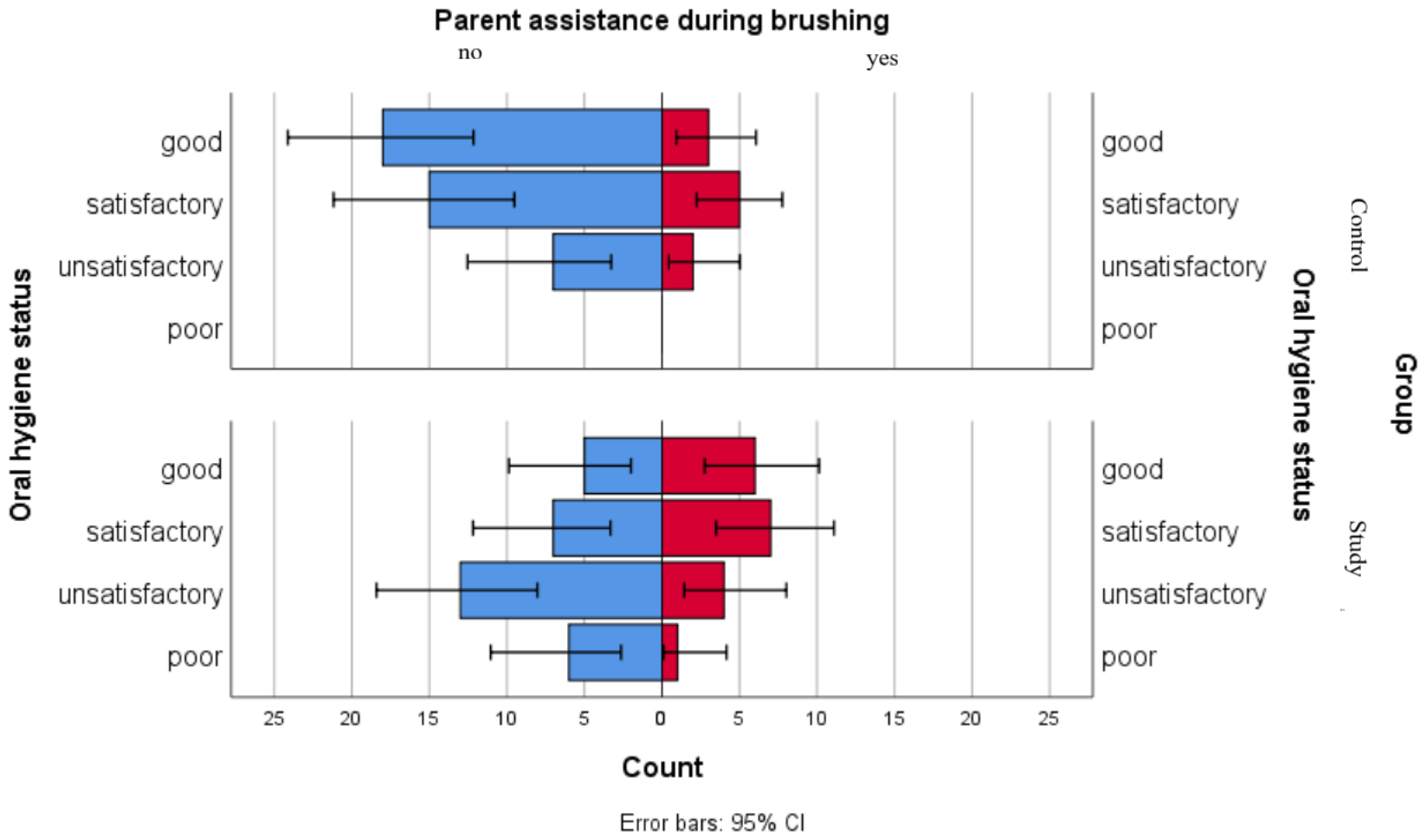
| Parent assistance during brushing | 3.417 (1) | 0.065 * | No | 40 (80.0) | 31 (63.3) |
| Yes | 10 (20.0) | 18 (36.7) | |||
| Total | 50 (100) | 49 (100) | |||
| Brush type | 4.119 (3) | 0.249 | None | 8 (16.0) | 5 (10.2) |
| Manual | 27 (54.0) | 33 (67.3) | |||
| Electric | 8 (16.0) | 9 (18.4) | |||
| Both | 7 (14.0) | 2 (4.1) | |||
| Total | 50 (100) | 49 (100) | |||
| Mouthwash use | 3.198 (2) | 0.202 | No | 24 (48.0) | 32 (65.3) |
| Yes | 14 (28.0) | 8 (16.3) | |||
| Occasionally | 12 (24.0) | 9 (18.4) | |||
| Total | 50 (100) | 49 (100) | |||
| Dental floss use | 3.312 (1) | 0.069 * | No | 38 (76.0) | 44 (89.8) |
| Yes | 12 (24.0) | 5 (10.2) | |||
| Total | 50 (100) | 49 (100) |
| Question | Category | Mild | Moderate | Severe | Total n (%) | χ2 | p-Value |
|---|---|---|---|---|---|---|---|
| Smile complaints | Never | 20 | 13 | 12 | 45 (91.8) | 0.049 | 0.976 |
| Rarely | 2 | 1 | 1 | 4 (8.2) | |||
| Peer difficulties | Never | 22 | 14 | 12 | 48 (98.0) | 2.827 | 0.243 |
| Rarely | 0 | 0 | 1 | 1 (2.0) | |||
| Pain | Never | 13 | 6 | 6 | 25 (51.0) | 1.220 | 0.875 |
| Rarely | 6 | 5 | 4 | 15 (30.6) | |||
| Quite often | 3 | 3 | 3 | 9 (18.4) | |||
| Sleep disturbances | Never | 21 | 14 | 11 | 46 (93.9) | 2.949 | 0.229 |
| Rarely | 1 | 0 | 2 | 3 (6.1) | |||
| Concentration difficulties | Never | 22 | 14 | 13 | 49 (100) | – | – |
| School absenteeism | Never | 22 | 14 | 13 | 49 (100) | – | – |
| Burning sensation | Never | 17 | 8 | 7 | 32 (65.3) | 3.412 | 0.491 |
| Rarely | 3 | 4 | 5 | 12 (24.5) | |||
| Quite often | 2 | 2 | 1 | 5 (10.2) | |||
| Gingival bleeding | Never | 16 | 7 | 6 | 29 (59.2) | 4.149 | 0.386 |
| Rarely | 5 | 4 | 4 | 13 (26.5) | |||
| Quite often | 1 | 3 | 3 | 7 (14.3) | |||
| Ulcerations | Never | 7 | 2 | 1 | 10 (20.4) | 10.969 | 0.203 |
| Rarely | 10 | 5 | 5 | 20 (40.8) | |||
| Quite often | 5 | 2 | 4 | 11 (22.4) | |||
| Often | 0 | 3 | 2 | 5 (10.2) | |||
| Very often | 0 | 2 | 1 | 3 (6.1) | |||
| Dry mouth | Never | 14 | 11 | 3 | 28 (57.1) | 10.852 | 0.028 |
| Rarely | 4 | 3 | 7 | 14 (28.6) | |||
| Quite often | 4 | 0 | 3 | 7 (14.3) |
| Question | Category | Mild | Moderate | Total n (%) | χ2 | p-Value |
|---|---|---|---|---|---|---|
| Smile complaints | Never | 23 | 6 | 29 (58) | 2.798 | 0.424 |
| Rarely | 7 | 1 | 8 (16) | |||
| Quite often | 7 | 0 | 7 (14) | |||
| Often | 4 | 2 | 6 (12) | |||
| Peer difficulties | Never | 36 | 6 | 42 (84) | 2.454 | 0.117 |
| Rarely | 5 | 3 | 8 (16) | |||
| Pain | Never | 13 | 2 | 15 (30) | 2.712 | 0.438 |
| Rarely | 18 | 5 | 23 (46) | |||
| Quite often | 6 | 0 | 6 (12) | |||
| Often | 4 | 2 | 6 (12) | |||
| Sleep disturbances | Never | 21 | 3 | 24 (48) | 3.674 | 0.299 |
| Rarely | 10 | 1 | 11 (22) | |||
| Quite often | 5 | 3 | 8 (16) | |||
| Often | 5 | 2 | 7 (14) | |||
| Concentration difficulties | Never | 24 | 4 | 28 (56) | 1.123 | 0.772 |
| Rarely | 5 | 2 | 7 (14) | |||
| Quite often | 6 | 1 | 7 (14) | |||
| Often | 6 | 2 | 8 (16) | |||
| School absenteeism | Never | 23 | 5 | 28 (56) | 1.746 | 0.627 |
| Rarely | 8 | 3 | 11 (22) | |||
| Quite often | 5 | 0 | 5 (10) | |||
| Often | 5 | 1 | 6 (12) | |||
| Burning sensation | Never | 21 | 4 | 25 (50) | 0.200 | 0.978 |
| Rarely | 11 | 3 | 14 (28) | |||
| Quite often | 4 | 1 | 5 (10) | |||
| Often | 5 | 1 | 6 (12) | |||
| Gingival bleeding | Never | 17 | 3 | 20 (40) | 0.354 | 0.838 |
| Rarely | 14 | 4 | 18 (36) | |||
| Quite often | 10 | 2 | 12 (24) | |||
| Ulcerations | Never | 19 | 3 | 22 (44) | 0.624 | 0.732 |
| Rarely | 17 | 5 | 22 (44) | |||
| Often | 5 | 1 | 6 (12) | |||
| Dry mouth | Never | 15 | 2 | 17 (34) | 2.556 | 0.279 |
| Rarely | 18 | 3 | 21 (42) | |||
| Quite often | 8 | 4 | 12 (24) |
| Question | Category | Poor | Unsatisfactory | Satisfactory | Good | Total n (%) | Pearson Chi-Square | p-Value |
|---|---|---|---|---|---|---|---|---|
| Brushing frequency | Never brushes | 1 | 2 | 1 | 1 | 5 (10.2) | 0.766 | 0.993 |
| 1 | 4 | 8 | 7 | 5 | 24 (48.9) | |||
| 2 | 2 | 7 | 6 | 5 | 20 (40.8) | |||
| Parent assistance during brushing | No | 6 | 13 | 7 | 5 | 31 (63.2) | 5.355 | 0.148 * |
| Yes | 1 | 4 | 7 | 6 | 18 (36.7) | |||
| Brush type | None | 1 | 2 | 1 | 1 | 5 (10.2) | 6.397 | 0.700 |
| Manual | 3 | 10 | 12 | 8 | 33 (67.3) | |||
| Electric | 2 | 4 | 1 | 2 | 9 (18.3) | |||
| Both | 1 | 1 | 0 | 0 | 2 (4.1) | |||
| Mouthwash use | No | 5 | 10 | 11 | 6 | 32 (65.3) | 2.562 | 0.861 |
| Yes | 1 | 3 | 2 | 2 | 8 (16.3) | |||
| Occasionally | 1 | 4 | 1 | 3 | 9 (18.3) | |||
| Dental floss use | No | 6 | 17 | 14 | 7 | 44 (89.7) | 11.865 | 0.008 |
| Yes | 1 | 0 | 0 | 4 | 5 (10.2) |
| Question | Category | Unsatisfactory | Satisfactory | Good | Total n (%) | χ2 | p-Value |
|---|---|---|---|---|---|---|---|
| Brushing frequency | Never brushes | 1 | 5 | 0 | 6 (12) | ||
| 1/day | 6 | 8 | 9 | 23 (46) | 8.598 | 0.072 | |
| 2/day | 2 | 7 | 12 | 21 (42) | |||
| Parent assistance during brushing | No | 7 | 15 | 18 | 40 (80) | 0.769 | 0.681 |
| Yes | 2 | 5 | 3 | 10 (20) | |||
| Brush type | None | 1 | 6 | 1 | 8 (16) | 9.095 | 0.168 |
| Manual | 6 | 7 | 14 | 27 (54) | |||
| Electric | 2 | 4 | 2 | 8 (16) | |||
| Both | 0 | 3 | 4 | 7 (14) | |||
| Mouthwash use | No | 3 | 11 | 10 | 24 (48) | 7.279 | 0.122 |
| Yes | 2 | 3 | 9 | 14 (28) | |||
| Occasionally | 4 | 6 | 2 | 12 (24) | |||
| Dental floss use | No | 7 | 14 | 17 | 38 (72) | 0.693 | 0.707 |
| Yes | 2 | 6 | 4 | 12 (24) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2026 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license.
Share and Cite
Adumitroaie, A.; Toma, V.; Badescu, M.C.; Cioloca, D.; Spinei, A.; Jdid, N.; Trandafirescu, M.F.; Leferman, C.E.; Foia, L.G. Assessment of Oral Health-Related Quality of Life in Children with Leukemia and Gingival Inflammation. J. Pers. Med. 2026, 16, 84. https://doi.org/10.3390/jpm16020084
Adumitroaie A, Toma V, Badescu MC, Cioloca D, Spinei A, Jdid N, Trandafirescu MF, Leferman CE, Foia LG. Assessment of Oral Health-Related Quality of Life in Children with Leukemia and Gingival Inflammation. Journal of Personalized Medicine. 2026; 16(2):84. https://doi.org/10.3390/jpm16020084
Chicago/Turabian StyleAdumitroaie, Alina, Vasilica Toma, Minerva Codruta Badescu, Daniel Cioloca, Aurelia Spinei, Nura Jdid, Mioara Florentina Trandafirescu, Carmen Ecaterina Leferman, and Liliana Georgeta Foia. 2026. "Assessment of Oral Health-Related Quality of Life in Children with Leukemia and Gingival Inflammation" Journal of Personalized Medicine 16, no. 2: 84. https://doi.org/10.3390/jpm16020084
APA StyleAdumitroaie, A., Toma, V., Badescu, M. C., Cioloca, D., Spinei, A., Jdid, N., Trandafirescu, M. F., Leferman, C. E., & Foia, L. G. (2026). Assessment of Oral Health-Related Quality of Life in Children with Leukemia and Gingival Inflammation. Journal of Personalized Medicine, 16(2), 84. https://doi.org/10.3390/jpm16020084








