Ultrasound-Guided Regional Block in Renal Transplantation: Towards Personalized Pain Management
Abstract
1. Introduction
2. Methods
2.1. Data Analysis
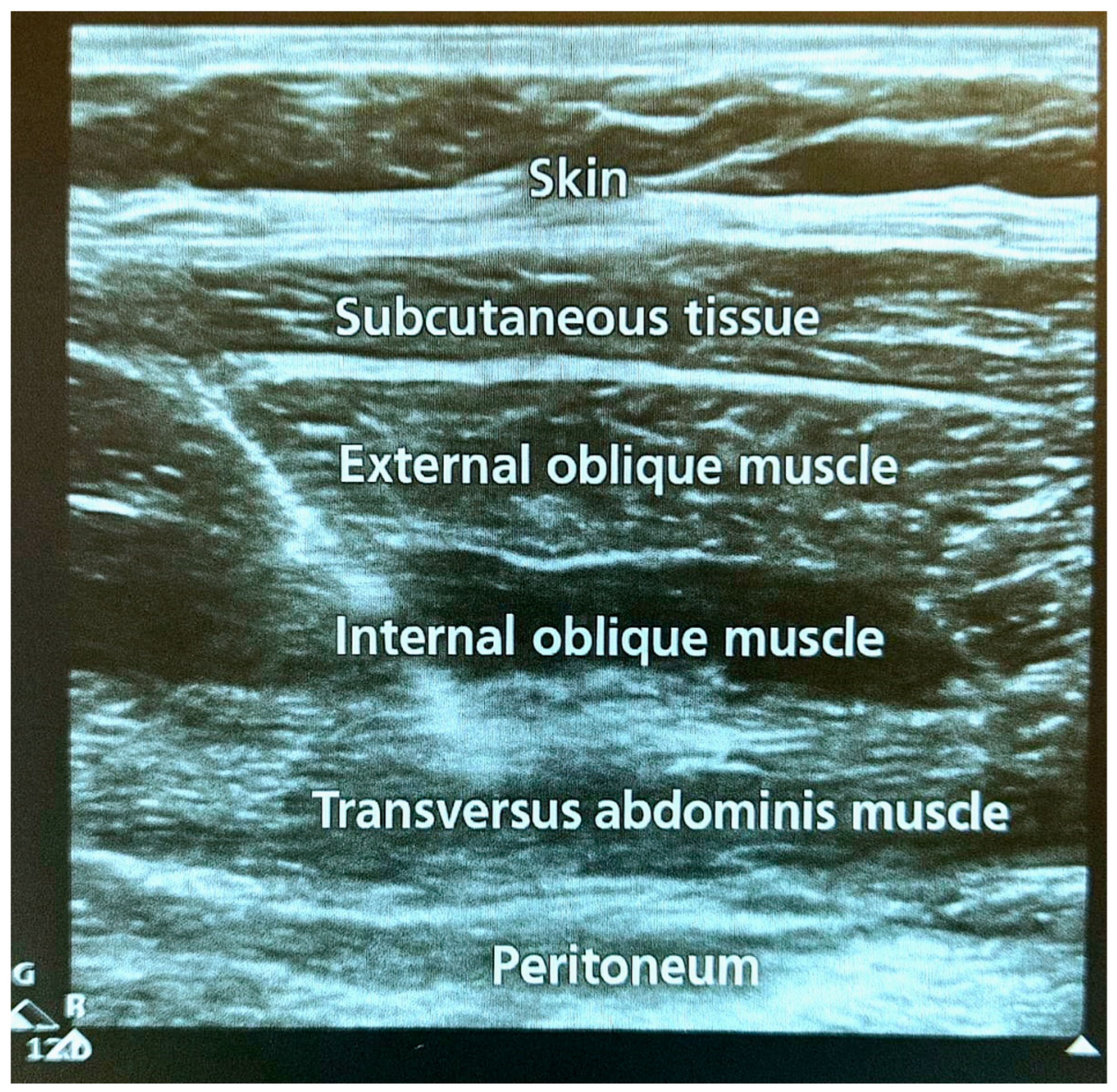
2.2. Procedure of Regional Block
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| AKI | Acute kidney injury |
| ASA | American Society of Anesthesiologists |
| M6G | Morphine-6-glucuronide |
| PCA | Patient-controlled analgesia |
| RCT | Randomized controlled trial |
| TAP | Transversus abdominis plane |
| UNOS | United Network of Organ Sharing |
| VAS | Visual analog scale |
References
- Golder, H.J.; Papalois, V. Enhanced Recovery after Surgery: History, Key Advancements and Developments in Transplant Surgery. J. Clin. Med. 2021, 10, 1634. [Google Scholar] [CrossRef]
- Morkane, C.M.; Fabes, J.; Banga, N.R.; Berry, P.D.; Kirwan, C.J. Perioperative management of adult cadaveric and live donor renal transplantation in the UK: A survey of national practice. Clin. Kidney J. 2019, 12, 880–887. [Google Scholar] [CrossRef]
- Jeong, R.; Lentine, K.L.; Quinn, R.R.; Ravani, P.; Wiebe, N.; Davison, S.N.; Barr, B.; Lam, N.N. NSAID prescriptions in kidney transplant recipients. Clin. Transplant. 2021, 35, e14405. [Google Scholar] [CrossRef]
- Sridharan, K.; Shah, S. Use of non-steroidal anti-inflammatory drugs in renal transplant patients: A retrospective study. Int. J. Risk Saf. Med. 2023, 34, 379–386. [Google Scholar] [CrossRef]
- Amer, A.; Scuffell, C.; Dowen, F.; Wilson, C.H.; Manas, D.M. A national survey on enhanced recovery for renal transplant recipients: Current practices and trends in the UK. Ann. R. Coll. Surg. Engl. 2023, 105, 166–172. [Google Scholar] [CrossRef]
- Gao, S.; He, Q. Opioids and the kidney: Two sides of the same coin. Front. Pharmacol. 2024, 15, 1421248. [Google Scholar] [CrossRef] [PubMed]
- Lafargue, M.C.; Caliskan, Y.; Lentine, K.L.; Riella, L.V. Opioids and Kidney Transplantation. Semin. Nephrol. 2021, 41, 42–53. [Google Scholar] [CrossRef] [PubMed]
- Tsai, H.C.; Yoshida, T.; Chuang, T.Y.; Yang, S.F.; Chang, C.C.; Yao, H.Y.; Tai, Y.-T.; Lin, J.-A.; Chen, K.-Y. Transversus Abdominis Plane Block: An Updated Review of Anatomy and Techniques. BioMed Res. Int. 2017, 2017, 8284363. [Google Scholar] [CrossRef] [PubMed]
- Zheng, C.; Yang, H.; Yang, L.; Luo, J.; Xiong, B. The Effect of Transversus Abdominis Plane Block in Kidney Transplantation: A Systematic Review and Meta-Analysis. Urol. Int. 2023, 107, 608–616. [Google Scholar] [CrossRef]
- Temirov, T.; Ben-David, B.; Mustafin, A.; Viderman, D. Erector Spinae Plane Block in Management of Pain After Kidney Transplantation. Pain Med. 2019, 20, 1053–1054. [Google Scholar] [CrossRef]
- Sindwani, G.; Sahu, S.; Suri, A.; Sureka, S.; Thomas, M. Efficacy of ultrasound guided quadratus lumborum block as postoperative analgesia in renal transplantation recipients: A randomised double blind clinical study. Indian J. Anaesth. 2020, 64, 605–610. [Google Scholar] [CrossRef]
- Kim, Y.; Kim, J.T.; Yang, S.M.; Kim, W.H.; Han, A.; Ha, J.; Min, S.; Park, S.-K. Anterior quadratus lumborum block for analgesia after living-donor renal transplantation: A double-blinded randomized controlled trial. Reg. Anesth. Pain Med. 2024, 49, 550–557. [Google Scholar] [CrossRef]
- Yang, P.; Luo, Y.; Lin, L.; Zhang, H.; Liu, Y.; Li, Y. The efficacy of transversus abdominis plane block with or without dexmedetomidine for postoperative analgesia in renal transplantation. A randomized controlled trial. Int. J. Surg. 2020, 79, 196–201. [Google Scholar] [CrossRef]
- Ali, A.; Pawelec, K.; Cacciola, R.; Puliatti, C.; Sammartino, C.; Sivaparakasam, R.; Fernandes, S. Effectiveness of Enhanced Recovery Programme in Kidney Transplant Recipient.: Abstract# A451. Transplantation 2014, 98, 810. [Google Scholar]
- Brogi, E.; Kazan, R.; Cyr, S.; Giunta, F.; Hemmerling, T.M. Transversus abdominal plane block for postoperative analgesia: A systematic review and meta-analysis of randomized-controlled trials. Can. J. Anaesth. 2016, 63, 1184–1196. [Google Scholar] [CrossRef]
- El-Boghdadly, K.; Pawa, A.; Chin, K.J. Local anesthetic systemic toxicity: Current perspectives. Local Reg. Anesth. 2018, 11, 35–44. [Google Scholar] [CrossRef] [PubMed]
- Shigeta, H.; Yasumura, R.; Kotake, Y. Comparison of plasma levobupivacaine concentrations with and without epinephrine following erector spinae plane block for breast cancer surgery: A randomized controlled trial. BMC Anesthesiol. 2022, 22, 86. [Google Scholar] [CrossRef] [PubMed]
- Soltani Mohammadi, S.; Dabir, A.; Shoeibi, G. Efficacy of transversus abdominis plane block for acute postoperative pain relief in kidney recipients: A double-blinded clinical trial. Pain Med. 2014, 15, 460–464. [Google Scholar] [CrossRef]
- Rozier, R.; Le Guennec, Y.; Capdevila, X.; Le Louarn, E.; Balbo, J.; Lavrut, T.; Baque, P.; Perus, O.; Destere, A.; Maurice-Szamburski, A. Impact of epinephrine on ropivacaine pharmacokinetics in TAP blocks: A randomized controlled trial. Reg Anesth. Pain Med. 2025; ahead of print. [Google Scholar]
- Uppal, V.; Sancheti, S.; Kalagara, H. Transversus Abdominis Plane (TAP) and Rectus Sheath Blocks: ATechnical Description and Evidence Review. Curr. Anesthesiol. Rep. 2019, 9, 479–487. [Google Scholar] [CrossRef]
- Bova, S.; Samet, R.E.; Deering, J.; Gaines, S.; Weinrub, A.; Bhati, C.; Niederhaus, S. Successful Opioid Minimization Following Kidney Transplant: A Quality Improvement Initiative. Cureus 2024, 16, e52917. [Google Scholar] [CrossRef]
- Odoma, V.A.; Pitliya, A.; AlEdani, E.; Bhangu, J.; Javed, K.; Manshahia, P.K.; Nahar, S.; Kanda, S.; Chatha, U.; Mohammed, L. Opioid Prescription in Patients With Chronic Kidney Disease: A Systematic Review of Comparing Safety and Efficacy of Opioid Use in Chronic Kidney Disease Patients. Cureus 2023, 15, e45485. [Google Scholar] [CrossRef]
- Zarate Rodriguez, J.; Edgley, C.; Lee, S.; Leigh, N.; Wolfe, R.; Sanford, D.; Hammill, C. Preoperative transversus abdominis plane block decreases intraoperative opiate consumption during minimally invasive cholecystectomy. Surg. Endosc. 2022, 37, 2209–2214. [Google Scholar] [CrossRef]
- Erdogan, M.A.; Ozgul, U.; Uçar, M.; Yalin, M.R.; Colak, Y.Z.; Çolak, C.; Toprak, H.I. Effect of transversus abdominis plane block in combination with general anesthesia on perioperative opioid consumption, hemodynamics, and recovery in living liver donors: The prospective, double-blinded, randomized study. Clin. Transplant. 2017, 31, e12931. [Google Scholar] [CrossRef]
- Zárate Rodriguez, J.G.; Leigh, N.; Edgley, C.; Cos, H.; Wolfe, R.; Sanford, D.; Hammill, C.W. Preoperative transversus abdominis plane block decreases intraoperative opiate use during pancreatoduodenectomy. HPB 2022, 24, 1162–1167. [Google Scholar] [CrossRef] [PubMed]
- Mukhtar, K.; Khattak, I. Transversus abdominis plane block for renal transplant recipients. Br. J. Anaesth. 2010, 104, 663–664. [Google Scholar] [CrossRef] [PubMed]
- Mavarez, A.C.; Hendrix, J.M.; Ahmed, A.A. Transabdominal Plane Block. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2025. Available online: http://www.ncbi.nlm.nih.gov/books/NBK560527/ (accessed on 5 August 2025).
- Leão, A.; Leao, C.; Silva, M.; Moraes, A. Analgesic efficacy of Transverse Abdomen Plane Block in Kidney Transplantation. Braz. J. Transplant. 2023, 13, 26. [Google Scholar] [CrossRef]
- Farag, E.; Guirguis, M.N.; Helou, M.; Dalton, J.E.; Ngo, F.; Ghobrial, M.; O’hAra, J.; Seif, J.; Krishnamurthi, V.; Goldfarb, D. Continuous transversus abdominis plane block catheter analgesia for postoperative pain control in renal transplant. J. Anesth. 2015, 29, 4–8. [Google Scholar] [CrossRef]
- Viderman, D.; Aubakirova, M.; Nabidollayeva, F.; Aryngazin, A.; Romero-Garcia, N.; Badenes, R.; Abdildin, Y.G. The Effect of Transversus Abdominis Plane Block on Pain-Related Outcomes in Kidney Transplantation: A Systematic Review with Meta-Analysis and Trial Sequential Analysis. J. Clin. Med. 2025, 14, 1879. [Google Scholar] [CrossRef]
- Jankovic, Z.B.; Pollard, S.G.; Nachiappan, M.M. Continuous transversus abdominis plane block for renal transplant recipients. Anesth. Analg. 2009, 109, 1710–1711. [Google Scholar] [CrossRef]
- Freir, N.M.; Murphy, C.; Mugawar, M.; Linnane, A.; Cunningham, A.J. Transversus abdominis plane block for analgesia in renal transplantation: A randomized controlled trial. Anesth. Analg. 2012, 115, 953–957. [Google Scholar] [CrossRef]
- Gulyam Kuruba, S.M.; Mukhtar, K.; Singh, S.K. A randomised controlled trial of ultrasound-guided transversus abdominis plane block for renal transplantation. Anaesthesia 2014, 69, 1222–1226. [Google Scholar] [CrossRef] [PubMed]
- Garmon, E.H.; Hendrix, J.M.; Huecker, M.R. Topical, Local, and Regional Anesthesia and Anesthetics. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2025. Available online: https://www.ncbi.nlm.nih.gov/books/NBK430894/ (accessed on 21 February 2025).
| Group A (Regional Block) n = 50 | Group B (No Regional Block) n = 50 | |
|---|---|---|
| Age (years) | 53.33 ± 12.53 | 53.48 ± 12.74 |
| Body mass index (kg/m2) | 29.27 ± 5.73 | 29.58 ± 5.10 |
| Gender | ||
| Male | 31 (62.0%) | 34 (68.0%) |
| Female | 19 (38.0%) | 16 (32.0%) |
| Race | ||
| Black | 36 (72.0%) | 41 (82.0%) |
| Caucasian | 11 (22.0%) | 5 (10.0%) |
| Hispanic | 2 (4.0%) | 3 (6.0%) |
| Asian | 1 (2.0%) | 1 (2.0%) |
| Cause of end-stage renal disease | ||
| Hypertension | 18 (36.0%) | 21 (42.0%) |
| Diabetes mellitus | 17 (34.0%) | 14 (28.0%) |
| Focal segmental glomerulosclerosis | 1 (2.0%) | 1 (2.0%) |
| Previous transplant | 4 (8.0%) | 3 (6.0%) |
| Autoimmune nephropathies | 7 (14.0%) | 9 (18.0%) |
| Polycystic kidney disease | 3 (6.0%) | 2 (4.0%) |
| ASA score | ||
| 3 | 40 (80.0%) | 41 (82.0%) |
| 4 | 10 (20.0%) | 9 (18.0%) |
| Medication | All Subjects (Group A and B) n = 100 | Group A (Regional Block) n = 50 | Group B (No Regional Block) n = 50 | p-Value (Group A vs. Group B) |
|---|---|---|---|---|
| Intraoperative fentanyl (μg) | 186.75 ± 105.67 | 171.0 ± 93.32 | 202.5 ± 115.53 | 0.04 |
| Intraoperative hydromorphone (mg) | 0.72 ± 0.48 | 0.72 ± 0.49 | 0.71 ± 0.48 | 0.84 |
| Hydromorphone (mg) in 24 h | 0.97± 0.74 | 0.94 ± 0.80 | 1.007 ± 0.68 | 0.66 |
| Oxycodone (mg) in 24 h | 24.85 ± 16.07 | 25.6 ± 15.83 | 24.59 ± 16.22 | 0.75 |
| Acetaminophen (grams) in 24 h | 2.67 ± 0.89 | 2.71 ± 0.78 | 2.63 ± 0.99 | 0.64 |
| Group A (Regional Block) n = 50 | Group B (No Regional Block) n = 50 | p-Value | |
|---|---|---|---|
| Nausea | |||
| Yes | 7 (14.0%) | 6 (12.0%) | 0.766 |
| No | 43 (86.0%) | 44 (88.0%) | |
| Vomiting | |||
| Yes | 5 (10.0%) | 2 (4.0%) | 0.436 |
| No | 45 (90.0%) | 48 (96.0%) | |
| Pruritus | |||
| Yes | 2 (4.0%) | 1 (98.0%) | 1 |
| No | 48 (96.0%) | 49 (2.0%) | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mirza, A.; Khan, M.; Massey, Z.; Baig, U.; Gani, I.; Beigh, S. Ultrasound-Guided Regional Block in Renal Transplantation: Towards Personalized Pain Management. J. Pers. Med. 2025, 15, 411. https://doi.org/10.3390/jpm15090411
Mirza A, Khan M, Massey Z, Baig U, Gani I, Beigh S. Ultrasound-Guided Regional Block in Renal Transplantation: Towards Personalized Pain Management. Journal of Personalized Medicine. 2025; 15(9):411. https://doi.org/10.3390/jpm15090411
Chicago/Turabian StyleMirza, Ahmad, Munazza Khan, Zachary Massey, Usman Baig, Imran Gani, and Shameem Beigh. 2025. "Ultrasound-Guided Regional Block in Renal Transplantation: Towards Personalized Pain Management" Journal of Personalized Medicine 15, no. 9: 411. https://doi.org/10.3390/jpm15090411
APA StyleMirza, A., Khan, M., Massey, Z., Baig, U., Gani, I., & Beigh, S. (2025). Ultrasound-Guided Regional Block in Renal Transplantation: Towards Personalized Pain Management. Journal of Personalized Medicine, 15(9), 411. https://doi.org/10.3390/jpm15090411





