Endoscopic Sinus Surgery in Frontal Sinus Inverted Papilloma: A Systematic Review
Abstract
1. Introduction
2. Materials and Methods
2.1. Synthesis Without Meta-Analysis Criteria
2.2. Protocol and Registration
2.3. Inclusion Criteria
2.4. Sources
2.5. Literature Search Strategy
2.6. Article Selection
2.7. Data Collection and Selection
2.8. Risk of Bias Assessment Methods
2.9. Main Results
3. Results
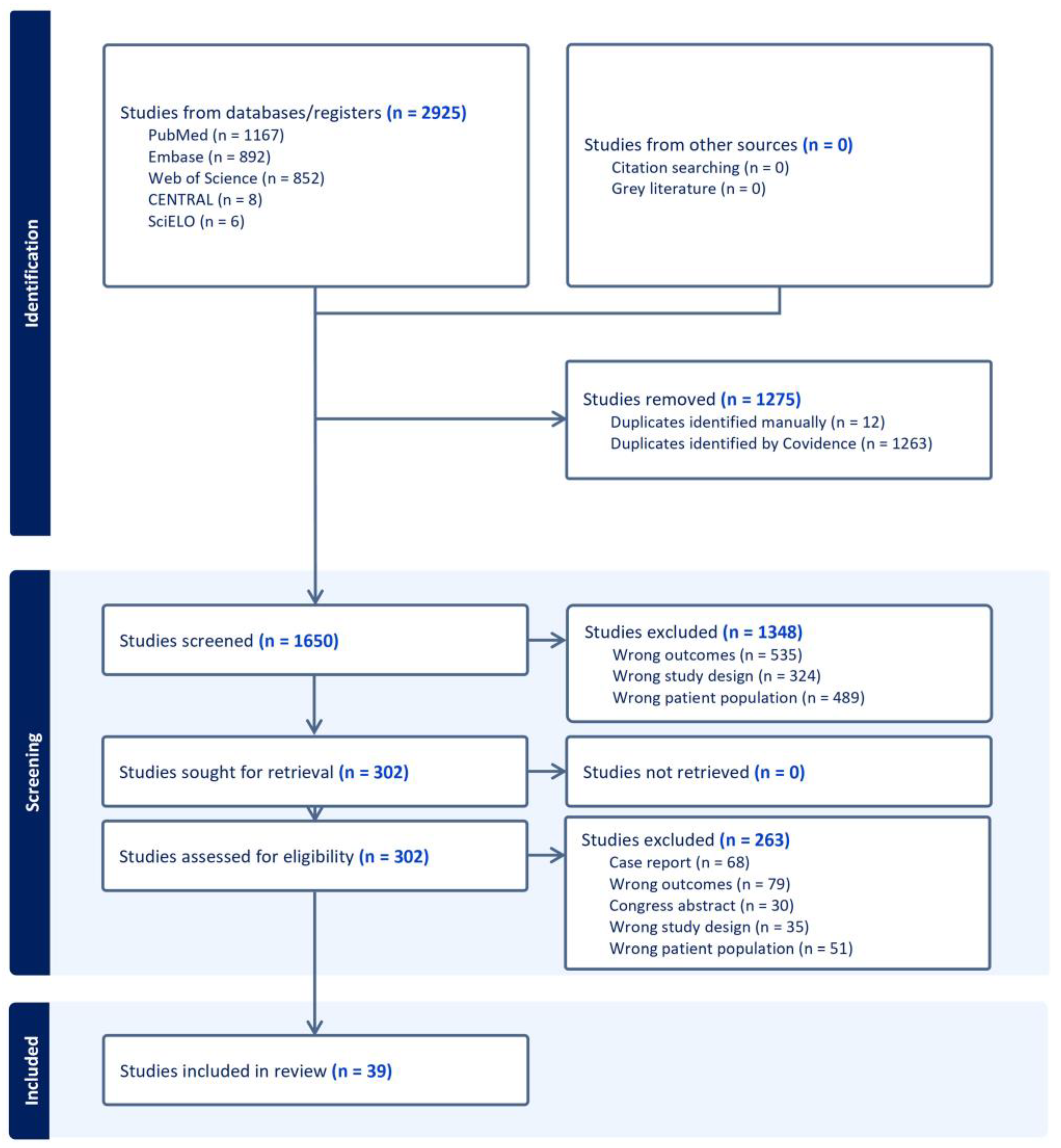
3.1. Study Selection
3.2. Description of Included Studies
3.3. Recurrence Rate After Surgery in Frontal Sinus IP
3.4. Risk of Bias Assessment
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| IP | Inverted Papilloma |
| MINORS | Methodological Index for Non-Randomized Studies |
| SWIM | Systematic Review without Meta-Analysis |
| EPOS | European Position Paper on Sinus |
References
- Wang, M.; Noel, J.E. Etiology of Sinonasal Inverted Papilloma: A Narrative Review. World J. Otorhinolaryngol.-Head Neck Surg. 2017, 3, 54–58. [Google Scholar] [CrossRef] [PubMed]
- Vorasubin, N.; Vira, D.; Suh, J.D.; Bhuta, S.; Wang, M.B. Schneiderian Papillomas: Comparative Review of Exophytic, Oncocytic, and Inverted Types. Am. J. Rhinol. Allergy 2013, 27, 287–292. [Google Scholar] [CrossRef]
- Lisan, Q.; Laccourreye, O.; Bonfils, P. Sinonasal Inverted Papilloma: From Diagnosis to Treatment. Eur. Ann. Otorhinolaryngol. Head Neck Dis. 2016, 133, 337–341. [Google Scholar] [CrossRef] [PubMed]
- Elliot, A.; Marklund, L.; Håkansson, N.; Song, H.; Ye, W.; Stjärne, P.; Hammarstedt-Nordenvall, L. Incidence of IP and Risk of Malignant Transformation in the Swedish Population 1960–2010. Eur. Arch. Oto-Rhino-Laryngol. 2017, 274, 1445–1448. [Google Scholar] [CrossRef] [PubMed]
- Lawson, W.; Schlecht, N.F.; Brandwein-Gensler, M. The Role of the Human Papillomavirus in the Pathogenesis of Schneiderian Inverted Papillomas: An Analytic Overview of the Evidence. Head Neck Pathol. 2008, 2, 49–59. [Google Scholar] [CrossRef]
- Govindaraj, S.; Wang, H. Does Human Papilloma Virus Play a Role in Sinonasal Inverted Papilloma? Curr. Opin. Otolaryngol. Head Neck Surg. 2014, 22, 47–51. [Google Scholar] [CrossRef]
- d’Errico, A.; Zajacova, J.; Cacciatore, A.; Baratti, A.; Zanelli, R.; Alfonzo, S.; Beatrice, F. Occupational Risk Factors for Sinonasal Inverted Papilloma: A Case–Control Study. Occup. Environ. Med. 2013, 70, 703–708. [Google Scholar] [CrossRef]
- Buchwald, C.; Franzmann, M.; Tos, M. Sinonasal Papillomas: A Report of 82 Cases in Copenhagen County, Including a Longitudinal Epidemiological and Clinical Study. Laryngoscope 1995, 105, 72–79. [Google Scholar] [CrossRef]
- Kamel, R.H.; Khaled, A.; Abdelfattah, A.F.; Awad, A.G. Surgical Treatment of Sinonasal Inverted Papilloma. Curr. Opin. Otolaryngol. Head Neck Surg. 2022, 30, 26–32. [Google Scholar] [CrossRef]
- Russo, C.; Elefante, A.; Romano, A.; Cama, A.; Erra, M.; Ugga, L.; Brunetti, L.; Motta, G.; Califano, L.; Iengo, M.; et al. A Multimodal Diagnostic Approach to Inverted Papilloma: Proposal of a Novel Diagnostic Flow-Chart. Curr. Probl. Diagn. Radiol. 2021, 50, 499–504. [Google Scholar] [CrossRef]
- Kuan, E.C.; Wang, E.W.; Adappa, N.D.; Beswick, D.M.; London, N.R.; Su, S.Y.; Wang, M.B.; Abuzeid, W.M.; Alexiev, B.; Alt, J.A.; et al. International Consensus Statement on Allergy and Rhinology: Sinonasal Tumors. Int. Forum Allergy Rhinol. 2024, 14, 149–608. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.J.; Roland, L.T.; Licata, J.J.; Orlowski, H.L.P.; Jiramongkolchai, P.; Piccirillo, J.F.; Kallogjeri, D.; Klatt-Cromwell, C.N.; Chernock, R.D.; Schneider, J.S. Morphologic, Intraoperative, and Histologic Risk Factors for Sinonasal Inverted Papilloma Recurrence. Laryngoscope 2020, 130, 590–596. [Google Scholar] [CrossRef] [PubMed]
- Shohet, J.; Duncavage, J. Management of the Frontal Sinus with Inverted Papilloma. Otolaryngol. Head Neck Surg. 1996, 114, 649–652. [Google Scholar] [CrossRef] [PubMed]
- Kim, D.-Y.; Hong, S.-L.; Lee, C.H.; Jin, H.-R.; Kang, J.M.; Lee, B.-J.; Moon, I.J.; Chung, S.-K.; Rha, K.-S.; Cho, S.H.; et al. Inverted Papilloma of the Nasal Cavity and Paranasal Sinuses: A Korean Multicenter Study. Laryngoscope 2012, 122, 487–494. [Google Scholar] [CrossRef]
- Krouse, J.H. Development of a Staging System for Inverted Papilloma. Laryngoscope 2000, 110, 965–968. [Google Scholar] [CrossRef]
- Gaudioso, P.; Vinciguerra, A.; Verillaud, B.; Herman, P. Management of Frontal Sinus and Frontal Recess Inverted Papilloma: Our Experience and Systematic Review. Acta Otorhinolaryngol. Ital. 2024, 44, 252–260. [Google Scholar] [CrossRef]
- Campbell, M.; McKenzie, J.E.; Sowden, A.; Katikireddi, S.V.; Brennan, S.E.; Ellis, S.; Hartmann-Boyce, J.; Ryan, R.; Shepperd, S.; Thomas, J.; et al. Synthesis without Meta-Analysis (SWiM) in Systematic Reviews: Reporting Guideline. BMJ 2020, 368, l6890. [Google Scholar] [CrossRef]
- Slim, K.; Nini, E.; Forestier, D.; Kwiatkowski, F.; Panis, Y.; Chipponi, J. Methodological Index for Non-Randomized Studies (Minors): Development and Validation of a New Instrument. ANZ J. Surg. 2003, 73, 712–716. [Google Scholar] [CrossRef]
- Adriaensen, G.F.J.P.M.; Lim, K.-H.; Georgalas, C.; Reinartz, S.M.; Fokkens, W.J. Challenges in the Management of Inverted Papilloma: A Review of 72 Revision Cases. Laryngoscope 2016, 126, 322–328. [Google Scholar] [CrossRef]
- Adriaensen, G.F.; van der Hout, M.W.; Reinartz, S.M.; Georgalas, C.; Fokkens, W.J. Endoscopic Treatment of Inverted Papilloma Attached in the Frontal Sinus/Recess. Rhinology 2015, 53, 317–324. [Google Scholar] [CrossRef]
- Akkari, M.; Lassave, J.; Mura, T.; Gascou, G.; Pierre, G.; Cartier, C.; Garrel, R.; Crampette, L. Atypical Presentations of Sinonasal Inverted Papilloma: Surgical Management and Influence on the Recurrence Rate. Am. J. Rhinol. Allergy 2016, 30, 149–154. [Google Scholar] [CrossRef]
- Bertrand, B.; Eloy, P.; Jorissen, M.; Rombaux, P.; Daele, J.; Boniver, V.; Collet, S.; Demanez, J.P.; Verheyden, P.J.; Bachert, C. Surgery of Inverted Papillomas under Endoscopic Control. Acta Otorhinolaryngol. Belg. 2000, 54, 139–150. [Google Scholar] [PubMed]
- Cho, S.W.; Kim, S.G.; Han, D.H.; Kim, H.J.; Kim, J.W.; Kim, D.Y.; Rhee, C.S.; Won, T.B. Treatment Outcome and Prognostic Factors of Inverted Papilloma Involving the Frontal Sinus. Laryngoscope Investig. Otolaryngol. 2024, 9, e1206. [Google Scholar] [CrossRef] [PubMed]
- Choi, W.R.; Lee, B.J.; Kim, J.H. Long-Term Outcome Following Resection of Sinonasal Inverted Papillomas: A Single Surgeon’s Experience in 127 Patients. Clin. Otolaryngol. 2019, 44, 652–655. [Google Scholar] [CrossRef]
- Coutinho, G.; Marques, J.; Leal, M.; Spratley, J.; Fernandes, M.S.; Santos, M. Surgical Outcomes of Sinonasal Inverted Papilloma: A 17 Year Review. Braz. J. Otorhinolaryngol. 2020, 86, 315–320. [Google Scholar] [CrossRef]
- Dragonetti, A.; Gera, R.; Sciuto, A.; Scotti, A.; Bigoni, A.; Barbaro, E.; Minni, A. Sinonasal Inverted Papilloma: 84 Patients Treated by Endoscopy and Proposal for a New Classification. Rhinology 2011, 49, 207–213. [Google Scholar] [CrossRef]
- Dubin, M.G.; Sonnenburg, R.E.; Melroy, C.T.; Ebert, C.S.; Coffey, C.S.; Senior, B.A. Staged Endoscopic and Combined Open/Endoscopic Approach in the Management of Inverted Papilloma of the Frontal Sinus. Am. J. Rhinol. 2005, 19, 442–445. [Google Scholar] [CrossRef] [PubMed]
- Ferrari, M.; Schreiber, A.; Mattavelli, D.; Rampinelli, V.; Bertazzoni, G.; Tomasoni, M.; Gualtieri, T.; Nicolai, P. How Aggressive Should Resection of Inverted Papilloma Be? Refinement of Surgical Planning Based on the 25-Year Experience of a Single Tertiary Center. Int. Forum. Allergy Rhinol. 2020, 10, 619–628. [Google Scholar] [CrossRef]
- Glikson, E.; Dragonetti, A.; Soudry, E.; Rozendoren, N.; Alon, E.E.; Landsberg, R.; Schneider, S.; Bedrin, L.; Mozzanica, F.; Bulgheroni, C.; et al. Is Intraoperative Margin Sampling Necessary in Inverted Papilloma Resection? Eur. Arch. Otorhinolaryngol. 2022, 279, 2935–2942. [Google Scholar] [CrossRef]
- Healy, D.Y., Jr.; Chhabra, N.; Metson, R.; Holbrook, E.H.; Gray, S.T. Surgical Risk Factors for Recurrence of Inverted Papilloma. Laryngoscope 2016, 126, 796–801. [Google Scholar] [CrossRef]
- Holzmann, D.; Hegyi, I.; Rajan, G.P.; Harder-Ruckstuhl, M. Management of Benign Inverted Sinonasal Papilloma Avoiding External Approaches. J. Laryngol. Otol. 2007, 121, 548–554. [Google Scholar] [CrossRef]
- Kamel, R.H.; Abdel Fattah, A.F.; Awad, A.G. Origin Oriented Management of Inverted Papilloma of the Frontal Sinus. Rhinology 2012, 50, 262–268. [Google Scholar] [CrossRef] [PubMed]
- Karligkiotis, A.; Pistochini, A.; Turri-Zanoni, M.; Terranova, P.; Volpi, L.; Battaglia, P.; Bignami, M.; Castelnuovo, P. Endoscopic Endonasal Orbital Transposition to Expand the Frontal Sinus Approaches. Am. J. Rhinol. Allergy 2015, 29, 449–456. [Google Scholar] [CrossRef]
- Kim, Y.M.; Kim, H.S.; Park, J.Y.; Koo, B.S.; Park, Y.H.; Rha, K.S. External vs. Endoscopic Approach for Inverted Papilloma of the Sino-Nasal Cavities: A Retrospective Study of 136 Cases. Acta Otolaryngol. 2008, 128, 909–914. [Google Scholar] [CrossRef] [PubMed]
- Lawson, W.; Ho, B.T.; Shaari, C.M.; Biller, H.F. Inverted Papilloma: A Report of 112 Cases. Laryngoscope 1995, 105, 282–288. [Google Scholar] [CrossRef] [PubMed]
- Lawson, W.; Kaufman, M.R.; Biller, H.F. Treatment Outcomes in the Management of Inverted Papilloma: An Analysis of 160 Cases. Laryngoscope 2003, 113, 1548–1556. [Google Scholar] [CrossRef]
- Lombardi, D.; Tomenzoli, D.; Buttà, L.; Bizzoni, A.; Farina, D.; Sberze, F.; Karligkiotis, A.; Castelnuovo, P.; Nicolai, P. Limitations and Complications of Endoscopic Surgery for Treatment for Sinonasal Inverted Papilloma: A Reassessment after 212 Cases. Head Neck 2011, 33, 1154–1161. [Google Scholar] [CrossRef]
- Minni, A.; Gera, R.; Bulgheroni, C.; Ralli, M.; Cialente, F.; Candelori, F.; Mevio, N.; Dragonetti, A. Endoscopic Resection of Sinonasal Inverted Papilloma: A Multivariate Retrospective Analysis of Factors Affecting Recurrence and Persistence. Ear Nose Throat J. 2021, 100, 542s–548s. [Google Scholar] [CrossRef]
- Minovi, A.; Kollert, M.; Draf, W.; Bockmühl, U. Inverted Papilloma: Feasibility of Endonasal Surgery and Long-Term Results of 87 Cases. Rhinology 2006, 44, 205–210. [Google Scholar]
- Nygren, A.; Kiss, K.; von Buchwald, C.; Bilde, A. Rate of Recurrence and Malignant Transformation in 88 Cases with Inverted Papilloma between 1998-2008. Acta Otolaryngol. 2016, 136, 333–336. [Google Scholar] [CrossRef]
- Pietrobon, G.; Karligkiotis, A.; Turri-Zanoni, M.; Fazio, E.; Battaglia, P.; Bignami, M.; Castelnuovo, P. Surgical Management of Inverted Papilloma Involving the Frontal Sinus: A Practical Algorithm for Treatment Planning. Acta Otorhinolaryngol. Ital. 2019, 39, 28–39. [Google Scholar] [CrossRef]
- Promsopa, C.; Thanahirunrojh, S. Surgical Outcomes of Sinonasal Inverted Papillomas in Songklanagarind Hospital. J. Med. Assoc. Thai 2015, 98, 1209–1214. [Google Scholar] [PubMed]
- Sautter, N.B.; Citardi, M.J.; Batra, P.S. Minimally Invasive Resection of Frontal Recess/Sinus Inverted Papilloma. Am. J. Otolaryngol. 2007, 28, 221–224. [Google Scholar] [CrossRef] [PubMed]
- Sciarretta, V.; Fernandez, I.J.; Farneti, P.; Pasquini, E. Endoscopic and Combined External-Transnasal Endoscopic Approach for the Treatment of Inverted Papilloma: Analysis of 110 Cases. Eur. Arch. Otorhinolaryngol. 2014, 271, 1953–1959. [Google Scholar] [CrossRef] [PubMed]
- Sham, C.L.; van Hasselt, C.A.; Chow, S.M.W.; Lee, D.L.Y.; Cho, R.H.W.; Woo, J.K.S.; Tong, M.C.F. Frontal Inverted Papillomas: A 25-Year Study. Laryngoscope 2020, 130, 1622–1628. [Google Scholar] [CrossRef]
- Takahashi, Y.; Shoji, F.; Katori, Y.; Hidaka, H.; Noguchi, N.; Abe, Y.; Kakuta, R.K.; Suzuki, T.; Suzuki, Y.; Ohta, N.; et al. Endoscopic Surgical Management of Sinonasal Inverted Papilloma Extending to Frontal Sinuses. Otolaryngol. Pol. 2016, 70, 26–32. [Google Scholar] [CrossRef]
- Verillaud, B.; Le Clerc, N.; Blancal, J.P.; Guichard, J.P.; Kania, R.; Classe, M.; Herman, P. Mucocele Formation after Surgical Treatment of Inverted Papilloma of the Frontal Sinus Drainage Pathway. Am. J. Rhinol. Allergy 2016, 30, 181–184. [Google Scholar] [CrossRef]
- Von Buchwald, C.; Larsen, A.S. Endoscopic Surgery of Inverted Papillomas under Image Guidance—A Prospective Study of 42 Consecutive Cases at a Danish University Clinic. Otolaryngol. Head Neck Surg. 2005, 132, 602–607. [Google Scholar] [CrossRef]
- Yoon, B.N.; Batra, P.S.; Citardi, M.J.; Roh, H.J. Frontal Sinus Inverted Papilloma: Surgical Strategy Based on the Site of Attachment. Am. J. Rhinol. Allergy 2009, 23, 337–341. [Google Scholar] [CrossRef]
- Yu, S.; Grose, E.; Lee, D.J.; Wu, V.; Pellarin, M.; Lee, J.M. Evaluation of Inverted Papilloma Recurrence Rates and Factors Associated Recurrence after Endoscopic Surgical Resection: A Retrospective Review. J. Otolaryngol. Head Neck Surg. 2023, 52, 34. [Google Scholar] [CrossRef]
- Zhang, L.; Han, D.; Wang, C.; Ge, W.; Zhou, B. Endoscopic Management of the Inverted Papilloma with Attachment to the Frontal Sinus Drainage Pathway. Acta Otolaryngol. 2008, 128, 561–568. [Google Scholar] [CrossRef] [PubMed]
- Delaine, E.; Gorostidi, F.; Guilcher, P.; Lambercy, K.; Litzistorf, Y.; Bron, L.; Reinhard, A. Risk Factors for Recurrence after Surgical Resection of Sinonasal Inverted Papilloma. Int. Arch. Otorhinolaryngol. 2024, 28, e568–e573. [Google Scholar] [CrossRef] [PubMed]
- Woodworth, B.A.; Bhargave, G.A.; Palmer, J.N.; Chiu, A.G.; Cohen, N.A.; Lanza, D.C.; Bolger, W.E.; Kennedy, D.W. Clinical Outcomes of Endoscopic and Endoscopic-Assisted Resection of Inverted Papillomas: A 15-Year Experience. Am. J. Rhinol. 2007, 21, 591–600. [Google Scholar] [CrossRef]
- SamimiArdestani, S. The Characteristics of Sinonasal Inverted Papilloma and Recurrence Factors: An Analysis of 207 Cases. World J. Otorhinolaryngol. Head Neck Surg. 2024, 1–6. [Google Scholar] [CrossRef]
- Busquets, J.M.; Hwang, P.H. Endoscopic Resection of Sinonasal Inverted Papilloma: A Meta-Analysis. Otolaryngol.-Head Neck Surg. 2006, 134, 476–482. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.S.; Kwon, S.H. Recurrence of Sinonasal Inverted Papilloma Following Surgical Approach: A Meta-Analysis. Laryngoscope 2017, 127, 52–58. [Google Scholar] [CrossRef]
- Bastier, P.L.; de Gabory, L. Design and Assessment of an Anatomical Diagram for Sinonasal Malignant Tumour Resection. Rhinology 2016, 54, 361–367. [Google Scholar] [CrossRef]
- Wang, Y.; An, Y.; Zhao, C.; Dong, R.; Cheng, F. Attachment-Oriented Endoscopic Treatment of Inverted Papilloma Involving the Frontal Sinus/Recess. J. Craniofac. Surg. 2020, 31, e778–e781. [Google Scholar] [CrossRef]
- Yan, Y.; Liu, Y.; Tao, J.; Li, Z.; Qu, X.; Guo, J.; Xian, J. Preoperative Prediction of Malignant Transformation of Sinonasal Inverted Papilloma Using MR Radiomics. Front. Oncol. 2022, 12, 870544. [Google Scholar] [CrossRef]
- Lawson, W.; Ho, Y. Open Frontal Sinus Surgery: A Lost Art. Otolaryngol. Clin. N. Am. 2016, 49, 1067–1089. [Google Scholar] [CrossRef]
| Characteristics (n = 25 Studies) | Other Approaches | Purely Endoscopic | p-Value |
|---|---|---|---|
| Mean number of patients per study (±SD) | 5.6 (7.0) | 13.8 (15.2) | 0.003 |
| Age in years (±SD) | 59.0 (5.6) | 52.6 (2.8) | 0.095 |
| Follow-up in months (±SD) | 40.2 (0.4) | 30.7 (11.7) | 0.381 |
| Rate of recurrence | 16.5% | 14.7% | 0.675 |
| Time to recurrence; n = 5 studies | 73.2 (40.8) | 28.0 (11.3) | 0.095 |
| Author. Year | Sample Size (n) | Age (Years) | Follow up (Month) | Recurrence (n) | Recurrence Time (Month) | MINOR Score | MINOR Maximum Score |
|---|---|---|---|---|---|---|---|
| Lawson. 1995 [35] | 7 | 57.3 | 54.0 | 3 | NA | 11 | 16 |
| Bertrand. 2000 [22] | 85 | 58.4 | 41.9 | 15 | 8 | 16 | 24 |
| Lawson. 2003 [36] | 13 | NA | NA | 3 | NA | 14 | 24 |
| Dubin. 2005 [27] | 6 | NA | NA | 5 | 13.3 | 14 | 24 |
| Von Buchwald. 2005 [48] | 13 | 61.0 | 37.0 | 0 | 9 | 16 | 24 |
| Minovi. 2006 [39] | 13 | NA | NA | 0 | NA | 14 | 24 |
| Holzmann. 2007 [31] | 9 | NA | 35.0 | 1 | 35 | 11 | 16 |
| Woodworth. 2007 [53] | 9 | NA | 40 | 4 | NA | 11 | 16 |
| Sautter. 2007 [43] | 5 | 55.0 | NA | 0 | 16.8 | 14 | 24 |
| Kim. 2008 [34] | 5 | 51.4 | 41.9 | 0 | NA | 16 | 24 |
| Zhang. 2008 [51] | 9 | 50.2 | 15.1 | 0 | NA | 15 | 24 |
| Yoon. 2009 [49] | 18 | 55.0 | 36.6 | 4 | 36 | 16 | 24 |
| Dragonetti. 2011 [26] | 8 | NA | NA | 1 | NA | 14 | 24 |
| Lombardi. 2011 [37] | 27 | NA | NA | 2 | NA | 14 | 24 |
| Kamel. 2012 [32] | 6 | 49.0 | 27.0 | 0 | NA | 16 | 24 |
| Kim. 2012 [14] | 22 | 54.1 | 41.0 | 6 | 32.6 | 16 | 24 |
| Sciarretta. 2014 [44] | 9 | 58.7 | 18.0 | 2 | 18 | 14 | 24 |
| Promsopa. 2015 [42] | 17 | 55.0 | 7.5 | 0 | 7.5 | 10 | 16 |
| Adriaensen. 2015 [20] | 20 | 53.7 | 47.6 | 2 | 42 | 16 | 24 |
| Karligkiotis. 2015 [33] | 5 | 48.0 | 40.6 | 0 | NA | 16 | 24 |
| Akkari. 2016 [21] | 12 | NA | NA | 3 | 23.6 | 9 | 16 |
| Nygren. 2016 [40] | 10 | NA | NA | 10 | NA | 9 | 16 |
| Takahashi. 2016 [46] | 10 | 58.4 | 39.5 | 0 | NA | 11 | 16 |
| Adriaensen. 2016 [19] | 17 | NA | NA | 3 | 26.6 | 14 | 24 |
| Healy. 2016 [30] | 26 | 56.9 | 96.0 | 4 | 32.4 | 16 | 24 |
| Verillaud. 2016 [47] | 27 | 58.0 | 40.0 | 2 | 40 | 16 | 24 |
| Choi. 2019 [24] | 23 | NA | NA | 6 | 37.76 | 9 | 16 |
| Pietrobon. 2019 [41] | 47 | 57.0 | 43.0 | 2 | 24 | 16 | 24 |
| Coutinho. 2020 [25] | 5 | NA | NA | 1 | 11.4 | 9 | 16 |
| Ferrari. 2020 [28] | 12 | NA | NA | 1 | 34 | 9 | 16 |
| Lee. 2020 [12] | 14 | NA | NA | 9 | NA | 14 | 24 |
| Sham. 2020 [45] | 29 | 55.0 | 56.4 | 12 | 39.8 | 16 | 24 |
| Minni. 2021 [38] | 21 | NA | NA | 3 | NA | 14 | 24 |
| Glikson. 2022 [29] | 17 | NA | NA | 3 | NA | 9 | 16 |
| Yu. 2023 [50] | 9 | NA | NA | 1 | NA | 14 | 24 |
| Cho. 2024 [23] | 13 | 60.6 | NA | 0 | NA | 9 | 16 |
| Delaine. 2024 [52] | 5 | 55.5 | NA | 3 | 23.8 | 9 | 16 |
| SamimiArdestani. 2024 [54] | 9 | NA | NA | 4 | NA | 9 | 16 |
| Gaudioso. 2024 [16] | 30 | 57 | 37 | 3 | NA | 16 | 24 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Fieux, M.; Favier, V.; Sousa Machado, A.; Nourredine, M.; Giroudon, C.; Carsuzaa, F.; Naik, P.P.; the yo-IFOS Group. Endoscopic Sinus Surgery in Frontal Sinus Inverted Papilloma: A Systematic Review. J. Pers. Med. 2025, 15, 183. https://doi.org/10.3390/jpm15050183
Fieux M, Favier V, Sousa Machado A, Nourredine M, Giroudon C, Carsuzaa F, Naik PP, the yo-IFOS Group. Endoscopic Sinus Surgery in Frontal Sinus Inverted Papilloma: A Systematic Review. Journal of Personalized Medicine. 2025; 15(5):183. https://doi.org/10.3390/jpm15050183
Chicago/Turabian StyleFieux, Maxime, Valentin Favier, Andre Sousa Machado, Mikail Nourredine, Caroline Giroudon, Florent Carsuzaa, Paresh P. Naik, and the yo-IFOS Group. 2025. "Endoscopic Sinus Surgery in Frontal Sinus Inverted Papilloma: A Systematic Review" Journal of Personalized Medicine 15, no. 5: 183. https://doi.org/10.3390/jpm15050183
APA StyleFieux, M., Favier, V., Sousa Machado, A., Nourredine, M., Giroudon, C., Carsuzaa, F., Naik, P. P., & the yo-IFOS Group. (2025). Endoscopic Sinus Surgery in Frontal Sinus Inverted Papilloma: A Systematic Review. Journal of Personalized Medicine, 15(5), 183. https://doi.org/10.3390/jpm15050183







