Innovative Approach to Embolization of Pelvic Varices Using Endovaginal Guidance: Methodology and Early Outcomes †
Abstract
1. Introduction
2. Materials and Methods
2.1. Patients
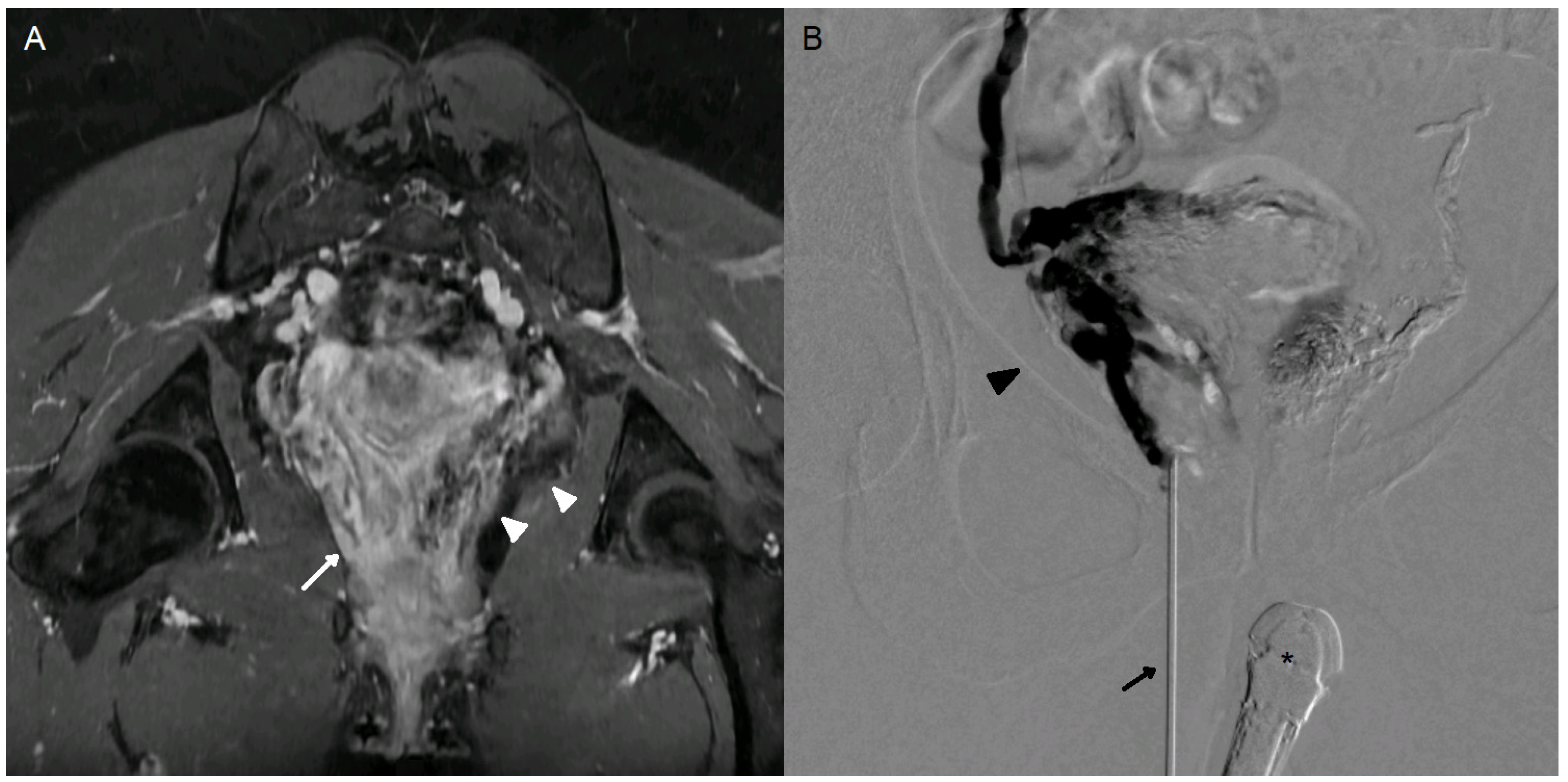
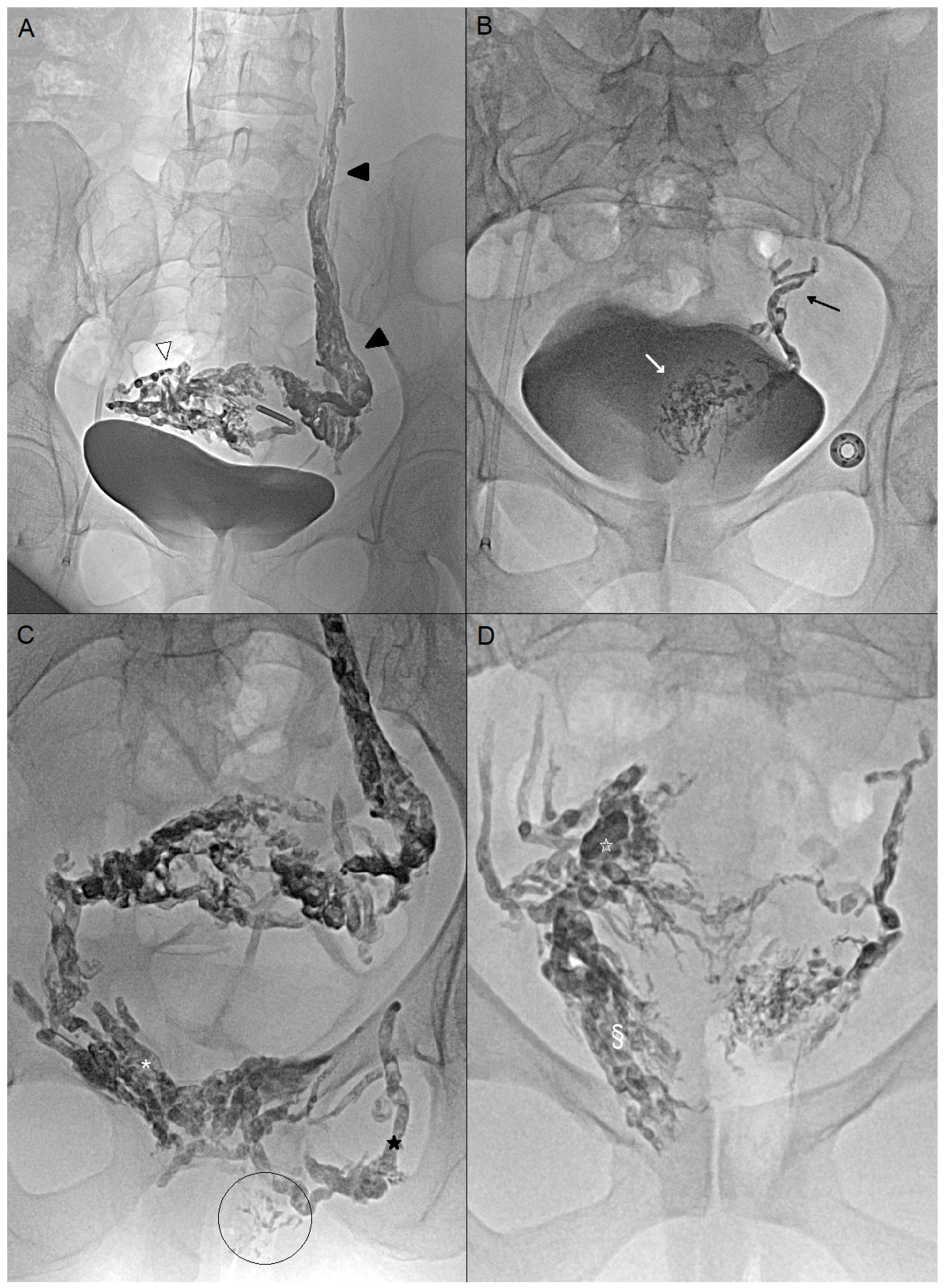
2.2. Procedure
2.3. Efficacy
2.4. Safety
2.4.1. Contrast Volume and Radiation Exposure Were Recorded
2.4.2. Clinical and Imaging Follow-Up
2.4.3. Statistical Analysis
3. Results
3.1. Patients
3.2. Procedure Safety and Technical Success
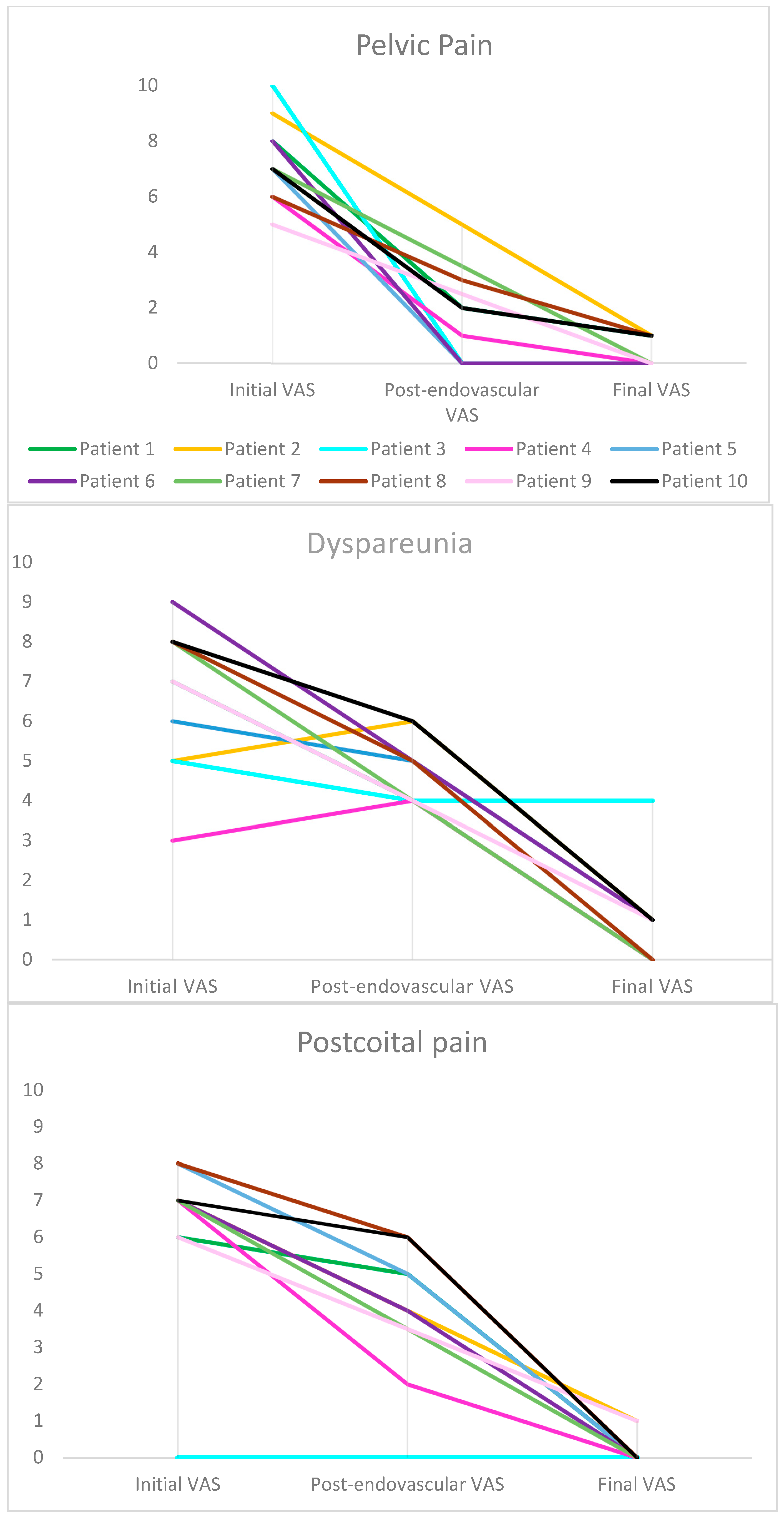
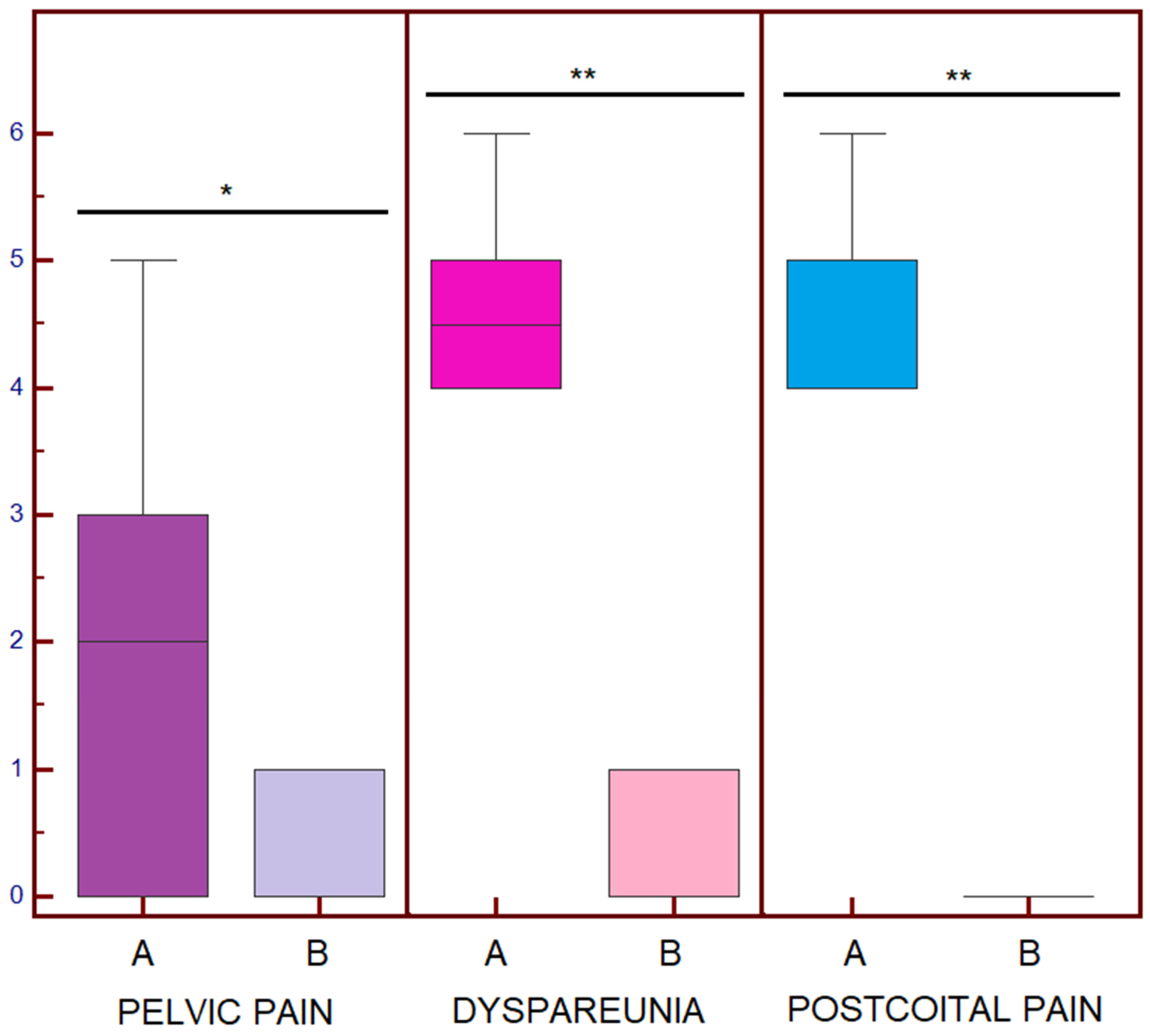
3.3. Primary Efficacy and Outcomes
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| VAS | Visual Analogue Scale |
| EVOH | Ethylene vinyl alcohol copolymer |
| DMSO | Dimethyl sulfoxide |
References
- Pennec, V.L.; Douane, F.; Brun, J.L.; Thouveny, F.; Martinelli, T.; Bravetti, M.; Mastier, C.; Le Bras, Y.; Rogopoulos, A.; Barral, P.A.; et al. Endovascular management of pelvic congestion syndrome: An expert consensus statement from the French Society of Cardiovascular Imaging (SFICV), Interventional Radiology Federation (FRI), College of French Radiology Teachers (CERF), and French Society of Women’s Imaging (SIFEM). Diagn. Interv. Imaging 2025, 106, 356–366. [Google Scholar] [CrossRef] [PubMed]
- Bergan, J.J.; Schmid-Schönbein, G.W.; Smith, P.D.C.; Nicolaides, A.N.; Boisseau, M.R.; Eklof, B. Chronic venous disease. N. Engl. J. Med. 2006, 355, 488–498. [Google Scholar] [CrossRef] [PubMed]
- Danziger, N. Pathophysiology of pain in venous disease. J. Mal. Vasc. 2007, 32, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Jambon, E.; Le Bras, Y.; Coussy, A.; Petitpierre, F.; Hans, H.; Lasserre, A.; Cazalas, G.; Grenier, N.; Marcelin, C. Embolization in pelvic venous disorders using ethylene vinyl alcohol copolymer (Onyx®) and Aetoxysclerol: A prospective evaluation of safety and long-term efficacy. Eur. Radiol. 2022, 32, 4679–4686. [Google Scholar] [CrossRef] [PubMed]
- Loffroy, R. Rationale for Adding Occlusive Liquid Polymers to Coils When Embolizing the Pelvic Reservoir in Pelvic Venous Disorders. Ann. Vasc. Surg. 2025, 115, 1–2. [Google Scholar] [CrossRef] [PubMed]
- Leiber, L.; Thouveny, F.; Bouvier, A.; Labriffe, M.; Berthier, E.; Aubé, C.; Willoteaux, S. MRI and venographic aspects of pelvic venous insufficiency. Diagn. Interv. Imaging 2014, 95, 1091–1102. [Google Scholar] [CrossRef] [PubMed]
- Bookwalter, C.A.; VanBuren, W.M.; Neisen, M.J.; Bjarnason, H. Imaging Appearance and Nonsurgical Management of Pelvic Venous Congestion Syndrome. RadioGraphics 2019, 39, 596–608. [Google Scholar] [CrossRef] [PubMed]
- Pitoulias, A.G.; Andrioti Petropoulou, N.; Bontinis, V.; Chatzelas, D.A.; Bontinis, A.; Thano, A.; Pitoulias, G.A. Ultrasonography in the diagnosis of pelvic vein insufficiency, a systematic review and meta-analysis. Phlebology 2025, 40, 386–394. [Google Scholar] [CrossRef] [PubMed]
- Guimaraes, M.; Wooster, M. Onyx (Ethylene-vinyl Alcohol Copolymer) in Peripheral Applications. Semin. Interv. Radiol. 2011, 28, 350–356. [Google Scholar] [CrossRef] [PubMed]
- Raissi, D.; Yu, Q.; Mardini, S.H. Upper Gastrointestinal Bleed Embolization with Onyx®: The “Tattoo Effect”. J. Clin. Imaging Sci. 2018, 8, 46. [Google Scholar] [CrossRef] [PubMed]
- Laborda, A.; Medrano, J.; de Blas, I.; Urtiaga, I.; Carnevale, F.C.; de Gregorio, M.A. Endovascular treatment of pelvic congestion syndrome: Visual analog scale (VAS) long-term follow-up clinical evaluation in 202 patients. Cardiovasc. Interv. Radiol. 2013, 36, 1006–1014. [Google Scholar] [CrossRef] [PubMed]
- Senechal, Q.; Echegut, P.; Bravetti, M.; Florin, M.; Jarboui, L.; Bouaboua, M.; Teriitehau, C.; Feignoux, J.; Legou, F.; Pessis, E. Endovascular Treatment of Pelvic Congestion Syndrome: Visual Analog Scale Follow-Up. Front. Cardiovasc. Med. 2021, 8, 751178. [Google Scholar] [CrossRef] [PubMed]
- Kim, A.S.; Greyling, L.A.; Davis, L.S. Vulvar Varicosities: A Review. Dermatol. Surg. 2017, 43, 351–356. [Google Scholar] [CrossRef] [PubMed]
- Gavrilov, S.G. Vulvar varicosities: Diagnosis, treatment, and prevention. Int. J. Womens Health 2017, 9, 463–475. [Google Scholar] [CrossRef] [PubMed]
- Beard, R.W.; Reginald, P.W.; Wadsworth, J. Clinical features of women with chronic lower abdominal pain and pelvic congestion. BJOG: Int. J. Obstet. Gynaecol. 1988, 95, 153–161. [Google Scholar] [CrossRef] [PubMed]
- Herrera-Betancourt, A.L.; Villegas-Echeverri, J.D.; López-Jaramillo, J.D.; López-Isanoa, J.D.; Estrada-Alvarez, J.M. Sensitivity and specificity of clinical findings for the diagnosis of pelvic congestion syndrome in women with chronic pelvic pain. Phlebology 2018, 33, 303–308. [Google Scholar] [CrossRef] [PubMed]
- Meissner, M.H.; Khilnani, N.M.; Labropoulos, N.; Gasparis, A.P.; Gibson, K.; Greiner, M.; Learman, L.A.; Atashroo, D.; Lurie, F.; Passman, M.A.; et al. The Symptoms-Varices-Pathophysiology classification of pelvic venous disorders: A report of the American Vein & Lymphatic Society International Working Group on Pelvic Venous Disorders. Phlebol. J. Venous Dis. 2021, 36, 342–360. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Valero, I.; Garcia-Jimenez, R.; Valdevieso, P.; Garcia-Mejido, J.A.; Gonzalez-Herráez, J.V.; Pelayo-Delgado, I.; Fernandez-Palacin, A.; Sainz-Bueno, J.A. Identification of Pelvic Congestion Syndrome Using Transvaginal Ultrasonography. A Useful Tool. Tomography 2022, 8, 89–99. [Google Scholar] [CrossRef] [PubMed]
- Hansrani, V.; Dhorat, Z.; McCollum, C.N. Diagnosing of pelvic vein incompetence using minimally invasive ultrasound techniques. Vascular 2017, 25, 253–259. [Google Scholar] [CrossRef] [PubMed]

| N | Age (Years) | G-P | Duration Pain (Years) | Initial VAS | Embolized Veins * | Post-Endovascular VAS | Final VAS | Perivaginal Veins Size (mm) |
|---|---|---|---|---|---|---|---|---|
| 1 | 33 | G2P2 | 8 | 8-7-6 | LOV ROV RPV | 2-4-5 | 1-0-0 | 4 |
| 2 | 37 | G3P3 | 7 | 9-5-7 | LOV ObV RVV | 5-6-4 | 2-1-1 | 3 |
| 3 | 39 | G6P4 | 3 | 10-5-0 | LOV UV PV | 0-4-0 | 0-4-0 | 2 |
| 4 | 45 | G3P2 | 15 | 6-3-7 | LOV LVV | 1-4-2 | 0-0-0 | 5 |
| 5 | 32 | G2P2 | 1 | 7-6-8 | LOV ROV LUV | 0-5-5 | 0-1-0 | 4 |
| 6 | 35 | G1P1 | 3 | 8-9-7 | LUV LVV | 0-5-4 | 0-1-0 | 4 |
| 7 | 23 | G0P0 | 3 | 7-8-7 | NA | N/A | 0-0-0 | 3 |
| 8 | 36 | G2P2 | 5 | 6-8-8 | LOV LPV ObV | 3-5-6 | 1-0-0 | 3 |
| 9 | 40 | G4P2 | 8 | 5-7-6 | LOV | N/A | 0-1-1 | 4 |
| 10 | 32 | G2P1 | 5 | 7-8-7 | LOV ROV LUV PV | 2-6-6 | 1-1-0 | 3 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Fourage-Jambon, E.; Soueidan, R.; Sawalha, H.; Lamfichekh, Y.; Linares, B.; Hans, H.; David, M.; Molina-Andreo, I.; Douchez, C.; Pangon, N.; et al. Innovative Approach to Embolization of Pelvic Varices Using Endovaginal Guidance: Methodology and Early Outcomes. J. Pers. Med. 2025, 15, 500. https://doi.org/10.3390/jpm15100500
Fourage-Jambon E, Soueidan R, Sawalha H, Lamfichekh Y, Linares B, Hans H, David M, Molina-Andreo I, Douchez C, Pangon N, et al. Innovative Approach to Embolization of Pelvic Varices Using Endovaginal Guidance: Methodology and Early Outcomes. Journal of Personalized Medicine. 2025; 15(10):500. https://doi.org/10.3390/jpm15100500
Chicago/Turabian StyleFourage-Jambon, Eva, Rayann Soueidan, Hamza Sawalha, Yassine Lamfichekh, Benjamin Linares, Hugo Hans, Mathieu David, Isabelle Molina-Andreo, Charlotte Douchez, Nicolas Pangon, and et al. 2025. "Innovative Approach to Embolization of Pelvic Varices Using Endovaginal Guidance: Methodology and Early Outcomes" Journal of Personalized Medicine 15, no. 10: 500. https://doi.org/10.3390/jpm15100500
APA StyleFourage-Jambon, E., Soueidan, R., Sawalha, H., Lamfichekh, Y., Linares, B., Hans, H., David, M., Molina-Andreo, I., Douchez, C., Pangon, N., Le Bras, Y., Maaloum, R., & Marcelin, C. (2025). Innovative Approach to Embolization of Pelvic Varices Using Endovaginal Guidance: Methodology and Early Outcomes. Journal of Personalized Medicine, 15(10), 500. https://doi.org/10.3390/jpm15100500






