Child–Pugh Class and Not Thrombocytopenia Impacts the Risk of Complications of Endoscopic Band Ligation in Patients with Cirrhosis and High Risk Varices
Abstract
:1. Introduction
2. Patients and Methods
3. Statistical Analysis
4. Results
5. Discussion
Author Contributions
Funding
Data Availability Statement
Conflicts of Interest
Abbreviations
References
- Reverter, E.; Tandon, P.; Augustin, S.; Turon, F.; Casu, S.; Bastiampillai, R.; Keough, A.; Llop, E.; González, A.; Seijo, S.; et al. A MELD-based model to determine risk of mortality among patients with acute variceal bleeding. Gastroenterology 2014, 146, 412–419.e3. [Google Scholar] [CrossRef] [PubMed]
- Garcia-Tsao, G.; Abraldes, J.G.; Berzigotti, A.; Bosch, J. Portal hypertensive bleeding in cirrhosis: Risk stratification, diagnosis, and management: 2016 practice guidance by the American Association for the study of liver diseases. Hepatology 2017, 65, 310–335. [Google Scholar] [CrossRef] [PubMed]
- Tripathi, D.; Stanley, A.J.; Hayes, P.C.; Patch, D.; Millson, C.; Mehrzad, H.; Austin, A.; Ferguson, J.W.; Olliff, S.P.; Hudson, M.; et al. UK guidelines on the management of variceal haemorrhage in cirrhotic patients. Gut 2015, 64, 1680–1704. [Google Scholar] [CrossRef] [PubMed]
- Sinclair, M.; Vaughan, R.; Angus, P.W.; Gow, P.J.; Parker, F.; Hey, P.; Efthymiou, M. Risk factors for band-induced ulcer bleeding after prophylactic and therapeutic endoscopic variceal band ligation. Eur. J. Gastroenterol. Hepatol. 2015, 27, 928–932. [Google Scholar] [CrossRef] [PubMed]
- Dueñas, E.; Cachero, A.; Amador, A.; Rota, R.; Salord, S.; Gornals, J.; Xiol, X.; Castellote, J. Ulcer bleeding after band ligation of esophageal varices: Risk factors and prognosis. Dig. Liver Dis. 2020, 52, 79–83. [Google Scholar] [CrossRef] [PubMed]
- Northup, P.G.; Garcia-Pagan, J.C.; Garcia-Tsao, G.; Intagliata, N.M.; Superina, R.A.; Roberts, L.N.; Lisman, T.; Valla, D.C. Vascular liver disorders, portal vein thrombosis, and procedural bleeding in patients with liver disease: 2020 practice guidance by the American association for the study of liver diseases. Hepatology 2021, 73, 366–413. [Google Scholar] [CrossRef] [PubMed]
- Slichter, S.J. Relationship between platelet count and bleeding risk in thrombocytopenic patients. Transfus. Med. Rev. 2004, 18, 153–167. [Google Scholar] [CrossRef] [PubMed]
- Khuroo, M.S.; Farahat, K.L.C.; Sofi, A.A.; Dahab, S.T. Meta-analysis: Endoscopic variceal ligation for primary prophylaxis of oesophageal variceal bleeding. Aliment Pharmacol. Ther. 2005, 21, 347–361. [Google Scholar] [CrossRef] [PubMed]
- Singh, P.; Pooran, N.; Indaram, A.; Bank, S. Combined ligation and sclerotherapy versus ligation alone for secondary prophylaxis of esophageal variceal bleeding: A meta analysis. Am. J. Gastroenterol. 2002, 97, 623–662. [Google Scholar] [CrossRef] [PubMed]
- Triantos, C.; Kalafateli, M. Endoscopic treatment of esophageal varices in patients with liver cirrhosis. World J. Gastroenterol. 2014, 20, 13015–13026. [Google Scholar] [CrossRef] [PubMed]
- da Rocha, E.C.V.; D’Amico, E.A.; Caldwell, S.H.; da Rocha, T.R.F.; Silva, C.S.S.S.E.; Bomfim, V.D.S.; Felga, G.; Barbosa, W.F.; Kassab, F.; Polli, D.A.; et al. A prospective study of conventional and expanded coagulation indices in predicting ulcer bleeding after variceal band ligation. Clin. Gastroenterol. Hepatol. 2009, 7, 988–993. [Google Scholar] [CrossRef] [PubMed]
- De Pietri, L.; Bianchini, M.; Montalti, R.; De Maria, N.; Di Maira, T.; Begliomini, B.; Gerunda, G.E.; di Benedetto, F.; Garcia-Tsao, G.; Villa, E. Thrombelastography-guided blood product use before invasive procedures in cirrhosis with severe coagulopathy: A randomized, controlled trial. Hepatology 2016, 63, 566–573. [Google Scholar] [CrossRef] [PubMed]
- De Pietri, L.; Bianchini, M.; Rompianesi, G.; Bertellini, E.; Begliomini, B. Thromboelastographic reference ranges for a cirrhotic patient population undergoing liver transplantation. World J. Transplant. 2016, 6, 583–593. [Google Scholar] [CrossRef] [PubMed]
- Blasi, A.; Machlab, S.; Risco, R.; Costa-Freixas, J.P.; Hernández-Cely, G.; Horta, D.; Bofill, A.; Ruiz-Ramirez, P.; Profitos, J.; Sanahuja, J.M.; et al. A multicenter analysis of the role of prophylactic transfusion of blood products in patients with cirrhosis and esophageal varices undergoing endoscopic band ligation. JHEP Rep. 2021, 3, 100363. [Google Scholar] [CrossRef] [PubMed]
| Patients (Tot: 431) | |
|---|---|
| Age, y ± SD | 62.7 ± 12.7 |
| Sex M, n (%) | 281 (65.2%) |
| INR ± SD | 1.2 ± 0.3 |
| Bilirubin mg/dL ± SD | 1.5 ± 1.5 |
| Albumin g/dL ± SD | 3.3 ± 0.6 |
| Creatinie mg/dL | 0.7 ± 0.6 |
| Platelets/mm3 | 92,272 ± 83,320 |
| Child–Pugh (median) | 6 |
| A | 281 (65.2%) |
| B | 134 (31.1%) |
| C | 16 (3.7%) |
| Etiology n (%) | |
| Viral | 238 (55.2) |
| - ASH | 40 (9.3) |
| - NASH | 61 (14.2) |
| - Autoimmune hepatitis | 15 (3.5) |
| - ASH + viral | 7 (1.6) |
| Other | 70 (16.2) |
| Portal vein diameter, mm ± SD | 13.0 ± 0.85 |
| Spleen LD, cm ± SD | 16.1 ± 0.7 |
| - Liver events, n (%) | |
| - Ascites n (%) | 183 (42.5) |
| - Mild | 62 (14.4) |
| - Moderate | 82 (19) |
| - Severe | 39 (9) |
| Pleural effusion n (%) | 22 (5) |
| - HE n (%) | 27 (6.3) |
| - Portal vein thrombosis n (%) | 72 (16.7) |
| HCC n (%) | 73 (17) |
| Antithrombotic therapy | 38 (8.8) |
| Antiplatelets (ASA or cropidogrel) | 13 (3.0) |
| LMWH | 19 (4.4) |
| Warfarin | 6 (1.4) |
| Esophageal Varices n (%) | |
|---|---|
| - F2 | 130 (30) |
| - (F2 occ—dim, median) | 40–40 |
| - F2 red marks | 48 (11) |
| - (F2 red marks occ—dim, median) | 40–50 |
| - F3 | 81 (18.8) |
| - (F3 occ—dim, median) | 60–70 |
| - F3 red marks | 172 (39.9) |
| - (F3 red marks occ—dim, median) | 70–80 |
| Gastric varices n (%) | 76 (17.6) |
| Gov1 | 47 (10.9) |
| Gov2 | 15 (3.5) |
| Igv1 | 9 (2) |
| Igv2 | 3 (0.7) |
| Other GV | 5 (1.2) |
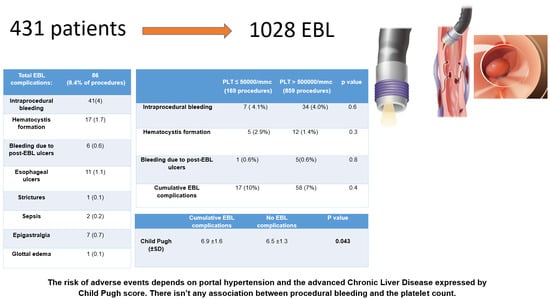
| Complications | EBL Number (%) |
|---|---|
| Total | 86 (8.4) |
| Intraprocedural bleeding | 41(4) |
| Need for intervention | 6 (14.6) |
| Hematocystic spots’ formation | 17 (1.7) |
| Bleeding due to post-EBL ulcers | 6 (0.6) |
| Esophageal ulcers | 11 (1.1) |
| Strictures | 1 (0.1) |
| Sepsis | 2 (0.2) |
| Epigastralgia | 7 (0.7) |
| Glottal edema | 1 (0.1) |
| Intraprocedural Bleeding (41) | No Bleeding (987) | p Value | |
|---|---|---|---|
| EV n(%) | 0.5 | ||
| F2 | 16 (39) | 389 (39.4) | |
| F3 | 25 (61) | 598 (60.6) | |
| PLT mean | 80,948.00 ± 37.658 | 87,837.00 ± 75.729 | 0.5 |
| PLT ≥ 50,000 | 34 (83) | 825 (83.6) | |
| PLT < 50,000 | 7 (17.0) | 162 (16.4) | 0.6 |
| Bands N | 5.1 ± 1.3 | 5.2 ± 1.5 | 0.7 |
| Antithrombotic drugs | 2 (4.9) | 36 (3.6) | 0.7 |
| MELD | 8.3 ± 4.7 | 8.4 ± 3.4 | 0.8 |
| CP | 6.8 ± 1.8 | 6.5 ± 1.5 | 0.3 |
| Hematocystic Spots (17) | No Hematocystic Spots (1011) | p Value | |
|---|---|---|---|
| EV n (%) | 0.019 | ||
| F2 | 12 (70) | 394 (39) | |
| F3 | 5 (30) | 617 (61) | |
| Mean PLT ± SD | 79,250.00 ± 44,713 | 87,170 ± 74,825 | 0.7 |
| PLT < 50,000 | 5 (29.4%) | 164 (16.2%) | 0.3 |
| N bands ± SD | 5.3 ± 1.1 | 5.2 ± 1.5 | 0.7 |
| Antithrombotic drugs | 1 (5.9) | 37 (3.7) | 0.5 |
| MELD ± SD | 8.4 ± 2.8 | 8.4 ± 3.5 | 0.9 |
| CP ± SD | 6.8 ± 1.1 | 6.5 ± 1.3 | 0.5 |
| Bleeding Due to Post-EBL Ulcers (6) | No Bleeding Due to Post-EBL Ulcers (1022) | p Value | |
|---|---|---|---|
| EV n (%) | 0.2 | ||
| F2 | 4 (66.6) | 402 (39.3) | |
| F3 | 2 (33.4) | 620 (60.7) | |
| PLT mean ± SD | 125,666.00 ew ± 112,384 | 87,217 ± 74,011 | 0.4 |
| PLT < 50.000 | 1 (16.7) | 168 (16.4) | 0.08 |
| Bands N ± SD | 5.8 ± 1.6 | 5.2 ± 1.5 | 0.3 |
| Antithrombotic drugs | 0 | 38 (3.7) | 0.9 |
| MELD ± SD | 8.5 ± 3 | 8.4 ± 3.5 | 0.9 |
| CP ± SD | 6.8 ± 1.6 | 6.5 ± 1.4 | 0.73 |
| Cumulative Events (75) | No Events (953) | p Value | |
|---|---|---|---|
| EV n (%) | 0.2 | ||
| F2 | 35 (46.7) | 372 (39) | |
| F3 | 40 (53.3) | 581 (61) | |
| PLT mean ± DS | 84,235 ± 54,175 | 77,804 ± 75,949 | 0.7 |
| PLT < 50,000 pl | 17 (22.7%) | 152 (15.9%) | 0.4 |
| Bands N. ± SD | 5.1 ± 1.6 | 5.2 ± 1.5 | 0.8 |
| Antithrombotic drugs | 3 (4) | 35 (3.7) | 0.7 |
| MELD ± SD | 8.5 ± 4.2 | 8.4 ± 3.4 | 0.9 |
| CP ± SD | 6.9 ± 1.6 | 6.5 ± 1.3 | 0.043 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Di Martino, V.; Simone, F.; Grasso, M.; Abdel-Hadi, Y.; Peralta, M.; Veneziano, M.; Lombardo, A.; Peralta, S.; Calvaruso, V. Child–Pugh Class and Not Thrombocytopenia Impacts the Risk of Complications of Endoscopic Band Ligation in Patients with Cirrhosis and High Risk Varices. J. Pers. Med. 2023, 13, 764. https://doi.org/10.3390/jpm13050764
Di Martino V, Simone F, Grasso M, Abdel-Hadi Y, Peralta M, Veneziano M, Lombardo A, Peralta S, Calvaruso V. Child–Pugh Class and Not Thrombocytopenia Impacts the Risk of Complications of Endoscopic Band Ligation in Patients with Cirrhosis and High Risk Varices. Journal of Personalized Medicine. 2023; 13(5):764. https://doi.org/10.3390/jpm13050764
Chicago/Turabian StyleDi Martino, Vincenzo, Fabio Simone, Maria Grasso, Yasmin Abdel-Hadi, Marco Peralta, Marzia Veneziano, Antonino Lombardo, Sergio Peralta, and Vincenza Calvaruso. 2023. "Child–Pugh Class and Not Thrombocytopenia Impacts the Risk of Complications of Endoscopic Band Ligation in Patients with Cirrhosis and High Risk Varices" Journal of Personalized Medicine 13, no. 5: 764. https://doi.org/10.3390/jpm13050764
APA StyleDi Martino, V., Simone, F., Grasso, M., Abdel-Hadi, Y., Peralta, M., Veneziano, M., Lombardo, A., Peralta, S., & Calvaruso, V. (2023). Child–Pugh Class and Not Thrombocytopenia Impacts the Risk of Complications of Endoscopic Band Ligation in Patients with Cirrhosis and High Risk Varices. Journal of Personalized Medicine, 13(5), 764. https://doi.org/10.3390/jpm13050764