The Real Post-Operative Range of Motion Differs from the Virtual Pre-Operative Planned Range of Motion in Reverse Shoulder Arthroplasty
Abstract
1. Introduction
2. Materials and Methods
2.1. Ethics
2.2. Patients and Implants
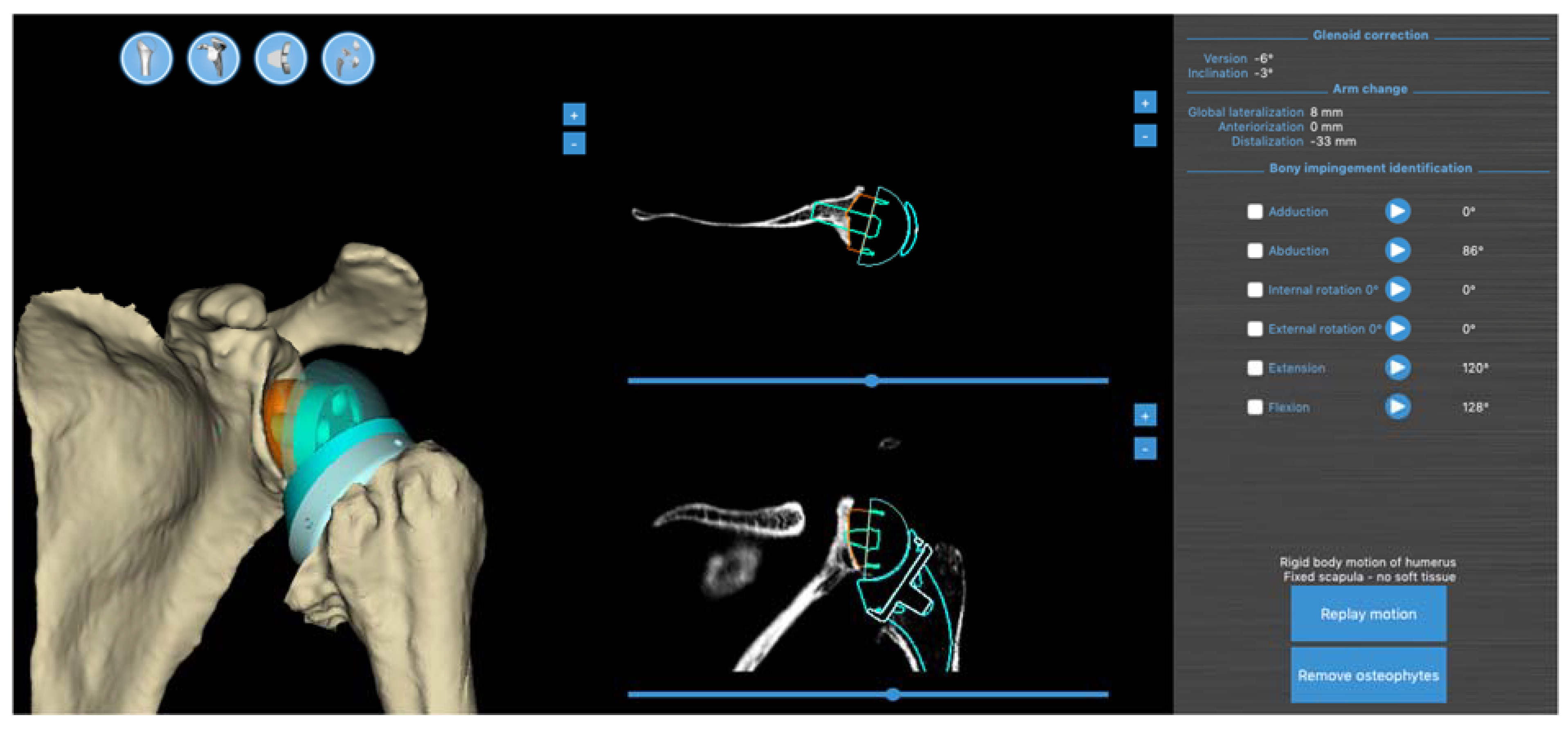
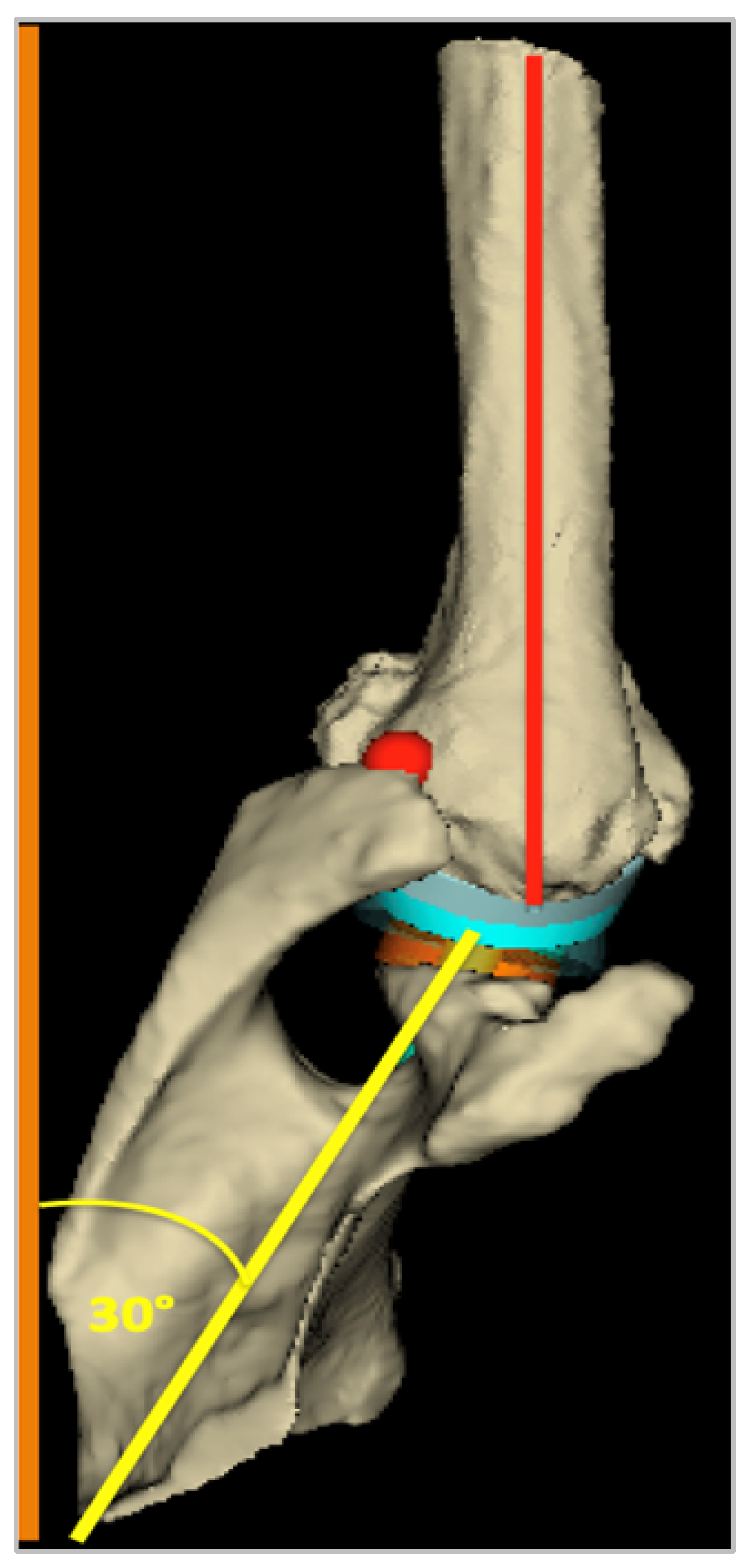
2.3. D Pre-Operative Planning Software
2.4. Study Protocol
- After the usual pre-operative evaluation (clinical exam, X-ray, and CT scan), the RSA procedure was performed for each patient;
- At a minimum follow-up of 18 months, a post-operative CT scan was performed for each patient using the acquisition characteristics required by the BluePrint® 3D Planning software, in addition to the routine clinical and radiological assessments, which were conducted by a single surgeon;
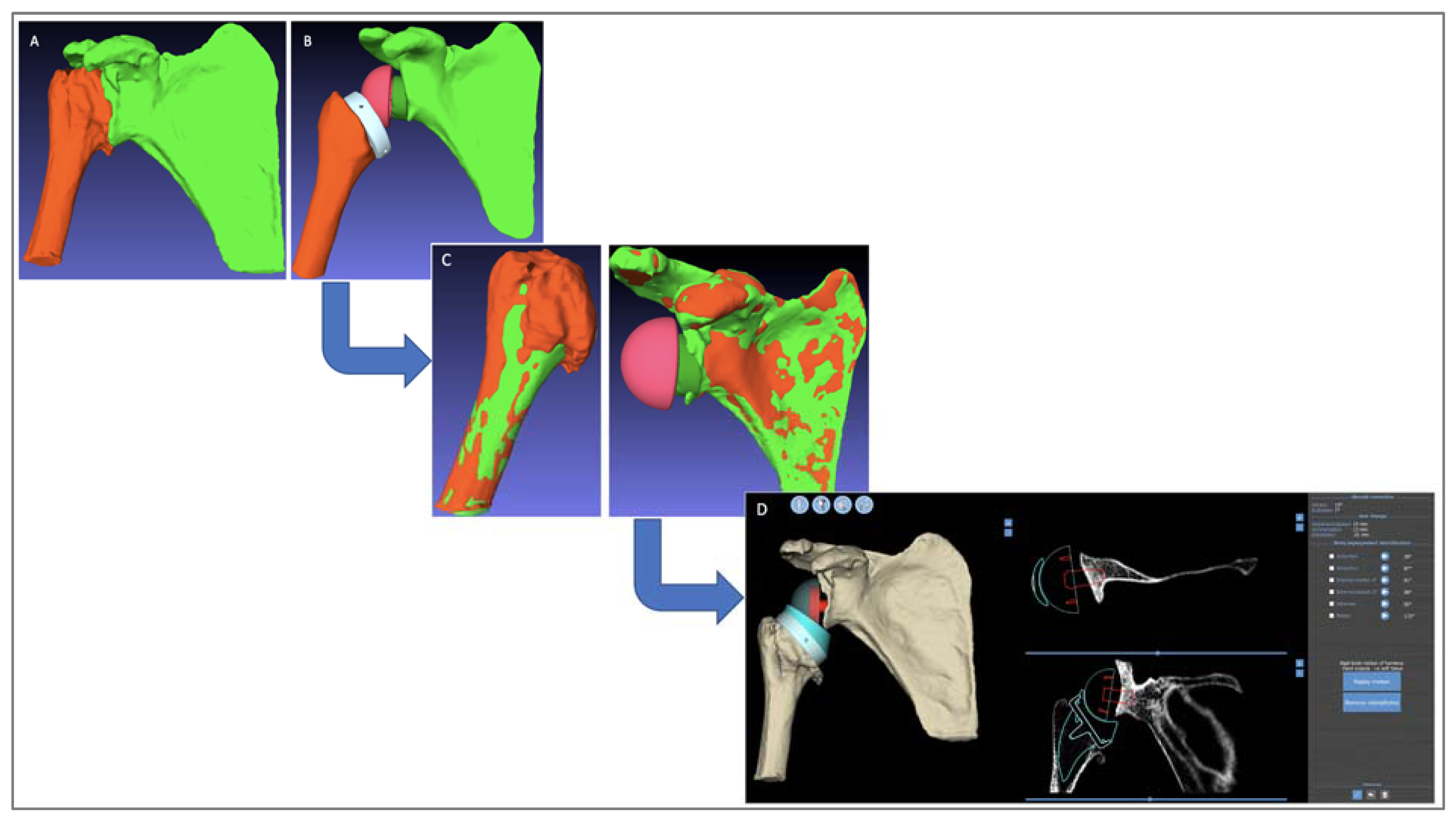
- For all shoulders, the planning software’s automated segmentation algorithm was used to extract the pre-operative humerus and scapula 3D models from the pre-operative CTs (Figure 3A);
- On all the post-operative CTs, the humerus, scapula, and implants were segmented manually (Figure 3B);
- Registration and superposition were performed between the pre- and post-operative bony structures using the PTC Creo® Version 6.0 software (Parametric Technology Corporation, Needham, MA, USA) (Figure 3C);
- A software program that takes the registration data and generates “post-operative planning” files equivalent to the real post-operative implant positioning was developed;
- Surgeons could open the post-operative planning file and access all BluePrint® 3D Planning software measurements, in particular, the RoM analysis (Figure 3D).
2.5. Clinical and Radiological Assessment Criteria
2.6. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Bacle, G.; Nove-Josserand, L.; Garaud, P.; Walch, G. Long-Term Outcomes of Reverse Total Shoulder Arthroplasty: A Follow-up of a Previous Study. J. Bone Jt. Surg. Am. 2017, 99, 454–461. [Google Scholar] [CrossRef]
- Arenas-Miquelez, A.; Murphy, R.J.; Rosa, A.; Caironi, D.; Zumstein, M.A. Impact of humeral and glenoid component variations on range of motion in reverse geometry total shoulder arthroplasty: A standardized computer model study. J. Shoulder Elb. Surg. 2021, 30, 763–771. [Google Scholar] [CrossRef]
- Mollon, B.; Mahure, S.A.; Roche, C.P.; Zuckerman, J.D. Impact of scapular notching on clinical outcomes after reverse total shoulder arthroplasty: An analysis of 476 shoulders. J. Shoulder Elb. Surg. 2017, 26, 1253–1261. [Google Scholar] [CrossRef]
- Lädermann, A.; Denard, P.J.; Collin, P.; Zbinden, O.; Chiu, J.C.-H.; Boileau, P.; Olivier, F.; Walch, G. Effect of humeral stem and glenosphere designs on range of motion and muscle length in reverse shoulder arthroplasty. Int. Orthop. 2020, 44, 519–530. [Google Scholar] [CrossRef]
- Werner, B.S.; Hudek, R.; Burkhart, K.J.; Gohlke, F. The influence of three-dimensional planning on decision-making in total shoulder arthroplasty. J. Shoulder Elb. Surg. 2017, 26, 1477–1483. [Google Scholar] [CrossRef] [PubMed]
- Berhouet, J.; Gulotta, L.; Dines, D.; Craig, E.; Warren, R.; Choi, D.; Chen, X.; Kontaxis, A. Preoperative planning for accurate glenoid component positioning in reverse shoulder arthroplasty. Orthop. Traumatol. Surg. Res. 2017, 103, 407–413. [Google Scholar] [CrossRef]
- Lädermann, A.; Tay, E.; Collin, P.; Piotton, S.; Chiu, C.-H.; Michelet, A.; Charbonnier, C. Effect of critical shoulder angle, glenoid lateralization, and humeral inclination on range of movement in reverse shoulder arthroplasty. Bone Jt. Res. 2019, 8, 378–386. [Google Scholar] [CrossRef] [PubMed]
- Werner, B.S.; Chaoui, J.; Walch, G. Glenosphere design affects range of movement and risk of friction-type scapular impingement in reverse shoulder arthroplasty. Bone Jt. J. 2018, 100-B, 1182–1186. [Google Scholar] [CrossRef] [PubMed]
- Blaimont, P.; Taheri, A.; Vanderhofstadt, A. Displacement of the instantaneous center of rotation of the humeral head during abduction: Implication for scapulohumeral muscular function. Rev. Chir. Orthop. Reparatrice L'appareil Mot. 2005, 91, 399–406. [Google Scholar] [CrossRef]
- Kwon, Y.W.; Pinto, V.J.; Yoon, J.; Frankle, M.A.; Dunning, P.E.; Sheikhzadeh, A. Kinematic analysis of dynamic shoulder motion in patients with reverse total shoulder arthroplasty. J. Shoulder Elb. Surg. 2012, 21, 1184–1190. [Google Scholar] [CrossRef]
- Terrier, A.; Scheuber, P.; Pioletti, D.P.; Farron, A. Activities of daily living with reverse prostheses: Importance of scapular compensation for functional mobility of the shoulder. J. Shoulder Elb. Surg. 2013, 22, 948–953. [Google Scholar] [CrossRef]
- Boileau, P.; Walch, G.; Liotard, J.P. Radio-cinematographic study of active elevation of the prosthetic shoulder. Rev. Chir. Orthop. Reparatrice L'appareil Mot. 1992, 78, 355–364. [Google Scholar]
- Moroder, P.; Urvoy, M.M.; Raiss, P.; Werthel, J.-D.; Akgün, D.; Chaoui, J.; Siegert, P. Patient Posture Affects Simulated ROM in Reverse Total Shoulder Arthroplasty: A Modeling Study Using Preoperative Planning Software. Clin. Orthop. Relat. Res. 2022, 480, 619–631. [Google Scholar] [CrossRef] [PubMed]
- Marcoin, A.; Nerot, C.; Lestra, T.; Blasco, L.; Ferrier, A.; Siboni, R.; Ohl, X. The precision of patient-specific instrumentation guides for the positioning of the glenoid component in total reverse shoulder arthroplasty: An in vivo scanographic study. Int. Orthop. 2020, 44, 1761–1766. [Google Scholar] [CrossRef]
- Boileau, P.; Cheval, D.; Gauci, M.O.; Holzer, N.; Chaoui, J.; Walch, G. Automated Three-Dimensional Measurement of Glenoid Version and Inclination in Arthritic Shoulders. J. Bone Joint Surg Am. 2018, 100, 57–65. [Google Scholar] [CrossRef]
- Walch, G.; Vezeridis, P.S.; Boileau, P.; Deransart, P.; Chaoui, J. Three-dimensional planning and use of patient-specific guides improve glenoid component position: An in vitro study. J. Shoulder Elbow Surg. 2015, 24, 302–309. [Google Scholar] [CrossRef] [PubMed]
- Falaise, V.; Levigne, C.; Favard, L. Scapular notching in reverse shoulder arthroplasties: The influence of glenometaphyseal angle. Orthop. Traumatol. Surg. Res. 2011, 97 (Suppl. S6), S131–S137. [Google Scholar] [CrossRef]
- Alta, T.D.; de Toledo, J.M.; Veeger, D.; Janssen, T.; Willems, W.J. The active and passive kinematic difference between primary reverse and total shoulder prostheses. J. Shoulder Elb. Surg. 2014, 23, 1395–1402. [Google Scholar] [CrossRef]
- Maier, M.W.; Caspers, M.; Zeifang, F.; Dreher, T.; Klotz, M.C.; Wolf, S.I.; Kasten, P. How does reverse shoulder replacement change the range of motion in activities of daily living in patients with cuff tear arthropathy? A prospective optical 3D motion analysis study. Arch. Orthop. Trauma. Surg. 2014, 134, 1065–1071. [Google Scholar] [CrossRef] [PubMed]
- Poppen, N.; Walker, P. Normal and abnormal motion of the shoulder. J. Bone Jt. Surg. Am. 1976, 58, 195–201. [Google Scholar] [CrossRef]
- Poppen, N.K.; Walker, P.S. Forces at the glenohumeral joint in abduction. Clin. Orthop. Relat. Res. 1978, 135, 165–170. [Google Scholar] [CrossRef]
- Patel, M.; Martin, J.R.; Campbell, D.H.; Fernandes, R.R.; Amini, M.H. Inferior tilt of the glenoid leads to medialization and increases impingement on the scapular neck in reverse shoulder arthroplasty. J. Shoulder Elb. Surg. 2021, 30, 1273–1281. [Google Scholar] [CrossRef] [PubMed]
- Pitocchi, J.; Plessers, K.; Wirix-Speetjens, R.; Debeer, P.; van Lenthe, G.H.; Jonkers, I.; Pérez, M.A.; Sloten, J.V. Automated muscle elongation measurement during reverse shoulder arthroplasty planning. J. Shoulder Elb. Surg. 2021, 30, 561–571. [Google Scholar] [CrossRef] [PubMed]


| Virtual (1) | Real GH (2) | Real GH + ST (3) | p-Value (1 vs. 2) | p-Value (1 vs. 3) | |
|---|---|---|---|---|---|
| Passive Abduction (°) | 80.8 ± 13.6 | 65.6 ± 18.2 | 136.7 ± 27.7 | <0.0001 | <0.0001 |
| Passive Forward Elevation (°) | 90.8 ± 23.1 | 63.3 ± 19.7 | 141.1 ± 23.82 | <0.002 | <0.0001 |
| External rotation arm at side (°) | 24.1 ± 25.6 | 22.1 ± 19.4 | 19.2 ± 12.4 | 0.42 | 0.38 |
| Planning | Post-Operative | p-Value | |
|---|---|---|---|
| Gleno-Metaphyseal Angle (°) | 42.8 ± 15.2 | 29.1 ± 18.2 | <0.0001 |
| GH angle (°) | 85.2 ± 8.8 | 99.5 ± 12.5 | <0.0001 |
| MH angle (°) | 133.3 ± 11.1 | 128.6 ± 12.3 | 0.33 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Berhouet, J.; Samargandi, R.; Favard, L.; Turbillon, C.; Jacquot, A.; Gauci, M.-O. The Real Post-Operative Range of Motion Differs from the Virtual Pre-Operative Planned Range of Motion in Reverse Shoulder Arthroplasty. J. Pers. Med. 2023, 13, 765. https://doi.org/10.3390/jpm13050765
Berhouet J, Samargandi R, Favard L, Turbillon C, Jacquot A, Gauci M-O. The Real Post-Operative Range of Motion Differs from the Virtual Pre-Operative Planned Range of Motion in Reverse Shoulder Arthroplasty. Journal of Personalized Medicine. 2023; 13(5):765. https://doi.org/10.3390/jpm13050765
Chicago/Turabian StyleBerhouet, Julien, Ramy Samargandi, Luc Favard, Céline Turbillon, Adrien Jacquot, and Marc-Olivier Gauci. 2023. "The Real Post-Operative Range of Motion Differs from the Virtual Pre-Operative Planned Range of Motion in Reverse Shoulder Arthroplasty" Journal of Personalized Medicine 13, no. 5: 765. https://doi.org/10.3390/jpm13050765
APA StyleBerhouet, J., Samargandi, R., Favard, L., Turbillon, C., Jacquot, A., & Gauci, M.-O. (2023). The Real Post-Operative Range of Motion Differs from the Virtual Pre-Operative Planned Range of Motion in Reverse Shoulder Arthroplasty. Journal of Personalized Medicine, 13(5), 765. https://doi.org/10.3390/jpm13050765






