Applying Multi-Metric Deformable Image Registration for Dose Accumulation in Combined Cervical Cancer Radiotherapy
Abstract
1. Introduction
2. Materials and Methods
2.1. Patient Data
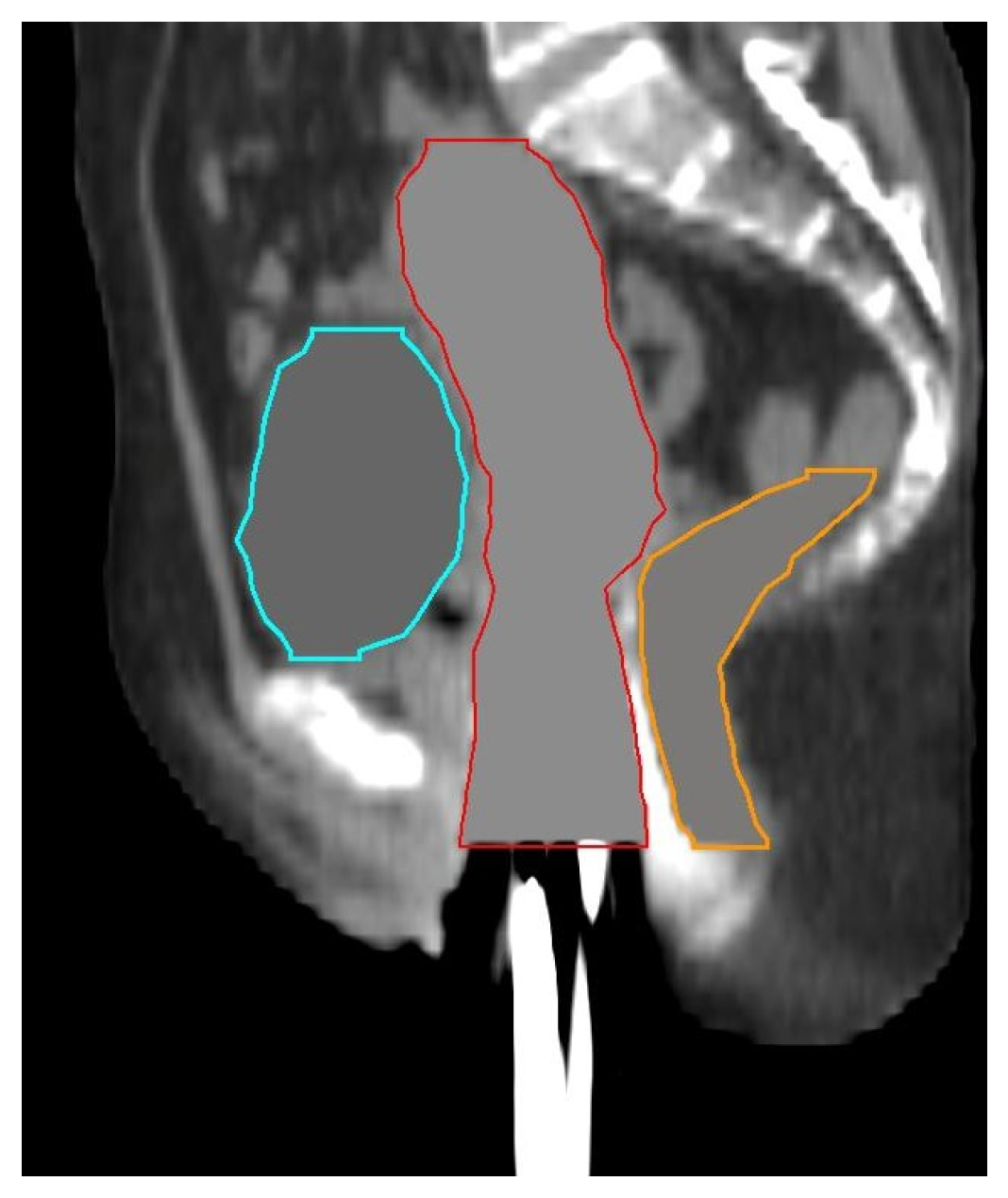
2.2. Preprocessing
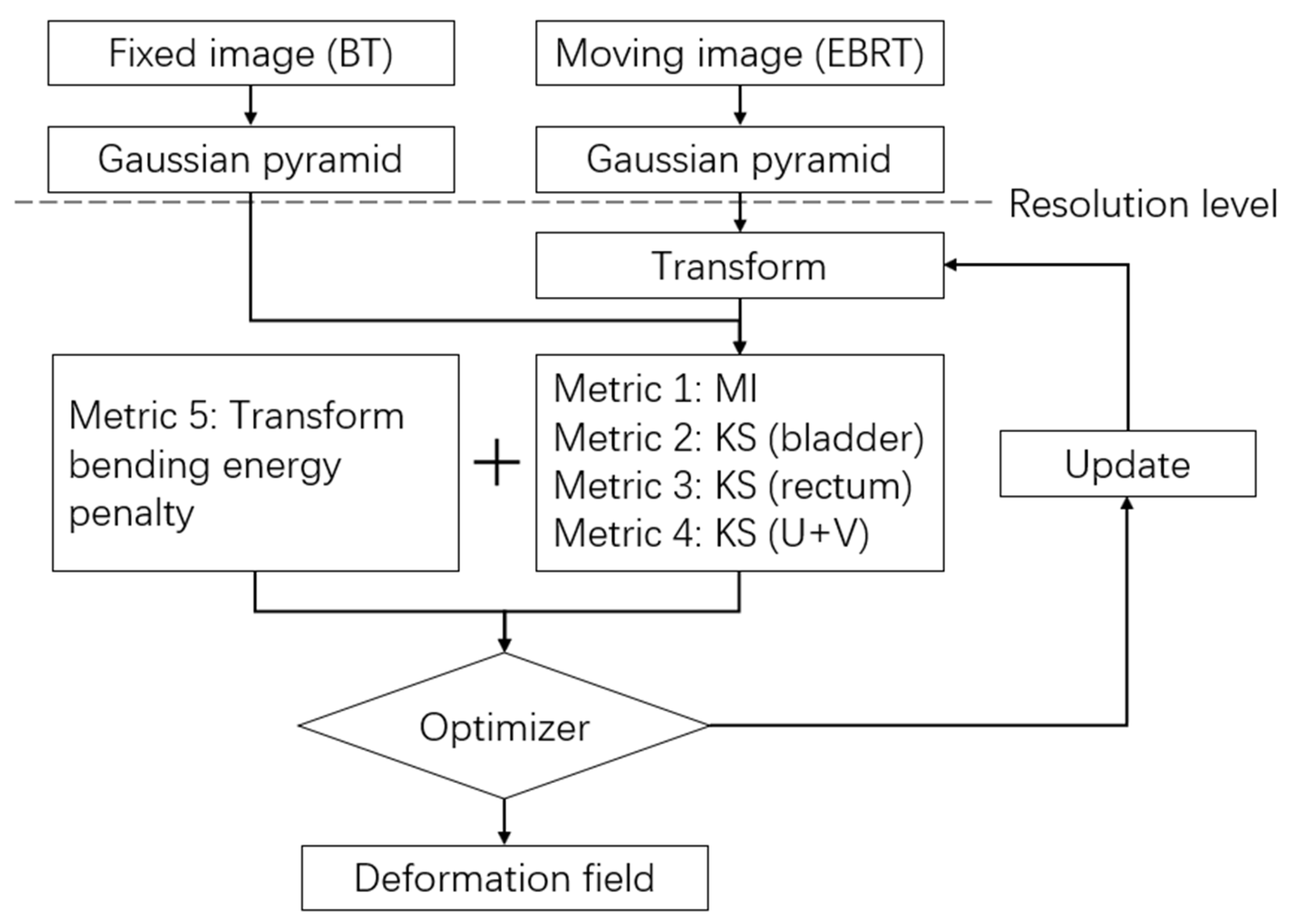
2.3. Registration
2.4. Evaluation
2.5. Dose Accumulation
3. Results
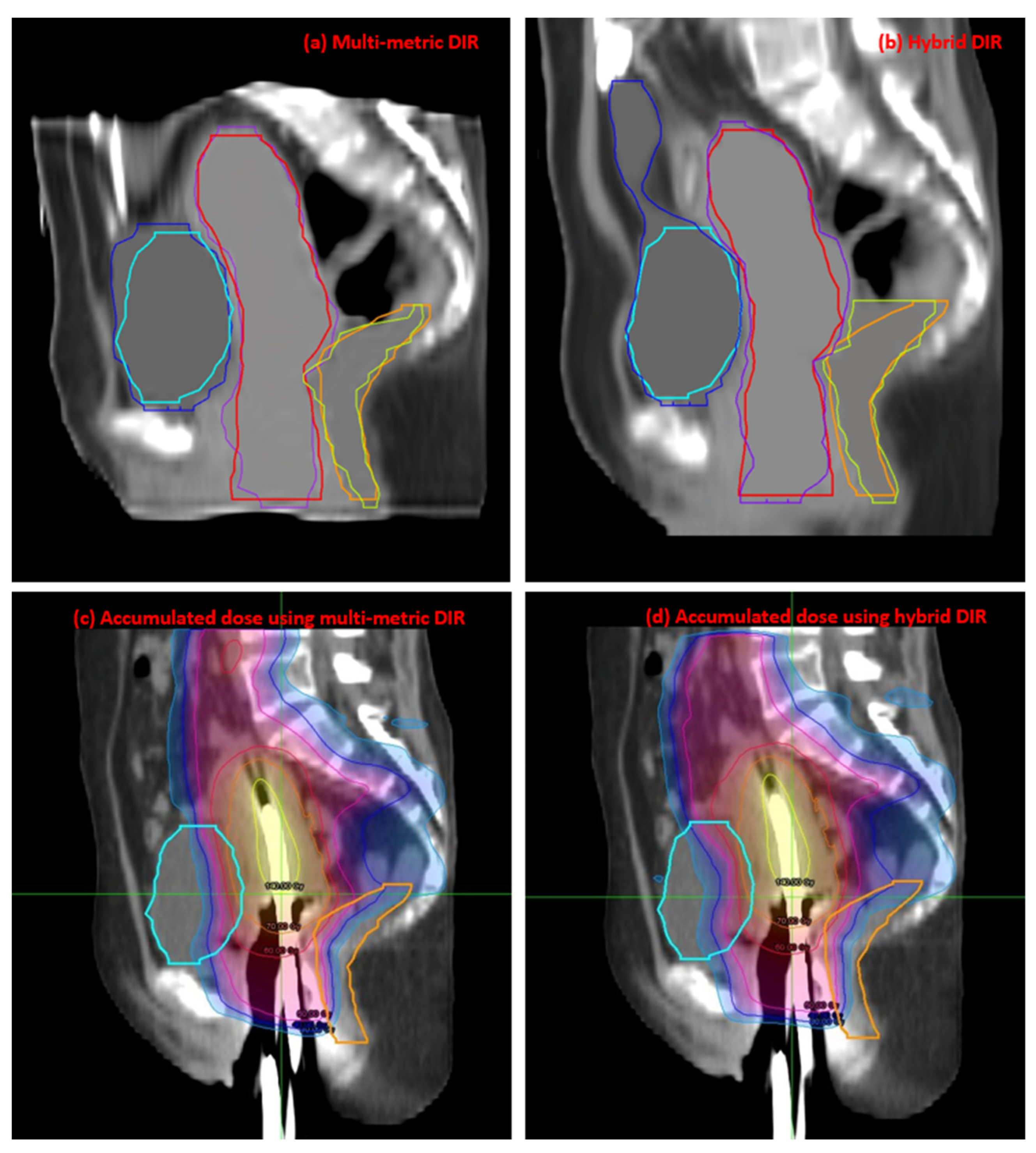
3.1. Registration Accuracy
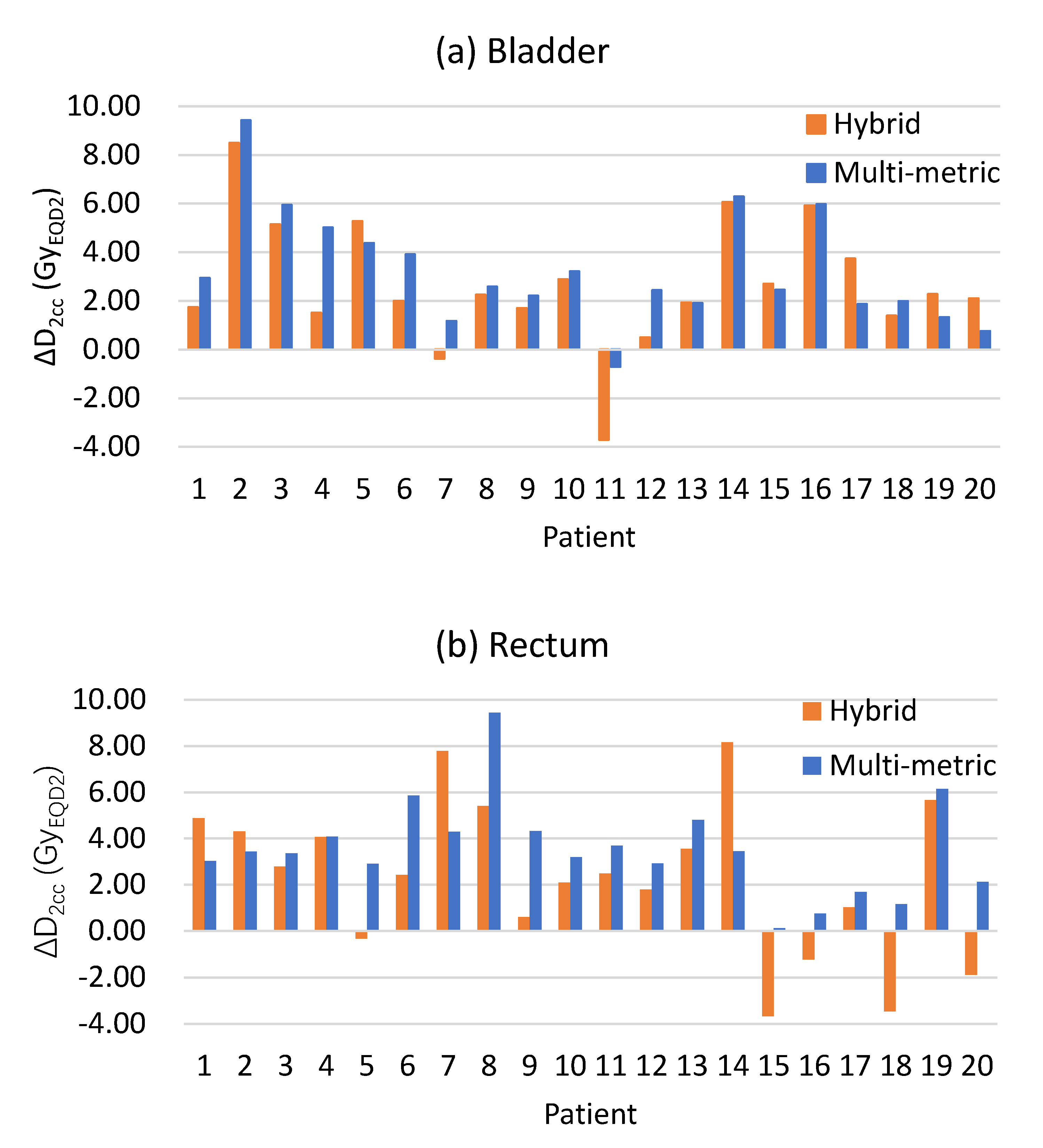
3.2. Dosimetric Accuracy
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Potter, R.; Haie, M.C.; Van, L.E.; Barillot, I.; De, B.M.; Dimopoulos, J.; Dumas, I.; Erickson, B.; Lang, S.; Nulens, A.; et al. Recommendations from gynaecological (GYN) GEC ESTRO working group (II): Concepts and terms in 3D image-based treatment planning in cervix cancer brachytherapy-3D dose volume parameters and aspects of 3D image-based anatomy, radiation physics, radiobiology. Radiother. Oncol. J. Eur. Soc. Ther. Radiol. Oncol. 2006, 78, 67–77. [Google Scholar] [CrossRef] [PubMed]
- Brock, K.K.; Mutic, S.; McNutt, T.R.; Li, H.; Kessler, M.L. Use of image registration and fusion algorithms and techniques in radiotherapy: Report of the AAPM Radiation Therapy Committee Task Group No. 132. Med. Phys. 2017, 44, e43–e76. [Google Scholar] [CrossRef] [PubMed]
- Swamidas, J.; Kirisits, C.; De Brabandere, M.; Hellebust, T.P.; Siebert, F.A.; Tanderup, K. Image registration, contour propagation and dose accumulation of external beam and brachytherapy in gynecological radiotherapy. Radiother. Oncol. 2020, 143, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Tait, L.M.; Hoffman, D.; Benedict, S.; Valicenti, R.; Mayadev, J.S. The use of MRI deformable image registration for CT-based brachytherapy in locally advanced cervical cancer. Brachytherapy 2016, 15, 333–340. [Google Scholar] [CrossRef]
- Flower, E.; Do, V.; Sykes, J.; Dempsey, C.; Holloway, L.; Summerhayes, K.; Thwaites, D.I. Deformable image registration for cervical cancer brachytherapy dose accumulation: Organ at risk dose–volume histogram parameter reproducibility and anatomic position stability. Brachytherapy 2017, 16, 387–392. [Google Scholar] [CrossRef]
- Abe, T.; Tamaki, T.; Makino, S.; Ebara, T.; Hirai, R.; Miyaura, K.; Kumazaki, Y.; Ohno, T.; Shikama, N.; Nakano, T.; et al. Assessing cumulative dose distributions in combined radiotherapy for cervical cancer using deformable image registration with pre-imaging preparations. Radiother. Oncol. 2014, 9, 293. [Google Scholar] [CrossRef]
- Teo, B.K.; Millar, L.P.B.; Ding, X.; Lin, L.L. Assessment of cumulative external beam and intracavitary brachytherapy organ doses in gynecologic cancers using deformable dose summation. Radiother. Oncol. 2015, 115, 195–202. [Google Scholar] [CrossRef]
- Mohammadi, R.; Mahdavi, S.R.; Jaberi, R.; Siavashpour, Z.; Janani, L.; Meigooni, A.S.; Reiazi, R. Evaluation of deformable image registration algorithm for determination of accumulated dose for brachytherapy of cervical cancer patients. J. Contemp. Brachyther. 2019, 11, 469. [Google Scholar] [CrossRef]
- Kim, H.; Huq, M.S.; Houser, C.; Beriwal, S.; Michalski, D. Mapping of dose distribution from IMRT onto MRI-guided high dose rate brachytherapy using deformable image registration for cervical cancer treatments: Preliminary study with commercially available software. J. Contemp. Brachyther. 2014, 6, 178–184. [Google Scholar] [CrossRef]
- Chapman, C.H.; Polan, D.; Vineberg, K.; Jolly, S.; Maturen, K.E.; Brock, K.K.; Prisciandaro, J.I. Deformable image registration based contour propagation yields clinically acceptable plans for MRI based cervical cancer brachytherapy planning. Brachytherapy 2018, 17, 360–367. [Google Scholar] [CrossRef]
- Van Heerden, L.E.; Visser, J.; Koedooder, K.; Rasch, C.R.; Pieters, B.R.; Bel, A. Role of deformable image registration for delivered dose accumulation of adaptive external beam radiation therapy and brachytherapy in cervical cancer. J. Contemp. Brachyther. 2018, 10, 542. [Google Scholar] [CrossRef] [PubMed]
- Hayashi, K.; Isohashi, F.; Akino, Y.; Wakai, N.; Mabuchi, S.; Suzuki, O.; Seo, Y.; Ootani, Y.; Sumida, I.; Yoshioka, Y.; et al. Estimation of the total rectal dose of radical external beam and intracavitary radiotherapy for uterine cervical cancer using the deformable image registration method. J. Radiat. Res. 2015, 56, 546–552. [Google Scholar] [CrossRef] [PubMed]
- Kadoya, N.; Miyasaka, Y.Y.; Yamamoto, T.; Kuroda, Y.; Ito, K.; Chiba, M.; Nakajima, Y.; Takahashi, N.; Kubozono, M.; Umezawa, R.; et al. Evaluation of rectum and bladder dose accumulation from external beam radiotherapy and brachytherapy for cervical cancer using two different deformable image registration techniques. J. Radiat. Res. 2017, 58, 720–728. [Google Scholar] [CrossRef]
- Rigaud, B.; Klopp, A.; Vedam, S.; Venkatesan, A.; Taku, N.; Simon, A.; Haigron, P.; de Crevoisier, R.; Brock, K.K.; Cazoulat, G. Deformable image registration for dose mapping between external beam radiotherapy and brachytherapy images of cervical cancer. Phys. Med. Biol. 2019, 64, 115023. [Google Scholar] [CrossRef] [PubMed]
- Van Heerden, L.E.; Houweling, A.C.; Koedooder, K.; van Kesteren, Z.; van Wieringen, N.; Rasch, C.R.N.; Pieters, B.R.; Bel, A. Structure-based deformable image registration: Added value for dose accumulation of external beam radiotherapy and brachytherapy in cervical cancer. Radiother. Oncol. 2017, 123, 319–324. [Google Scholar] [CrossRef] [PubMed]
- Reniers, B.; Janssens, G.; Orban de Xivry, J.O.; Landry, G.; Verhaegen, F. Dose distribution for gynecological brachytherapy with dose accumulation between insertions: Feasibility study. Brachytherapy 2016, 15, 504–513. [Google Scholar] [CrossRef] [PubMed]
- Bondar, L.; Hoogeman, M.S.; Vásquez Osorio, E.M.; Heijmen, B.J. A symmetric nonrigid registration method to handle large organ deformations in cervical cancer patients. Med. Phys. 2010, 37, 3760–3772. [Google Scholar] [CrossRef]
- Rodriguez-Vila, B.; Garcia-Vicente, F.; Gomez, E.J. Methodology for registration of distended rectums in pelvic CT studies. Med. Phys. 2012, 39, 6351–6359. [Google Scholar] [CrossRef]
- Vásquez Osorio, E.M.; Kolkman-Deurloo, I.K.K.; Schuring-Pereira, M.; Zolnay, A.; Heijmen, B.J.; Hoogeman, M.S. Improving anatomical mapping of complexly deformed anatomy for external beam radiotherapy and brachytherapy dose accumulation in cervical cancer. Med. Phys. 2015, 42, 206–220. [Google Scholar] [CrossRef]
- Andersen, E.S.; Muren, L.P.; Sørensen, T.S.; Noe, K.O.; Thor, M.; Petersen, J.B.; Høyer, M.; Bentzen, L.; Tanderup, K. Bladder dose accumulation based on a biomechanical deformable image registration algorithm in volumetric modulated arc therapy for prostate cancer. Phys. Med. Biol. 2012, 57, 7089. [Google Scholar] [CrossRef]
- Zhen, X.; Chen, H.; Yan, H.; Zhou, L.; Mell, L.K.; Yashar, C.M.; Jiang, S.; Jia, X.; Gu, X.; Cervino, L. A segmentation and point-matching enhanced efficient deformable image registration method for dose accumulation between HDR CT images. Phys. Med. Biol. 2015, 60, 2981. [Google Scholar] [CrossRef] [PubMed]
- Andersen, E.S.; Noe, K.Ø.; Sørensen, T.S.; Nielsen, S.K.; Fokdal, L.; Paludan, M.; Lindegaard, J.C.; Tanderup, K. Simple DVH parameter addition as compared to deformable registration for bladder dose accumulation in cervix cancer brachytherapy. Radiother. Oncol. 2013, 107, 52–57. [Google Scholar] [CrossRef] [PubMed]
- Rigaud, B.; Cazoulat, G.; Vedam, S.; Venkatesan, A.M.; Peterson, C.B.; Taku, N.; Klopp, A.H.; Brock, K.K. Modeling complex deformations of the sigmoid colon between external beam radiation therapy and brachytherapy images of cervical cancer. Int. J. Radiat. Oncol. Biol. Phys. 2020, 106, 1084–1094. [Google Scholar] [CrossRef] [PubMed]
- Klein, S.; Staring, M.; Murphy, K.; Viergever, M.A.; Pluim, J.P. elastix: A toolbox for intensity-based medical image registration. IEEE Trans. Med. Imaging 2010, 29, 196–205. [Google Scholar] [CrossRef]
- Shamonin, D.P.; Bron, E.E.; Lelieveldt, B.P.; Smits, M.; Klein, S.; Staring, M.; Alzheimer’s Disease Neuroimaging Initiative. Fast parallel image registration on CPU and GPU for diagnostic classification of Alzheimer’s disease. Front. Neuroinform. 2013, 7, 50. [Google Scholar] [CrossRef]
- Staring, M.; Klein, S.; Reiber, J.H.C.; Niessen, W.J.; Stoel, B.C. Pulmonary image registration with elastix using a standard intensity-based algorithm. Med. Image Anal. Clin. A Grand Chall. 2010, 73–79. [Google Scholar]
- Broggi, S.; Scalco, E.; Belli, M.L.; Logghe, G.; Verellen, D.; Moriconi, S.; Chiara, A.; Palmisano, A.; Mellone, R.; Fiorino, C.; et al. A comparative evaluation of 3 different free-form deformable image registration and contour propagation methods for head and neck MRI: The case of parotid changes during radiotherapy. Technol. Cancer Res. Treat. 2017, 16, 373–381. [Google Scholar] [CrossRef]
- Zukauskaite, R.; Brink, C.; Hansen, C.R.; Bertelsen, A.; Johansen, J.; Grau, C.; Eriksen, J.G. Open-source deformable image registration system for treatment planning and recurrence CT scans. Strahlenther. Onkol. 2016, 192, 545–551. [Google Scholar] [CrossRef]
- Akbarzadeh, A.; Gutierrez, D.; Baskin, A.; Ay, M.R.; Ahmadian, A.; Riahi Alam, N.; Lövblad, K.O.; Zaidi, H. Evaluation of whole-body MR to CT deformable image registration. J. Appl. Clin. Med. Phys. 2013, 14, 238–253. [Google Scholar] [CrossRef]
- Xie, X.; Song, Y.; Ye, F.; Yan, H.; Wang, S.; Zhao, X.; Dai, J. Improving deformable image registration with point metric and masking technique for postoperative breast cancer radiotherapy. Quant. Imaging Med. Surg. 2021, 11, 1196–1208. [Google Scholar] [CrossRef]
- Xie, X.; Song, Y.; Ye, F.; Yan, H.; Wang, S.; Zhao, X.; Dai, J. The application of multiple metrics in deformable image registration for target volume delineation of breast tumor bed. J. Appl. Clin. Med. Phys. 2022, 20, e13793. [Google Scholar] [CrossRef] [PubMed]
- Thévenaz, P.; Unser, M. Optimization of mutual information for multiresolution image registration. IEEE Trans. Image Process. A Publ. IEEE Signal Process. Soc. 2000, 9, 2083–2099. [Google Scholar] [CrossRef]
- Pinter, C.; Lasso, A.; Wang, A.; Jaffray, D.; Fichtinger, G. SlicerRT: Radiation therapy research toolkit for 3D Slicer. Med. Phys. 2012, 39, 6332–6338. [Google Scholar] [CrossRef] [PubMed]
- Dice, L.R. Measures of the amount of ecologic association between species. Ecology 1945, 26, 297–302. [Google Scholar] [CrossRef]
- Huttenlocher, D.P.; Klanderman, G.A.; Rucklidge, W.J. Comparing images using the Hausdorff distance. IEEE Trans. Pattern Anal. Mach. Intell. 1993, 15, 850–863. [Google Scholar] [CrossRef]
- Jamema, S.V.; Mahantshetty, U.; Tanderup, K.; Malvankar, D.; Sharma, S.; Engineer, R.; Chopra, S.; Shrivastava, S.K.; Deshpande, D.D. Inter-application variation of dose and spatial location of D(2cm(3)) volumes of OARs during MR image based cervix brachytherapy. Radiother. Oncol. 2013, 107, 58–62. [Google Scholar] [CrossRef]
- Chetty, I.J.; Rosu-Bubulac, M. Deformable Registration for Dose Accumulation. Semin. Radiat. Oncol. 2019, 29, 198–208. [Google Scholar] [CrossRef] [PubMed]
- Potter, R.; Kirisits, C.; Erickson, B.; Haie-Meder, C.; Van Limbergen, E.; Lindegaard, J.C.; Rownd, J.; Tanderup, K.; Thomadsen, B.R.; DeLuca, P.M. ICRU report no. 89: Prescribing, recording, and reporting brachytherapy for cancer of the cervix. JICRU 2013, 13, 1–258. [Google Scholar] [CrossRef]
- Kim, H.; Lee, Y.C.; Benedict, S.H.; Dyer, B.; Price, M.; Rong, Y.; Ravi, A.; Leung, E.; Beriwal, S.; Bernard, M.E.; et al. Dose Summation Strategies for External Beam Radiation Therapy and Brachytherapy in Gynecologic Malignancy: A Review from the NRG Oncology and NCTN Medical Physics Subcommittees. Int. J. Radiat. Oncol. Biol. Phys. 2021, 111, 999–1010. [Google Scholar] [CrossRef]

| Contour | Parameters | Multi-Metric | Hybrid | p-Value |
|---|---|---|---|---|
| Bladder | DSC | 0.84 ± 0.09 | 0.76 ± 0.15 | 0.001 |
| HD (mm) | 18.68 ± 9.99 | 41.98 ± 28.27 | <0.001 | |
| Rectum | DSC | 0.84 ± 0.04 | 0.77 ± 0.07 | <0.001 |
| HD (mm) | 14.23 ± 7.89 | 17.35 ± 10.01 | 0.155 | |
| U + V | DSC | 0.89 ± 0.02 | 0.86 ± 0.05 | 0.011 |
| HD (mm) | 16.92 ± 5.92 | 17.56 ± 9.85 | 0.756 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Fu, Q.; Xie, X.; Xu, Y.; Zuo, J.; Yang, X.; Xia, W.; An, J.; Huang, M.; Yan, H.; Dai, J. Applying Multi-Metric Deformable Image Registration for Dose Accumulation in Combined Cervical Cancer Radiotherapy. J. Pers. Med. 2023, 13, 323. https://doi.org/10.3390/jpm13020323
Fu Q, Xie X, Xu Y, Zuo J, Yang X, Xia W, An J, Huang M, Yan H, Dai J. Applying Multi-Metric Deformable Image Registration for Dose Accumulation in Combined Cervical Cancer Radiotherapy. Journal of Personalized Medicine. 2023; 13(2):323. https://doi.org/10.3390/jpm13020323
Chicago/Turabian StyleFu, Qi, Xin Xie, Yingjie Xu, Jing Zuo, Xi Yang, Wenlong Xia, Jusheng An, Manni Huang, Hui Yan, and Jianrong Dai. 2023. "Applying Multi-Metric Deformable Image Registration for Dose Accumulation in Combined Cervical Cancer Radiotherapy" Journal of Personalized Medicine 13, no. 2: 323. https://doi.org/10.3390/jpm13020323
APA StyleFu, Q., Xie, X., Xu, Y., Zuo, J., Yang, X., Xia, W., An, J., Huang, M., Yan, H., & Dai, J. (2023). Applying Multi-Metric Deformable Image Registration for Dose Accumulation in Combined Cervical Cancer Radiotherapy. Journal of Personalized Medicine, 13(2), 323. https://doi.org/10.3390/jpm13020323






