Impact of Female Gender in Inflammatory Bowel Diseases: A Narrative Review
Abstract
1. Introduction
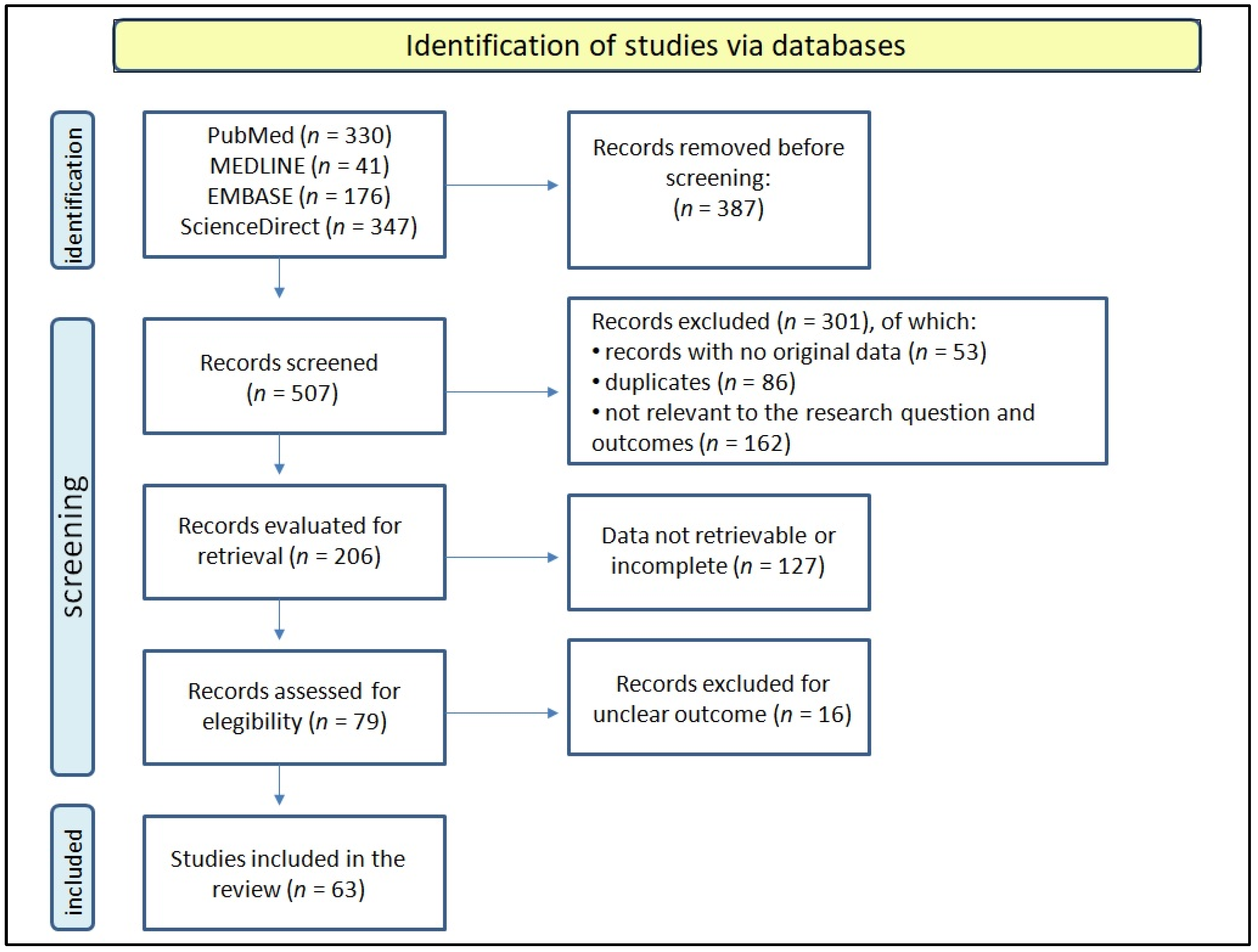
2. Methods
3. Sex-Related Differences in IBD Epidemiology and Pathogenesis
4. Genetics
5. Disease Phenotype and Complications in Females
6. IBD Medical Treatment
7. IBD and Female Infertility
8. Pregnancy
9. IBD and Female Hormones
10. IBD and Menstrual Cycle
11. IBD and Female Psychology
12. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Adolph, T.E.; Meyer, M.; Schwärzler, J.; Mayr, L.; Grabherr, F.; Tilg, H. The metabolic nature of inflammatory bowel diseases. Nat. Rev. Gastroenterol. Hepatol. 2022, 19, 753–767. [Google Scholar] [CrossRef] [PubMed]
- Greuter, T.; Manser, C.; Pittet, V.; Vavricka, S.; Biedermann, L. Gender Differences in Inflammatory Bowel Disease. Digestion 2020, 101, 98–104. [Google Scholar] [CrossRef]
- De Simone, V.; Matteoli, G. Estrogen-Mediated Effects Underlie Gender Bias in Inflammatory Bowel Disease. Cell. Mol. Gastroenterol. Hepatol. 2018, 5, 638–639. [Google Scholar] [CrossRef]
- Ooi, C.; Fock, K.; Makharia, G.; Goh, K.; Ling, K.; Hilmi, I.; Lim, W.; Kelvin, T.; Gibson, P.; Gearry, R.; et al. The Asia-Pacific consensus on ulcerative colitis. J. Gastroenterol. Hepatol. 2010, 25, 453–468. [Google Scholar] [CrossRef] [PubMed]
- Fujimoto, T.; Kato, J.; Nasu, J.; Kuriyama, M.; Okada, H.; Yamamoto, H.; Mizuno, M.; Shiratori, Y. Change of clinical characteristics of ulcerative colitis in Japan: Analysis of 844 hospital-based patients from 1981 to 2000. Eur. J. Gastroenterol. Hepatol. 2007, 19, 229–235. [Google Scholar] [CrossRef] [PubMed]
- Jiang, L.; Xia, B.; Li, J.; Ye, M.; Yan, W.; Deng, C.; Ding, Y.; Luo, H.; Hou, W.; Zhao, Q.; et al. Retrospective survey of 452 patients with inflammatory bowel disease in Wuhan city, central China. Inflamm. Bowel Dis. 2006, 12, 212–217. [Google Scholar] [CrossRef] [PubMed]
- Yang, S.; Yun, S.; Kim, J.; Park, J.; Kim, H.; Kim, Y.; Chang, D.; Kim, J.; Song, I.; Park, J.; et al. Epidemiology of inflammatory bowel disease in the Songpa-Kangdong district, Seoul, Korea, 1986–2005: A KASID study. Inflamm. Bowel Dis. 2008, 14, 542–549. [Google Scholar] [CrossRef]
- Gearry, R.; Richardson, A.; Frampton, C.; Collett, J.; Burt, M.; Chapman, B.; Barclay, M. High incidence of Crohn’s disease in Canterbury, New Zealand: Results of an epidemiologic study. Inflamm. Bowel Dis. 2006, 12, 936–943. [Google Scholar] [CrossRef]
- Thia, K.; Loftus, E.; Sandborn, W.; Yang, S. An update on the epidemiology of inflammatory bowel disease in Asia. Am. J. Gastroenterol. 2008, 103, 3167–3182. [Google Scholar] [CrossRef]
- Shah, S.; Khalili, H.; Gower-Rousseau, C.; Olen, O.; Benchimol, E.; Lynge, E.; Nielsen, K.; Brassard, P.; Vutcovici, M.; Bitton, A.; et al. Sex-Based Differences in Incidence of Inflammatory Bowel Diseases-Pooled Analysis of Population-Based Studies from Western Countries. Gastroenterology 2018, 155, 1079–1089. [Google Scholar] [CrossRef]
- Wagtmans, M.; Verspaget, H.; Lamers, C.; van Hogezand, R. Gender-related differences in the clinical course of Crohn’s disease. Am. J. Gastroenterol. 2001, 96, 1541–1546. [Google Scholar] [CrossRef] [PubMed]
- Kyle, J. Crohn’s disease in the northeastern and northern Isles of Scotland: An epidemiological review. Gastroenterology 1992, 103, 392–399. [Google Scholar] [CrossRef]
- Latour, P.; Louis, E.; Belaiche, J. Incidence of inflammatory bowel disease in the area of Liège: A 3 years prospective study (1993–1996). Acta Gastro-Enterol. Belg. 1998, 61, 410–413. [Google Scholar]
- Shivananda, S.; Peña, A.; Nap, M.; Weterman, I.; Mayberry, J.; Ruitenberg, E.; Hoedemaeker, P. Epidemiology of Crohn’s disease in Regio Leiden, The Netherlands. A population study from 1979 to 1983. Gastroenterology 1987, 93, 966–974. [Google Scholar] [CrossRef] [PubMed]
- Whelan, G. Epidemiology of inflammatory bowel disease. Med. Clin. N. Am. 1990, 74, 1–12. [Google Scholar] [CrossRef]
- Prideaux, L.; Kamm, M.; De Cruz, P.; Chan, F.; Ng, S. Inflammatory bowel disease in Asia: A systematic review. J. Gastroenterol. Hepatol. 2012, 27, 1266–1280. [Google Scholar] [CrossRef]
- Leong, R.; Lau, J.; Sung, J. The epidemiology and phenotype of Crohn’s disease in the Chinese population. Inflamm. Bowel Dis. 2004, 10, 646–651. [Google Scholar] [CrossRef]
- Severs, M.; Spekhorst, L.; Mangen, M.; Dijkstra, G.; Löwenberg, M.; Hoentjen, F.; van der Meulen-de Jong, A.; Pierik, M.; Ponsioen, C.; Bouma, G.; et al. Sex-Related Differences in Patients with Inflammatory Bowel Disease: Results of 2 Prospective Cohort Studies. Inflamm. Bowel Dis. 2018, 24, 1298–1306. [Google Scholar] [CrossRef]
- Zelinkova, Z.; Stokkers, P.; van der Linde, K.; Kuipers, E.; Peppelenbosch, M.; van der Woude, C. Maternal imprinting and female predominance in familial Crohn’s disease. J. Crohn’s Colitis 2012, 6, 771–776. [Google Scholar] [CrossRef]
- Tedde, A.; Putignano, A.; Bagnoli, S.; Congregati, C.; Milla, M.; Sorbi, S.; Genuardi, M.; Papi, L. Interleukin-10 promoter polymorphisms influence susceptibility to ulcerative colitis in a gender-specific manner. Scand. J. Gastroenterol. 2008, 43, 712–718. [Google Scholar] [CrossRef]
- Lin, Z.; Poritz, L.; Franke, A.; Li, T.; Ruether, A.; Byrnes, K.; Wang, Y.; Gebhard, A.; MacNeill, C.; Thomas, N.; et al. Genetic association of nonsynonymous variants of the IL23R with familial and sporadic inflammatory bowel disease in women. Dig. Dis. Sci. 2010, 55, 739–746. [Google Scholar] [CrossRef] [PubMed]
- Jaźwińska-Tarnawska, E.; Jęśkowiak, I.; Waszczuk, E.; Mulak, A.; Głowacka, K.; Hurkacz, M.; Paradowski, L.; Zaleska, Z.; Wiela-Hojeńska, A. Genetic polymorphism of ABCB1 gene (C3435T) in patients with inflammatory bowel diseases. Is there any gender dependency? Pharmacol. Rep. 2015, 67, 294–298. [Google Scholar] [CrossRef] [PubMed]
- Friedrichs, F.; Brescianini, S.; Annese, V.; Latiano, A.; Berger, K.; Kugathasan, S.; Broeckel, U.; Nikolaus, S.; Daly, M.; Schreiber, S.; et al. Evidence of transmission ratio distortion of DLG5 R30Q variant in general and implication of an association with Crohn disease in men. Hum. Genet. 2006, 119, 305–311. [Google Scholar] [CrossRef] [PubMed]
- Biank, V.; Friedrichs, F.; Babusukumar, U.; Wang, T.; Stoll, M.; Broeckel, U.; Kugathasan, S. DLG5 R30Q variant is a female-specific protective factor in pediatric onset Crohn’s disease. Am. J. Gastroenterol. 2007, 102, 391–398. [Google Scholar] [CrossRef] [PubMed]
- Arulanantham, K.; Kramer, M.; Gryboski, J. The association of inflammatory bowel disease and X chromosomal abnormality. Pediatrics 1980, 66, 63–67. [Google Scholar] [CrossRef]
- Vermeire, S.; Satsangi, J.; Peeters, M.; Parkes, M.; Jewell, D.; Vlietinck, R.; Rutgeerts, P. Evidence for inflammatory bowel disease of a susceptibility locus on the X chromosome. Gastroenterology 2001, 120, 834–840. [Google Scholar] [CrossRef]
- Lee, H.; Oh, H.; Yang, S.; Baek, J.; Jung, S.; Hong, M.; Kim, K.; Shin, H.; Kim, K.; Park, S.; et al. X Chromosome-wide Association Study Identifies a Susceptibility Locus for Inflammatory Bowel Disease in Koreans. J. Crohn’s Colitis 2017, 11, 820–830. [Google Scholar] [CrossRef]
- Kudelka, M.; Hinrichs, B.; Darby, T.; Moreno, C.; Nishio, H.; Cutler, C.; Wang, J.; Wu, H.; Zeng, J.; Wang, Y.; et al. Cosmc is an X-linked inflammatory bowel disease risk gene that spatially regulates gut microbiota and contributes to sex-specific risk. Proc. Natl. Acad. Sci. USA 2016, 113, 14787–14792. [Google Scholar] [CrossRef]
- Libert, C.; Dejager, L.; Pinheiro, I. The X chromosome in immune functions: When a chromosome makes the difference. Nat. Rev. Immunol. 2010, 10, 594–604. [Google Scholar] [CrossRef]
- Invernizzi, P.; Miozzo, M.; Selmi, C.; Persani, L.; Battezzati, P.; Zuin, M.; Lucchi, S.; Meroni, P.; Marasini, B.; Zeni, S.; et al. X chromosome monosomy: A common mechanism for autoimmune diseases. J. Immunol. 2005, 175, 575–578. [Google Scholar] [CrossRef]
- Svyryd, Y.; Hernández-Molina, G.; Vargas, F.; Sánchez-Guerrero, J.; Segovia, D.; Mutchinick, O. X chromosome monosomy in primary and overlapping autoimmune diseases. Autoimmun. Rev. 2012, 11, 301–304. [Google Scholar] [CrossRef] [PubMed]
- Romberg-Camps, M.; Dagnelie, P.; Kester, A.; Hesselink-van de Kruijs, M.; Cilissen, M.; Engels, L.; Van Deursen, C.; Hameeteman, W.; Wolters, F.; Russel, M.; et al. Influence of phenotype at diagnosis and of other potential prognostic factors on the course of inflammatory bowel disease. Am. J. Gastroenterol. 2009, 104, 371–383. [Google Scholar] [CrossRef] [PubMed]
- Mazor, Y.; Maza, I.; Kaufman, E.; Ben-Horin, S.; Karban, A.; Chowers, Y.; Eliakim, R. Prediction of disease complication occurrence in Crohn’s disease using phenotype and genotype parameters at diagnosis. J. Crohn’s Colitis 2011, 5, 592–597. [Google Scholar] [CrossRef]
- Blumenstein, I.; Herrmann, E.; Filmann, N.; Zosel, C.; Tacke, W.; Bock, H.; Dignass, A.; Hartmann, F.; Zeuzem, S.; Stein, J.; et al. Female patients suffering from inflammatory bowel diseases are treated less frequently with immunosuppressive medication and have a higher disease activity: A subgroup analysis of a large multi-centre, prospective, internet-based study. J. Crohn’s Colitis 2011, 5, 203–210. [Google Scholar] [CrossRef] [PubMed]
- Bokemeyer, B.; Hardt, J.; Hüppe, D.; Prenzler, A.; Conrad, S.; Düffelmeyer, M.; Hartmann, P.; Hoffstadt, M.; Klugmann, T.; Schmidt, C.; et al. Clinical status, psychosocial impairments, medical treatment and health care costs for patients with inflammatory bowel disease (IBD) in Germany: An online IBD registry. J. Crohn’s Colitis 2013, 7, 355–368. [Google Scholar] [CrossRef]
- Greuter, T.; Piller, A.; Fournier, N.; Safroneeva, E.; Straumann, A.; Biedermann, L.; Godat, S.; Nydegger, A.; Scharl, M.; Rogler, G.; et al. Upper Gastrointestinal Tract Involvement in Crohn’s Disease: Frequency, Risk Factors, and Disease Course. J. Crohn’s Colitis 2018, 12, 1399–1409. [Google Scholar] [CrossRef]
- Sebastian, S.; Hernández, V.; Myrelid, P.; Kariv, R.; Tsianos, E.; Toruner, M.; Marti-Gallostra, M.; Spinelli, A.; van der Meulen-de Jong, A.; Yuksel, E.; et al. Colorectal cancer in inflammatory bowel disease: Results of the 3rd ECCO pathogenesis scientific workshop (I). J. Crohn’s Colitis 2014, 8, 5–18. [Google Scholar] [CrossRef]
- Jussila, A.; Virta, L.; Pukkala, E.; Färkkilä, M. Mortality and causes of death in patients with inflammatory bowel disease: A nationwide register study in Finland. J. Crohn’s Colitis 2014, 8, 1088–1096. [Google Scholar] [CrossRef]
- Peyrin-Biroulet, L.; Harmsen, W.; Tremaine, W.; Zinsmeister, A.; Sandborn, W.; Loftus, E. Surgery in a population-based cohort of Crohn’s disease from Olmsted County, Minnesota (1970–2004). Am. J. Gastroenterol. 2012, 107, 1693–1701. [Google Scholar] [CrossRef]
- Walldorf, J.; Krummenerl, A.; Engler, K.; Busch, J.; Dollinger, M.; Seufferlein, T.; Albert, J. Health care for osteoporosis in inflammatory bowel disease: Unmet needs in care of male patients? J. Crohn’s Colitis 2013, 7, 901–907. [Google Scholar] [CrossRef]
- Priadko, K.; Moretti, A.; Iolascon, G.; Gravina, A.; Miranda, A.; Sgambato, D.; De Musis, C.; Romano, M.; Gimigliano, F. Bone Alterations in Inflammatory Bowel Diseases: Role of Osteoprotegerin. J. Clin. Med. 2022, 11, 1840. [Google Scholar] [CrossRef] [PubMed]
- Sigurdsson, G.; Schmidt, S.; Mellström, D.; Ohlsson, C.; Saalman, R.; Lorentzon, M. Young Adult Male Patients with Childhood-onset IBD Have Increased Risks of Compromised Cortical and Trabecular Bone Microstructures. Inflamm. Bowel Dis. 2022. [Google Scholar] [CrossRef] [PubMed]
- Leslie, W.; Lix, L.; Johansson, H.; Oden, A.; McCloskey, E.; Kanis, J. Independent clinical validation of a Canadian FRAX tool: Fracture prediction and model calibration. J. Bone Miner. Res. 2010, 25, 2350–2358. [Google Scholar] [CrossRef] [PubMed]
- Ghafoori, S.; Keshtkar, A.; Khashayar, P.; Ebrahimi, M.; Ramezani, M.; Mohammadi, Z.; Saeidifard, F.; Nemati, N.; Khoshbin, M.; Azizian, S.; et al. The risk of osteoporotic fractures and its associating risk factors according to the FRAX model in the Iranian patients: A follow-up cohort. J. Diabetes Metab. Disord. 2014, 13, 93. [Google Scholar] [CrossRef]
- Maharlouei, N.; Khodayari, M.; Forouzan, F.; Rezaianzadeh, A.; Lankarani, K. The incidence rate of hip fracture in Shiraz, Iran during 2008–2010. Arch. Osteoporos. 2014, 9, 165. [Google Scholar] [CrossRef]
- Valizadeh, M.; Mazloomzadeh, S.; Azizi, R. Epidemiology of hip fractures in Zanjan, Iran. Arch. Osteoporos. 2008, 3, 1–5. [Google Scholar] [CrossRef]
- Caio, G.; Lungaro, L.; Caputo, F.; Zoli, E.; Giancola, F.; Chiarioni, G.; De Giorgio, R.; Zoli, G. Nutritional Treatment in Crohn’s Disease. Nutrients 2021, 13, 1628. [Google Scholar] [CrossRef]
- Caio, G.; Lungaro, L.; Chiarioni, G.; Giancola, F.; Caputo, F.; Guarino, M.; Volta, U.; Testino, G.; Pellicano, R.; Zoli, G.; et al. Beyond biologics: Advanced therapies in inflammatory bowel diseases. Minerva Gastroenterol. 2022, 68, 319–332. [Google Scholar] [CrossRef]
- Samuel, S.; Ingle, S.; Dhillon, S.; Yadav, S.; Harmsen, W.; Zinsmeister, A.; Tremaine, W.; Sandborn, W.; Loftus, E. Cumulative incidence and risk factors for hospitalization and surgery in a population-based cohort of ulcerative colitis. Inflamm. Bowel Dis. 2013, 19, 1858–1866. [Google Scholar] [CrossRef]
- Heath, E.; Kim, R.; Wilson, A. A Comparative Analysis of Drug Therapy, Disease Phenotype, and Health Care Outcomes for Men and Women with Inflammatory Bowel Disease. Dig. Dis. Sci. 2022, 67, 4287–4294. [Google Scholar] [CrossRef]
- Billioud, V.; Sandborn, W.; Peyrin-Biroulet, L. Loss of response and need for adalimumab dose intensification in Crohn’s disease: A systematic review. Am. J. Gastroenterol. 2011, 106, 674–684. [Google Scholar] [CrossRef] [PubMed]
- Lopez, A.; Billioud, V.; Peyrin-Biroulet, C.; Peyrin-Biroulet, L. Adherence to anti-TNF therapy in inflammatory bowel diseases: A systematic review. Inflamm. Bowel Dis. 2013, 19, 1528–1533. [Google Scholar] [CrossRef]
- Carini, F.; Mazzola, M.; Gagliardo, C.; Scaglione, M.; Giammanco, M.; Tomasello, G. Inflammatory bowel disease and infertility: Analysis of literature and future perspectives. Acta Bio-Med. Atenei Parm. 2021, 92, e2021264. [Google Scholar] [CrossRef]
- Laube, R.; Paramsothy, S.; Leong, R. Review of pregnancy in Crohn’s disease and ulcerative colitis. Ther. Adv. Gastroenterol. 2021, 14, 17562848211016242. [Google Scholar] [CrossRef] [PubMed]
- Baird, D.; Narendranathan, M.; Sandler, R. Increased risk of preterm birth for women with inflammatory bowel disease. Gastroenterology 1990, 99, 987–994. [Google Scholar] [CrossRef]
- Hudson, M.; Flett, G.; Sinclair, T.; Brunt, P.; Templeton, A.; Mowat, N. Fertility and pregnancy in inflammatory bowel disease. Int. J. Gynaecol. Obstet. 1997, 58, 229–237. [Google Scholar] [CrossRef] [PubMed]
- Khosla, R.; Willoughby, C.; Jewell, D. Crohn’s disease and pregnancy. Gut 1984, 25, 52–56. [Google Scholar] [CrossRef] [PubMed]
- Marri, S.; Ahn, C.; Buchman, A. Voluntary childlessness is increased in women with inflammatory bowel disease. Inflamm. Bowel Dis. 2007, 13, 591–599. [Google Scholar] [CrossRef]
- Fréour, T.; Miossec, C.; Bach-Ngohou, K.; Dejoie, T.; Flamant, M.; Maillard, O.; Denis, M.; Barriere, P.; Bruley des Varannes, S.; Bourreille, A.; et al. Ovarian reserve in young women of reproductive age with Crohn’s disease. Inflamm. Bowel Dis. 2012, 18, 1515–1522. [Google Scholar] [CrossRef]
- Ban, L.; Tata, L.; Humes, D.; Fiaschi, L.; Card, T. Decreased fertility rates in 9639 women diagnosed with inflammatory bowel disease: A United Kingdom population-based cohort study. Aliment. Pharmacol. Ther. 2015, 42, 855–866. [Google Scholar] [CrossRef]
- Şenateş, E.; Çolak, Y.; Erdem, E.; Yeşil, A.; Coşkunpınar, E.; Şahin, Ö.; Altunöz, M.; Tuncer, I.; Kurdaş Övünç, A. Serum anti-Müllerian hormone levels are lower in reproductive-age women with Crohn’s disease compared to healthy control women. J. Crohn’s Colitis 2013, 7, e29–e34. [Google Scholar] [CrossRef]
- Lee, H.; Bae, J.; Lee, B.; Lee, K.; Wie, J.; Kim, J.; Cho, Y.; Jung, S.; Kim, S.; Choi, H.; et al. Pregnancy outcomes in women with inflammatory bowel disease: A 10-year nationwide population-based cohort study. Aliment. Pharmacol. Ther. 2020, 51, 861–869. [Google Scholar] [CrossRef] [PubMed]
- Cornish, J.; Tan, E.; Teare, J.; Teoh, T.; Rai, R.; Darzi, A.; Paraskevas, P.; Clark, S.; Tekkis, P. The effect of restorative proctocolectomy on sexual function, urinary function, fertility, pregnancy and delivery: A systematic review. Dis. Colon Rectum 2007, 50, 1128–1138. [Google Scholar] [CrossRef] [PubMed]
- Oresland, T.; Palmblad, S.; Ellström, M.; Berndtsson, I.; Crona, N.; Hultén, L. Gynaecological and sexual function related to anatomical changes in the female pelvis after restorative proctocolectomy. Int. J. Color. Dis. 1994, 9, 77–81. [Google Scholar] [CrossRef]
- Waljee, A.; Waljee, J.; Morris, A.; Higgins, P. Threefold increased risk of infertility: A meta-analysis of infertility after ileal pouch anal anastomosis in ulcerative colitis. Gut 2006, 55, 1575–1580. [Google Scholar] [CrossRef] [PubMed]
- Wikland, M.; Jansson, I.; Asztély, M.; Palselius, I.; Svaninger, G.; Magnusson, O.; Hultén, L. Gynaecological problems related to anatomical changes after conventional proctocolectomy and ileostomy. Int. J. Color. Dis. 1990, 5, 49–52. [Google Scholar] [CrossRef]
- Mountifield, R.; Bampton, P.; Prosser, R.; Muller, K.; Andrews, J. Fear and fertility in inflammatory bowel disease: A mismatch of perception and reality affects family planning decisions. Inflamm. Bowel Dis. 2009, 15, 720–725. [Google Scholar] [CrossRef]
- Riis, L.; Vind, I.; Politi, P.; Wolters, F.; Vermeire, S.; Tsianos, E.; Freitas, J.; Mouzas, I.; Ruiz Ochoa, V.; O’Morain, C.; et al. Does pregnancy change the disease course? A study in a European cohort of patients with inflammatory bowel disease. Am. J. Gastroenterol. 2006, 101, 1539–1545. [Google Scholar] [CrossRef]
- Palomba, S.; Sereni, G.; Falbo, A.; Beltrami, M.; Lombardini, S.; Boni, M.; Fornaciari, G.; Sassatelli, R.; La Sala, G. Inflammatory bowel diseases and human reproduction: A comprehensive evidence-based review. World J. Gastroenterol. 2014, 20, 7123–7136. [Google Scholar] [CrossRef] [PubMed]
- Bortoli, A.; Pedersen, N.; Duricova, D.; D’Inca, R.; Gionchetti, P.; Panelli, M.; Ardizzone, S.; Sanroman, A.; Gisbert, J.; Arena, I.; et al. Pregnancy outcome in inflammatory bowel disease: Prospective European case-control ECCO-EpiCom study, 2003–2006. Aliment. Pharmacol. Ther. 2011, 34, 724–734. [Google Scholar] [CrossRef]
- Munkholm, P. Pregnancy, fertility, and disease course in patients with Crohn’s disease and ulcerative colitis. Eur. J. Intern. Med. 2000, 11, 215–221. [Google Scholar] [CrossRef] [PubMed]
- van der Giessen, J.; van der Woude, C.; Peppelenbosch, M.; Fuhler, G. A Direct Effect of Sex Hormones on Epithelial Barrier Function in Inflammatory Bowel Disease Models. Cells 2019, 8, 261. [Google Scholar] [CrossRef]
- Julsgaard, M.; Nørgaard, M.; Hvas, C.; Buck, D.; Christensen, L. Self-reported adherence to medical treatment prior to and during pregnancy among women with ulcerative colitis. Inflamm. Bowel Dis. 2011, 17, 1573–1580. [Google Scholar] [CrossRef] [PubMed]
- Bharadwaj, S.; Kulkarni, G.; Shen, B. Menstrual cycle, sex hormones in female inflammatory bowel disease patients with and without surgery. J. Dig. Dis. 2015, 16, 245–255. [Google Scholar] [CrossRef] [PubMed]
- Heitkemper, M.; Chang, L. Do fluctuations in ovarian hormones affect gastrointestinal symptoms in women with irritable bowel syndrome? Gend. Med. 2009, 6, 152–167. [Google Scholar] [CrossRef] [PubMed]
- Pierdominici, M.; Maselli, A.; Varano, B.; Barbati, C.; Cesaro, P.; Spada, C.; Zullo, A.; Lorenzetti, R.; Rosati, M.; Rainaldi, G.; et al. Linking estrogen receptor β expression with inflammatory bowel disease activity. Oncotarget 2015, 6, 40443–40451. [Google Scholar] [CrossRef]
- Goodman, W.; Garg, R.; Reuter, B.; Mattioli, B.; Rissman, E.; Pizarro, T. Loss of estrogen-mediated immunoprotection underlies female gender bias in experimental Crohn’s-like ileitis. Mucosal Immunol. 2014, 7, 1255–1265. [Google Scholar] [CrossRef]
- Kane, S.; Sable, K.; Hanauer, S. The menstrual cycle and its effect on inflammatory bowel disease and irritable bowel syndrome: A prevalence study. Am. J. Gastroenterol. 1998, 93, 1867–1872. [Google Scholar] [CrossRef]
- Weber, A.; Ziegler, C.; Belinson, J.; Mitchinson, A.; Widrich, T.; Fazio, V. Gynecologic history of women with inflammatory bowel disease. Obstet. Gynecol. 1995, 86, 843–847. [Google Scholar] [CrossRef]
- Saha, S.; Zhao, Y.; Shah, S.; Esposti, S.; Lidofsky, S.; Salih, S.; Bright, R.; Law, M.; Moniz, H.; Flowers, N.; et al. Menstrual cycle changes in women with inflammatory bowel disease: A study from the ocean state Crohn’s and colitis area registry. Inflamm. Bowel Dis. 2014, 20, 534–540. [Google Scholar] [CrossRef]
- Lichtarowicz, A.; Norman, C.; Calcraft, B.; Morris, J.; Rhodes, J.; Mayberry, J. A study of the menopause, smoking, and contraception in women with Crohn’s disease. Q. J. Med. 1989, 72, 623–631. [Google Scholar] [PubMed]
- Rosenblatt, E.; Kane, S. Sex-Specific Issues in Inflammatory Bowel Disease. Gastroenterol. Hepatol. 2015, 11, 592. [Google Scholar]
- Kane, S.; Reddy, D. Hormonal replacement therapy after menopause is protective of disease activity in women with inflammatory bowel disease. Am. J. Gastroenterol. 2008, 103, 1193–1196. [Google Scholar] [CrossRef] [PubMed]
- Khalili, H.; Higuchi, L.; Ananthakrishnan, A.; Manson, J.; Feskanich, D.; Richter, J.; Fuchs, C.; Chan, A. Hormone therapy increases risk of ulcerative colitis but not Crohn’s disease. Gastroenterology 2012, 143, 1199–1206. [Google Scholar] [CrossRef]
- Timmer, A.; Sutherland, L.; Martin, F.; Canadian Mesalamine for Remission of Crohn’s Disease Study Group. Oral contraceptive use and smoking are risk factors for relapse in Crohn’s disease. Gastroenterology 1998, 114, 1143–1150. [Google Scholar] [CrossRef] [PubMed]
- Cosnes, J.; Carbonnel, F.; Carrat, F.; Beaugerie, L.; Gendre, J. Oral contraceptive use and the clinical course of Crohn’s disease: A prospective cohort study. Gut 1999, 45, 218–222. [Google Scholar] [CrossRef]
- Khalili, H.; Higuchi, L.; Ananthakrishnan, A.; Richter, J.; Feskanich, D.; Fuchs, C.; Chan, A. Oral contraceptives, reproductive factors and risk of inflammatory bowel disease. Gut 2013, 62, 1153–1159. [Google Scholar] [CrossRef]
- Aslanidis, S.; Pyrpasopoulou, A.; Douma, S.; Poulakos, P.; Triantafyllou, A. Restoration of menstruation in premature ovarian failure after initiation of adalimumab. Scand. J. Rheumatol. 2008, 37, 488–490. [Google Scholar] [CrossRef]
- Scheinfeld, N. Menorrhagia and severe menstrual pain related to the use of adalimumab in a psoriatic. J. Dermatol. Treat. 2008, 19, 188–189. [Google Scholar] [CrossRef]
- Lu, D.; Song, H.; Shi, G. Anti-TNF-α treatment for pelvic pain associated with endometriosis. Cochrane Database Syst. Rev. 2013, CD008088. [Google Scholar] [CrossRef]
- Metcalf, A.; Dozois, R.; Kelly, K. Sexual function in women after proctocolectomy. Ann. Surg. 1986, 204, 624–627. [Google Scholar] [CrossRef] [PubMed]
- Kaemmerer, E.; Westerkamp, M.; Kasperk, R.; Niepmann, G.; Scherer, A.; Gassler, N. Coincidence of active Crohn’s disease and florid endometriosis in the terminal ileum: A case report. World J. Gastroenterol. 2013, 19, 4413–4417. [Google Scholar] [CrossRef] [PubMed]
- Jess, T.; Frisch, M.; Jørgensen, K.; Pedersen, B.; Nielsen, N. Increased risk of inflammatory bowel disease in women with endometriosis: A nationwide Danish cohort study. Gut 2012, 61, 1279–1283. [Google Scholar] [CrossRef]
- Saha, S.; Midtling, E.; Roberson, E.; Nair, V.; Wald, A.; Reichelderfer, M. Dysmenorrhea in women with Crohn’s disease: A case-control study. Inflamm. Bowel Dis. 2013, 19, 1463–1469. [Google Scholar] [CrossRef] [PubMed]
- Ananthakrishnan, A.; Higuchi, L.; Huang, E.; Khalili, H.; Richter, J.M.; Fuchs, C.; Chan, A. Aspirin, nonsteroidal anti-inflammatory drug use, and risk for Crohn disease and ulcerative colitis: A cohort study. Ann. Intern. Med. 2012, 156, 350–359. [Google Scholar] [CrossRef]
- Takeuchi, K.; Smale, S.; Premchand, P.; Maiden, L.; Sherwood, R.; Thjodleifsson, B.; Bjornsson, E.; Bjarnason, I. Prevalence and mechanism of nonsteroidal anti-inflammatory drug-induced clinical relapse in patients with inflammatory bowel disease. Clin. Gastroenterol. Hepatol. 2006, 4, 196–202. [Google Scholar] [CrossRef] [PubMed]
- Nurmi, E.; Haapamäki, J.; Paavilainen, E.; Rantanen, A.; Hillilä, M.; Arkkila, P. The burden of inflammatory bowel disease on health care utilization and quality of life. Scand. J. Gastroenterol. 2013, 48, 51–57. [Google Scholar] [CrossRef]
- Graff, L.; Walker, J.; Lix, L.; Clara, I.; Rawsthorne, P.; Rogala, L.; Miller, N.; Jakul, L.; McPhail, C.; Ediger, J.; et al. The relationship of inflammatory bowel disease type and activity to psychological functioning and quality of life. Clin. Gastroenterol. Hepatol. 2006, 4, 1491–1501. [Google Scholar] [CrossRef]
- Hauser, G.; Tkalcić, M.; Stimac, D.; Milić, S.; Sincić, B. Gender related differences in quality of life and affective status in patients with inflammatory bowel disease. Coll. Antropol. 2011, 35, 203–207. [Google Scholar]
- Yan, X.; Qiao, Y.; Tong, J.; Mao, R.; Liang, J.; Lv, C.; Chen, Y.; Wang, Y.; Shen, J. Assessment of patient-centered outcomes (PROs) in inflammatory bowel disease (IBD): A multicenter survey preceding a cross-disciplinary (functional) consensus. Health Qual. Life Outcomes 2020, 18, 241. [Google Scholar] [CrossRef]
- Pittet, V.; Vaucher, C.; Froehlich, F.; Burnand, B.; Michetti, P.; Maillard, M. Patient self-reported concerns in inflammatory bowel diseases: A gender-specific subjective quality-of-life indicator. PLoS ONE 2017, 12, e0171864. [Google Scholar] [CrossRef]
- Saraiva, S.; Cortez-Pinto, J.; Barosa, R.; Castela, J.; Moleiro, J.; Rosa, I.; da Siva, J.; Dias Pereira, A. Evaluation of fatigue in inflammatory bowel disease—A useful tool in daily practice. Scand. J. Gastroenterol. 2019, 54, 465–470. [Google Scholar] [CrossRef]
- Bager, P.; Befrits, R.; Wikman, O.; Lindgren, S.; Moum, B.; Hjortswang, H.; Hjollund, N.; Dahlerup, J. Fatigue in out-patients with inflammatory bowel disease is common and multifactorial. Aliment. Pharmacol. Ther. 2012, 35, 133–141. [Google Scholar] [CrossRef]
- Le Berre, C.; Peyrin-Biroulet, L.; Buisson, A.; Olympie, A.; Ravel, M.; Bienenfeld, C.; Gonzalez, F. Impact of inflammatory bowel diseases on working life: A French nationwide survey. Dig. Liver Dis. 2019, 51, 961–966. [Google Scholar] [CrossRef]
- Van de Vijver, E.; Van Gils, A.; Beckers, L.; Van Driessche, Y.; Moes, N.; van Rheenen, P. Fatigue in children and adolescents with inflammatory bowel disease. World J. Gastroenterol. 2019, 25, 632–643. [Google Scholar] [CrossRef]
- Jedel, S.; Hood, M.; Keshavarzian, A. Getting personal: A review of sexual functioning, body image, and their impact on quality of life in patients with inflammatory bowel disease. Inflamm. Bowel Dis. 2015, 21, 923–938. [Google Scholar] [CrossRef]
- Perez de Arce, E.; Quera, R.; Ribeiro Barros, J.; Yukie Sassaki, L. Sexual Dysfunction in Inflammatory Bowel Disease: What the Specialist Should Know and Ask. Int. J. Gen. Med. 2021, 14, 2003–2015. [Google Scholar] [CrossRef]
- Marrie, R.; Walker, J.; Graff, L.; Patten, S.; Bolton, J.; Marriott, J.; Fisk, J.; Hitchon, C.; Peschken, C.; Bernstein, C. Gender differences in information needs and preferences regarding depression among individuals with multiple sclerosis, inflammatory bowel disease and rheumatoid arthritis. Patient Educ. Couns. 2019, 102, 1722–1729. [Google Scholar] [CrossRef]
- Lebel, U.; Luwisch-Omer, S.; Possick, C. “Backstage Autonomy”: Religious-Zionist State Widows in Second Marriages Manage Competing Expectations. J. Women Politics Policy 2018, 39, 336–358. [Google Scholar] [CrossRef]
- Lebel, U.; Masad, D. Life Scripts, Counter Scripts and Online Videos: The Struggle of Religious-Nationalist Community Epistemic Authorities against Military Service for Women. Religions 2021, 12, 750. [Google Scholar] [CrossRef]

| Study | Study Population | Outcome |
|---|---|---|
| Fujimoto et al., 2007 [5]. | 844 UC patients. | Male UC patients significantly increased from 1981 to 2000. |
| Jiang et al., 2006 [6]. | 63 CD, 389 UC patients. | Male predominance in IBD. Ratio male to female patients = 1.53:1 in UC, 2.32:1 in CD. |
| Yang et al., 2008 [7]. | 138 CD, 341 UC patients. | Marked male predominance in CD incidence but not in UC. CD: 102 men, 36 women; UC: 170 men, 171 women. |
| Gearry et al., 2006 [8]. | 715 CD, 668 UC patients. | Female predominance in CD incidence but not in UC: CD: 293 men, 422 women; UC: 342 men, 326 women. |
| Shah et al., 2018 [10]. | 95,605 CD patients (42,831 males, 52,774 females) 112,004 UC patients (61,672 males, 50,332 females). | No gender difference in UC incidence except for the age group of 5–9 years, until age 45 years; thereafter, men had a significantly higher incidence of UC than women. |
| Kyle, 1992 [12]. | 914 CD patients. | Female predominance (63%) in CD incidence. |
| Latour et al., 1998 [13]. | 137 CD, 111 UC patients. | Female predominance in CD. CD Female/male ratio: 1.6; UC Female/male ratio: 0.5. |
| Shivananda et al., 1987 [14]. | 1040 IBS patients: 210 CD, 257 UC and 573 patients with no disease classification for incomplete data. | Female predominance in CD (male/female ratio = 1:1.33). |
| Leong et al., 2004 [17]. | 80 CD patients. | Male predominance in CD (male/female ratio = 2.5:1). |
| Zelinkova et al., 2012 [19]. | 608 familial IBD and 415 sporadic IBDs patients. | Females in familial IBD population was significantly higher (61%; female/male ratio = 1.5) compared with sporadic IBD (54%; female/male ratio = 1.2). Significantly higher female to female transmission vs. female to male transmission rate (36 vs. 18). Significantly higher number of mother-to-child transmissions vs. father to child transmissions (55 vs. 32). The female imprinting was specifically related to Crohn’s disease (31 vs. 14 mother vs. father to child transmissions, respectively). |
| Tedde et al., 2008 [20]. | 203 UC unrelated patients, 391 controls. | Significant association between mean age at onset of UC and the different IL10-1082 genotypes, observed only in females after gender stratification. |
| Lin Z. et al., 2010 [21]. | 106 familial IBDs and 107 sporadic IBDs patients. | Association of IL23R-L310P variant with female UC and female IBD overall, but not with female CD. Association of IL23R-R381Q variant with female CD, but not with female UC, nor with IBD overall. This evidence suggests in females a protective role of IL23R variant R381Q against CD and IBD overall and of the variant L310P against UC. |
| Jaźwińska-Tarnawska et al., 2015 [22]. | 61 IBDs patients, 101 controls. | In frequency distributions, significant correlation between gender and C3435T genotype of ABCB1 gene, both for IBD and CD patients, with 3435CT heterozygote prevailing in IBD and CD males. In odds ratio, significant difference for the 3435CT genotype between control and: IBDs as a whole; IBD males; CD males; and for 3435TT variant in control vs. IBD males. Data suggesting 3435CT genotype as risk factor for IBD and CD in males, while 3435TT genotype in males as protective for IBD. |
| Friedrichs et al., 2006 [23]. | 613 CD patients, 749 controls. | Odds ratio for the R30Q variant of DLG5 gene in CD patients: 2.49 in males; 1.01 in females. R30Q variant constitutes a susceptibility factor for CD in men. |
| Biank et al., 2007 [24]. | 281 CD (181 trios) patients, 479 controls in pediatric age. | Significant negative association for R30Q in female children (OR 0.39), but not in male children. DLG5 protective effect in CD for female children. |
| Vermeire et al., 2001 [26]. | 79 sibling pairs (68 CD, 11 mixed) were genotyped at 12 microsatellite markers covering the X chromosome. In the second stage, 10 additional markers in the X-pericentromeric region were studied in the families involved in stage 1 together with 62 additional families (52 sibling pairs, 14 s-degree relative pairs). | In the first stage, evidence for linkage was found over a 30-cM pericentromeric region spanning dXs991, dXs990, and dXs8096 (multipoint maximum LOD score in the CD subgroup, 2.5; p = 0.0003). The remainder of the X chromosome was excluded (exclusion under LOD-2) for a locus with lambda(s) = 2. Fine mapping in the second stage confirmed linkage and narrowed and shifted the linked region to Xq21.3 around dXs1203 (nonparametric linkage (NPL), 2.90; p = 0.0017). The NPL-1 interval around the linkage peak comprises 19.7 cM. |
| Lee et al., 2017 [27]. | 1505 IBD patients (922 CD, 583 UC during the discovery phase), and 4041 controls. Additional 1989 IBD patients (993 CD, 996 UC) and 3491 controls. | Significant association of a previously reported inflammatory bowel disease susceptibility locus at chromosome Xq26.3 (CD40LG-ARHGEF6; odds ratio, 1.22; 95% confidence interval, 1.16–1.28; combined p = 3.79 × 10−15). This locus accounted for 0.18% and 0.12% of genetic variance in CD and UC, respectively, and increased the total autosomal chromosome genetic variance from 6.65% to 6.83% and from 5.47% to 5.59% for CD and UC risk, respectively, in the Korean population. Sex-stratified analyses did not reveal sex-related differences in effect sizes. |
| Kudelka et al., 2018 [28]. | Mice: Cosmcf/y (KO), Vil-Cre+; Cosmcf/+ (mosaic), and Vil-Cre+ (WT) controls. | Cosmc regulates host genes, bacterial ligands, and nutrient availability to control microbiota biogeography. Loss of one Cosmc allele in males (IEC-Cosmc-/y) resulted in a compromised mucus layer, spontaneous microbe-dependent inflammation, and enhanced experimental colitis; however, females with loss of one allele and mosaic deletion of Cosmc in 50% of crypts (IEC-Cosmc+/−) were protected from spontaneous inflammation and partially protected from experimental colitis, likely due to lateral migration of normal mucin glycocalyx from WT cells over KO crypts. |
| Study | Study Population | Outcome |
|---|---|---|
| Wagtmans et al., 2001 [11]. | 541 CD patients (266 males, 275 females). | No difference in mean lag time between onset of symptoms and diagnosis, and no differences in presenting symptoms and initial localization of lesions. Similar percentage of patients who underwent an abdominal operation (81% vs. 77%). No difference in mean lag-time between onset of symptoms and first bowel resection. Lag-time between bowel resection and recurrence of disease shorter in women than in men (4.8 yr vs. 6.5 yr), ileocecal resections more frequent in female than male patients (44% and 32%, respectively). Female patients have significantly more often relatives in the first or second degree affected by CD than male (15% vs. 8.3%). |
| Severs et al., 2018 [18]. | Dutch IBD Biobank study: 2118 CD and 1269 UC patients. COIN study: 1139 CD and 1213 UC patients. | Early onset CD (<16 years) more frequent in males than in females (20% vs. 12%). Male CDs have more often ileal disease (28% vs. 20%) and underwent more often small bowel and ileocecal resection. Male CDs used prednisone more often and suffered more often from osteopenia. IBD-specific healthcare costs did not differ between male and female IBD patients. Extraintestinal manifestations more frequent in female IBD patients than male. |
| Mazor et al., 2011 [33]. | 146 patients with CD (76 females, 70 males) treated during a 10-year period. | The only independent risk factors associated with developing a complication were smoking and male gender. There was no association between developing complications and the presence of selected SNPs (p = 0.07 for tyrosine residue on both alleles in NCF4 SNP rs4821544 and p = 0.06 for a guanine residue on both alleles in ATG16L SNP rs2241880). Multivariate analysis using a backwards logistic regression model left only male gender as an independent statistically significant association with complicated disease (OR 2.6017, 95% CI: 1.17 to 5.75). The median time to developing a complication was 4 years, and the most common complication was the need for surgical intervention (54%). |
| Blumenstein et al., 2011 [34]. | 986 patients with IBD (515 CD, 471 UC—537 females, 449 males). | Extended disease duration in women, no significant gender-related differences in demographic and clinical characteristics observed. Men showed a significantly higher remission rate than women (p = 0.025), while women received significantly less immunosuppressive medication compared to men (p = 0.011). Treatment with immunosuppressants was not different in women with child-bearing potential compared to menopausal women. |
| Bokemeyer et al., 2013 [35]. | 1032 patients with IBD (511 CD, 519 UC, 2 IBD-U). | About one third of the IBD patients were not in clinical remission (CDAI ≥ 150/CAI > 4) (CD: 45%; UC: 27%), although high rates of immunosuppressive drugs (CD: 47%; UC 26%) were administered. This study shows a large burden of active disease associated with an unexpectedly high (co)morbidity and high psychosocial impairments, indicating a reduced health state in IBD patients. |
| Greuter et al., 2018 [36]. | 1638 CD patients (107 presented with upper GI tract involvement at the time of diagnosis, 214 at any time). | In a multivariate logistic regression model, male sex, and diagnosis between 2009 and 2016 (versus before 1995) were independent predictors for presence of upper GI tract involvement at CD diagnosis (odds ratio [OR] 1.600, p = 0.021 and OR 2.686, p < 0.001, respectively), whereas adult age was a negative predictor (OR 0.388, p = 0.001). Patients with upper GI tract involvement showed a disease course similar to control patients (hazard ratio [HR] for any complications 0.887, (95% confidence interval [CI] 0.409–1.920), and a trend towards occurrence of fewer intestinal fistulas (log-rank test p = 0.054). |
| Jussila et al., 2014 [38]. | 21,964 patients with IBD (5315 CD, 16,649 UC). | Overall mortality was increased among patients with CD (standardized mortality ratio (SMR) 1.33, 95% confidence interval 1.21–1.46) and UC (1.10, 1.05–1.15). SMR was significantly increased for gastrointestinal causes in CD (6.53, 4.91–8.52) and UC (2.81, 2.32–3.34). Patients with UC were found also to have increased SMR from pulmonary (1.24, 1.02–1.46) and cardiovascular disease (1.14, 1.06–1.22) and cancers of the colon (1.90, 1.38–2.55), rectum (1.79, 1.14–2.69) and biliary tract (5.65, 3.54–8.54), whereas SMR from alcohol-related deaths was decreased (0.54, 0.39–0.71). Patients with CD had a significantly increased SMR for pulmonary diseases (2.01, 1.39–2.80), infections (4.27, 2.13–7.63) and cancers of the biliary tract (4.51, 1.23–11.5) and lymphoid and hematopoietic tissue (2.95, 1.85–4.45). |
| Peyrin-Biroulet et al., 2013 [39]. | 310 patients with CD (154 females, 156 males). | The cumulative probability of major abdominal surgery was 38, 48, and 58% at 5, 10, and 20 years after diagnosis, respectively. Baseline factors significantly associated with time to major abdominal surgery were: ileocolonic (hazards ratios (HRs) 3.3), small bowel (HR, 3.4), and upper gastrointestinal (HR, 4.0) extent, relative to colonic alone; current cigarette smoking (HR, 1.7), male gender (HR, 1.6), penetrating disease behavior (HR, 2.7), and early corticosteroid use (HR = 1.6). Major abdominal surgery rates remained stable, with 5-year cumulative probabilities in 1970–1974 and 2000–2004 of 37.5 and 35.1%, respectively. The cumulative probability of major abdominal surgery in this population-based cohort of Crohn’s disease approached 60% after 20 years of disease, and many patients required second or third surgeries. Non-colonic disease extent, current smoking, male gender, penetrating disease behavior, and early steroid use were significantly associated with major abdominal surgery. |
| Walldorf et al., 2013 [40]. | 293 patients with IBD (195 CD, 98 UC—110 males, 183 females). | DEXA-scan was performed in 174 patients (59 males, 115 females). Bone mineral density (BMD) was impaired in 38.5% of these patients. Male patients were diagnosed more often with osteopenia or osteoporosis than females (55.9% vs. 29.6%, p = 0.03) and had a risk of bone disease comparable to postmenopausal women. Additionally, duration of corticosteroid treatment and IBD were identified as risk factors for osteoporosis. Follow up DEXA-scan demonstrated an overall deterioration of BMD in patients with normal baseline results. |
| Sigurdsson et al., 2022 [42]. | 49 young adult male patients with childhood-onset IBD and 245 matched controls. | The group of young adult patients had, in comparison with the controls, significantly smaller median cortical area (126.1 mm2 vs 151.1 mm2, p < 0.001), lower median total vBMD (296.7 mg/cm3 vs. 336.7 mg/cm3, p < 0.001), and lower median cortical vBMD (854.4 mg/cm3 vs. 878.5 mg/cm3, p < 0.001). Furthermore, the patients compared with the controls had lower median trabecular volume fraction (16.8% vs. 18.2%, p < 0.001) and thinner median trabeculae (0.084 mm vs. 0.089 mm, p < 0.001). The differences between the patients with IBD and controls persisted in multivariable analyses that included adjustments for SMI and physical exercise. |
| Heath et al., 2022 [50]. | 1015 patients; 656 CD (59.0% women) and 359 UC (47.9% women). | Women were more likely prescribed budesonide than men (23.6% vs. 13.4%; p < 0.0001), more men were exposed to prednisone for IBD management (73.5% vs. 67.4%; p = 0.04). Immunomodulator use was higher in men with CD versus women (86.6% vs. 78.3%; p = 0.008) and of those exposed, women more commonly experienced ADRs (29.5% vs. 21.2%; p = 0.01). Though no sex-related difference was identified, age was a predictor of biologic exposure in women with CD and men with UC, with those > 55 being less likely to receive biologics. |
| Study | Study Population | Outcome |
|---|---|---|
| Baird et al., 1990 [55]. | 261 women with IBD, (177 CD, 84 UC) matched controls. | No evidence of increased risk of pregnancy loss. The risk of preterm birth was significantly elevated for patients with CD (odds ratio, 3.1; 95% confidence interval, 1.8–5.4) and for those with UC (odds ratio, 2.7; 95% confidence interval, 1.8–5.4). |
| Hudson et al., 1997 [56]. | 409 women with IBD (177 CD, 232 UC). | Women with UC and CD had normal fertility when compared with the general population. However, unresolved infertility problems were more frequent in women who had undergone surgery for inflammatory bowel disease compared with those who had not (12% vs. 5% for Crohn’s disease; 25% vs. 7% for ulcerative colitis). Disease relapse rates did not increase in pregnancy. |
| Khosla et al., 1984 [57]. | 112 married women with CD. | Infertility rate (12%) similar to the general population. Patients in remission during conception had a normal pregnancy. In the majority CD remained quiescent. |
| Marri et al., 2007 [58]. | 169 females aged 15–44 years with IBD (110 CD, 59 UC). | The rates of no voluntary childlessness in IBD were similar to the general population. Women with IBD also had fewer children than their national counterparts. |
| Fréour et al., 2012 [59]. | Serum levels of AMH were measured (50 women with CD in remission, 163 controls). | Women with CD do not have severe ovarian reserve alterations compared to a control population. Age ≥ 30 years and a colonic location of the disease could be associated with an accelerated loss of follicles. |
| Ban et al., 2015 [60]. | 9639 women with IBD (4475 CD, 4354 UC), and 2,131,864 controls. | Women with CD have marginally lower fertility rates. These rates decreased following flares and surgical interventions. Fertility rates returned almost to normal when women were not prescribed contraception but the reduction following surgical intervention remained. |
| Şenateş et al., 2013 [61]. | Serum AMH levels measured in 35 women with CD and 35 age-matched controls. | AMH levels in CD patients (1.02 ± 0.72) were significantly lower compared to the controls (1.89 ± 1.80) (p = 0.009). Serum AMH levels in CD patients with active disease (0.33 ± 0.25) were significantly lower compared to CD patients who were in remission (1.53 ± 0.49) (p = 0.001). In CD patients, a negative correlation between CD disease activity and serum AMH levels was found (r = −0.718, p < 0.001). |
| Lee et al., 2020 [62]. | 2058 women with IBD (589 CD, 1469 UC) and 20,580 age-matched controls. | With the exception of moderate to severe disease, the incidences of adverse pregnancy outcomes in women with IBD are similar to that of the general population. |
| Oresland, 1994 [64]. | 21 women with UC operated with endoanal mucosectomy and a handsewn ileal pouch-anal anastomosis. | Gross abnormalities were seen on hysterosalpingography but were of a magnitude no greater than that after the conventional proctocolectomy. 2/3 of the women who attempted to become pregnant, failed in five years of fu, indicating a high incidence of infertility. |
| Wikland, 1990 [66]. | 71 women who had a proctocolectomy (30 CD, 41 UC). | Fertility was significantly reduced after surgery since only 37% (10/27) of the women who attempted to become pregnant succeeded within 5 years follow-up. Conventional proctocolectomy in women will result in distressing vaginal discharge, and dyspareunia in a considerable proportion of the patients. The operation seems to decrease their chances of becoming pregnant. |
| Mountifield et al., 2009 [67]. | 255 patients (72 males, 183 females- 127 CD, 85 UC, 5 IBD-U). | The average fertility rate was no different between women with CD and UC (1.0 and 1.2 births/woman, respectively; p = 0.553), compared with 1.81 for all Australian women. Although 42.7% of IBD patients reported a fear of infertility, patients only sought medical fertility advice at the same rate as the general population. Fear of infertility was most evident in women, those with CD, and those reporting previous surgery. Specific patient concerns, which appear to have decreased patients’ family size, included IBD heritability, the risk of congenital abnormalities, and medication teratogenicity. |
| Bortoli et al., 2011 [70]. | 332 pregnant women with IBD (145 CD, 187 UC) and 332 controls. | No statistically significant differences in frequency of abortions, preterm deliveries, caesarean sections, congenital abnormalities, and birth weight were observed comparing CD and UC women with their non-IBD controls. |
| Van der Giessen et al., 2011 [72]. | IBD patient-derived inflammatory organoid models and 2D cell lines models. | Progesterone and estrogen improved wound healing and epithelial barrier function in intestinal epithelial cells via upregulation of tight junction proteins. Furthermore, these sex hormones significantly reduced ER stress and reduce pro-inflammatory cytokine production in intestinal epithelial models. The study shows that estrogen and progesterone alleviate ER stress, decrease pro-inflammatory cytokine production, stimulate wound healing, and increase barrier function of epithelial cells. Pregnancy hormones can have beneficial effects on disease activity by positively modulating the intestinal epithelial lining. |
| Julsgaard et al., 2011 [73]. | 115 women with UC who gave birth. | Adherence to the therapy was high despite fear of a negative effect on fertility or the fetus. Counseling predicted higher adherence. This may be important because our study suggests an increase in UC activity during pregnancy. |
| Pierdominici et al., 2015 [76]. | Intracellular expression of ERα and ERβ in peripheral blood T lymphocytes from 48 patients with IBD (26 CD, 22 UC) and 29 healthy controls. | Significant reduction (p < 0.05) in estrogen receptor (ER) β expression in peripheral blood T lymphocytes from CD/UC patients with active disease (n = 27) as compared to those in remission (n = 21) and healthy controls (n = 29). |
| Goodman et al., 2014 [77]. | SAMP1/YitFc (SAMP) mice—model of chronic intestinal inflammation similar to human CD. | Conventional T cells (Tconv) and Tregs responded differentially to estrogen signaling, leading to distinct immunoprotective effects mediated by distinct estrogen receptor (ER) isoforms. These mechanisms were impaired in T cells from SAMP-F mice. Thus, hormone signaling influences the expansion and function of GALT Tregs in an ER-dependent manner and contributes to gender-based differences in experimental CD. |
| Webe et al., 1995 [79]. | 662 women with IBD (360 CD, 251 UC, 51 IBD-U). | 60% of women with CD and 53% with UC experienced menstrual cycle abnormalities. Gynecologic conditions are common in women with inflammatory bowel disease, including menstrual abnormalities, vaginal discharge, infertility, and gynecologic surgery. |
| Saha et al., 2014 [80]. | 121 women with IBD. | 25% of patients experienced a change in cycle interval in the year before IBD diagnosis and 21% experienced a change in the duration of flow. Among women with dysmenorrhea, 40% experienced a change in the intensity of their menstrual pain, 31% experienced a change in its duration. Overall cycle regularity increased over time. Changes in menstrual function occur frequently in the year before IBD diagnosis. |
| Lichtarowicz et al., 1989 [81]. | 146 women with CD. | A logistic analysis showed that 50% of women with CD had the menopause at 47.6 years compared with 49.6 years in a group of healthy women from the same area. The two groups had similar smoking habits. Premature menopause seems associated with CD. |
| Khalili et al., 2012 [84]. | 108,844 postmenopausal women without a prior history of CD or UC. | Postmenopausal hormone therapy was associated with an increased risk of UC but not CD. These findings indicate that pathways related to estrogens might mediate the pathogenesis of UC. HR for UC was 1.71 (95% CI, 1.07–2.74) among women who currently used hormones and 1.65 (95% CI, 1.03–2.66) among past users. |
| Timmer et al., 1998 [85]. | 152 patients with CD, 88 women. | Unfavorable outcomes for women (p = 0.05), current smokers (p = 0.005), and use of oral contraceptives (p = 0.001) for what concerns relapses in patients with CD. |
| Cosnes et al., 1999 [86]. | 331 women with CD. | Unlike smoking, oral contraceptives have no effect on CD activity. |
| Khalili et al., 2013 [87]. | 117,375 women enrolled since 1976 in the Nurses Health Study I (NHS I) and 115,077 women enrolled since 1989 in the Nurses’ Health Study II (NHS II) with no prior history of UC or CD. | Oral contraceptive use was associated with risk of CD. |
| Saha et al., 2013 [94]. | 110 women 40% had dysmenorrheal (54 CD, 66 controls). | Dysmenorrhea is common in women with CD and has an additive effect on overall pain severity. Menstrual distress is positively correlated with CD activity scores and associated with lower HRQOL by some measures. |
| Ananthakrishnan et al., 2012 [95]. | 76,795 women who provided data about aspirin and NSAID use. | 123 incident cases of CD and 117 cases of UC occurred over 18 years and 1,295,317 person-years of follow-up. Frequent use of NSAIDs but not aspirin seemed to be associated with increased absolute incidence of CD and UC. |
| Takeuchi et al., 2006 [96]. | 209 patients with IBD. | Nonselective NSAIDs were associated with a 17–28% relapse rate within 9 days of ingestion. No patient had an early relapse on acetaminophen, nimesulide, or aspirin, whereas those on naproxen and nabumetone (20%) experienced relapse. These clinical relapses were associated with escalating intestinal inflammatory activity. |
| Study | Study Population | Outcome |
|---|---|---|
| Nurmi et al., 2013 [97]. | 556 patients with IBD (292 females, 264 males). | Women had seen doctors more often than men (p < 0.001). Women were absent from work more frequently than men (p = 0.01). The amount of physician visits, work absenteeism, and a higher amount of undergone procedures were related to impaired HRQoL (p < 0.001 on all accounts). |
| Graff et al., 2006 [98]. | 388 patients with IBD. | Multivariate regression showed that those with active disease had higher levels of distress, health anxiety, and perceived stress, lower social support, well-being and mastery, and poorer disease-specific QOL, relative to those with inactive disease. Participants with either active or inactive disease had suboptimal general QOL. |
| Hauser et al., 2011 [99]. | 112 IBD patients (51 CD, 61 UC—50 females, 62 males). | Women have expressed significantly lower level of the general HRQoL and more emotional disturbances connected with their disease as well as more frequent bowel symptoms compared with men. |
| Yan et al., 2020 [100]. | 891 IBD patients (522 CD, 363 UC, 6 IBD-U—362 females, 529 males). | Female patients showed a higher tendency to feel that the quality of communication with specialists (p = 0.037) and quality of IBD care (p = 0.019) was less satisfactory than male patients. Female patients with IBD show a larger number of intense concerns, a greater level of psychological disturbance, a higher symptom load, and a poorer QoL than men, resulting in reduced satisfaction ratings. |
| Pittet et al., 2017 [101]. | 1102 IBD patients (596 CD, 475 UC, 31 IBD-U—598 females, 504 males). | Women had significantly higher overall levels of concern than did men (sum score: 47.5 vs. 42.8, respectively, p < 0.001). Women at home or unemployed had higher concerns about disease-related constraints and uncertainty (p = 0.004). Patients seem to have important gender-specific concerns related to their illness. |
| Saraiva et al., 2019 [102]. | 105 IBD patients (60 CD, 45 UC—60 females, 45 males). | Female gender and active CD were significantly associated with a severe level of fatigue (p = 0.05 and p = 0.04). |
| Bager et al., 2012 [103]. | 425 IBD patients (251 CD, 174 UC). | Female IBD patients tend to experience more fatigue than males. When comparing the IBD patients with disease activity to the IBD patients in remission, all dimensions of fatigue were statistically significant (p <0.05). Fatigue in IBD is common regardless of anaemia or iron deficiency. Fatigue in IBD is most marked for patients <60 years of age. Fatigue is expressed differently between groups. |
| Le Berre et al., 2019 [104]. | 1410 IBD patients (875 CD, 496 UC, 39 IBD-U). | Among the disabling symptoms at work, fatigue was the most frequent (41%) followed by diarrhea (25%) and fecal incontinence (18%). IBD has a strong negative impact on working life. While work satisfaction remains high, IBD affects career plans. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lungaro, L.; Costanzini, A.; Manza, F.; Barbalinardo, M.; Gentili, D.; Guarino, M.; Caputo, F.; Zoli, G.; De Giorgio, R.; Caio, G. Impact of Female Gender in Inflammatory Bowel Diseases: A Narrative Review. J. Pers. Med. 2023, 13, 165. https://doi.org/10.3390/jpm13020165
Lungaro L, Costanzini A, Manza F, Barbalinardo M, Gentili D, Guarino M, Caputo F, Zoli G, De Giorgio R, Caio G. Impact of Female Gender in Inflammatory Bowel Diseases: A Narrative Review. Journal of Personalized Medicine. 2023; 13(2):165. https://doi.org/10.3390/jpm13020165
Chicago/Turabian StyleLungaro, Lisa, Anna Costanzini, Francesca Manza, Marianna Barbalinardo, Denis Gentili, Matteo Guarino, Fabio Caputo, Giorgio Zoli, Roberto De Giorgio, and Giacomo Caio. 2023. "Impact of Female Gender in Inflammatory Bowel Diseases: A Narrative Review" Journal of Personalized Medicine 13, no. 2: 165. https://doi.org/10.3390/jpm13020165
APA StyleLungaro, L., Costanzini, A., Manza, F., Barbalinardo, M., Gentili, D., Guarino, M., Caputo, F., Zoli, G., De Giorgio, R., & Caio, G. (2023). Impact of Female Gender in Inflammatory Bowel Diseases: A Narrative Review. Journal of Personalized Medicine, 13(2), 165. https://doi.org/10.3390/jpm13020165









