Abstract
We evaluated the sex-specific difference in response upon participation in an exercise program with respect to the risk of adverse clinical outcomes among patients with peripheral artery disease (PAD) and claudication. The records of 400 PAD patients were assessed between 2012 and 2015. Two hundred of them were addressed to a walking program prescribed at the hospital and executed at home at symptom-free walking speed (Ex), while the remaining 200 acted as a control group (Co). The number and date of deaths, all-cause hospitalizations, and amputations for a 7-year period were collected from the regional registry. At baseline, no differences were observed (MEX n = 138; FEX n = 62; MCO n = 149; FCO n = 51). The 7-year survival rate was significantly higher in FEX (90%) than in MEX (82% hazard ratio, HR: 0.542 95% CI 0.331–0.885), FCO (45%, HR: 0.164 95% CI 0.088–0.305), and MCO (44%; HR: 0.157 95% CI 0.096–0.256). A significantly lower rate of hospitalization (p < 0.001) and amputations (p = 0.016) was observed for the Ex group compared to the Co group, without differences by sex. In conclusion, in PAD patients, active participation in a home-based pain-free exercise program was associated with a lower rate of death and better long-term clinical outcomes, particularly among women.
1. Introduction
Cardiovascular diseases (CVDs) are the leading cause of death globally, accounting for an estimated 17.9 million lives each year [1]. Their incidence, which is lower in premenopausal women, rises after the menopausal transition, possibly due to the loss of the cardioprotective role of sex steroid hormones and their receptors [2,3,4,5,6]. In light of the fact that biological factors may be responsible for sex-specific protective and harmful effects, sex differences may impact the presentation, development, clinical management, and outcome of CVD, including peripheral artery disease (PAD) [6,7,8,9]. This expression of systemic atherosclerosis, which affects more than 6 million individuals ≥40 years of age [6], may affect mobility and is associated with higher rates of cardiovascular death and major cardiovascular events [10,11,12].
In terms of presentation, among women, the lower limb symptoms typical of PAD may be more frequently absent, atypical, or underrecognized for concomitant musculoskeletal or osteoarticular diseases [13,14]. However, their functioning may be worse than that of men, with women showing lower functional status, lower limb strength, and faster functional decline [15,16,17,18]. In terms of outcomes, the data from invasive treatments are contradictory. Worse clinical outcomes are reported for women, such as a higher rate of adverse events, postoperative outcomes and in-hospital mortality, and discharge to a nonhome facility after surgery [19,20,21,22,23,24,25]. Conversely, equal or even better outcomes are also reported among females when compared to males [26,27,28]. However, in addition to a lower willingness to undergo vascular surgery interventions [29], women are also undertreated or poorly adherent to risk factor control therapy [30,31,32,33].
Considering all these issues, rehabilitation, which in PAD is a recommended alternative to revascularization at intermediate stages of disease [34,35] due to its capacity to counteract walking disability and cardiovascular risk [35], may represent a crucial intervention for women’s health. Data from the SWEDEHEART registry showed that participation in an exercise-based rehabilitation program was associated with reduced total mortality, particularly in women [7]. Unfortunately, for rehabilitative outcomes, sex differences are also reported, with participation in exercise programs in PAD, as in various chronic diseases, being limited by barriers in terms of referral, enrollment, and completion and outcomes, particularly among women [36,37,38]. Conversely, a structured pain-free exercise program for PAD patients prescribed at a hospital and performed at home designed to reduce most barriers to exercise [39,40] proved to obtain adherence and functional outcomes without gender differences [41,42].
In the absence of data reporting the long-term outcomes following rehabilitation in PAD, we investigated whether sex differences in clinical outcomes and rate of survival are observable at the 7-year follow-up in a cohort of patients discharged from the mentioned structured home-based program [39] compared to a cohort of PAD patients not exposed to rehabilitation.
2. Materials and Methods
2.1. Study Design and Setting
This is a single-center cohort study carried out at the University Hospital of Ferrara. The Local Ethics Committee (CE-AVEC) approved the study (number 277/2019), but written informed consent was not attainable from all participants. The study is reported according to the STROBE guidelines [43].
This single-center study retrospectively analyzed a prospectively collected database of PAD patients who were studied at the Units of Vascular Surgery or at the Unit of Clinica Medica and partly referred for the training program at the Unit of Rehabilitation Medicine.
A total of 400 consecutive PAD patients were recruited between 2012 and 2015. The follow-up period started from their recruitment and lasted for 7 years. Data concerning long-term outcomes were gathered from the Emilia-Romagna health service registry.
2.2. Participants
Two hundred PAD patients at Leriche-Fontaine’s stage II were enrolled in the rehabilitation program. Patients with ischemic rest pain or foot ulcers or with severe cardiovascular conditions contraindicating exercise were excluded.
A parallel group of another 200 PAD patients with the same inclusion and exclusion criteria was also studied from the cohort of patients referred to the Units of Vascular Surgery and Clinica Medica in the same temporal frame. These patients were not referred to the rehabilitation program, or they refused or postponed participation.
According to study objectives, the patients were then categorized into four subgroups: males and females who underwent the exercise program (MEX and FEX) and control males and females (MCO and FCO).
2.3. Exercise Group
All patients received the “test in–train out” home-based exercise program [39,40]. The structured exercise was prescribed at the hospital during circa-monthly visits and was executed at home. The program encompassed two daily 10-min sessions of intermittent walking (with a 1:1 walk:rest ratio) at a prescribed speed. The training speed, converted into a walking cadence (steps/minute) and paced at home by a metronome, was slower than the individual’s walking speed at the beginning and increased weekly. The walking speed was increased by approximately by 3±1 steps per minute each week. A record of the training sessions was requested and collected at each visit. The patients were discharged from the program when a satisfactory improvement in the pain-free walking distance was attained, usually within 9 months. More details on the exercise program are reported elsewhere [39,40].
2.4. Control Group
Patients in the control group were treated with optimal medical therapy and advised to maintain a healthy and active lifestyle, according to the guidelines and follow-up visits from the vascular surgeons [35].
2.5. Study Variables
The primary outcome was survival probability, assessed from the date of enrollment to the following seven years. For patients who did not reach that follow-up limit, data were censored on 30 June 2020.
Secondary outcomes included all-cause hospitalizations and amputations. In this secondary analysis, both minor and major amputations were considered; in case of multiple procedures, only the first one was considered. Additionally, for the secondary outcomes, in patients who did not reach the 7-year follow-up limit, data were censored at the date of death, if present, or at the date of 30 June 2020.
2.6. Statistical Analysis
A Shapiro-Wilk test was performed to verify the data distribution. Differences in baseline characteristics for the two groups and the four subgroups were assessed using Chi-squared tests, Student’s t test or Mann-Whitney test, or one-way analysis of variance or Kruskal-Wallis test, as appropriate. Since no baseline differences were present in the four subgroups, a propensity-score matched analysis was not performed.
Kaplan–Meier estimates of the distribution of time from enrollment to date of the event (death, hospitalization, amputation) and a log-rank test for trend were used to compare the curves of the patient subgroups.
Multivariate Cox proportional hazards regression analyses were used to analyze the effect of several predictor variables on the primary outcome for each subgroup. Because of the limited number of events, multivariate hazard ratios (HRs) were calculated using a forward approach, with an entry limit of p < 0.05. A p value < 0.05 was considered statistically significant.
All statistical analyses were performed using MedCalc Statistical Software version 20.216 (MedCalc Software bvba, Ostend, Belgium).
3. Results
The clinical records of 400 patients were successfully assessed.
The final sample for the study included 113 females (51 belonging to the FCO subgroup and 62 to the FEX subgroup) and 287 males (149 MCO and 138 MEX). At baseline, the four subgroups under study did not differ in any demographic or clinical characteristics (Table 1) or in PAD severity.

Table 1.
Baseline comparison between the four study groups.
3.1. Exercise Group
All patients included in the Exercise group completed the exercise program that lasted a median of 253 (interquartile range 187–322) days, with a median of 6 (interquartile range 4–9) serial visits.
Adherence to the exercise program was high, with a mean value of 85% of the prescribed exercise sessions completed. No differences in compliance with rehabilitation were observed between males and females (85 vs. 86%, respectively; p = 0.80).
No adverse events occurred during the testing procedures, and none were reported during the home walking sessions.
3.2. Survival Probability
The median follow-up time was 6.25 years (interquartile range 4.8–7.0), and there were 143 deaths during the follow-up period, 34 in females (30%) and 109 in males (38%). Thirty-one patients died in the Exercise group, and 112 died in the Control group. Finally, according to the subgroup division, the survival rate was 90% in FEX, 82% in MEX, 45% in FCO, and 44% in MCO. The number of deaths that occurred in each subgroup is reported in Table 2.

Table 2.
Number of deaths for each group and subgroup and hazard ratios for risk of mortality comparison between the exercise vs. control group and females vs. males.
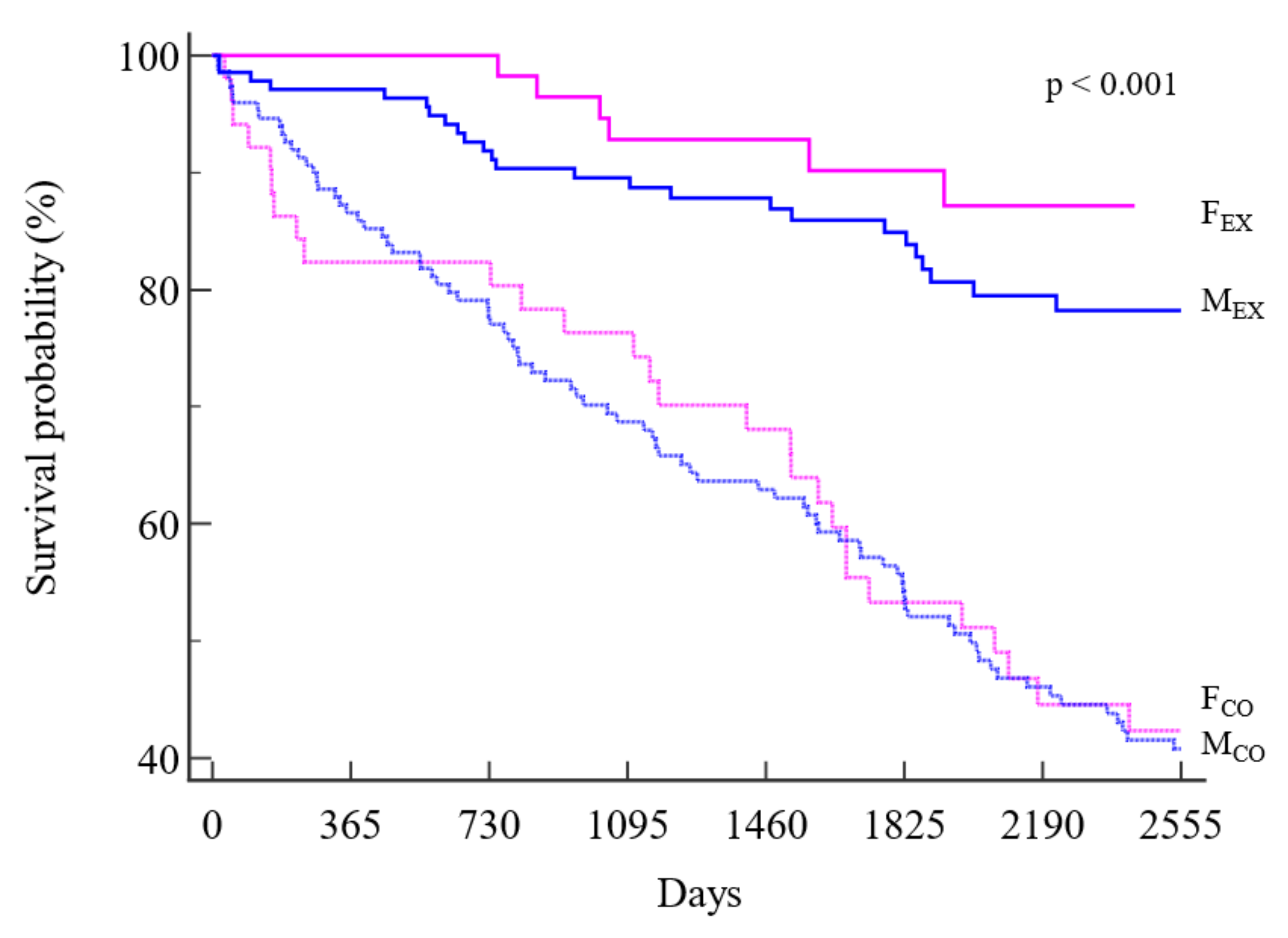
Kaplan–Meier analyses (Figure 1) showed a significantly lower mortality risk for the FEX subgroup than for all the other subgroups, including MEX. In addition, a significant difference was observed for MEX with respect to control patients of both sexes. The hazard ratios and the corresponding 95% confidence intervals are reported in Table 3.
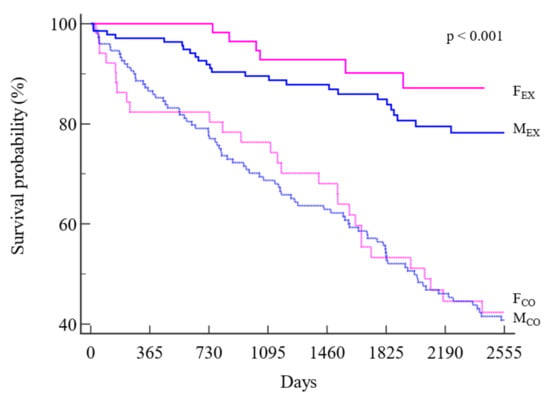
Figure 1.
Kaplan-Meier survival curves of survival in the four subgroups. Legend: dotted lines: control group; straight lines: exercise group; pink: females; blue: males.

Table 3.
Hazard ratios with 95% confidence intervals for survival probability in the four subgroups.
3.3. Predictors of Survival Probability
Age (HR: 1.09; 1.06 to 1.11), chronic kidney disease (HR: 2.04; 1.45 to 2.87), and control group (HR: 4.40; 2.93 to 6.59) were the only predictors of mortality in the entire population, according to multivariate Cox regression. No differences were observed according to sex, although an almost-significant protective factor was calculated for females (HR: 0.68; 0.46 to 1.01).
The multivariate analyses conducted in the four subgroups confirmed the results of the entire population (Table 4).

Table 4.
Multivariate hazard ratios (95% confidence interval) of the study variables for the prediction of 7-year survival probability in the four patient subgroups.
3.4. Secondary Outcomes
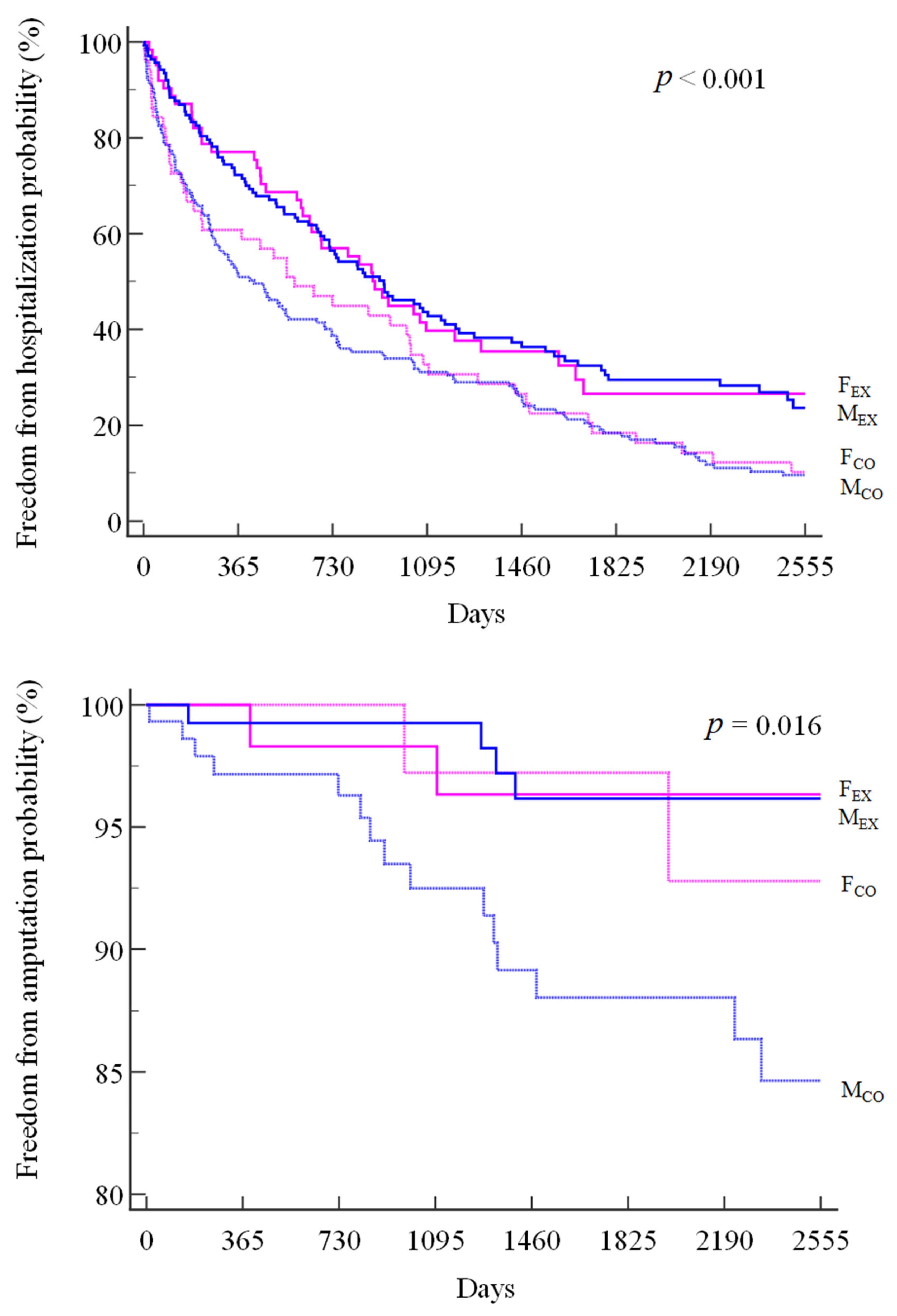
A total of 312 patients underwent hospitalization, divided into 66% in FEX, 68% in MEX, 88% in FCO, and 89% in MCO, with a significantly lower hospitalization risk (log-rank p < 0.001) for FEX (HR: 0.62; 95% CI 0.45 to 0.87) and MEX (HR: 0.62; 95% CI 0.47 to 0.80) than for MCO.
A similar pattern was observed for amputations, which occurred in 3% of patients in the FEX and MEX groups, 4% in the FCO group, and 10% in the MCO group (log-rank p = 0.016), with a significant between-group difference for FEX (HR: 0.26; 95% CI 0.08 to 0.90) and MEX (HR: 0.24; 95% CI 0.09 to 0.64) when compared to MCO. (Figure 2)
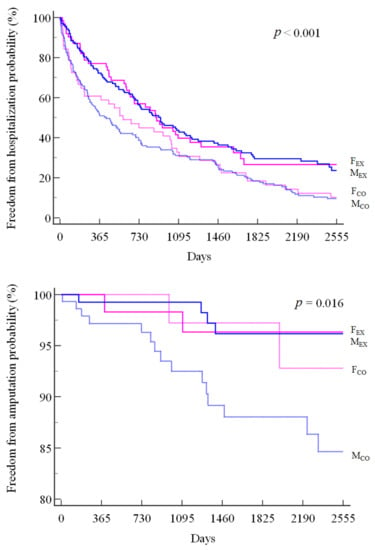
Figure 2.
Kaplan-Meier curves of all-cause hospitalizations (top panel) and amputations (bottom panel) in the four subgroups.
4. Discussion
The study showed that in a PAD population, participation, and adherence to a home rehabilitation program were associated with a lower rate of mortality at the 7-year follow-up compared to patients receiving usual care, with active women deriving greater benefit than men. In addition, better long-term rates of hospitalizations and amputations were observed following the rehabilitation program, in this case without sex differences, compared to subjects of both sexes not undergoing rehabilitation.
The study emphasizes the impact of rehabilitation on a disease such as PAD, which is responsible for restricted mobility and low functioning, particularly in women [10,13,15,16], with associated high cardiovascular risk [7,10,11]. Among PAD patients in general, a high mortality rate ranging from 15% to 40–45% is reported in studies with a follow-up at 1 to 7 years [11,13,44], with greater impact among symptomatic patients or at higher severity of peripheral disease [7,11,13]. In addition, a high rate of nonfatal cardiovascular events has been reported [45], ranging from 15% annually to 21% in 5 years [11,44].
From this perspective, at the intermediate stages of the disease, the recovery of mobility is a crucial preventive issue. Revascularization is a possible option, but with negative and even definitely nonunivocal reports of unfavorable sex- and gender-related gaps [44,46,47].
In particular, in terms of preference, a negative attitude of women to undergoing stenting or atherectomy was reported [29], as well as to undergoing surgery for abdominal aortic aneurysm and for PAD compared with males with the same disease [22].
In terms of outcomes, vascular procedures were less successful in women [48]. In particular, following endovascular treatment, women showed higher rates of death or major amputation, higher rates of major adverse lower-limb events, and procedural complications than men [24], and higher rates of occlusion and reintervention [29]. Moreover, early graft failure and higher length of stay among black females compared to white men following lower extremity bypass [49] were reported, as well as poor outcomes among young females following iliac artery stenting [50], worse postoperative outcomes after lower extremity bypass surgery, and loss of independence [19]. Finally, similar procedural success but a higher rate of vascular complications, transfusions, and embolism [51] as well as a higher risk of wound complications [52] were also noted in women.
Considering these issues, in the intermediate stages of the disease, rehabilitative exercise may exert a preminent role [35,53] considering the unfavorable cost-effectiveness of revascularization [13,54,55], the risk of a second intervention after the first revascularization, and poor outcomes [44,46,47]. However, exercise therapy also has a complementary role after revascularization [46,56].
The present study supports the importance of rehabilitation in PAD in terms of protection. If the 7-year mortality outcome observed for the usual care group was almost within the range reported in the literature [13], the outcome in the active cohort appears dramatically more favorable. The patients with PAD after performing a structured home-based protocol at 7 years showed a double rate of survival when compared to controls, with a 94% survival rate in women. This remarkable outcome among women also confirms the data among patients after myocardial infarction, with a lower 5-year risk of mortality after rehabilitation, which is particularly favorable for women [7].
If the predictive importance of exercise capacity on the long-term mortality of PAD patients is known [57], the long-term effects of participation in exercise programs on PAD are poorly reported. In a previous study in a population of more than 1000 PAD patients undergoing the rehabilitative program reported here, we observed a worse 10-year outcome for those who discontinued the program for non-health reasons [58]. Furthermore, we observed that among patients who completed the program, the most favorable clinical outcomes were observed for those persons who gained at least 0.4 km/h or 0.1 m/s of maximal speed during rehabilitation in an incremental test to exhaustion, independent of the baseline value [59]. This change in exercise capacity was related to an increase in walking speed, a protective factor according to the literature [60,61], as well to an improvement in cardiovascular fitness as calculated peak oxygen consumption, which increased by approximately 6–10% with respect to the individual baseline level. Additional preventive actions are represented by the educational activity on risk factor management developed during the on-site visits by the progressive reintroduction of a more active lifestyle at discharge from rehabilitation and in subjects with limitations [62,63], plus a rapid improvement of night-time leg symptoms with recovery of sleep quality [64].
A further positive outcome is represented by the lower number of hospitalizations for all causes observed in the exercise group compared to the controls, in this case without a difference between sexes. It is interesting to note that the difference between the active and nonactive groups is already evident at 6 months from the start of the observation. A similar early impact was observed in dialysis patients who completed the same 6-month walking program in a multicenter trial [65].
Unfortunately, it is known that the possible beneficial effects of rehabilitation may be counteracted by barriers to participation. In the different phases of cardiac rehabilitation, which include referral, enrollment, adherence, and effect, some issues may be unsatisfactory, particularly among women compared to men [7]. Interestingly, in this study, males and females equally adhered to and completed the program, suggesting that the type and characteristics of the exercise may have positively addressed some of these barriers in favor of women, such as the in-home execution for a few minutes during the day. It is known that in addition to lack of interest, which may similarly affect both sexes in adherence to cardiac rehabilitation [8], transportation problems due to distance from the center are a strong predictor of nonattendance, as well as family obligations, which may affect women’s enrollment and program completion [8,13,66]. In addition, performance fatigability and related mechanisms, which may differ between men and women, represent a barrier, particularly for women, considering their lower physical and psychological status, comorbidities, osteoarticular disorders, and lower pain tolerance [37,67,68,69,70,71,72]. This issue may be particularly relevant in PAD, where supervised and most home-based programs are performed at a medium-to-severe degree of pain [70,73,74,75]. Conversely, pain-free programs, such as the program discussed here, based on low-intensity graded exercise, may encourage participation [37,42].
Finally, in terms of effects, different training responses may be observed between sexes, as observed in cardiac rehabilitation, possibly related to physiological determinants such as metabolic or cardiovascular factors, age, comorbidities, or a lower capacity for exercise at comparable disease severity [76,77]. In a randomized study including claudication patients comparing supervised exercise therapy (SET) under a physiotherapist’s control to walking advice, women showed a lower benefit during the first 3 months of SET and a lower walking performance after 1 year of follow-up, even in the presence of similar clinical and functional data at baseline [37]. A similar lower response among women was observed in a large cohort of patients with intermittent claudication after SET [36]. Diabetic women with PAD and claudication also showed a poor response to exercise rehabilitation compared to nondiabetic women [38].
Considering home-based programs, no significantly different response to the exercise intervention according to sex was reported [74]. At discharge from the present graded program, no different functional outcomes were observed between sexes, nor a different response to training in a fitness fatigue model of performance developed in PAD [41,42].
The limitations of the study are related to its retrospective design, with partial data in the control cohort that were impossible to retrieve. For example, patients in the control group may have participated in rehabilitation programs or community-based activities in gym clubs or manifested low adherence to risk factor control. Moreover, being an observational study, a cause-effect relationship between intervention and outcomes cannot be claimed, considering all the potential factors that may affect the results.
5. Conclusions
The necessity to improve cardiovascular protection and delay physical decline in women, particularly in elderly women, makes rehabilitation programs a strategic intervention. However, if tailored strategies need to be developed to improve cardiac rehabilitation participation rates equally for both sexes, this is particularly true for PAD. The favorable clinical outcomes in PAD patients, particularly among women, associated with a personalized low-intensity home-based walking program need to be confirmed in prospective randomized studies.
Author Contributions
Conceptualization, R.M. and F.M.; methodology, N.L., L.T., C.S., E.T., N.R.; formal analysis, N.L., L.T., C.S., E.T., F.G., N.N., F.M.; data curation, N.L., C.S., E.T., F.G., N.N.; writing—original draft preparation, N.L., L.T., E.T., R.M., F.M.; writing—review and editing, C.S., N.R., S.S., F.G., N.N., V.G.; supervision, S.S., R.M., V.G.; funding acquisition, R.M. All authors have read and agreed to the published version of the manuscript.
Funding
This work has been supported, in part, by a research grant from the University of Ferrara (Fondo Ateneo Ricerca-FAR 2021, Prof. Roberto Manfredini).
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki, and approved by The Local Ethics Committee (CE-AVEC), (number 277/2019).
Informed Consent Statement
Informed consent was obtained from the majority of subjects involved in the study (those who were alive at the time of study design).
Data Availability Statement
The dataset analyzed in this article is available upon reasonable request to Dr. Nicola Lamberti (nicola.lamberti@unife.it).
Conflicts of Interest
The authors declare no conflict of interest. The funders had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript; or in the decision to publish the results.
References
- Roth, G.A.; Mensah, G.A.; Johnson, C.O.; Addolorato, G.; Ammirati, E.; Baddour, L.M.; Barengo, N.C.; Beaton, A.Z.; Benjamin, E.J.; Benziger, C.P.; et al. Global Burden of Cardiovascular Diseases and Risk Factors, 1990–2019: Update from the GBD 2019 Study. J. Am. Coll. Cardiol. 2020, 76, 2982–3021. [Google Scholar] [CrossRef]
- Mendelsohn, M.E.; Karas, R.H. Molecular and Cellular Basis of Cardiovascular Gender Differences. Science 2005, 308, 1583–1587. [Google Scholar] [CrossRef] [PubMed]
- Ndzie Noah, M.L.; Adzika, G.K.; Mprah, R.; Adekunle, A.O.; Adu-Amankwaah, J.; Sun, H. Sex-Gender Disparities in Cardiovascular Diseases: The Effects of Estrogen on ENOS, Lipid Profile, and NFATs During Catecholamine Stress. Front. Cardiovasc. Med. 2021, 8, 639946. [Google Scholar] [CrossRef] [PubMed]
- Boese, A.C.; Kim, S.C.; Yin, K.-J.; Lee, J.-P.; Hamblin, M.H. Sex Differences in Vascular Physiology and Pathophysiology: Estrogen and Androgen Signaling in Health and Disease. Am. J. Physiol. Heart Circ. Physiol. 2017, 313, H524–H545. [Google Scholar] [CrossRef]
- Kittnar, O. Selected Sex Related Differences in Pathophysiology of Cardiovascular System. Physiol. Res. 2020, 69, 21–31. [Google Scholar] [CrossRef]
- Pabon, M.; Cheng, S.; Altin, S.E.; Sethi, S.S.; Nelson, M.D.; Moreau, K.L.; Hamburg, N.; Hess, C.N. Sex Differences in Peripheral Artery Disease. Circ. Res. 2022, 130, 496–511. [Google Scholar] [CrossRef]
- Ekblom, Ö.; Cider, Å.; Hambraeus, K.; Bäck, M.; Leosdottir, M.; Lönn, A.; Börjesson, M. Participation in Exercise-Based Cardiac Rehabilitation Is Related to Reduced Total Mortality in Both Men and Women: Results from the SWEDEHEART Registry. Eur. J. Prev. Cardiol. 2022, 29, 485–492. [Google Scholar] [CrossRef] [PubMed]
- Smith, J.R.; Thomas, R.J.; Bonikowske, A.R.; Hammer, S.M.; Olson, T.P. Sex Differences in Cardiac Rehabilitation Outcomes. Circ. Res. 2022, 130, 552–565. [Google Scholar] [CrossRef]
- Arnold, A.P.; Cassis, L.A.; Eghbali, M.; Reue, K.; Sandberg, K. Sex Hormones and Sex Chromosomes Cause Sex Differences in the Development of Cardiovascular Diseases. Arterioscler. Thromb. Vasc. Biol. 2017, 37, 746–756. [Google Scholar] [CrossRef]
- Tsao, C.W.; Aday, A.W.; Almarzooq, Z.I.; Anderson, C.A.M.; Arora, P.; Avery, C.L.; Baker-Smith, C.M.; Beaton, A.Z.; Boehme, A.K.; Buxton, A.E.; et al. Heart Disease and Stroke Statistics-2023 Update: A Report From the American Heart Association. Circulation 2023, 147, e93–e621. [Google Scholar] [CrossRef]
- Sigvant, B.; Hasvold, P.; Kragsterman, B.; Falkenberg, M.; Johansson, S.; Thuresson, M.; Nordanstig, J. Cardiovascular Outcomes in Patients with Peripheral Arterial Disease as an Initial or Subsequent Manifestation of Atherosclerotic Disease: Results from a Swedish Nationwide Study. J. Vasc. Surg. 2017, 66, 507–514.e1. [Google Scholar] [CrossRef]
- Lane, R.; Harwood, A.; Watson, L.; Leng, G.C. Exercise for Intermittent Claudication. Cochrane Database Syst. Rev. 2017, 12, CD000990. [Google Scholar] [CrossRef] [PubMed]
- Sartipy, F.; Sigvant, B.; Lundin, F.; Wahlberg, E. Ten Year Mortality in Different Peripheral Arterial Disease Stages: A Population Based Observational Study on Outcome. Eur. J. Vasc. Endovasc. Surg. Off. J. Eur. Soc. Vasc. Surg. 2018, 55, 529–536. [Google Scholar] [CrossRef]
- McDermott, M.M.; Fried, L.; Simonsick, E.; Ling, S.; Guralnik, J.M. Asymptomatic Peripheral Arterial Disease Is Independently Associated with Impaired Lower Extremity Functioning: The Women’s Health and Aging Study. Circulation 2000, 101, 1007–1012. [Google Scholar] [CrossRef] [PubMed]
- Barochiner, J.; Aparicio, L.S.; Waisman, G.D. Challenges Associated with Peripheral Arterial Disease in Women. Vasc. Health Risk Manag. 2014, 10, 115–128. [Google Scholar] [CrossRef] [PubMed]
- Porras, C.P.; Bots, M.L.; Teraa, M.; van Doorn, S.; Vernooij, R.W.M. Differences in Symptom Presentation in Women and Men with Confirmed Lower Limb Peripheral Artery Disease: A Systematic Review and Meta-Analysis. Eur. J. Vasc. Endovasc. Surg. Off. J. Eur. Soc. Vasc. Surg. 2022, 63, 602–612. [Google Scholar] [CrossRef]
- Gardner, A.W. Sex Differences in Claudication Pain in Subjects with Peripheral Arterial Disease. Med. Sci. Sports Exerc. 2002, 34, 1695–1698. [Google Scholar] [CrossRef]
- McDermott, M.M.; Greenland, P.; Liu, K.; Criqui, M.H.; Guralnik, J.M.; Celic, L.; Chan, C. Sex Differences in Peripheral Arterial Disease: Leg Symptoms and Physical Functioning. J. Am. Geriatr. Soc. 2003, 51, 222–228. [Google Scholar] [CrossRef]
- Ilonzo, N.; Lee, J.; James, C.; Phair, J.; Ting, W.; Faries, P.; Vouyouka, A. Sex-Based Differences in Loss of Independence after Lower Extremity Bypass Surgery. Am. J. Surg. 2022, 223, 170–175. [Google Scholar] [CrossRef]
- Lee, M.H.-Y.; Li, P.Y.; Li, B.; Shakespeare, A.; Samarasinghe, Y.; Feridooni, T.; Cuen-Ojeda, C.; Alshabanah, L.; Kishibe, T.; Al-Omran, M. A Systematic Review and Meta-Analysis of Sex- and Gender-Based Differences in Presentation Severity and Outcomes in Adults Undergoing Major Vascular Surgery. J. Vasc. Surg. 2022, 76, 581–594.e25. [Google Scholar] [CrossRef]
- Lo, R.C.; Bensley, R.P.; Dahlberg, S.E.; Matyal, R.; Hamdan, A.D.; Wyers, M.; Chaikof, E.L.; Schermerhorn, M.L. Presentation, Treatment, and Outcome Differences between Men and Women Undergoing Revascularization or Amputation for Lower Extremity Peripheral Arterial Disease. J. Vasc. Surg. 2014, 59, 409–418.e3. [Google Scholar] [CrossRef] [PubMed]
- McGinigle, K.L.; Browder, S.E.; Strassle, P.D.; Shalhub, S.; Harris, L.M.; Minc, S.D. Sex-Related Disparities in Intervention Rates and Type of Intervention in Patients with Aortic and Peripheral Arterial Diseases in the National Inpatient Sample Database. J. Vasc. Surg. 2021, 73, 2081–2089.e7. [Google Scholar] [CrossRef] [PubMed]
- Hess, C.N.; Baumgartner, I.; Anand, S.S.; Nehler, M.R.; Patel, M.R.; Debus, E.S.; Szarek, M.; Capell, W.; Muehlhofer, E.; Berkowitz, S.D.; et al. Sex-Based Differences in Outcomes Following Peripheral Artery Revascularization: Insights From VOYAGER PAD. J. Am. Heart Assoc. 2022, 11, e024655. [Google Scholar] [CrossRef] [PubMed]
- Choi, K.H.; Park, T.K.; Kim, J.; Ko, Y.-G.; Yu, C.W.; Yoon, C.-H.; Lee, J.-H.; Min, P.-K.; Koh, Y.S.; Chae, I.-H.; et al. Sex Differences in Outcomes Following Endovascular Treatment for Symptomatic Peripheral Artery Disease: An Analysis From the K- VIS ELLA Registry. J. Am. Heart Assoc. 2019, 8, e010849. [Google Scholar] [CrossRef]
- McDermott, M.M.; Ferrucci, L.; Liu, K.; Guralnik, J.M.; Tian, L.; Kibbe, M.; Liao, Y.; Tao, H.; Criqui, M.H. Women with Peripheral Arterial Disease Experience Faster Functional Decline than Men with Peripheral Arterial Disease. J. Am. Coll. Cardiol. 2011, 57, 707–714. [Google Scholar] [CrossRef]
- Makowski, L.; Feld, J.; Köppe, J.; Illner, J.; Kühnemund, L.; Wiederhold, A.; Dröge, P.; Günster, C.; Gerß, J.; Reinecke, H.; et al. Sex Related Differences in Therapy and Outcome of Patients with Intermittent Claudication in a Real-World Cohort. Atherosclerosis 2021, 325, 75–82. [Google Scholar] [CrossRef]
- Kotov, A.; Heidemann, F.; Kuchenbecker, J.; Peters, F.; Marschall, U.; Acar, L.; Debus, E.S.; L’Hoest, H.; Behrendt, C.-A. Sex Disparities in Long Term Outcomes After Open Surgery for Chronic Limb Threatening Ischemia: A Propensity Score Matched Analysis of Health Insurance Claims. Eur. J. Vasc. Endovasc. Surg. Off. J. Eur. Soc. Vasc. Surg. 2021, 61, 423–429. [Google Scholar] [CrossRef]
- Heidemann, F.; Kuchenbecker, J.; Peters, F.; Kotov, A.; Marschall, U.; L’Hoest, H.; Acar, L.; Ramkumar, N.; Goodney, P.; Debus, E.S.; et al. A Health Insurance Claims Analysis on the Effect of Female Sex on Long-Term Outcomes after Peripheral Endovascular Interventions for Symptomatic Peripheral Arterial Occlusive Disease. J. Vasc. Surg. 2021, 74, 780–787.e7. [Google Scholar] [CrossRef]
- Ramkumar, N.; Suckow, B.D.; Brown, J.R.; Sedrakyan, A.; MacKenzie, T.; Stone, D.H.; Cronenwett, J.L.; Goodney, P.P. Role of Sex in Determining Treatment Type for Patients Undergoing Endovascular Lower Extremity Revascularization. J. Am. Heart Assoc. 2019, 8, e013088. [Google Scholar] [CrossRef]
- Mahtta, D.; Ahmed, S.T.; Ramsey, D.J.; Akeroyd, J.M.; Lee, M.T.; Rodriguez, F.; Michos, E.D.; Itchhaporia, D.; Nasir, K.; Alam, M.; et al. Statin Prescription Rates, Adherence, and Associated Clinical Outcomes Among Women with PAD and ICVD. Cardiovasc. Drugs Ther. 2020, 34, 745–754. [Google Scholar] [CrossRef]
- Nanna, M.G.; Wang, T.Y.; Xiang, Q.; Goldberg, A.C.; Robinson, J.G.; Roger, V.L.; Virani, S.S.; Wilson, P.W.F.; Louie, M.J.; Koren, A.; et al. Sex Differences in the Use of Statins in Community Practice. Circ. Cardiovasc. Qual. Outcomes 2019, 12, e005562. [Google Scholar] [CrossRef]
- Rodriguez, F.; Olufade, T.O.; Ramey, D.R.; Friedman, H.S.; Navaratnam, P.; Heithoff, K.; Foody, J.M. Gender Disparities in Lipid-Lowering Therapy in Cardiovascular Disease: Insights from a Managed Care Population. J. Womens Health (Larchmt.) 2016, 25, 697–706. [Google Scholar] [CrossRef]
- Messiha, D.; Petrikhovich, O.; Lortz, J.; Mahabadi, A.A.; Hering, R.; Schulz, M.; Rassaf, T.; Rammos, C. Gender Differences in Outpatient Peripheral Artery Disease Management in Germany: A Population Based Study 2009-2018. Eur. J. Vasc. Endovasc. Surg. Off. J. Eur. Soc. Vasc. Surg. 2022, 63, 714–720. [Google Scholar] [CrossRef]
- Aboyans, V.; Ricco, J.-B.; Bartelink, M.-L.E.L.; Björck, M.; Brodmann, M.; Cohnert, T.; Collet, J.-P.; Czerny, M.; De Carlo, M.; Debus, S.; et al. 2017 ESC Guidelines on the Diagnosis and Treatment of Peripheral Arterial Diseases, in Collaboration with the European Society for Vascular Surgery (ESVS): Document Covering Atherosclerotic Disease of Extracranial Carotid and Vertebral, Mesenteric, Renal. Eur. Heart J. 2018, 39, 763–816. [Google Scholar] [CrossRef]
- Gerhard-Herman, M.D.; Gornik, H.L.; Barrett, C.; Barshes, N.R.; Corriere, M.A.; Drachman, D.E.; Fleisher, L.A.; Fowkes, F.G.R.; Hamburg, N.M.; Kinlay, S.; et al. 2016 AHA/ACC Guideline on the Management of Patients With Lower Extremity Peripheral Artery Disease: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J. Am. Coll. Cardiol. 2017, 69, e71–e126. [Google Scholar] [CrossRef]
- Dörenkamp, S.; Mesters, I.; de Bie, R.; Teijink, J.; van Breukelen, G. Patient Characteristics and Comorbidities Influence Walking Distances in Symptomatic Peripheral Arterial Disease: A Large One-Year Physiotherapy Cohort Study. PLoS ONE 2016, 11, e0146828. [Google Scholar] [CrossRef]
- Gommans, L.N.M.; Scheltinga, M.R.M.; van Sambeek, M.R.H.M.; Maas, A.H.E.M.; Bendermacher, B.L.W.; Teijink, J.A.W. Gender Differences Following Supervised Exercise Therapy in Patients with Intermittent Claudication. J. Vasc. Surg. 2015, 62, 681–688. [Google Scholar] [CrossRef] [PubMed]
- Gardner, A.W.; Parker, D.E.; Montgomery, P.S.; Blevins, S.M. Diabetic Women Are Poor Responders to Exercise Rehabilitation in the Treatment of Claudication. J. Vasc. Surg. 2014, 59, 1036–1043. [Google Scholar] [CrossRef] [PubMed]
- Manfredini, F.; Malagoni, A.M.; Mascoli, F.; Mandini, S.; Taddia, M.C.; Basaglia, N.; Manfredini, R.; Conconi, F.; Zamboni, P. Training Rather than Walking-The Test in-Train out Program for Home-Based Rehabilitation in Peripheral Arteriopathy. Circ. J. 2008, 72, 946–952. [Google Scholar] [CrossRef]
- Malagoni, A.M.; Vagnoni, E.; Felisatti, M.; Mandini, S.; Heidari, M.; Mascoli, F.; Basaglia, N.; Manfredini, R.; Zamboni, P.; Manfredini, F. Evaluation of Patient Compliance, Quality of Life Impact and Cost-Effectiveness of a “Test in-Train out” Exercise-Based Rehabilitation Program for Patients with Intermittent Claudication. Circ. J. 2011, 75, 2128–2134. [Google Scholar] [CrossRef] [PubMed]
- Lamberti, N.; Piva, G.; Businaro, F.; Caruso, L.; Crepaldi, A.; Lòpez-Soto, P.J.; Manfredini, F. A Fitness-Fatigue Model of Performance in Peripheral Artery Disease: Predicted and Measured Effects of a Pain-Free Exercise Program. J. Pers. Med. 2022, 12, 397. [Google Scholar] [CrossRef] [PubMed]
- Manfredini, R.; Lamberti, N.; Manfredini, F.; Straudi, S.; Fabbian, F.; Rodriguez Borrego, M.A.; Basaglia, N.; Carmona Torres, J.M.; Lopez Soto, P.J. Gender Differences in Outcomes Following a Pain-Free, Home-Based Exercise Program for Claudication. J. Women’s Health. 2019, 28, 1313–1321. [Google Scholar] [CrossRef] [PubMed]
- Vandenbroucke, J.P.; von Elm, E.; Altman, D.G.; Gøtzsche, P.C.; Mulrow, C.D.; Pocock, S.J.; Poole, C.; Schlesselman, J.J.; Egger, M. Strengthening the Reporting of Observational Studies in Epidemiology (STROBE): Explanation and Elaboration. PLoS Med. 2007, 4, e297. [Google Scholar] [CrossRef]
- Rantner, B.; Kollerits, B.; Pohlhammer, J.; Stadler, M.; Lamina, C.; Peric, S.; Klein-Weigel, P.; Mühlthaler, H.; Fraedrich, G.; Kronenberg, F. The Fate of Patients with Intermittent Claudication in the 21st Century Revisited-Results from the CAVASIC Study. Sci. Rep. 2017, 8, 45833. [Google Scholar] [CrossRef] [PubMed]
- Norgren, L.; Hiatt, W.R.; Dormandy, J.A.; Nehler, M.R.; Harris, K.A.; Fowkes, F.G.R. Inter-Society Consensus for the Management of Peripheral Arterial Disease (TASC II). J. Vasc. Surg. 2007, 45 (Suppl. 1), S5–S67. [Google Scholar] [CrossRef]
- Hogan, S.E.; Nehler, M.R.; Anand, S.; Patel, M.R.; Debus, S.; Jackson, M.T.; Buchanan, C.; King, R.W.; Hess, C.; Muehlhofer, E.; et al. Improvement in Walking Impairment Following Surgical and Endovascular Revascularization: Insights from VOYAGER PAD. Vasc. Med. 2022, 27, 343–349. [Google Scholar] [CrossRef]
- Secemsky, E.A.; Shen, C.; Schermerhorn, M.; Yeh, R.W. Longitudinal Assessment of Safety of Femoropopliteal Endovascular Treatment With Paclitaxel-Coated Devices Among Medicare Beneficiaries: The SAFE-PAD Study. JAMA Intern. Med. 2021, 181, 1071–1080. [Google Scholar] [CrossRef]
- Vouyouka, A.G.; Egorova, N.N.; Salloum, A.; Kleinman, L.; Marin, M.; Faries, P.L.; Moscowitz, A. Lessons Learned from the Analysis of Gender Effect on Risk Factors and Procedural Outcomes of Lower Extremity Arterial Disease. J. Vasc. Surg. 2010, 52, 1196–1202. [Google Scholar] [CrossRef]
- Jain, A.K.; Kalbaugh, C.A.; Farber, M.A.; Marston, W.A.; Vallabhaneni, R. Race and Gender Affect Outcomes of Lower Extremity Bypass. J. Vasc. Surg. 2014, 60, 1275–1281. [Google Scholar] [CrossRef]
- Bechter-Hugl, B.; Falkensammer, J.; Gorny, O.; Greiner, A.; Chemelli, A.; Fraedrich, G. The Influence of Gender on Patency Rates after Iliac Artery Stenting. J. Vasc. Surg. 2014, 59, 1588–1596. [Google Scholar] [CrossRef]
- Jackson, E.A.; Munir, K.; Schreiber, T.; Rubin, J.R.; Cuff, R.; Gallagher, K.A.; Henke, P.K.; Gurm, H.S.; Grossman, P.M. Impact of Sex on Morbidity and Mortality Rates after Lower Extremity Interventions for Peripheral Arterial Disease: Observations from the Blue Cross Blue Shield of Michigan Cardiovascular Consortium. J. Am. Coll. Cardiol. 2014, 63, 2525–2530. [Google Scholar] [CrossRef]
- Arnaoutakis, D.J.; Scully, R.E.; Sharma, G.; Shah, S.K.; Ozaki, C.K.; Belkin, M.; Nguyen, L.L. Impact of Body Mass Index and Gender on Wound Complications after Lower Extremity Arterial Surgery. J. Vasc. Surg. 2017, 65, 1713–1718.e1. [Google Scholar] [CrossRef]
- Redberg, R.F.; McDermott, M.M. High Mortality Rates in Medicare Patients After Peripheral Artery Disease Revascularization. JAMA Intern. Med. 2021, 181, 1041–1042. [Google Scholar] [CrossRef]
- Spronk, S.; Bosch, J.L.; den Hoed, P.T.; Veen, H.F.; Pattynama, P.M.T.; Hunink, M.G.M. Cost-Effectiveness of Endovascular Revascularization Compared to Supervised Hospital-Based Exercise Training in Patients with Intermittent Claudication: A Randomized Controlled Trial. J. Vasc. Surg. 2008, 48, 1472–1480. [Google Scholar] [CrossRef]
- Djerf, H.; Millinger, J.; Falkenberg, M.; Jivegård, L.; Svensson, M.; Nordanstig, J. Absence of Long-Term Benefit of Revascularization in Patients With Intermittent Claudication: Five-Year Results From the IRONIC Randomized Controlled Trial. Circ. Cardiovasc. Interv. 2020, 13, e008450. [Google Scholar] [CrossRef]
- Hageman, D.; Fokkenrood, H.J.; Gommans, L.N.; van den Houten, M.M.; Teijink, J.A. Supervised Exercise Therapy versus Home-Based Exercise Therapy versus Walking Advice for Intermittent Claudication. Cochrane Database Syst. Rev. 2018, 4, CD005263. [Google Scholar] [CrossRef]
- Leeper, N.J.; Myers, J.; Zhou, M.; Nead, K.T.; Syed, A.; Kojima, Y.; Caceres, R.D.; Cooke, J.P. Exercise Capacity Is the Strongest Predictor of Mortality in Patients with Peripheral Arterial Disease. J. Vasc. Surg. 2013, 57, 728–733. [Google Scholar] [CrossRef]
- Lamberti, N.; López-Soto, P.J.; Guerzoni, F.; Napoli, N.; Gasbarro, V.; Zamboni, P.; Tsolaki, E.; Taddia, M.C.; Rodríguez-Borrego, M.A.; Manfredini, R.; et al. Changes in Exercise Capacity and Risk of All-Cause Mortality in Patients with Peripheral Artery Disease: A 10-Year Retrospective Cohort Study. Intern. Emerg. Med. 2020, 15, 289–298. [Google Scholar] [CrossRef] [PubMed]
- Manfredini, F.; Lamberti, N.; Guerzoni, F.; Napoli, N.; Gasbarro, V.; Zamboni, P.; Mascoli, F.; Manfredini, R.; Basaglia, N.; Rodríguez-Borrego, M.A.; et al. Rehabilitative Exercise Reduced the Impact of Peripheral Artery Disease on Vascular Outcomes in Elderly Patients with Claudication: A Three-Year Single Center Retrospective Study. J. Clin. Med. 2019, 8, 210. [Google Scholar] [CrossRef] [PubMed]
- Hardy, S.E.; Perera, S.; Roumani, Y.F.; Chandler, J.M.; Studenski, S.A. Improvement in Usual Gait Speed Predicts Better Survival in Older Adults. J. Am. Geriatr. Soc. 2007, 55, 1727–1734. [Google Scholar] [CrossRef] [PubMed]
- Studenski, S.; Perera, S.; Patel, K.; Rosano, C.; Faulkner, K.; Inzitari, M.; Brach, J.; Chandler, J.; Cawthon, P.; Connor, E.B.; et al. Gait Speed and Survival in Older Adults. JAMA 2011, 305, 50–58. [Google Scholar] [CrossRef] [PubMed]
- Lamberti, N.; Straudi, S.; Lissia, E.; Cavazzini, L.; Buja, S.; Manfredini, R.; Basaglia, N.; Manfredini, F. Home-Based Exercise for Elderly Patients with Intermittent Claudication Limited by Osteoarticular Disorders-Feasibility and Eff Ectiveness of a Low-Intensity Programme. Vasa-Eur. J. Vasc. Med. 2018, 47, 227–234. [Google Scholar] [CrossRef]
- Garg, P.K.; Tian, L.; Criqui, M.H.; Liu, K.; Ferrucci, L.; Guralnik, J.M.; Tan, J.; McDermott, M.M. Physical Activity during Daily Life and Mortality in Patients with Peripheral Arterial Disease. Circulation 2006, 114, 242–248. [Google Scholar] [CrossRef]
- Lamberti, N.; López-Soto, P.J.; Rodríguez-Borrego, M.A.; Straudi, S.; Basaglia, N.; Zamboni, P.; Manfredini, R.; Manfredini, F. Restless Leg Syndrome in Peripheral Artery Disease: Prevalence among Patients with Claudication and Benefits from Low-Intensity Exercise. J. Clin. Med. 2019, 8, 1403. [Google Scholar] [CrossRef]
- Manfredini, F.; Mallamaci, F.; D’Arrigo, G.; Baggetta, R.; Bolignano, D.; Torino, C.; Lamberti, N.; Bertoli, S.; Ciurlino, D.; Rocca-Rey, L.; et al. Exercise in Patients on Dialysis: A Multicenter, Randomized Clinical Trial. J. Am. Soc. Nephrol. 2017, 28, 1259–1268. [Google Scholar] [CrossRef]
- Borg, S.; Öberg, B.; Leosdottir, M.; Lindolm, D.; Nilsson, L.; Bäck, M. Factors Associated with Non-Attendance at Exercise-Based Cardiac Rehabilitation. BMC Sport. Sci. Med. Rehabil. 2019, 11, 13. [Google Scholar] [CrossRef]
- Fillingim, R.B.; Maixner, W. Gender Differences in the Responses to Noxious Stimuli. Pain Forum 1995, 4, 209–221. [Google Scholar] [CrossRef]
- Cavalcante, B.R.; Farah, B.Q.; Barbosa, J.P.d.A.; Cucato, G.G.; da Rocha Chehuen, M.; da Silva Santana, F.; Wolosker, N.; de Moraes Forjaz, C.L.; Ritti-Dias, R.M. Are the Barriers for Physical Activity Practice Equal for All Peripheral Artery Disease Patients? Arch. Phys. Med. Rehabil. 2015, 96, 248–252. [Google Scholar] [CrossRef] [PubMed]
- Oka, R.K.; Szuba, A.; Giacomini, J.C.; Cooke, J.P. Gender Differences in Perception of PAD: A Pilot Study. Vasc. Med. 2003, 8, 89–94. [Google Scholar] [CrossRef]
- Treat-Jacobson, D.; McDermott, M.M.; Bronas, U.G.; Campia, U.; Collins, T.C.; Criqui, M.H.; Gardner, A.W.; Hiatt, W.R.; Regensteiner, J.G.; Rich, K. Optimal Exercise Programs for Patients with Peripheral Artery Disease: A Scientific Statement from the American Heart Association. Circulation 2019, 139, E10–E33. [Google Scholar] [CrossRef]
- Collins, T.C.; Suarez-Almazor, M.; Bush, R.L.; Petersen, N.J. Gender and Peripheral Arterial Disease. J. Am. Board Fam. Med. 2006, 19, 132–140. [Google Scholar] [CrossRef][Green Version]
- Grace, S.L.; Gravely Witte, S.; Kayaniyil, S.; Brual, J.; Suskin, N.; Stewart, D.E. A Multisite Examination of Sex Differences in Cardiac Rehabilitation Barriers by Participation Status. J. Womens Health (Larchmt.) 2009, 18, 209–216. [Google Scholar] [CrossRef] [PubMed]
- McDermott, M.M.; Spring, B.; Tian, L.; Treat-Jacobson, D.; Ferrucci, L.; Lloyd-Jones, D.; Zhao, L.; Polonsky, T.; Kibbe, M.R.; Bazzano, L.; et al. Effect of Low-Intensity vs High-Intensity Home-Based Walking Exercise on Walk Distance in Patients with Peripheral Artery Disease: The LITE Randomized Clinical Trial. JAMA-J. Am. Med. Assoc. 2021, 325, 1266–1276. [Google Scholar] [CrossRef] [PubMed]
- McDermott, M.M.; Spring, B.; Berger, J.S.; Treat-Jacobson, D.; Conte, M.S.; Creager, M.A.; Criqui, M.H.; Ferrucci, L.; Gornik, H.L.; Guralnik, J.M.; et al. Effect of a Home-Based Exercise Intervention of Wearable Technology and Telephone Coaching on Walking Performance in Peripheral Artery Disease: The Honor Randomized Clinical Trial. JAMA-J. Am. Med. Assoc. 2018, 319, 1665–1676. [Google Scholar] [CrossRef]
- Bearne, L.M.; Volkmer, B.; Peacock, J.; Sekhon, M.; Fisher, G.; Galea Holmes, M.N.; Douiri, A.; Amirova, A.; Farran, D.; Quirke-McFarlane, S.; et al. Effect of a Home-Based, Walking Exercise Behavior Change Intervention vs Usual Care on Walking in Adults With Peripheral Artery Disease The MOSAIC Randomized Clinical Trial. JAMA-J. Am. Med. Assoc. 2022, 327, 1344–1355. [Google Scholar] [CrossRef] [PubMed]
- Witvrouwen, I.; Van Craenenbroeck, E.M.; Abreu, A.; Moholdt, T.; Kränkel, N. Exercise Training in Women with Cardiovascular Disease: Differential Response and Barriers-Review and Perspective. Eur. J. Prev. Cardiol. 2019, 28, 779–790. [Google Scholar] [CrossRef]
- Lozano, F.S.; González-Porras, J.R.; March, J.R.; Carrasco, E.; Lobos, J.M. Differences between Women and Men with Intermittent Claudication: A Cross-Sectional Study. J. Womens Health (Larchmt.) 2014, 23, 834–841. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).