Guided Genioplasty: Comparison between Conventional Technique and Customized Guided Surgery
Abstract
1. Introduction
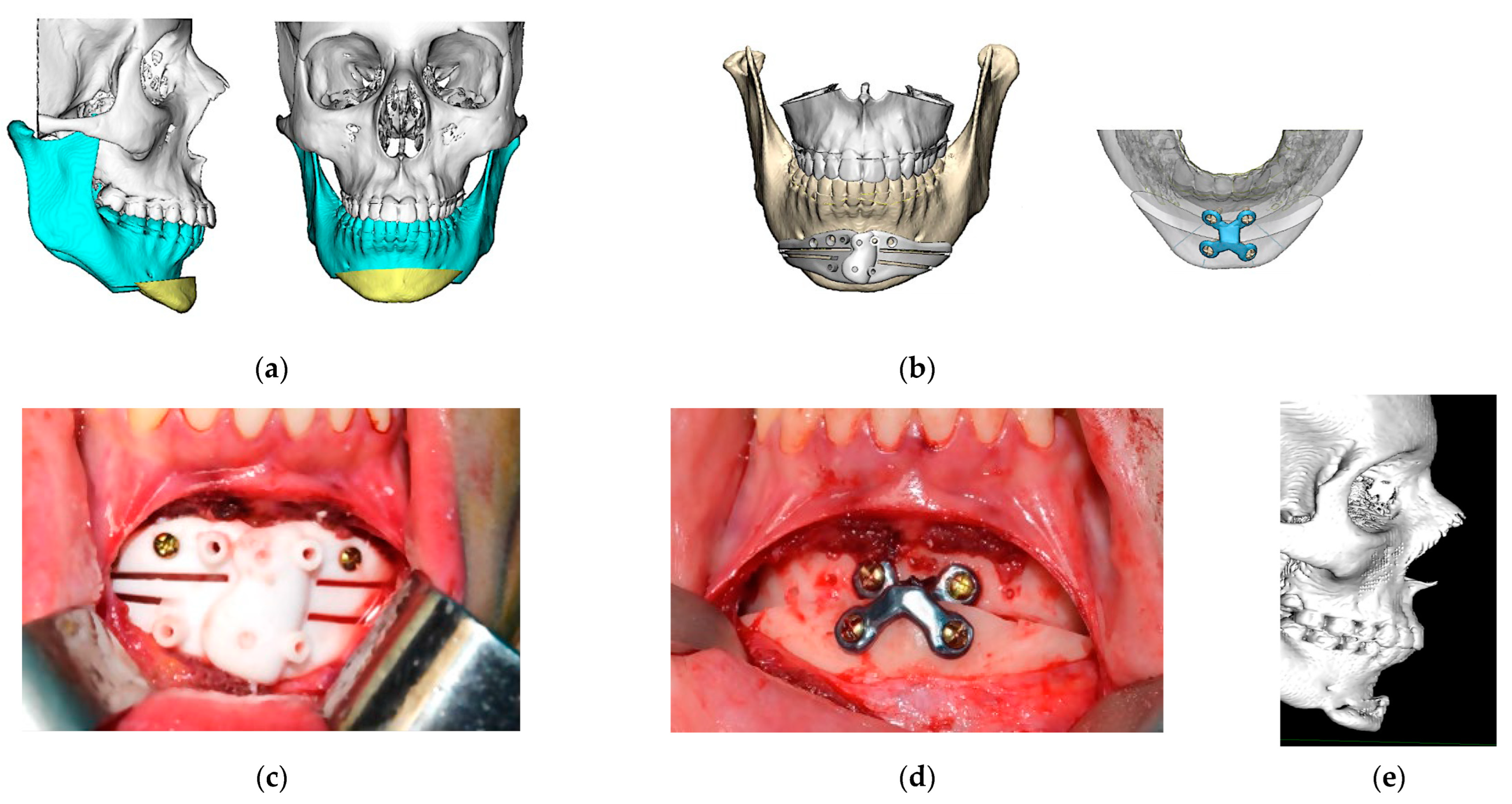
2. Materials and Methods
- (1)
- Difference between planned and achieved motion with both techniques (measured in millimeters, and in degrees for chin rotation cases). The Phillips IntelliSpace Portal© V.11.1(Koninklijke Philips N.V. Amsterdam, The Nederlands). radiological viewer was used for this purpose.
- (2)
- Intervention time and length of hospital stay between the two techniques.
- (3)
- Aesthetic outcome: an aesthetic assessment was performed by the patients to address scores in facial symmetry, facial healing, and facial projection. The results were classified as “excellent”, “good”, and “poor”.
3. Results
3.1. Differences between Planned and Achieved Surgical Motion
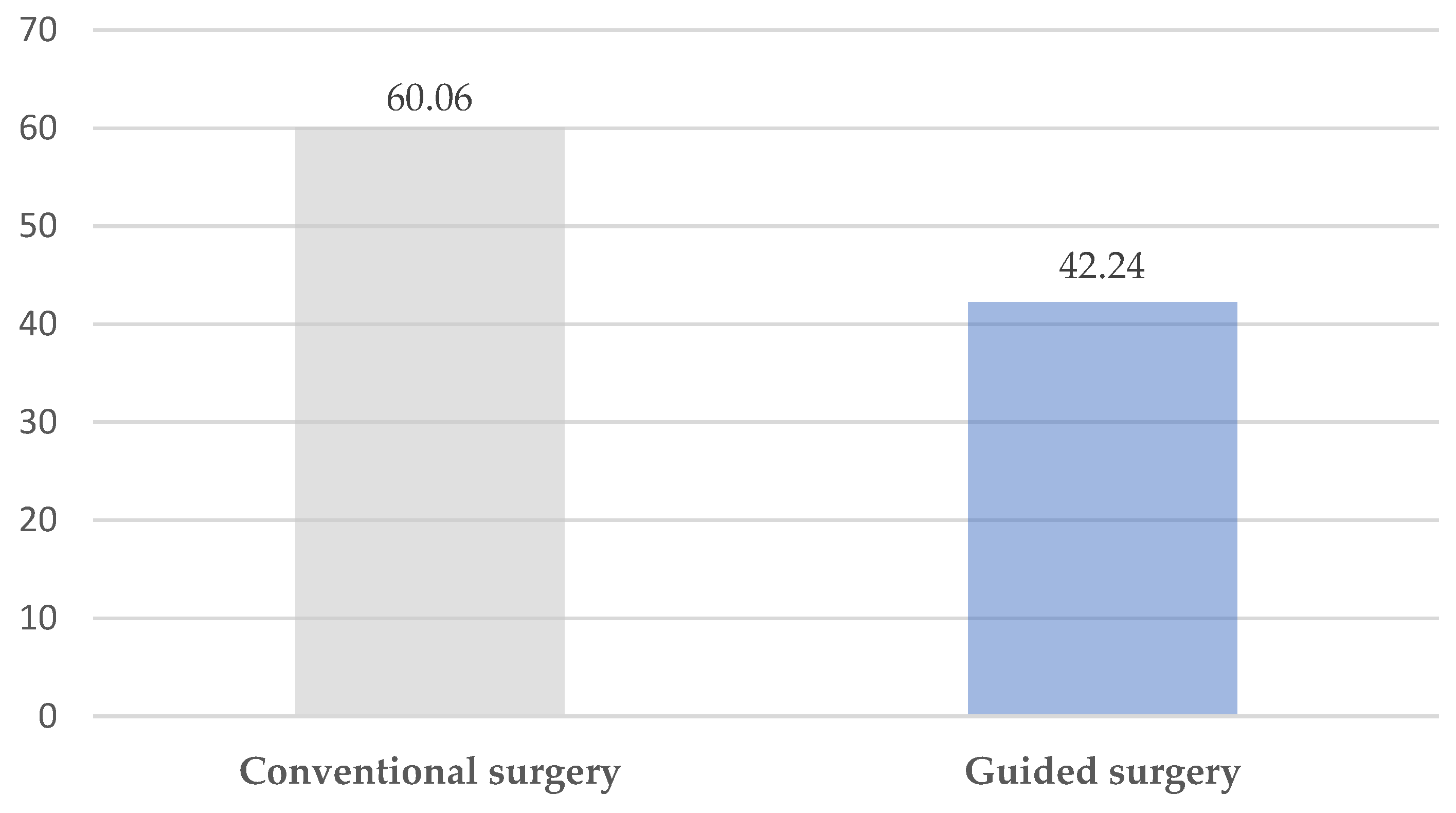
3.2. Surgical Time and Hospitalization
3.3. Aesthetic Outcome: Patient Perception
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Ferretti, C.; Reyneke, J.P. Genioplasty. Atlas Oral Maxillofac. Surg. Clin. N. Am. 2016, 24, 79–85. [Google Scholar] [CrossRef] [PubMed]
- Hofer, O. Operation der Prognathie und Mikrogenie. Dtsch Zahn Mund Kieferheilkd 1942, 9, 121–132. [Google Scholar]
- Gillies, H.; Millard, D.R. The Principles and Art of Plastic Surgery; Butterworth: Oxford, UK, 1957. [Google Scholar]
- Trauner, R.; Obwegeser, H. The surgical correction of mandibular prognathism and retrognathia with consideration of genioplasty. I. Surgical procedures to correct mandibular prognathism and reshaping of the chin. Oral Surg. Oral Med. Oral Pathol. 1957, 10, 677–689. [Google Scholar] [CrossRef] [PubMed]
- San Miguel Moragas, J.; Oth, O.; Büttner, M.; Mommaerts, M.Y. A systematic review on soft-to-hard tissue ratios in orthognathic surgery part II: Chin procedures. J. Cranio-Maxillofac. Surg. 2015, 43, 1530–1540. [Google Scholar] [CrossRef] [PubMed]
- Antúnez-Conde, R.; Navarro Cuéllar, C.; Salmerón Escobar, J.I.; Díez-Montiel, A.; Navarro Cuéllar, I.; Dell’Aversana Orabona, G.; Del Castillo Pardo de Vera, J.L.; Navarro Vila, C.; Cebrián Carretero, J.L. Intraosseous Venous Malformation of the Zygomatic Bone: Comparison between Virtual Surgical Planning and Standard Surgery with Review of the Literature. J. Clin. Med. 2021, 10, 4565. [Google Scholar] [CrossRef] [PubMed]
- Li, B.; Shen, S.G.; Yu, H.; Li, J.; Xia, J.J.; Wang, X. A new design of CAD/CAM surgical template system for two-piece narrowing genioplasty. Int. J. Oral Maxillofac. Surg. 2016, 45, 560. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Scolozzi, P. Computer-aided design and computer-aided modeling (CAD/CAM) generated surgical splints, cutting guides and custom-made implants: Which indications in orthognathic surgery? Rev. Stomatol. Chir. Maxillo-Faciale Chir. Orale 2015, 116, 343. [Google Scholar] [CrossRef] [PubMed]
- Shen, P.; Zhao, J.; Fan, L.; Qiu, H.; Xu, W.; Wang, Y.; Zhang, S.; Kim, Y.J. Accuracy evaluation of computer-designed surgical guide template in oral implantology. J. Cranio-Maxillofac. Surg. 2015, 43, 2189–2194. [Google Scholar] [CrossRef] [PubMed]
- Antúnez-Conde, R.; Salmerón, J.I.; Díez-Montiel, A.; Agea, M.; Gascón, D.; Sada, Á.; Navarro Cuéllar, I.; Tousidonis, M.; Ochandiano, S.; Arenas, G.; et al. Mandibular Reconstruction with Fibula Flap and Dental Implants through Virtual Surgical Planning and Three Different Techniques: Double-Barrel Flap, Implant Dynamic Navigation and CAD/CAM Mesh with Iliac Crest Graft. Front. Oncol. 2021, 11, 719712. [Google Scholar] [CrossRef]
- Flügge, T.V.; Nelson, K.; Schmelzeisen, R.; Metzger, M.C. Three-dimensional plot- ting and printing of an implant drilling guide: Simplifying guided implant surgery. J. Oral Maxillofac. Surg. 2013, 71, 1340–1346. [Google Scholar] [CrossRef]
- Kang, S.H.; Lee, J.W.; Lim, S.H.; Kim, Y.H.; Kim, M.K. Validation of mandibular genioplasty using a stereolithographic surgical guide: In vitro comparison with a manual measurement method based on preoperative surgical simulation. J. Oral Maxillofac. Surg. 2014, 72, 2032–2042. [Google Scholar] [CrossRef] [PubMed]
- Olszewski, R.; Tranduy, K.; Reychler, H. Innovative procedure for computer-assisted genioplasty: Three-dimensional cephalometry, rapid-prototyping model and surgical splint. Int. J. Oral Maxillofac. Surg. 2010, 39, 721–724. [Google Scholar] [CrossRef]
- Arcas, A.; Vendrell, G.; Cuesta, F.; Bermejo, L. Mentoplasty with Customized Guides and Plates Using 3D Technology: A More Precise and Safer Technique. Plast. Reconstr. Surg. Glob. Open 2019, 7, e2349. [Google Scholar] [CrossRef] [PubMed]
- Abadi, M.; Pour, O.B. Genioplasty. Facial Plast. Surg. 2015, 31, 513–522. [Google Scholar] [PubMed]
- Keyhan, S.O.; Jahangirnia, A.; Fallahi, H.R.; Navabazam, A.; Ghanean, S. Three-dimensional printer-assisted reduction genioplasty; surgical guide fabrication. Ann. Maxillofac. Surg. 2016, 6, 278–280. [Google Scholar] [PubMed]
- Berridge, N.; Heliotis, M. New technique to improve lower facial contour using a three-dimensional, custom-made, positional stent. Br. J. Oral Maxillofac. Surg. 2016, 54, 1044–1104. [Google Scholar] [CrossRef] [PubMed]
- Yamauchi, K.; Yamaguchi, Y.; Katoh, H.; Takahashi, T. Tooth-bone CAD/CAM surgical guide for genioplasty. Br. J. Oral Maxillofac. Surg. 2016, 54, 1134–1135. [Google Scholar] [CrossRef]
- Aston, S.J.; Smith, D.M. Taking it on the chin: Recognizing and accounting for lower face asymmetry in chin augmentation and genioplasty. Plast. Reconstr. Surg. 2015, 135, 1591–1595. [Google Scholar] [CrossRef]
- Liebregts, J.; Baan, F.; van Lierop, P.; de Koning, M.; Bergé, S.; Maal, T.; Xi, T. One-year postoperative skeletal stability of 3D planned bimaxillary osteotomies: Maxilla-first versus mandible-first surgery. Sci. Rep. 2019, 9, 3000. [Google Scholar] [CrossRef]
- White, J.B.; Dufresne, C.R. Management and avoidance of complications in chin augmentation. Aesthet. Surg. J. 2011, 31, 634–642. [Google Scholar] [CrossRef] [PubMed]
- Khan, M.; Sattar, N.; Erkin, M. Postoperative Complications in Genioplasty and Their Association with Age, Gender, and Type of Genioplasty. Int. J. Dent. 2021, 2021, 8134680. [Google Scholar] [CrossRef] [PubMed]
- Guyot, L. Orthognathic surgery: Surgical failures and complications. L’Orthodontie Française 2016, 87, 107–109. [Google Scholar] [CrossRef] [PubMed]
- Bargi, H.H.A.I.; Suleiman Alshehri, S.A. Massive submentalhematoma, a rare complication after osseous genioplasty. Literature Review and Case Report. J. Dent. Health Oral Disord. Ther. 2016, 5, 00151. [Google Scholar] [CrossRef]
- Bertossi, D.; Albanese, M.; Nocini, R.; Mortellaro, C.; Kumar, N.; Nocini, P.F. Osteotomy in Genioplasty by Piezosurgery. J. Craniofacial Surg. 2021, 32, e317–e321. [Google Scholar] [CrossRef]
- Oth, O.; Mestrallet, P.; Glineur, R. Clinical Study on the Minimally Invasive-Guided Genioplasty Using Piezosurgery and 3D Printed Surgical Guide. Ann. Maxillofac. Surg. 2020, 10, 91–95. [Google Scholar] [CrossRef]
- Lim, S.H.; Kim, M.K.; Kang, S.H. Genioplasty using a simple CAD/CAM (computer-aided design and computer-aided manufacturing) surgical guide. Maxillofac. Plast. Reconstr. Surg. 2015, 37, 44. [Google Scholar] [CrossRef]
- Navarro Cuéllar, C.; Tousidonis Rial, M.; Antúnez-Conde, R.; Ochandiano Caicoya, S.; Navarro Cuéllar, I.; Arenas de Frutos, G.; Sada Urmeneta, Á.; García-Hidalgo Alonso, M.I.; Navarro Vila, C.; Salmerón Escobar, J.I. Virtual Surgical Planning, Stereolitographic Models and CAD/CAM Titanium Mesh for Three-Dimensional Reconstruction of Fibula Flap with Iliac Crest Graft and Dental Implants. J. Clin. Med. 2021, 10, 1922. [Google Scholar] [CrossRef]
- Fleury, C.M.; Sayyed, A.A.; Baker, S.B. Custom Plates in Orthognathic Surgery: A Single Surgeon’s Experience and Learning Curve. J. Craniofacial Surg. 2022, 33, 1976–1981. [Google Scholar] [CrossRef] [PubMed]
- Van Sickels, J.E.; Tiner, B.D. Cost of a genioplasty under deep intravenous sedation in a private office versus general anesthesia in an outpatient surgical center. J. Oral Maxillofac. Surg. 1992, 50, 687–690. [Google Scholar] [CrossRef]
- Kumar, P.; Priya, K.; Kirti, S.; Johar, S.; Singh, V. Dexmedetomidine Supported Office Based Genioplasty: A Pilot Study. J. Maxillofac. Oral Surg. 2015, 14, 750–753. [Google Scholar] [CrossRef][Green Version]

| Conventional Genioplasty | Guided Genioplasty | p Value | |
|---|---|---|---|
| Advance (mm.) | 0.13 ± 0.05 | 0.46 ± 0.02 | 0.125 |
| Retrusion (mm.) | 0.18 ± 0.5 | 0.10 ±0.06 | 0.216 |
| Midline change (degrees) | 2.60 ± 0.51 | 0.50 ± 0.22 | 0.011 |
| Excellent | Good | Poor | |
|---|---|---|---|
| Conventional genioplasty | 15 | 3 | 0 |
| Guided genioplasty | 23 | 2 | 0 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Antúnez-Conde Hidalgo, R.; Silva Canal, J.L.; Navarro Cuéllar, C.; Sánchez Gallego-Albertos, C.; Arias Gallo, J.; Navarro Cuéllar, I.; López Davis, A.; Demaria Martínez, G.; Naranjo Aspas, N.; Zamorano León, J.; et al. Guided Genioplasty: Comparison between Conventional Technique and Customized Guided Surgery. J. Pers. Med. 2023, 13, 1702. https://doi.org/10.3390/jpm13121702
Antúnez-Conde Hidalgo R, Silva Canal JL, Navarro Cuéllar C, Sánchez Gallego-Albertos C, Arias Gallo J, Navarro Cuéllar I, López Davis A, Demaria Martínez G, Naranjo Aspas N, Zamorano León J, et al. Guided Genioplasty: Comparison between Conventional Technique and Customized Guided Surgery. Journal of Personalized Medicine. 2023; 13(12):1702. https://doi.org/10.3390/jpm13121702
Chicago/Turabian StyleAntúnez-Conde Hidalgo, Raúl, José Luis Silva Canal, Carlos Navarro Cuéllar, Celia Sánchez Gallego-Albertos, Javier Arias Gallo, Ignacio Navarro Cuéllar, Antonio López Davis, Gastón Demaria Martínez, Néstor Naranjo Aspas, José Zamorano León, and et al. 2023. "Guided Genioplasty: Comparison between Conventional Technique and Customized Guided Surgery" Journal of Personalized Medicine 13, no. 12: 1702. https://doi.org/10.3390/jpm13121702
APA StyleAntúnez-Conde Hidalgo, R., Silva Canal, J. L., Navarro Cuéllar, C., Sánchez Gallego-Albertos, C., Arias Gallo, J., Navarro Cuéllar, I., López Davis, A., Demaria Martínez, G., Naranjo Aspas, N., Zamorano León, J., & Chamorro Pons, M. (2023). Guided Genioplasty: Comparison between Conventional Technique and Customized Guided Surgery. Journal of Personalized Medicine, 13(12), 1702. https://doi.org/10.3390/jpm13121702








