Measuring Perceived Voice Disorders and Quality of Life among Female University Teaching Faculty
Abstract
:1. Introduction
2. Methods
2.1. Study Design and Setting
2.2. Sample Size and Sampling Techniques
2.3. Study Tool
2.4. Ethical Considerations
2.5. Statistical Analysis
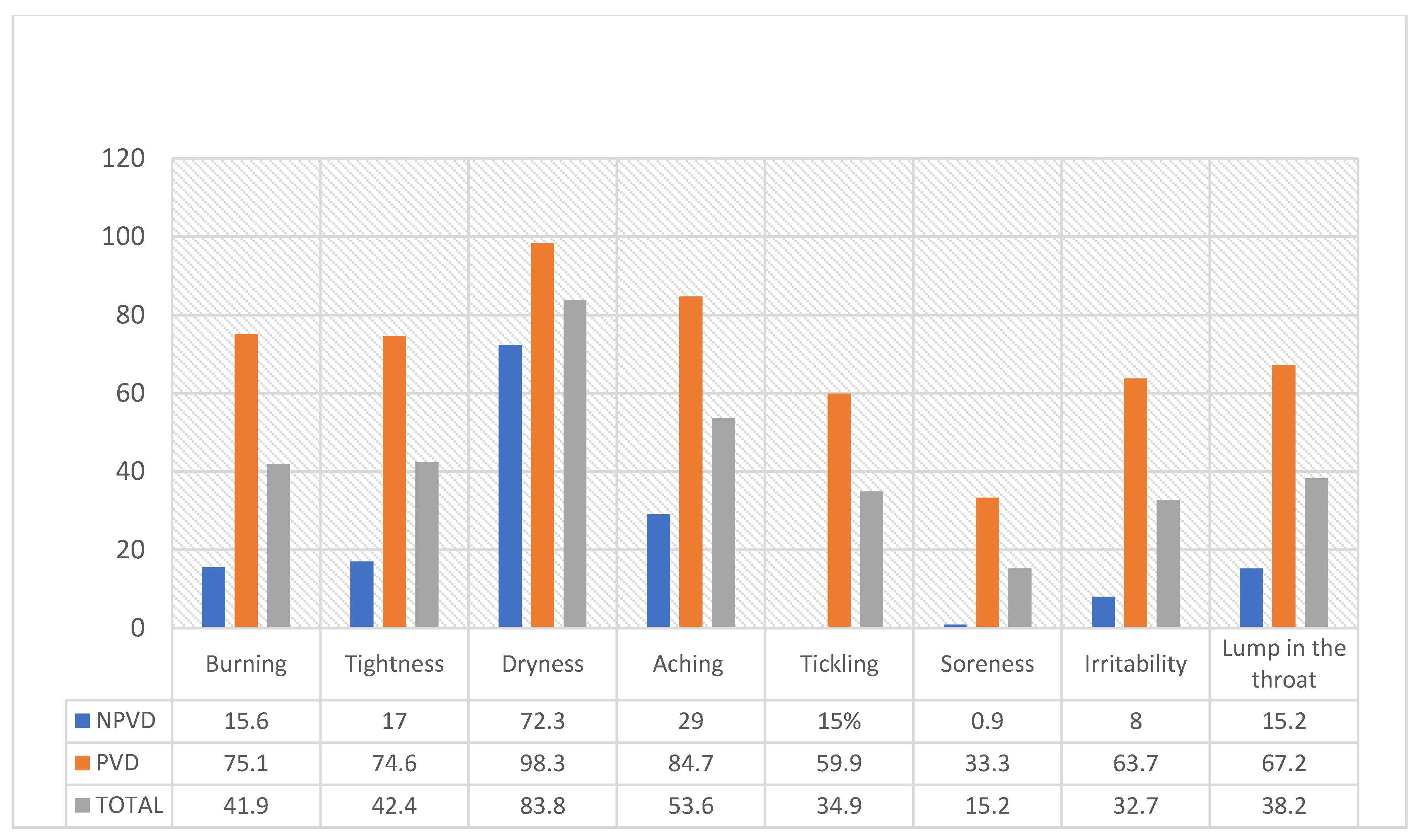
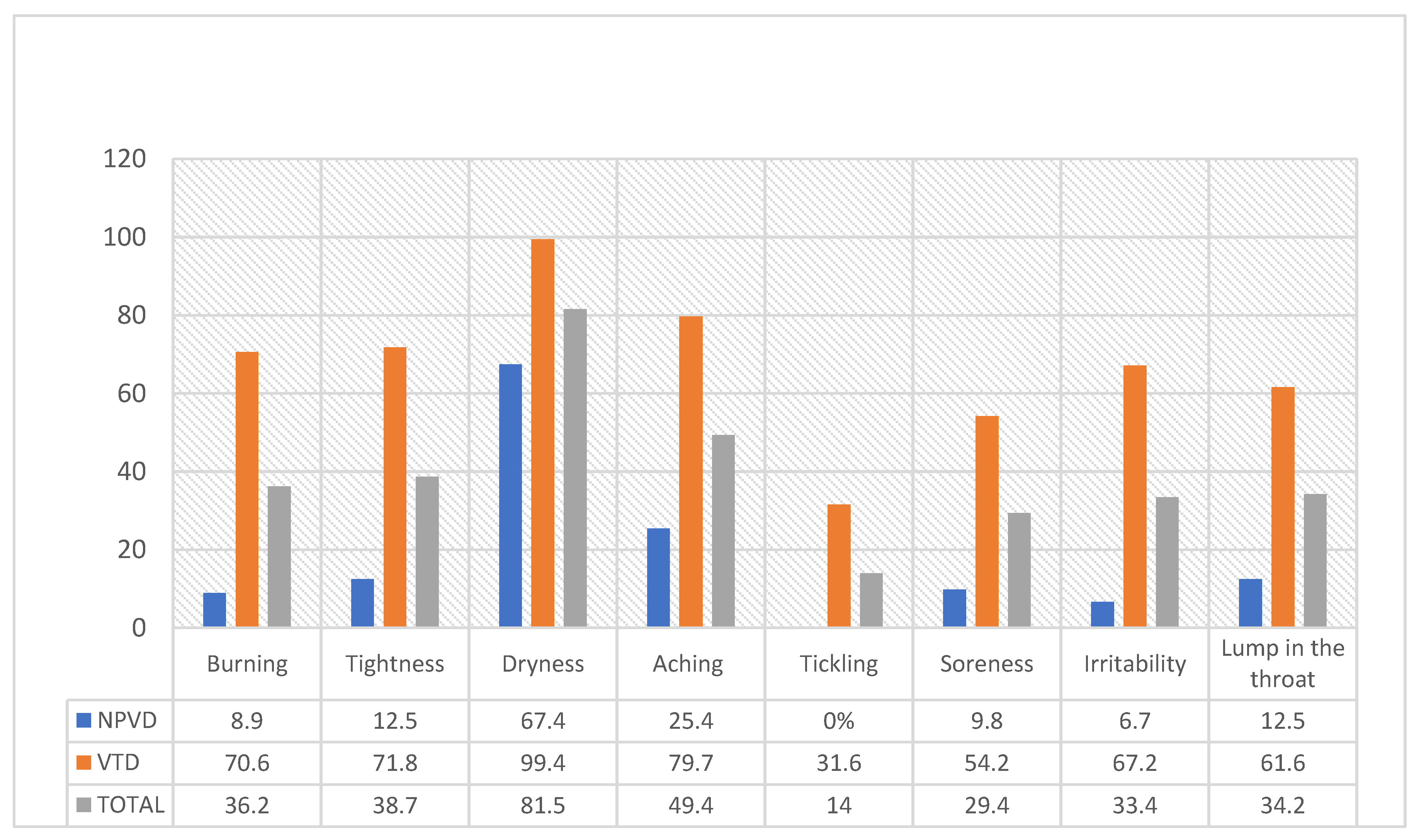
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Vilkman, E. Voice Problems at Work: A Challenge for Occupational Safety and Health Arrangement. Folia Phoniatr. Logop. 2000, 52, 120–125. [Google Scholar] [CrossRef] [PubMed]
- Koufmann, J.; Isaacson, G. Clinical Voice Pathology: Theory and Management, 2nd ed.; Singular Publishing Group: San Diego, CA, USA, 1991. [Google Scholar]
- Stemple, J.C.; Roy, N.; Klaben, B.K. Clinical Voice Pathology: Theory and Management; Plural Publishing: San Diego, CA, USA, 2018. [Google Scholar]
- Grillo, E.U.; Fugowski, J. Voice Characteristics of Female Physical Education Student Teachers. J. Voice 2011, 25, e149–e157. [Google Scholar] [CrossRef] [PubMed]
- Roy, N.; Merrill, R.M.; Thibeault, S.; Gray, S.D.; Smith, E.M. Voice Disorders in Teachers and the General Population. J. Speech Lang. Hear. Res. 2004, 47, 542–551. [Google Scholar] [CrossRef]
- Gomes, N.R.; Teixeira, L.C.; de Medeiros, A.M. Vocal Symptoms in University Professors: Their Association with Vocal Re-sources and with Work Environment. J. Voice 2020, 34, 352–357. [Google Scholar] [CrossRef]
- Lopes, L.W.; Cabral, G.F.; de Almeida, A.A.F. Vocal Tract Discomfort Symptoms in Patients with Different Voice Disorders. J. Voice 2015, 29, 317–323. [Google Scholar] [CrossRef]
- Korn, G.P.; Pontes, A.A.d.L.; Abranches, D.; Pontes, P.A.d.L. Hoarseness and Risk Factors in University Teachers. J. Voice 2015, 29, 518.e21–518.e28. [Google Scholar] [CrossRef]
- American Speech-Language-Hearing Association Definitions of Communication Disorders and Variations. Available online: https://www.asha.org/policy/RP1993-00208/ (accessed on 1 October 2023).
- Casper, J.K.; Leonard, R. Understanding Voice Problems: A Physiological Perspective for Diagnosis and Treatment; Lippincott Williams & Wilkins: Philadelphia, PA, USA, 2006. [Google Scholar]
- Azari, S.; Aghaz, A.; Maarefvand, M.; Ghelichi, L.; Pashazadeh, F.; Shavaki, Y.A. The Prevalence of Voice Disorders and the Related Factors in University Professors: A Systematic Review and Meta-Analysis. J. Voice 2022. [Google Scholar] [CrossRef]
- Mathieson, L.; Hirani, S.; Epstein, R.; Baken, R.; Wood, G.; Rubin, J. Laryngeal Manual Therapy: A Preliminary Study to Examine its Treatment Effects in the Management of Muscle Tension Dysphonia. J. Voice 2009, 23, 353–366. [Google Scholar] [CrossRef]
- Darawsheh, W.B.; Natour, Y.S.; Sada, E.G. Applicability of the Arabic version of Vocal Tract Discomfort Scale (VTDS) with student singers as professional voice users. Logop. Phoniatr. Vocol. 2017, 43, 80–91. [Google Scholar] [CrossRef]
- Skevington, S.M.; Lotfy, M.; O’Connell, K.A. The World Health Organization’s WHOQOL-BREF Quality of Life Assessment: Psychometric Properties and Results of the International Field Trial. A Report from the WHOQOL Group. Qual. Life Res. 2004, 13, 299–310. [Google Scholar] [CrossRef]
- Ohaeri, J.U.; Awadalla, A.W. The reliability and validity of the short version of the WHO Quality of Life Instrument in an Arab general population. Ann. Saudi Med. 2009, 29, 98–104. [Google Scholar] [CrossRef] [PubMed]
- Byeon, H. The Risk Factors Related to Voice Disorder in Teachers: A Systematic Review and Meta-Analysis. Int. J. Environ. Res. Public Health 2019, 16, 3675. [Google Scholar] [CrossRef] [PubMed]
- de Jong, F.; Kooijman, P.; Thomas, G.; Huinck, W.; Graamans, K.; Schutte, H. Epidemiology of Voice Problems in Dutch Teachers. Folia Phoniatr. Logop. 2006, 58, 186–198. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.J.; Lim, S.-E.; Choi, H.-S.; Lim, J.-Y. A Comparison of Voice Activity and Participation Profiles according to the Patterns of Professional Voice Use. Commun. Sci. Disord. 2019, 24, 758–769. [Google Scholar] [CrossRef]
- Padmashali, S.; Nayak, S.; Devadas, U. Prevalence of vocal fatigue and associated risk factors in university teachers. Speech Lang. Hear. 2022, 25, 507–514. [Google Scholar] [CrossRef]
- Higgins, K.P.; Smith, A.B. Prevalence and Characteristics of Voice Disorders in a Sample of University Teaching Faculty. Contemp. Issues Commun. Sci. Disord. 2012, 39, 69–75. [Google Scholar] [CrossRef]
- Article, O.; Alva, A.; Machado, M.; Bhojwani, K.; Sreedharan, S. Study of Risk Factors for Development of Voice Disorders and its Impact on the Quality of Life of School Teachers in Mangalore, India. J. Clin. Diagn. Res. 2017, 11, MC01–MC05. [Google Scholar] [CrossRef]
- Åhlander, V.L.; Rydell, R.; Löfqvist, A. Speaker’s Comfort in Teaching Environments: Voice Problems in Swedish Teaching Staff. J. Voice 2011, 25, 430–440. [Google Scholar] [CrossRef]
- Boominathan, P.; Samuel, J.; Arunachalam, R.; Nagarajan, R.; Mahalingam, S. Multi Parametric Voice Assessment: Sri Ramachandra University Protocol. Indian J. Otolaryngol. Head Neck Surg. 2014, 66, 246–251. [Google Scholar] [CrossRef]
- Villanueva-Reyes, A. Voice Disorders in the Metropolitan Area of San Juan, Puerto Rico: Profiles of Occupational Groups. J. Voice 2009, 25, 83–87. [Google Scholar] [CrossRef]
- Chen, S.H.; Chiang, S.-C.; Chung, Y.-M.; Hsiao, L.-C.; Hsiao, T.-Y. Risk Factors and Effects of Voice Problems for Teachers. J. Voice 2010, 24, 183–192. [Google Scholar] [CrossRef] [PubMed]
- Feng, S.; Weng, C.; Cai, S.; Yang, Z.; Wu, M.; Kang, N. The prevalence and risk factors for perceived voice disorders in public school teachers. Laryngoscope Investig. Otolaryngol. 2022, 7, 790–798. [Google Scholar] [CrossRef] [PubMed]
- Devadas, U.; Jose, N.; Gunjawate, D. Prevalence and Influencing Risk Factors of Voice Problems in Priests in Kerala. J. Voice 2016, 30, 771.e27–771.e32. [Google Scholar] [CrossRef]
- Georgalas, V.L.; Kalantzi, N.; Harpur, I.; Kenny, C. The Effects of Caffeine on Voice: A Systematic Review. J. Voice 2021, 37, 636.e7–636.e19. [Google Scholar] [CrossRef]
- Thibeault, S.L.; Merrill, R.M.; Roy, N.; Gray, S.D.; Smith, E.M. Occupational Risk Factors Associated with Voice Disorders among Teachers. Ann. Epidemiol. 2004, 14, 786–792. [Google Scholar] [CrossRef] [PubMed]
- Tavares, E.L.; Martins, R.H. Vocal Evaluation in Teachers with or without Symptoms. J. Voice 2007, 21, 407–414. [Google Scholar] [CrossRef]
- Preciado-López, J.; Pérez-Fernández, C.; Calzada-Uriondo, M.; Preciado-Ruiz, P. Epidemiological Study of Voice Disorders among Teaching Professionals of La Rioja, Spain. J. Voice 2008, 22, 489–508. [Google Scholar] [CrossRef]
- Pereira, E.R.B.N.; Tavares, E.L.M.; Martins, R.H.G. Voice Disorders in Teachers: Clinical, Videolaryngoscopical, and Vocal Aspects. J. Voice 2015, 29, 564–571. [Google Scholar] [CrossRef]
- Cantor-Cutiva, L.C.; Banks, R.E.; Hunter, E.J. The Effect of Upper Airway Ailments on Teachers’ Experience of Vocal Fatigue. J. Voice 2020, 36, 226–231. [Google Scholar] [CrossRef]
- Koufman, J.A.; Amin, M.R.; Panetti, M. Prevalence of Reflux in 113 Consecutive Patients with Laryngeal and Voice Disorders. Otolaryngol. Neck Surg. 2000, 123, 385–388. [Google Scholar] [CrossRef]
- Lowden, M.; Mcglashan, J.A.; Steel, A.; Strugala, V.; Lowden, M.; Mcglashan, J.A.; Steel, A.; Strugala, V.; Strugala, V.; Dettmar, P.W. Prevalence of Symptoms Suggestive of Extra-Oesophageal Reflux in a General Practice Population in the UK. Logop. Phoniatr. Vocology 2009, 34, 32–35. [Google Scholar] [CrossRef]
- Kotby, M.N.; Hassan, O.; El-Makhzangy, A.M.N.; Farahat, M.; Shadi, M.; Milad, P. Gastroesophageal Re-flux/Laryngopharyngeal Reflux Disease: A Critical Analysis of the Literature. Eur. Arch. Oto-Rhino-Laryngol. 2010, 267, 171–179. [Google Scholar] [CrossRef]
- Remacle, M.; Lawson, G. Diagnosis and Management of Laryngopharyngeal Reflux Disease. Curr. Opin. Otolaryngol. Head Neck Surg. 2006, 14, 143–149. [Google Scholar] [CrossRef] [PubMed]
- de Magalhães, T.A.; Ferreira, E.D.; de Souza, J.E.M.; Santos, V.M.; Rossi-Barbosa, L.A.R.; Nascimento, J.E.; Silveira, M.F.; Haikal, D.S. Voice Disorders and Mental health of Basic Education Teachers in a Brazilian Municipality. J. Voice 2023. [Google Scholar] [CrossRef]
- Dietrich, M.; Abbott, K.V.; Gartner-Schmidt, J.; Rosen, C.A. The Frequency of Perceived Stress, Anxiety, and Depression in Patients with Common Pathologies Affecting Voice. J. Voice 2008, 22, 472–488. [Google Scholar] [CrossRef]
- Kooijman, P.; de Jong, F.; Thomas, G.; Huinck, W.; Donders, R.; Graamans, K.; Schutte, H. Risk Factors for Voice Problems in Teachers. Folia Phoniatr. Logop. 2006, 58, 159–174. [Google Scholar] [CrossRef] [PubMed]
- Nybacka, I.; Simberg, S.; Santtila, P.; Sala, E.; Sandnabba, N.K. Genetic and Environmental Effects on Vocal Symptoms and Their Intercorrelations. J. Speech Lang. Hear. Res. 2012, 55, 541–553. [Google Scholar] [CrossRef] [PubMed]
- Johnson, A. Disorders of Speaking in the Professional Voice User. In Vocal Arts Medicine: The Care and Prevention of Professional Voice Disorders; Benninger, M., Jacobson, B., Johnson, A., Eds.; Thieme: New York, NY, USA, 1994. [Google Scholar]
- Rubén, D.; Huamán, T. Psychosocial Risk Factors and Perceived Stress in University Professors Factores de Riesgos Psicosociales y Estrés Percibido En Docentes Universitarios. J. Educ. Psychol.-Propos. Represent. 2019, 7, 339–354. [Google Scholar]
- García-González, M.A.; Torrano, F.; García-González, G. Analysis of Stress Factors for Female Professors at Online Universities. Int. J. Environ. Res. Public Health 2020, 17, 2958. [Google Scholar] [CrossRef]
- Gervais, R.L.; Millear, P.M. Women’s Contribution to the Workplace. In Exploring Resources, Life-Balance and Well-Being of Women Who Work in a Global Context; Springer: Berlin/Heidelberg, Germany, 2016; pp. 15–31. ISBN 9783319317366. [Google Scholar]
- Sun, W.; Wu, H.; Wang, L. Occupational Stress and Its Related Factors among University Teachers in China. J. Occup. Health 2011, 53, 280–286. [Google Scholar] [CrossRef]
- Bozzon, R.; Murgia, A.; Poggio, B.; Rapetti, E. Work–life interferences in the early stages of academic careers: The case of precarious researchers in Italy. Eur. Educ. Res. J. 2017, 16, 332–351. [Google Scholar] [CrossRef]
- Lyberg-Åhlander, V.; Rydell, R.; Fredlund, P.; Magnusson, C.; Wilén, S. Prevalence of Voice Disorders in the General Population, Based on the Stockholm Public Health Cohort. J. Voice 2014, 33, 900–905. [Google Scholar] [CrossRef] [PubMed]
- Moradi, N.; Pourshahbaz, A.; Soltani, M.; Javadipour, S. Cutoff Point at Voice Handicap Index Used to Screen Voice Disorders among Persian Speakers. J. Voice 2013, 27, 130.e1–130.e5. [Google Scholar] [CrossRef] [PubMed]
- Ramos, J.S.; Feniman, M.R.; Gielow, I.; Silverio, K.C.A. Correlation between Voice and Auditory Processing. J. Voice 2018, 32, 771.e25–771.e36. [Google Scholar] [CrossRef] [PubMed]
- Thompson, A. Pharmacological agents with effects on voice. Am. J. Otolaryngol. 1995, 16, 12–16. [Google Scholar] [CrossRef] [PubMed]
- Ramanathan, S.; Ayyasamy, G. Voice Disorders and Reflux Disease—A Prospective Study. J. Sci. Study 2021, 8, 8–11. [Google Scholar]
- Schwartz, S.R.; Cohen, S.M.; Dailey, S.H.; Rosenfeld, R.M.; Deutsch, E.S.; Gillespie, M.B.; Granieri, E.; Hapner, E.R.; Kimball, C.E.; Krouse, H.J.; et al. Clinical Practice Guideline: Hoarseness (Dysphonia). Otolaryngol. Neck Surg. 2009, 141, 1–31. [Google Scholar] [CrossRef]
- Chan, R.W.; Tayama, N. Biomechanical Effects of Hydration in Vocal Fold Tissues. Otolaryngol. Neck Surg. 2002, 126, 528–537. [Google Scholar] [CrossRef]
- Verdolini, K.; Titze, I.R.; Fennell, A. Dependence of Phonatory Effort on Hydration Level. J. Speech Lang. Hear. Res. 1994, 37, 1001–1007. [Google Scholar] [CrossRef]
- Hamdan, A.-L.; Sibai, A.; Rameh, C. Effect of Fasting on Voice in Women. J. Voice 2007, 21, 495–501. [Google Scholar] [CrossRef]
- Sivasankar, M.; Fisher, K.V. Oral Breathing Increases P Th and Vocal Effort by Superficial Drying of Vocal Fold Mucosa. J. Voice 2002, 16, 172–181. [Google Scholar] [CrossRef] [PubMed]
- Nichol, K.L.; Tummers, K.; Hoyer-Leitzel, A.; Marsh, J.; Moynihan, M.; McKelvey, S. Modeling Seasonal Influenza Outbreak in a Closed College Campus: Impact of Pre-Season Vaccination, In-Season Vaccination and Holidays/Breaks. PLoS ONE 2010, 5, e9548. [Google Scholar] [CrossRef]
- Ma, E.P.; Yiu, E.M. Voice Activity and Participation Profile: Assessing the Impact of Voice Disorders on Daily Activities. J. Speech Lang Hear. Res. 2001, 44, 511–524. [Google Scholar] [CrossRef]
- Lenderking, W.R.; Hillson, E.; Crawley, J.A.; Moore, D.; Berzon, R.; Pashos, C.L. The Clinical Characteristics and Impact of Laryngopharyngeal Reflux Disease on Health-Related Quality of Life. Value Health 2003, 6, 560–565. [Google Scholar] [CrossRef] [PubMed]
- Merrill, R.M.; Anderson, A.E.; Sloan, A. Quality of Life Indicators according to Voice Disorders and Voice-Related Conditions. Laryngoscope 2011, 121, 2004–2010. [Google Scholar] [CrossRef] [PubMed]
- Putnoki, D.d.S.; Hara, F.; Oliveira, G.; Behlau, M. Qualidade de Vida Em Voz: O Impacto de Uma Disfonia de Acordo Com Gênero, Idade e Uso Vocal Profissional. Rev. Soc. Bras. Fonoaudiol. 2010, 15, 485–490. [Google Scholar] [CrossRef]
- Yamasaki, R.; Madazio, G.; Leão, S.H.; Padovani, M.; Azevedo, R.; Behlau, M. Auditory-Perceptual Evaluation of Normal and Dysphonic Voices Using the Voice Deviation Scale. J. Voice 2017, 31, 67–71. [Google Scholar] [CrossRef]
- Lee, Y.; Kim, G.; Sohn, K.; Lee, B.; Lee, J.; Kwon, S. The Usefulness of Auditory Perceptual Assessment and Acoustic Analysis as a Screening Test for Voice Problems. Folia Phoniatr. Logop. 2021, 73, 34–41. [Google Scholar] [CrossRef]
- Awan, S.N.; Roy, N.; Zhang, D.; Cohen, S.M. Validation of the Cepstral Spectral Index of Dysphonia (CSID) as a Screening Tool for Voice Disorders: Development of Clinical Cutoff Scores. J. Voice 2016, 30, 130–144. [Google Scholar] [CrossRef]
| Characteristic | Study Group | Total n (%) | Test | p-Value | OR (95% CI) | ||
|---|---|---|---|---|---|---|---|
| NPVD n (%) | PVD n (%) | ||||||
| Age group (years) | ≤29 | 95 (42.4) | 79 (44.6) | 174 (43.4) | 0.272 | 0.87 | 1 |
| 30–49 | 82 (36.6) | 64 (36.2) | 146 (36.4) | 0.94 (0.60–1.46) | |||
| ≥50 | 47 (21.0) | 34 (19.2) | 81 (20.2) | 0.87 (0.51–1.48) | |||
| Marital status | Not married a | 48 (21.4) | 46 (26.0) | 94 (23.4) | 1.146 | 0.17 | 1 |
| Married | 176 (78.6) | 131 (74.0) | 307 (76.6) | 0.78 (0.489–1.234) | |||
| Number of children | ≤2 | 101 (45.1) | 91 (51.4) | 192 (47.9) | 1.58 | 0.12 | 1 |
| ≥3 | 123 (54.9) | 86 (48.6) | 209 (52.1) | 0.78 (0.52–1.15) | |||
| Academic rank | Professor | 23 (10.3) | 15 (8.5) | 38 (9.5) | 3.93 | 0.56 | 1 |
| Associate Professor | 47 (21.0) | 28 (15.8) | 75 (18.7) | 0.91 (0.41–2.04) | |||
| Assistant Professor | 74 (33.0) | 63 (35.6) | 137 (34.2) | 0.75 (0.35–1.59) | |||
| Lecturer | 57 (25.4) | 44 (24.9) | 101 (25.2) | 1.18 (0.55–2.53) | |||
| Demonstrator | 14 (6.2) | 16 (9.0) | 30 (7.5) | 1.75 (0.67–4.62) | |||
| Language teacher | 9 (4.0) | 11 (6.2) | 20 (5.0) | 1.87 (0.63–5.60) | |||
| Colleges ** | Humanities | 96 (42.9) | 64 (36.2) | 160 (39.9) | 1.9 | 0.75 | 1 |
| Sciences | 53 (23.7) | 48 (27.1) | 101 (25.2) | 1.36 (0.82–2.25) | |||
| Health Science | 54 (24.1) | 47 (26.6) | 101 (25.2) | 1.31 (0.790–2.16) | |||
| Deanships and Institutes | 16 (7.1) | 14 (7.9) | 30 (7.5) | 1.30 (0.59–2.87) | |||
| Applied Colleges | 5 (2.2) | 4 (2.3) | 9 (2.2) | 1.2 (0.31–4.64) | |||
| Total | 224 (55.9) | 177 (44.1) | 401 (100.0) | ||||
| Work-Related Characteristic | Study Group | Total n (%) | Test | p-Value | OR (95% CI) | ||
|---|---|---|---|---|---|---|---|
| NPVD n (%) | PVD n (%) | ||||||
| Teaching experience | <5 years | 30 (13.4) | 29 (16.4) | 59 (14.7) | 4.48 | 0.21 | 1 |
| 5–9 years | 55 (24.6) | 30 (16.9) | 85 (21.2) | 0.56 (0.29–1.11) | |||
| 10–14 years | 58 (25.9) | 56 (31.6) | 114 (28.4) | 0.99 (0.53–1.87) | |||
| ≥15 years | 81 (36.2) | 62 (35.0) | 143 (35.7) | 0.79 (0.43–1.46) | |||
| Administrative positions with teaching | No | 132 (58.9) | 94 (53.1) | 226 (56.4) | 1.36 | 0.24 | 1 |
| Yes | 92 (41.1) | 83 (46.9) | 175 (43.6) | 1.267 (0.85–1.89) | |||
| Average number of teaching hours (hours/week) | 3–5 | 34 (15.2) | 22 (12.4) | 56 (14.0) | 5.75 | 0.22 | 1 |
| 6–8 | 34 (15.2) | 27 (15.3) | 61 (15.2) | 1.23 (0.59–2.56) | |||
| 9–11 | 56 (25.0) | 31 (17.5) | 87 (21.7) | 0.86 (0.43–1.71) | |||
| 12–14 | 62 (27.7) | 55 (31.1) | 117 (29.2) | 1.37 (0.72–2.62) | |||
| ≥15 | 38 (17.0) | 42 (23.7) | 80 (20.0) | 1.71 (0.854–3.42) | |||
| Class size (average number of students/class) | 10–20 | 30 (13.4) | 22 (12.4) | 521 (3.0) | 7.14 | 0.13 | 1 |
| 21–30 | 71 (31.7) | 44 (24.9) | 115 (28.7) | 0.85 (0.43–1.65) | |||
| 31–40 | 61 (27.2) | 40 (22.6) | 101 (25.2) | 0.89 (0.45–1.76) | |||
| 41–50 | 21 (9.4) | 24 (13.6) | 45 (11.2) | 1.56 (0.698–3.48) | |||
| ≥51 | 41 (18.3) | 47 (26.6) | 88 (21.9) | 1.60 (0.78–3.12) | |||
| Remote teaching | No | 175 (78.1) | 137 (77.4) | 312 (77.8) | 0.03 | 0.86 | 1 |
| Yes | 49 (21.9) | 40 (22.6) | 89 (22.2) | 1.04 (0.65–1.68) | |||
| Total | 224 (55.9) | 177 (44.1) | 401 (100.0) | ||||
| Characteristic | Study Group | Total n (%) | Test | p-Value | OR (95% CI) | ||
|---|---|---|---|---|---|---|---|
| NPVD n (%) | PVD n (%) | ||||||
| Thyroid gland problems | No | 187 (83.5) | 153 (86.4) | 340 (84.8) | 0.67 | 0.41 | 1 |
| Yes | 37 (16.5) | 24 (13.6) | 61 (15.2) | 0.79 (0.46–1.38) | |||
| Reflux/ Heartburn | No | 174 (77.7) | 99 (55.9) | 273 (68.1) | 21.5 | <0.001 * | 1 |
| Yes | 50 (22.3) | 78 (44.1) | 128 (31.9) | 2.74 (1.78–4.23) | |||
| Asthma | No | 207 (92.4) | 158 (89.3) | 365 (91.0) | 1.20 | 0.27 | 1 |
| Yes | 17 (7.6) | 19 (10.7) | 36 (9.0) | 1.46 (0.74–2.91) | |||
| Fever | No | 216 (96.4) | 170 (96.0) | 386 (96.3) | 0.04 | 0.84 | 1 |
| Yes | 8 (3.6) | 7 (4.0) | 15 (3.7) | 1.11 (0.39–3.13) | |||
| Allergies | No | 179 (79.9) | 110 (62.1) | 289 (72.1) | 15.5 | <0.001 * | 1 |
| Yes | 45 (20.1) | 67 (37.9) | 112 (27.9) | 2.42 (1.55–3.76) | |||
| Hearing impairment | No | 216 (96.4) | 155 (87.6) | 371 (92.5) | 11.21 | 0.002 * | 1 |
| Yes | 8 (3.6) | 22 (12.4) | 30 (7.5) | 3.83 (1.66–8.83) | |||
| Frequent common cold | No | 187 (83.5) | 125 (70.6) | 312 (77.8) | 9.47 | 0.002 * | 1 |
| Yes | 37 (16.5) | 52 (29.4) | 89 (22.2) | 2.10 (1.30–3.39) | |||
| Depression | No | 205 (91.5) | 146 (82.5) | 351 (87.5) | 7.03 | 0.007 * | 1 |
| Yes | 19 (8.5) | 31 (17.5) | 50 (12.5) | 2.29 (1.25–4.21) | |||
| Fatigue | No | 112 (50.0) | 39 (22.0) | 151 (37.7) | 32.9 | <0.001 * | 1 |
| Yes | 112 (50.0) | 138 (78.0) | 250 (62.3) | 3.54 (2.28–5.50) | |||
| Total | 224 (55.9) | 177 (44.1) | 401 (100.0) | ||||
| Characteristic | Study Group | Total n (%) | Test | p-Value | OR (95% CI) | ||
|---|---|---|---|---|---|---|---|
| NPVD n (%) | PVD n (%) | ||||||
| Thyroid gland problems | No | 89 (39.7) | 77 (43.5) | 166 (41.4) | 0.66 | 0.72 | 1 |
| Yes | 29 (12.9) | 20 (11.3) | 49 (12.2) | 0.73 (0.42–1.52) | |||
| NA | 106 (47.3) | 80 (45.2) | 186 (46.4) | 0.78 (0.64–1.08) | |||
| Reflux/ Heartburn | No | 95 (42.4) | 74 (41.8) | 169 (42.1) | 13.86 | 0.001 * | 0.87 (0.57–1.33) |
| Yes | 24 (10.7) | 42 (23.7) | 66 (16.5) | 2.25 (1.25–4.04) | |||
| NA | 105 (46.9) | 61 (34.5) | 166 (41.4) | 0.75 (0.48–1.16) | |||
| Asthma | No | 92 (41.1) | 73 (41.2) | 165 (41.1) | 2.25 | 0.33 | 1 |
| Yes | 15 (6.7) | 19 (10.7) | 34 (8.5) | 1.59 (0.76–3.36) | |||
| NA | 117 (52.2) | 85 (48.0) | 202 (50.4) | 0.92 (0.60–1.39) | |||
| Fever | No | 95 (42.4) | 80 (45.2) | 175 (43.6) | 0.57 | 0.75 | 1 |
| Yes | 6 (2.7) | 6 (3.4) | 12 (3.0) | 1.19 (0.367–3.83) | |||
| NA | 123 (54.9) | 91 (51.4) | 214 (53.4) | 0.88 (0.59–1.31) | |||
| Allergies | No | 98 (43.8) | 68 (38.4) | 166 (41.4) | 12.13 | 0.002 * | 1 |
| Yes | 26 (11.6) | 44 (24.9) | 70 (17.5) | 2.44 (1.37–4.34) | |||
| NA | 100 (44.6) | 65 (36.7) | 165 (41.1) | 0.94 (0.60–1.45) | |||
| Hearing impairment | No | 98 (43.8) | 92 (52.0) | 190 (47.4) | 3.35 | 0.19 | 1 |
| Yes | 1 (0.4) | 1 (0.0) | 2 (0.4) | 0.9 (0.0717.28) | |||
| NA | 125 (55.8) | 85 (48.0) | 210 (52.4) | 0.72 (0.49–1.08) | |||
| Frequent common cold | No | 100 (44.6) | 77 (43.5) | 177 (44.1) | 4.73 | 0.09 | 1 |
| Yes | 22 (9.8) | 30 (16.9) | 52 (13.0) | 1.78 (0.95–3.31) | |||
| NA | 102 (45.5) | 70 (39.5) | 172 (42.9) | 0.89 (0.58–1.36) | |||
| Depression | No | 97 (43.3) | 83 (46.9) | 180 (44.9) | 3.23 | 0.19 | 1 |
| Yes | 9 (4.0) | 13 (7.3) | 22 (5.5) | 1.69 (0.694.15) | |||
| NA | 118 (52.7) | 81 (45.8) | 199 (49.6) | 0.80 (0.53–1.21) | |||
| Fatigue | No | 148 (66.1) | 117 (66.1) | 265 (66.1) | 20.53 | <0.001 * | 1 |
| Yes | 9 (4.0) | 28 (15.8) | 37 (9.2) | 3.9 (1.79–8.66) | |||
| NA | 67 (29.9) | 32 (18.1) | 99 (24.7) | 0.60 (0.37–0.98) | |||
| Total | 224 (55.9) | 177 (44.1) | 401 (100.0) | ||||
| Characteristic | Study Group | Total n (%) | p-Value | OR (95% CI) | |||
|---|---|---|---|---|---|---|---|
| NPVD n (%) | PVD n (%) | ||||||
| Smoking status | Never smoked | 216 (96.4) | 169 (95.5) | 385 (96.0) | 1.25 | 0.54 | 1 |
| Former smoker | 5 (2.2) | 3 (1.7) | 8 (2.0) | 0.77 (0.18–3.25) | |||
| Current smoker | 3 (1.3) | 5 (2.8) | 8 (2.0) | 2.13 (0.50–9.04) | |||
| Water drunk/day | ≤3 cups | 134 (59.8) | 115 (65.0) | 15 (63.1) | 2.67 | 0.45 | 1 |
| 4–6 cups | 68 (30.4) | 49 (27.7) | 117 (29.2) | 0.84 (0.54–1.31) | |||
| >6 cups | 22 (9.8) | 13 (7.3) | 35 (8.7) | 1.16 (0.55–2.45) | |||
| Caffeinated coffee and tea/day ** | ≤3 cups | 211 (94.2) | 165 (94.2) | 376 (93.7) | 0.632 | <0.001 * | 1 |
| 4–6 cups | 11 (4.9) | 9 (5.1) | 20 (5.0) | 1.05 (0.42–2.58) | |||
| >6 cups | 2 (0.9) | 3 (1.7) | 5 (1.2) | 28.77 (4.35–190.28) | |||
| Decaffeinated coffee and tea/day ** | ≤3 cups | 180 (80.4) | 146 (82.5) | 326 (81.3) | 0.29 | 0.59 | 1 |
| 4–6 cups | 44 (19.6) | 31 (17.5) | 75 (18.7) | 0.87 (0.52–1.45) | |||
| Practice other hobbies using their voice | No | 186 (83.0) | 135 (76.3) | 321 (80.0) | 2.83 | 0.09 | 1 |
| Yes | 38 (17.0) | 42 (23.7) | 80 (20.0) | 1.52 (0.93–2.49) | |||
| Total | 224 (55.9) | 177 (44.1) | 401 (100.0) | ||||
| Study Group | |||||
|---|---|---|---|---|---|
| Variable | Overall (N = 401) M ± SD | NPVD (n = 224) M ± SD | PVD (n = 177) M ± SD | T | p-Value |
| Overall QoL Mdn (IQR) | 4 (1) | 4 (1) | 4 (1) | 1432.5 U (z = −5.10) | <0.001 * |
| Overall health satisfaction Mdn (IQR) | 4 (2) | 4 (2) | 4 (1) | 1470.3 U (z = −4.81) | <0.001 * |
| Physical health M ± SD | 15.09 ± 2.83 | 15.90 ± 2.47 | 14.02 ± 2.92 | 6.12 | <0.001 * |
| Psychological health M ± SD | 14.31 ± 2.69 | 14.90 ± 2.52 | 13.51 ± 2.72 | 4.65 | <0.001 * |
| Social relation M ± SD | 14.61 ± 3.66 | 15.44 ± 3.29 | 13.49 ± 3.86 | 4.75 | <0.001 * |
| Environment M ± SD | 14.30 ± 2.54 | 14.97 ± 2.38 | 13.40 ± 2.49 | 5.55 | <0.001 * |
| WHOQOL-BREF M ± SD | 58.32 ± 10.09 | 61.22 ± 8.91 | 54.43 ±10.32 | 6.17 | <0.001 * |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Al Awaji, N.N.; Alghamdi, K.A.; Alfaris, A.M.; Alzamil, R.Z.; Alhijji, L.N.; Alyehya, G.S.; Al Harbi, S.M.; Mortada, E.M. Measuring Perceived Voice Disorders and Quality of Life among Female University Teaching Faculty. J. Pers. Med. 2023, 13, 1568. https://doi.org/10.3390/jpm13111568
Al Awaji NN, Alghamdi KA, Alfaris AM, Alzamil RZ, Alhijji LN, Alyehya GS, Al Harbi SM, Mortada EM. Measuring Perceived Voice Disorders and Quality of Life among Female University Teaching Faculty. Journal of Personalized Medicine. 2023; 13(11):1568. https://doi.org/10.3390/jpm13111568
Chicago/Turabian StyleAl Awaji, Nisreen Naser, Khaled Abdulraheem Alghamdi, Abdullah Mohammed Alfaris, Rahaf Zamil Alzamil, Lojain Naser Alhijji, Ghaida Saad Alyehya, Shadan Mohammed Al Harbi, and Eman M. Mortada. 2023. "Measuring Perceived Voice Disorders and Quality of Life among Female University Teaching Faculty" Journal of Personalized Medicine 13, no. 11: 1568. https://doi.org/10.3390/jpm13111568
APA StyleAl Awaji, N. N., Alghamdi, K. A., Alfaris, A. M., Alzamil, R. Z., Alhijji, L. N., Alyehya, G. S., Al Harbi, S. M., & Mortada, E. M. (2023). Measuring Perceived Voice Disorders and Quality of Life among Female University Teaching Faculty. Journal of Personalized Medicine, 13(11), 1568. https://doi.org/10.3390/jpm13111568





