Challenges and Strategies for Enhancing eHealth Capacity Building Programs in African Nations
Abstract
:1. Introduction
Factors Influencing the Integration and Use of eHealth
2. Objectives
3. Methods
- eHealth capacity building activities.
- Factors hindering eHealth capacity building among health professionals.
- Health workers IT literacy.
- Proposed suggestions to build IT skills among health professionals.
Quantitative and Qualitative Data Analyses
4. Results
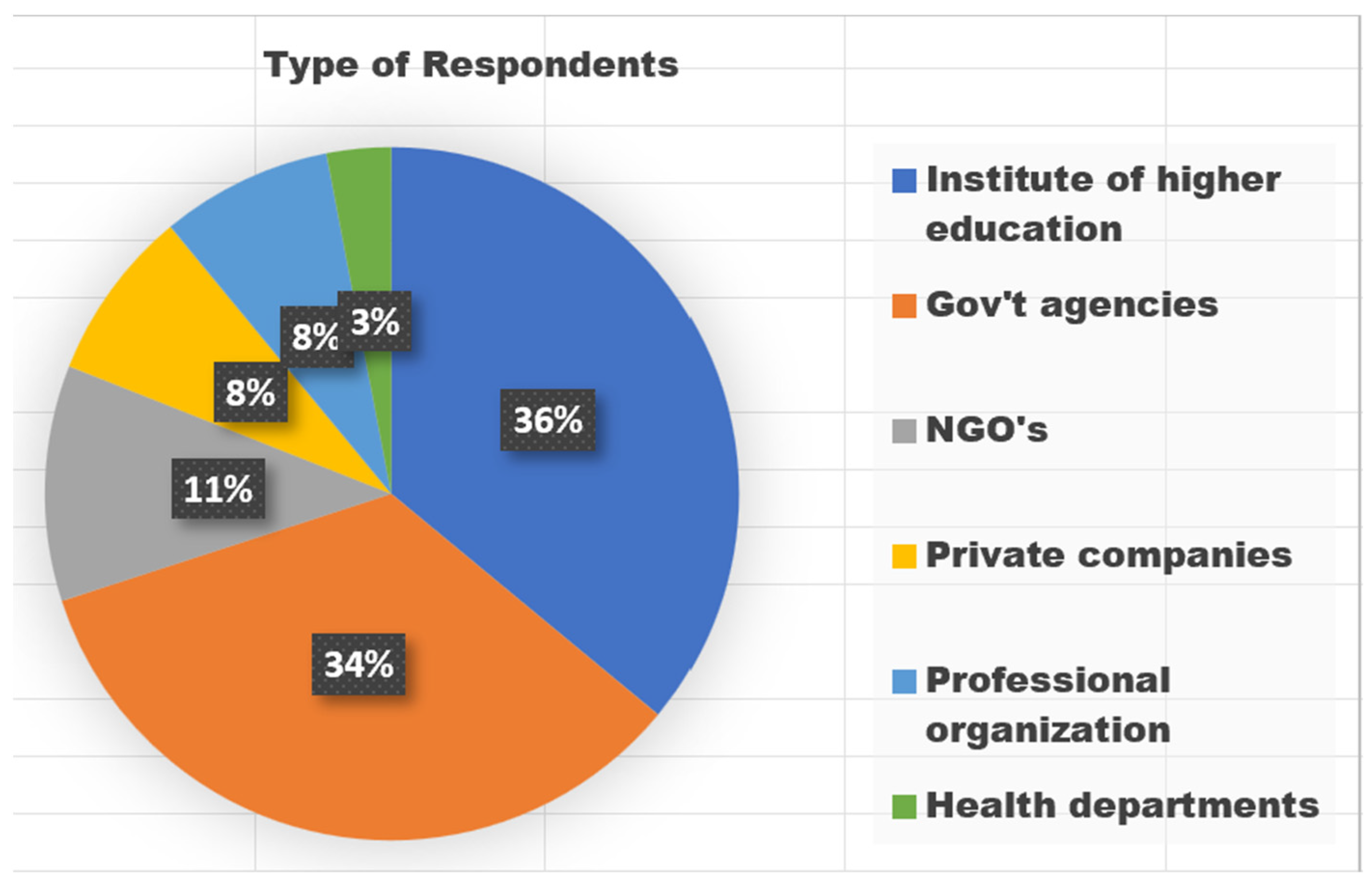
4.1. General Characteristics of Respondents i.e., Organizations
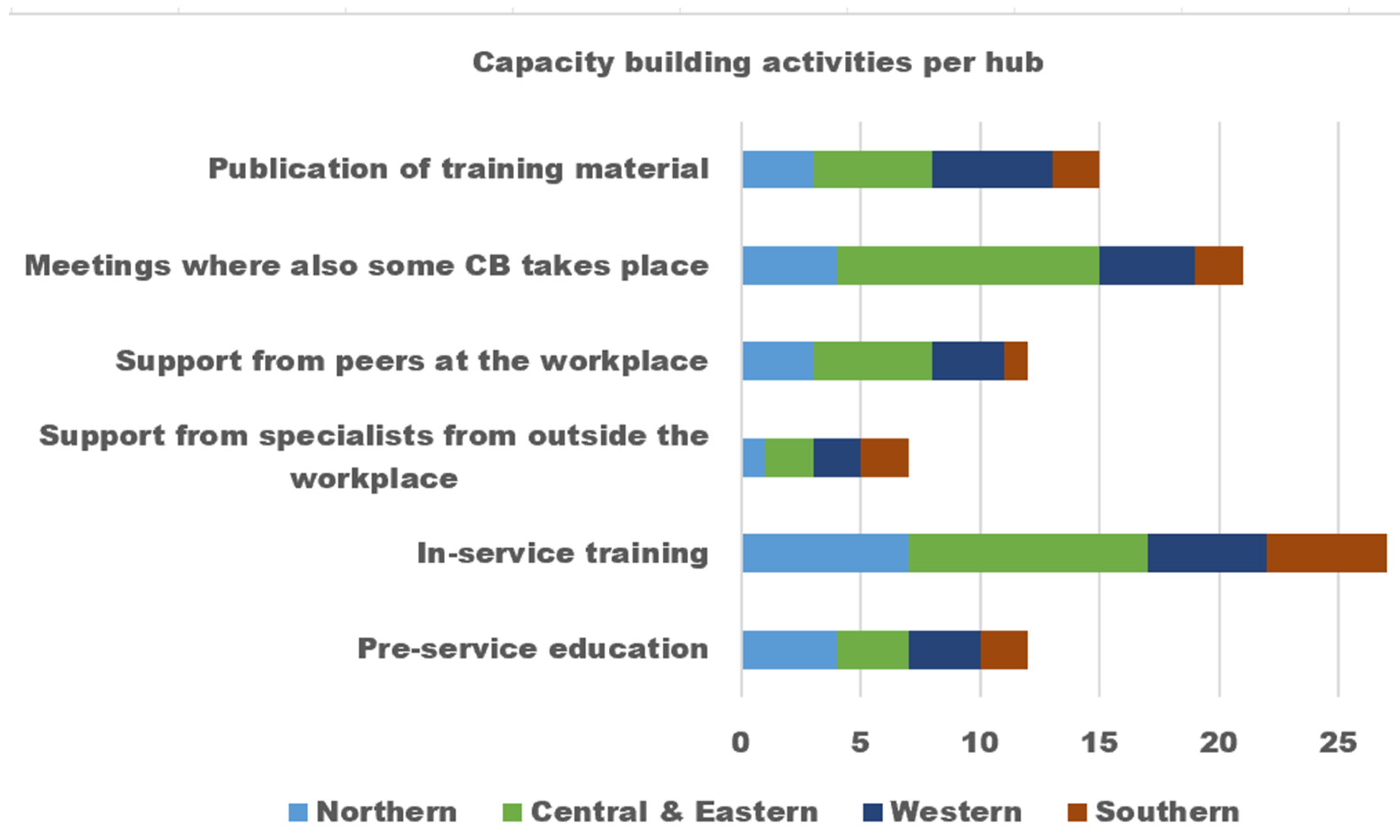
4.2. Capacity Building Activities
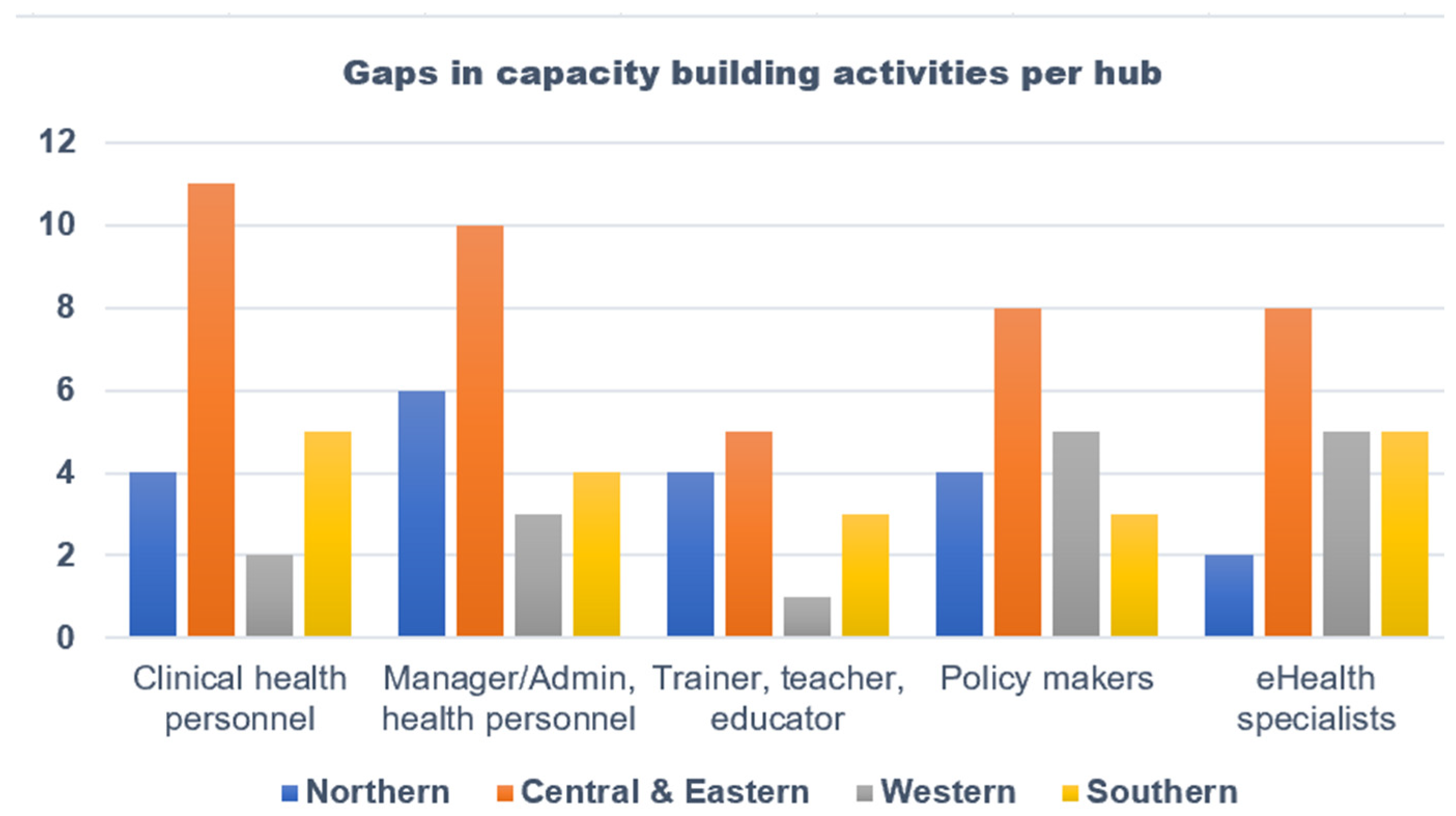
Gaps in Capacity Building Activities
4.3. Factors Hindering eHealth Capacity-Building Activities
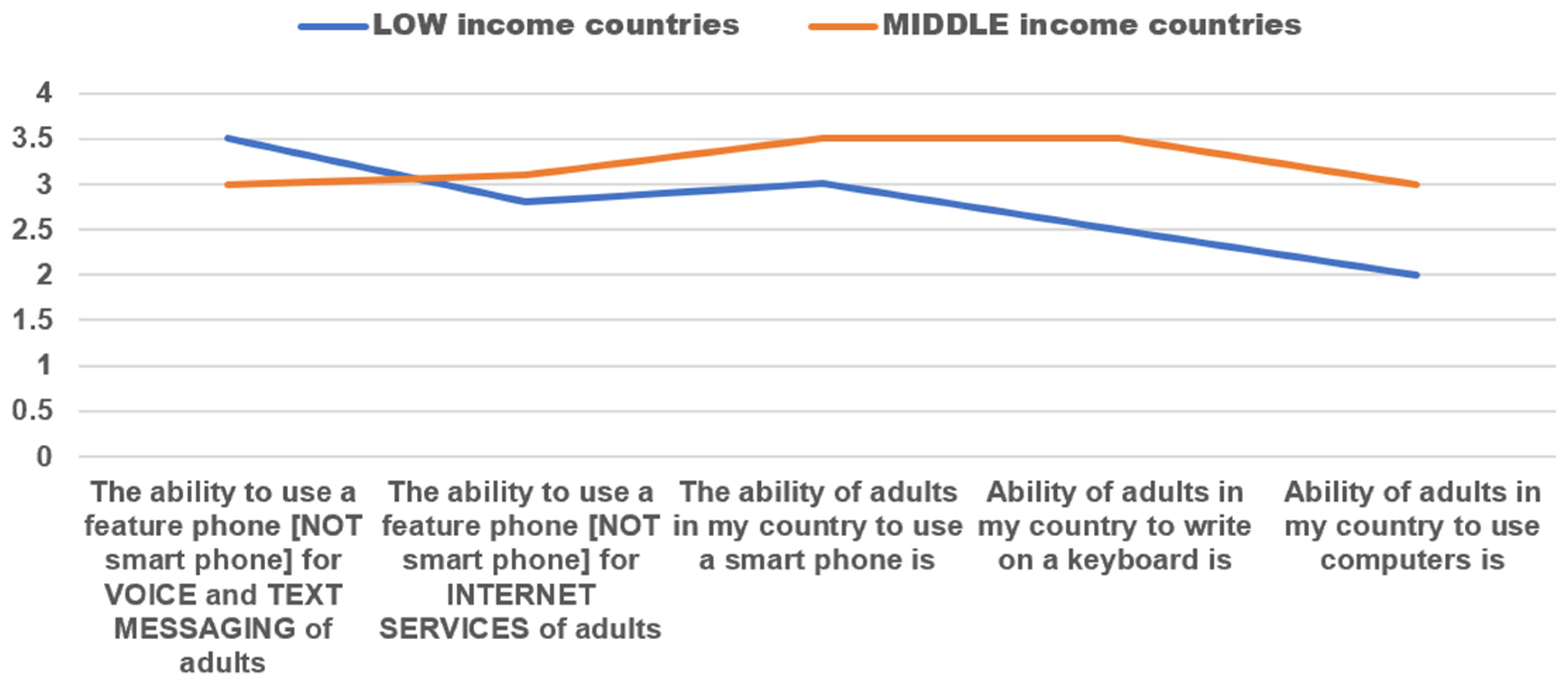
4.4. Health Workers’ IT Literacy
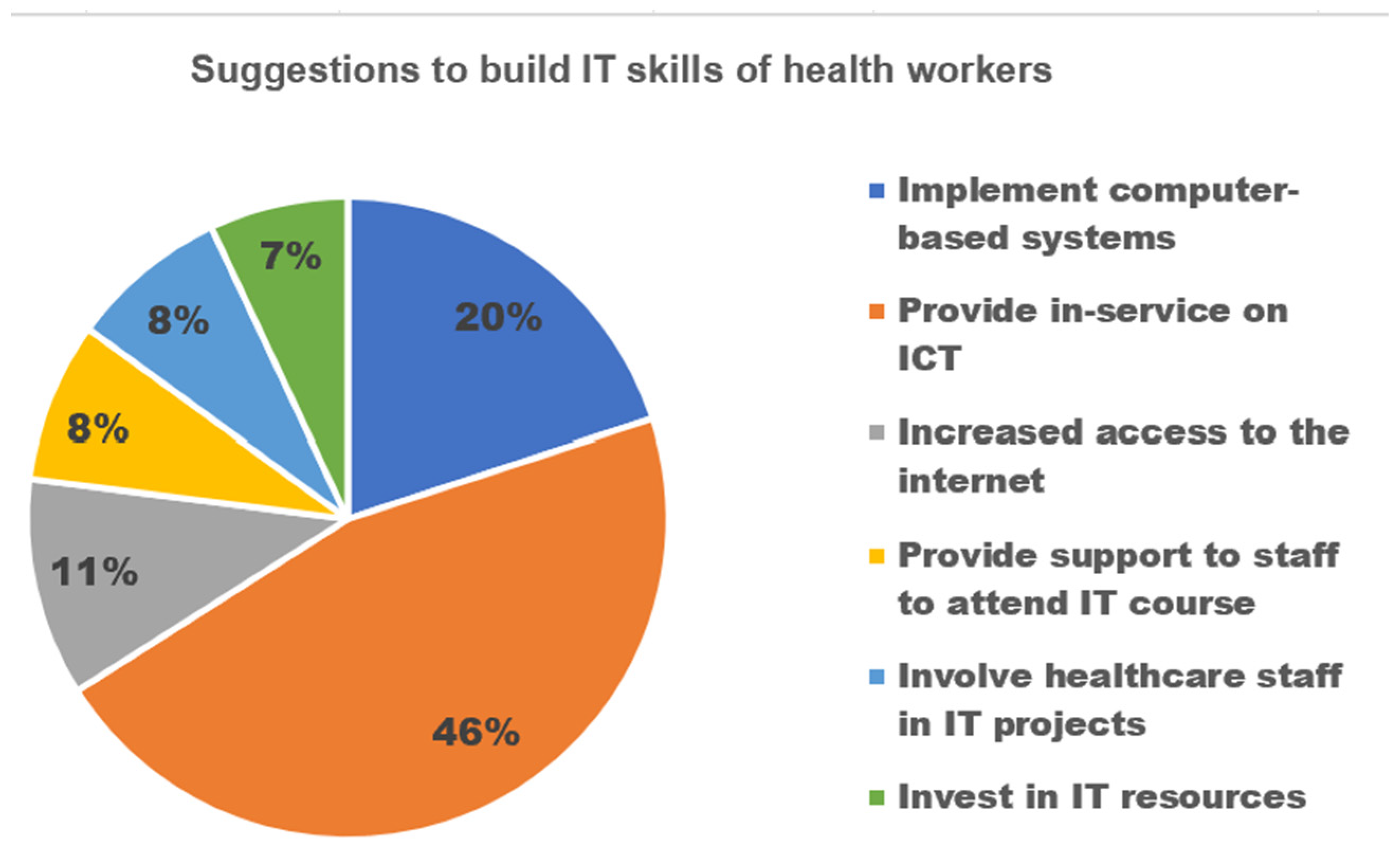
4.5. Proposed Suggestions to Build ICT Skills of Health Personnel
5. Discussion
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Labrique, A.B.; Wadhwani, C.; Williams, K.A.; Lamptey, P.; Hesp, C.; Luk, R.; Aerts, A. Best practices in scaling digital health in low and middle income countries. Glob. Health 2018, 14, 103. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Fifty-Eighth World Health Assembly, Geneva, 16–25 May 2005: Resolutions and Decisions, Annex [Internet]; WHO: Geneva, Switzerland, 2005; Available online: https://apps.who.int/iris/handle/10665/20398 (accessed on 20 July 2022).
- WHO. Global Strategy on Digital Health 2020–2025; WHO: Geneva, Switzerland, 2021. [Google Scholar]
- Manyazewal, T.; Woldeamanuel, Y.; Blumberg, H.M.; Fekadu, A.; Marconi, V.C. The potential use of digital health technologies in the African context: A systematic review of evidence from Ethiopia. NPJ Digit. Med. 2021, 4, 125. [Google Scholar] [CrossRef] [PubMed]
- Asah, F.N.; Kaasbøll, J.J.; Anthun, K.S. Obstacles of eHealth Capacity Building and Innovation Promotion Initiative in African Countries. Stud. Health Technol. Inform. 2022, 299, 33–43. [Google Scholar] [PubMed]
- Eysenbach, G. What is e-health? J. Med. Internet Res. 2001, 3, e833. [Google Scholar] [CrossRef]
- World Health Organization. Global Action Plan on Physical Activity 2018–2030: More Active People for a Healthier World; World Health Organization: Geneva, Switzerland, 2019. [Google Scholar]
- Kluge, E.-H.W. (Ed.) Chapter 5—Framework considerations. In Electron Health Rec [Internet]; Academic Press: Cambridge, MA, USA, 2020; pp. 105–133. Available online: https://www.sciencedirect.com/science/article/pii/B9780128220450000058 (accessed on 3 January 2023).
- Koivu, A.; Mavengere, N.; Ruohonen, M.J.; Hederman, L.; Grimson, J. Exploring the Information and ICT Skills of Health Professionals in Low- and Middle-Income Countries. In Proceedings of the IFIP TC 3 International Conference on Stakeholders and Information Technology in Education: SaITE 2016, Guimarães, Portugal, 5–8 July 2016; Revised Selected Papers 1. Brinda, T., Mavengere, N., Haukijärvi, I., Lewin, C., Passey, D., Eds.; Springer International Publishing: Cham, Switzerland, 2016; pp. 152–162. [Google Scholar]
- Vishwanath, A.; Scamurra, S.D. Barriers to the adoption of electronic health records: Using concept mapping to develop a comprehensive empirical model. Health Inform. J. 2007, 13, 119–134. [Google Scholar] [CrossRef]
- Mehl, G.L.; Tamrat, T.; Bhardwaj, S.; Blaschke, S.; Labrique, A. Digital health vision: Could MomConnect provide a pragmatic starting point for achieving universal health coverage in South Africa and elsewhere? BMJ Glob. Health 2018, 3, e000626. [Google Scholar] [CrossRef]
- Al-Shorbaji, N. Improving Healthcare Access through Digital Health: The Use of Information and Communication Technologies [Internet]. Healthc. Access. IntechOpen 2021. Available online: https://www.intechopen.com/chapters/undefined/state.item.id (accessed on 14 July 2022).
- Kraus, S.; Schiavone, F.; Pluzhnikova, A.; Invernizzi, A.C. Digital transformation in healthcare: Analyzing the current state-of-research. J. Bus. Res. 2021, 123, 557–567. [Google Scholar] [CrossRef]
- World Health Organization. Seventh Meeting of the European Health Information Initiative Steering Group: Copenhagen, Denmark, 21–22 March 2017; World Health Organization, Regional Office for Europe: Geneva, Switzerland, 2017. [Google Scholar]
- van Gemert-Pijnen, J.E.; Wynchank, S.; Covvey, H.D.; Ossebaard, H.C. Improving the credibility of electronic health technologies. Bull. World Health Organ. 2012, 1, 323–323A. [Google Scholar] [CrossRef]
- Hamad, W.B. CURRENT Position and Challenges of E-health in Tanzania: A review of literature. Glob. Sci. J. 2019, 7, 14. [Google Scholar]
- Anderson, J.G. Social, ethical and legal barriers to e-health. Int. J. Med. Inf. 2007, 76, 480–483. [Google Scholar]
- Asah, F.N. Challenges and Approaches of Implementing Standard Health Indicators in Hierarchical Organizations: A Multisited Study; The University of Oslo: Oslo, Norway, 2021. [Google Scholar]
- Mars, M. Building the capacity to build capacity in e-health in sub-Saharan Africa: The KwaZulu-Natal experience. Telemed. E-Health 2012, 18, 32–37. [Google Scholar] [CrossRef] [PubMed]
- Mars, M.; Scott, R.E. Global e-health policy: A work in progress. Health Aff. 2010, 29, 237–243. [Google Scholar] [CrossRef] [PubMed]
- Adebesin, F.; Kotzé, P.; Van Greunen, D.; Foster, R. Barriers & Challenges to the Adoption of E-Health Standards in Africa. In Proceedings of the Health Informatics South Africa Conference (HISA), Port Elizabeth, South Africa, 3–5 July 2013. [Google Scholar]
- Stiawan, D. Interoperability framework for integrated e-health services. Bull. Electr. Eng. Inform. 2020, 9, 354–361. [Google Scholar]
- Sluijs, M.; Veeken, H.; Overbeke, A. Deficient information in developing countries: Internet alone is no solution. Ned. Tijdschr. Geneeskd. 2006, 150, 1351–1354. [Google Scholar]
- Masud, M.; Hossain, S.; Alamri, A. Data Interoperability and Multimedia Content Management in e-Health Systems. IEEE Trans. Inf. Technol. Biomed. 2012, 16, 1015–1023. [Google Scholar] [CrossRef]
- Ahern, D.K.; Kreslake, J.M.; Phalen, J.M. What is eHealth (6): Perspectives on the evolution of eHealth research. J. Med. Internet Res. 2006, 8, e490. [Google Scholar] [CrossRef]
- Mburu, S.; Kamau, O. Framework for Development and Implementation of Digital Health Policies to Accelerate the Attainment of Sustainable Development Goals: Case of Kenya eHealth Policy (2016–2030). J. Health Inform. Afr. 2018, 5, 32–38. [Google Scholar] [CrossRef]
- Luna, D.; Almerares, A.; Mayan, J.C.; de Quirós, F.G.B.; Otero, C. Health informatics in developing countries: Going beyond pilot practices to sustainable implementations: A review of the current challenges. Healthc. Inform. Res. 2014, 20, 3–10. [Google Scholar] [CrossRef]
- Larbi, D.; Anthun, K.S.; Asah, F.N.; Debrah, O.; Antypas, K. Assessing Strategic Priority Factors in eHealth Policies of Four African Countries. In Proceedings of the 2022 IST-Africa Conference (IST-Africa), Virtual, 16–20 May 2022; pp. 1–9. [Google Scholar]
- Jamil, S. From digital divide to digital inclusion: Challenges for wide-ranging digitalization in Pakistan. Telecommun. Policy 2021, 45, 102206. [Google Scholar] [CrossRef]
- Staton, R.; Bautista, A.; Harwell, J.; Jensen, L.; Minister, A.; Roller, S. Computerized provider order entry awareness for nursing: Unintended consequences and remediation plan. CIN Comput. Inform. Nurs. 2013, 31, 401–405. [Google Scholar] [CrossRef] [PubMed]
- Alshahrani, A.; Stewart, D.; MacLure, K. A systematic review of the adoption and acceptance of eHealth in Saudi Arabia: Views of multiple stakeholders. Int. J. Med. Inf. 2019, 128, 7–17. [Google Scholar] [CrossRef] [PubMed]
- Asangansi Macleod, B.; Meremikwu, M. Improving the routine HMIS in Nigeria through mobile technology for community data collection. J. Health Inform. Dev. Ctries. 2013, 7, 76–87. [Google Scholar]
- Qureshi, Q.A.; Shah, B.; Najeebullah; Kundi, G.M.; Nawaz, A.; Miankhel, A.K.; Chishti, K.A.; Qureshi, N.A. Infrastructural barriers to e-health implementation in developing countries. Eur. J. Sustain. Dev. 2013, 2, 163. [Google Scholar]
- Cardellino, P.; Finch, E. Evidence of systematic approaches to innovation in facilities management. J. Facil. Manag. 2006, 4, 150–166. [Google Scholar] [CrossRef]
- Steen, L.; Mao, X. Digital Skills for Health Professionals. 2016, pp. 37–47. Available online: https://www.researchgate.net/publication/311271370_Digital_skills_for_health_professionals#fullTextFileContent (accessed on 10 July 2023).
- Detmer, D.E. Capacity Building in E-Health and Health Informatics: A Review of the Global Vision and Informatics Educational Initiatives of the American Medical Informatics Association. 2010. Available online: https://www.thieme-connect.com/products/ejournals/pdf/10.1055/s-0038-1638698.pdf (accessed on 10 July 2023).
- Shegaw, A.M. Analysing the Challenges of IS implementation in public health institutions of a developing country: The need for flexible strategies. J. Health Inform. Dev. Ctries. 2010, 4, 1–17. [Google Scholar]
- Tchao, E.T.; Acquah, I.; Kotey, S.D.; Aggor, C.S.; Kponyo, J.J. On Telemedicine Implementations in Ghana. Int. J. Adv. Comput. Sci. Appl. 2019, 10, 193–201. [Google Scholar] [CrossRef]
- Curioso, W.H. Building Capacity and Training for Digital Health: Challenges and Opportunities in Latin America. J. Med. Internet Res. 2019, 21, e16513. [Google Scholar] [CrossRef]
- Mengiste, S.A.; Antypas, K.; Johannessen, M.R.; Klein, J.; Kazemi, G.; Kassbøll, J. Research Landscape and Research Priorities in eHealth in four African Countries-A survey. EGOV-CeDEM-EPart 2022, 2022, 130. [Google Scholar]
- Khoja, S.; Durrani, H.; Nayani, P.; Fahim, A. Scope of policy issues in eHealth: Results from a structured literature review. J. Med. Internet Res. 2012, 14, e1633. [Google Scholar] [CrossRef]
- Omary, Z.; Lupiana, D.; Mtenzi, F.; Wu, B. Analysis of the challenges affecting e-healthcare adoption in developing countries: A case of Tanzania. Int. J. Inf. Stud. 2010, 2, 38–50. [Google Scholar]
- Vatsalan, D.; Arunatileka, S.; Chapman, K.; Senaviratne, G.; Sudahar, S.; Wijetileka, D.; Wickramasinghe, Y. Mobile technologies for enhancing eHealth solutions in developing countries. In Proceedings of the 2010 Second International Conference on eHealth, Telemedicine, and Social Medicine, Saint Maarten, Netherlands Antilles, 10–16 February 2010; pp. 84–89. [Google Scholar]
- DEDICATED Project 2020. Available online: https://www.mn.uio/hisp/english. (accessed on 9 July 2022).
- European Health Parliament. Digital Skills for Health Professionals. 2016. Available online: https://www.healthparliament.eu/wp-content/uploads/2017/09/Digital-skills-for-health-professionals.pdf (accessed on 9 September 2023).

| Names of Country | No. of Responses | Regions |
|---|---|---|
| Malawi | 6 | Southern |
| Tanzania | 2 | |
| South Africa | 2 | |
| Mozambique | 4 | |
| Ethiopia | 5 | Central & Eastern |
| Kenya | 3 | |
| Uganda | 1 | |
| Ghana | 4 | Western |
| Togo | 3 | |
| Tunisia | 3 | Northern |
| Mauritania | 2 | |
| Morocco | 1 | |
| Algeria | 1 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Asah, F.N.; Kaasbøll, J.J. Challenges and Strategies for Enhancing eHealth Capacity Building Programs in African Nations. J. Pers. Med. 2023, 13, 1463. https://doi.org/10.3390/jpm13101463
Asah FN, Kaasbøll JJ. Challenges and Strategies for Enhancing eHealth Capacity Building Programs in African Nations. Journal of Personalized Medicine. 2023; 13(10):1463. https://doi.org/10.3390/jpm13101463
Chicago/Turabian StyleAsah, Flora Nah, and Jens Johan Kaasbøll. 2023. "Challenges and Strategies for Enhancing eHealth Capacity Building Programs in African Nations" Journal of Personalized Medicine 13, no. 10: 1463. https://doi.org/10.3390/jpm13101463
APA StyleAsah, F. N., & Kaasbøll, J. J. (2023). Challenges and Strategies for Enhancing eHealth Capacity Building Programs in African Nations. Journal of Personalized Medicine, 13(10), 1463. https://doi.org/10.3390/jpm13101463






