Prostate Artery Embolization: Challenges, Tips, Tricks, and Perspectives
Abstract
1. Introduction
2. Tips and Tricks to Perform Prostate Artery Embolization (PAE)
2.1. Perform an Arterial Mapping: Preoperative Computerized Tomography (CT) Angiogram or Intraoperative Cone-Beam CT (CBCT)
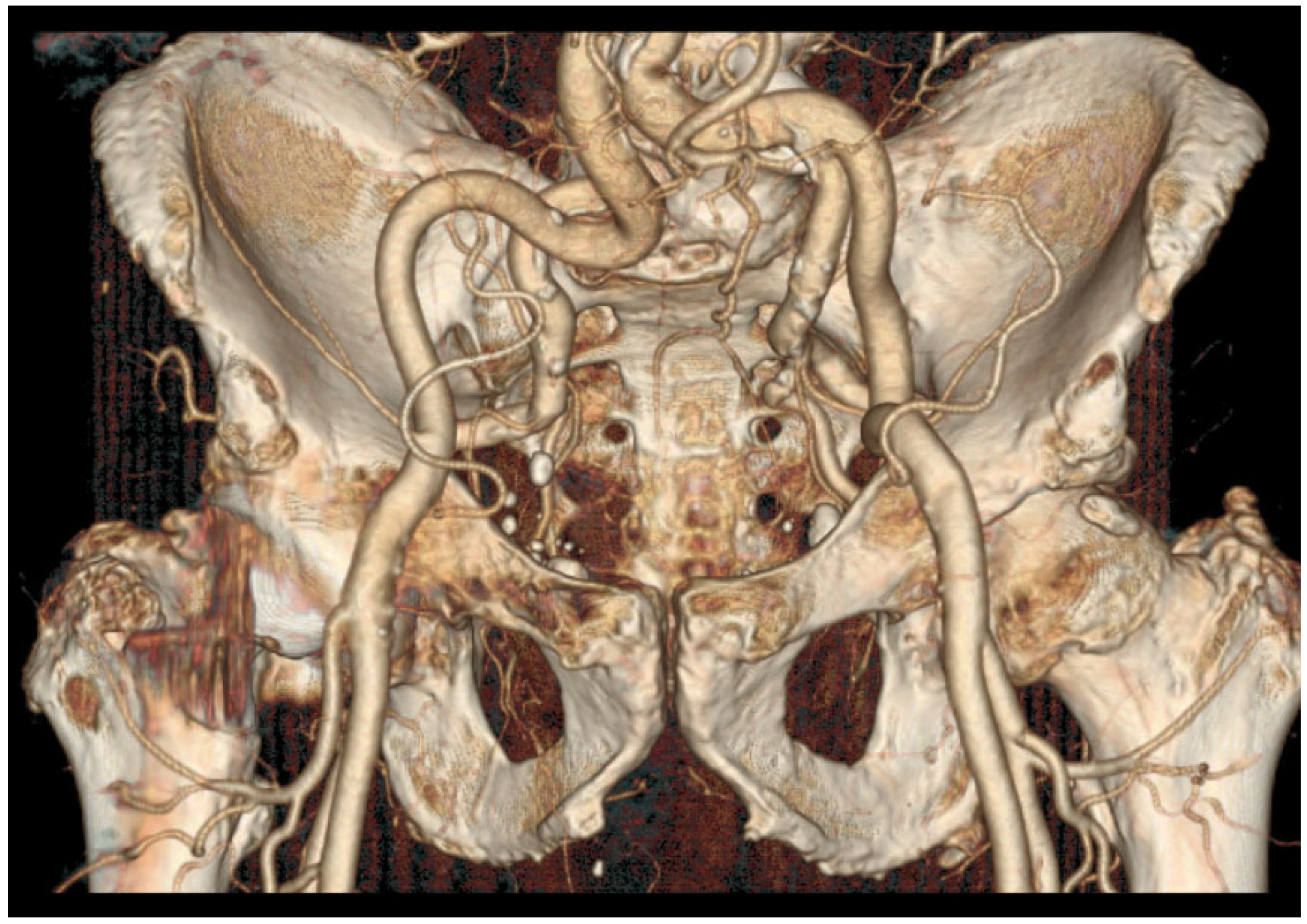
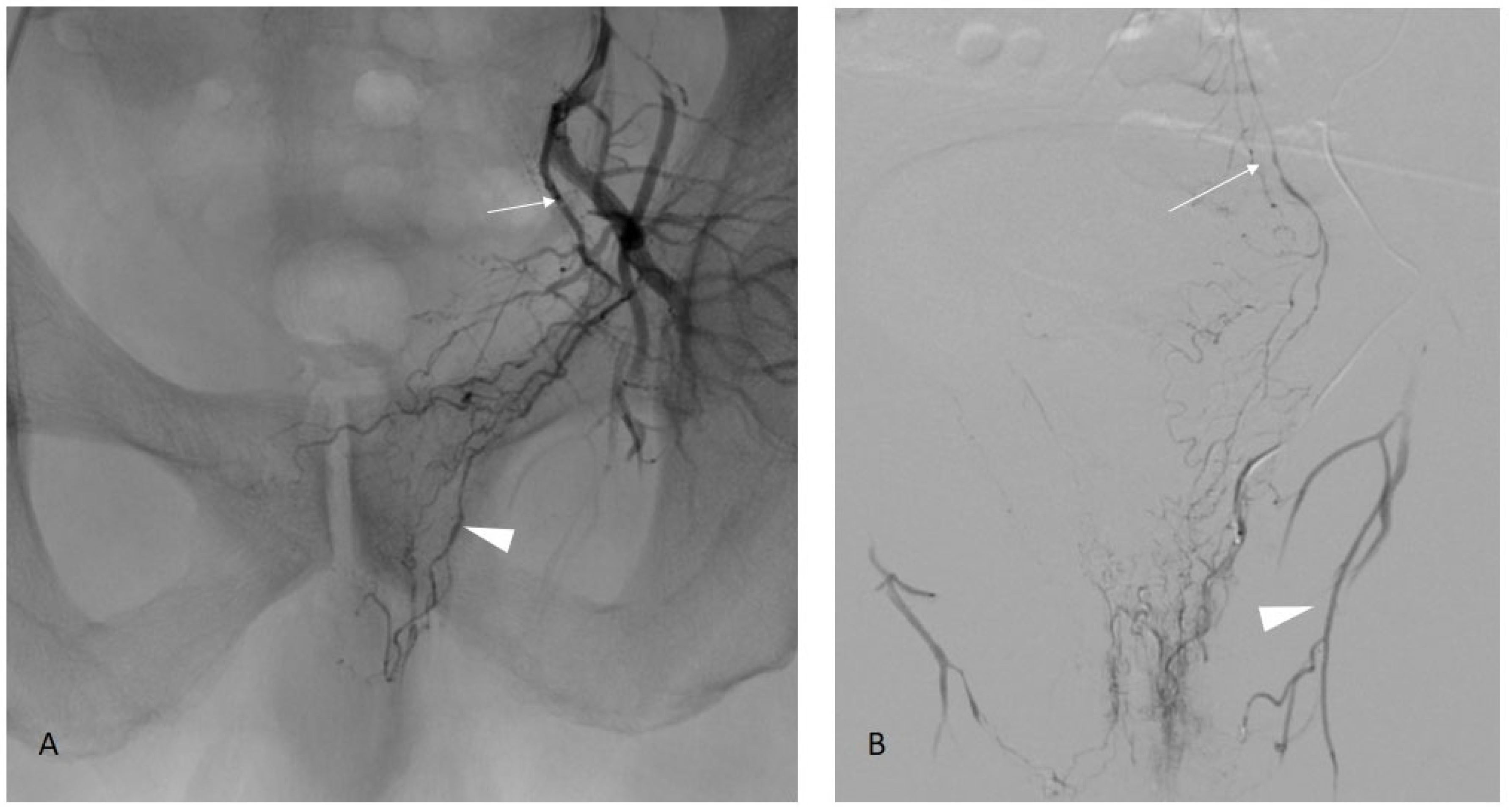
2.2. Manage Aortoiliac Anatomy
- Tortuous common iliac arteries (Figure 1);
- Aortic or iliac bifurcation forming a very acute angle.
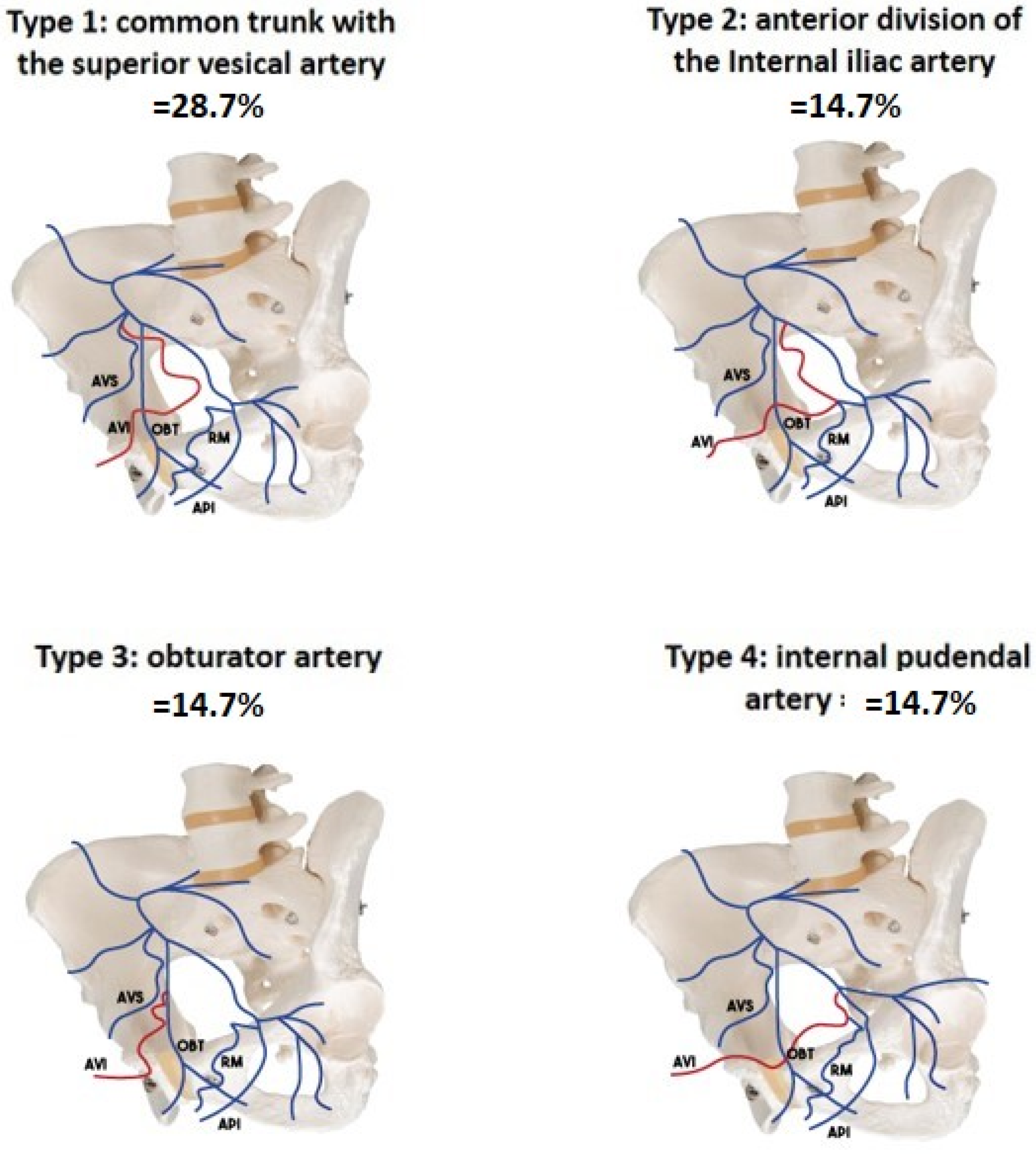
2.3. Identify the Origin of the Prostatic Artery
2.4. Manage the Prostatic Artery Catheterism
- -
- Atheroma and sinuous arteries (increasing with age);
- -
- Type 1 prostatic artery, with tight angulation between the anterior trunk of the internal iliac and the inferior bladder artery (this situation also sometimes occurs with the internal pudendal artery on type 4).
2.4.1. When the Internal Iliac Arteries Are Tortuous or When the Catheter Is Unstable
- -
- with the use of a longer sheath (45 centimeters for example), when a femoral approach is intended;
- -
- with the “buddy-wire technic” [9]: the use of an increased sheath caliber (7 french) and the positioning of a guidewire parallel to the catheter, to increase the stability of this one;
- -
- and with a radial approach [10], which can be considered to overcome the loss of stability inherent in the cross-over.
2.4.2. When the Prostatic Artery Arises with a Very Acute Angulation
- -
- Use a rigid torque catheter with a tight distal curve to directly catheterize the artery without a microcatheter. This type of catheter should be handled with care, as it is very rigid and can easily lead to dissection of the prostatic artery.
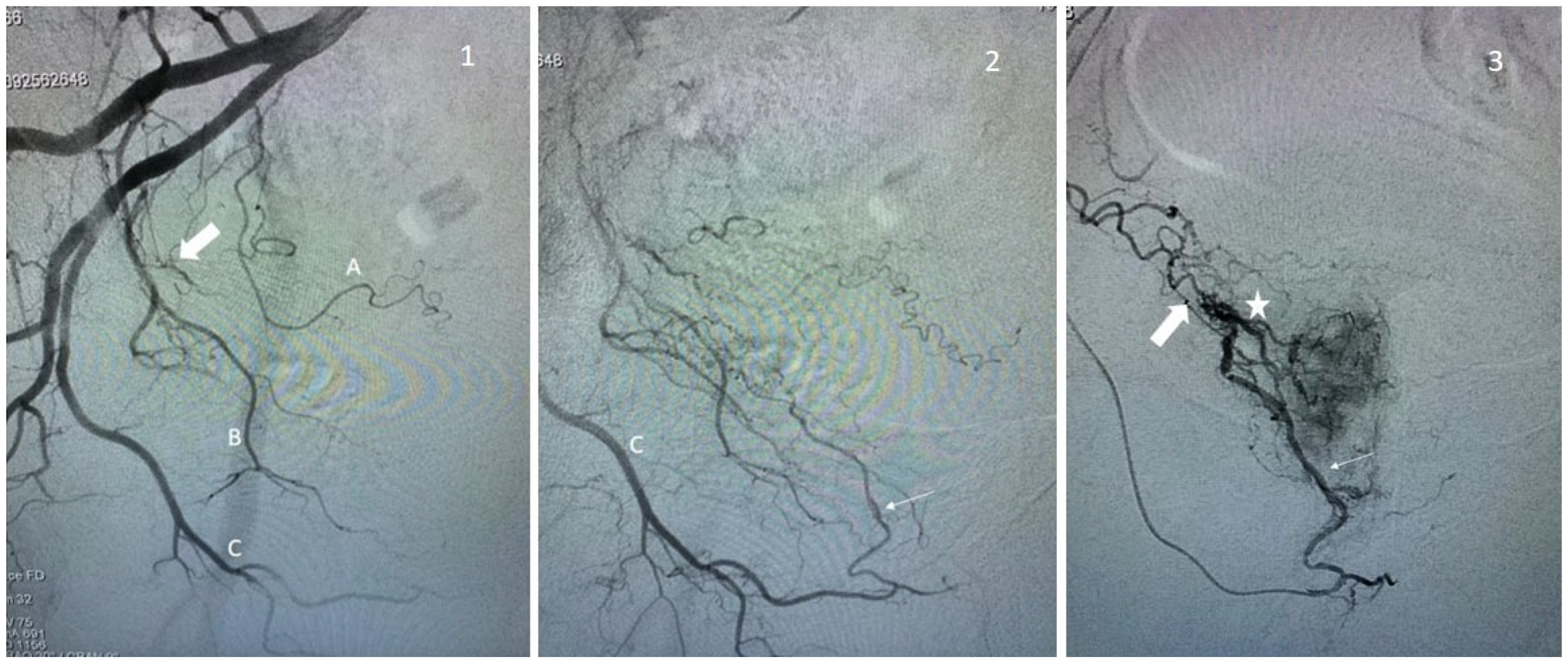
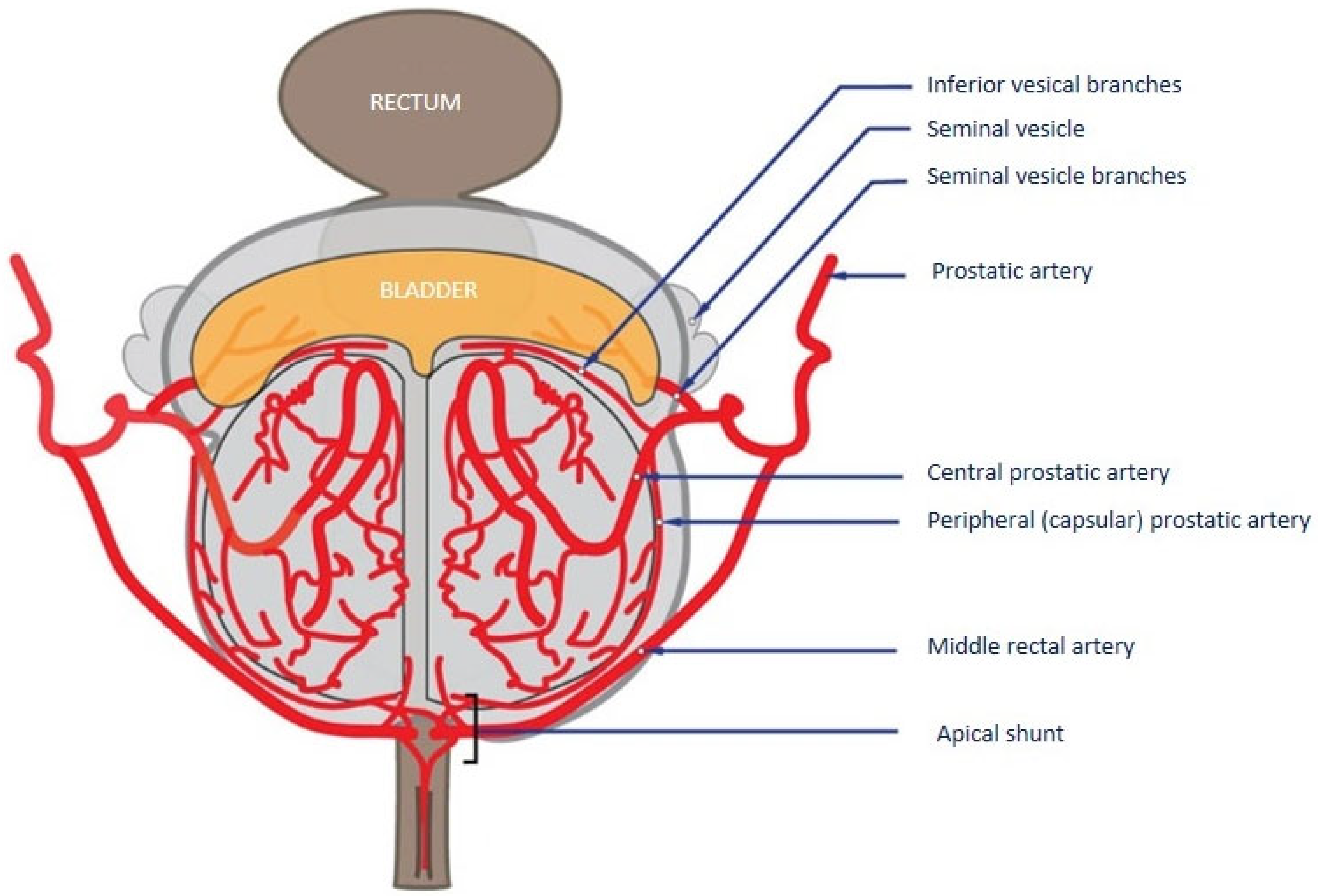
2.5. Know the Intra-Prostatic Anatomy, Detect and Protect the Shunt and Collaterals
2.5.1. Middle Rectal and Inferior Vesical Collaterals
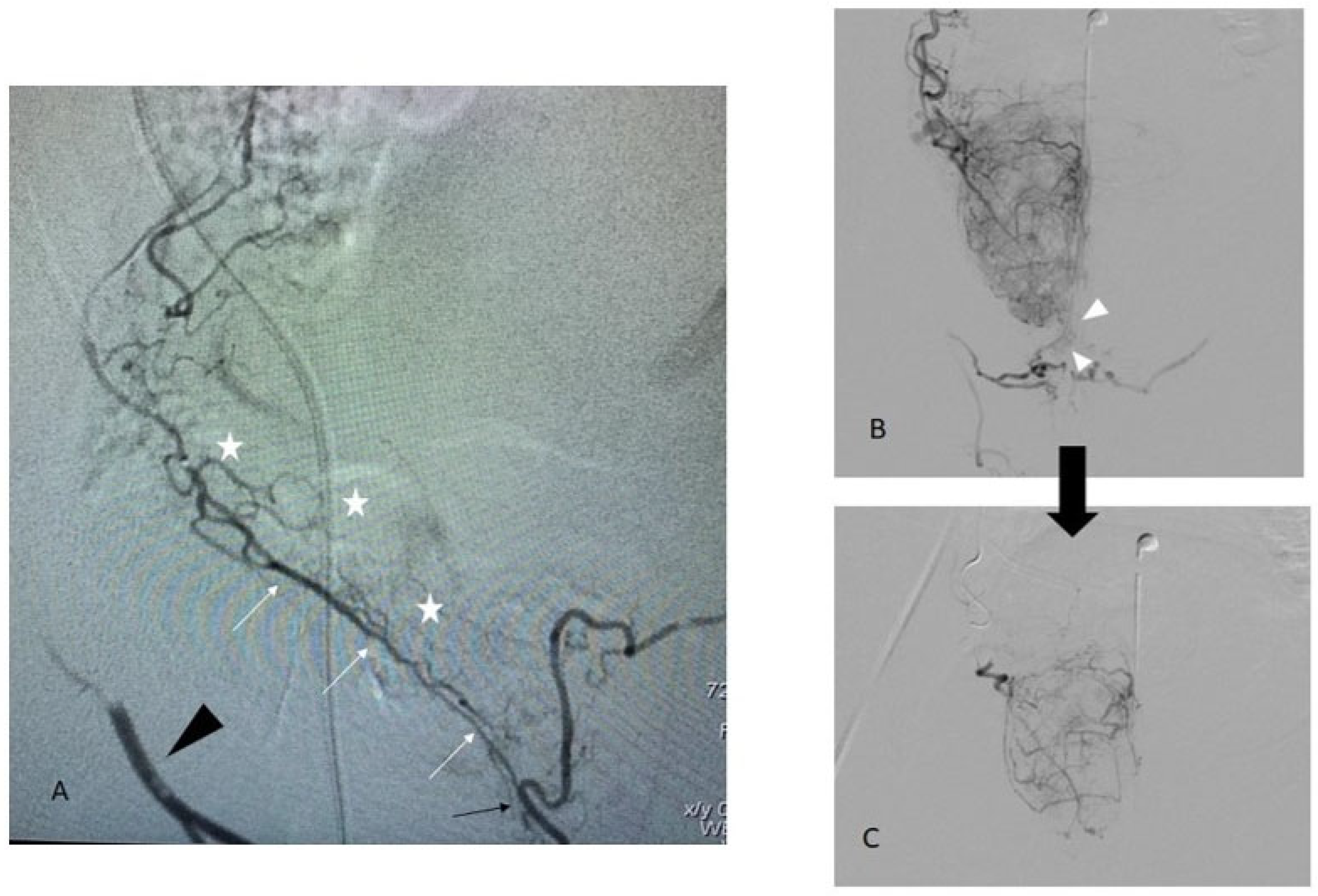
2.5.2. Internal Pudendal Artery Collateral
- -
- The post-capsular collaterals, which are usually found at the apex, are opacified during DSA with a flow rate usually superior to 0.5 cc/s. These collaterals disappear with the decrease in the injection rate. In these cases, embolization can be performed without risk but must be performed at a low flow rate;
- -
- The pre-capsular collaterals, which are true intra-prostatic arterial connections (usually described as the “accessory pudendal artery” (aPA)). In some extreme situations, there is no real prostatic artery, and the prostate is vascularized by several small branches along the latero-prostatic course of the aPA, which then gives the penile vascularization. As soon as the connections with the internal pudendal artery are of a certain size (we can consider that the visibility of a true course in angiography is a good cut-off) there is a significant risk of non-target embolization, including with low-flow embolization. These connections must, therefore, be protected prior to embolization.
- -
- First case: the central prostatic branches can be supraselectively catheterized. In this case, a very careful embolization can be performed. Most attention must be paid to avoid reflux into the aPA.
- -
- Second case: a supraselective catheterization is impossible. It is then necessary to occlude the accessory pudendal artery in its post-prostatic portion to be able to embolize upstream “by collaterality” of the prostatic branches. Nevertheless, the consequences of the occlusion of the aPA on penile vascularization must be taken into account. A recent study found no difference between a patient who received embolization of penile collateral in terms of erectile function [14]. These are still debated, despite numerous studies on the subject in the context of radical prostate surgeries for prostate cancer. These anatomical studies classified penile vascularization according to three categories [15] depending on whether the vascularization is performed only by the internal pudendal (type I, 61.9%), by the internal and accessory pudendal (type II, 32.8%), or only via the accessory pudendal arteries (type III, 5.4%). Put another way, this means that when an aPA is founded, it is the only supply to the penile in 14% of the case (type III/(type II + III)). By cross-referencing these data with MacLean [14], who reported around 12% of penile/aPA protection coiling during PAE, we arrived at a number of 1.7% (12% × 14%) of patients who are potentially at risk of protective occlusion of a type III vascularization. We, therefore, recommend before occluding an aPA to ensure that it is not the only artery supplying the penis, in which case the risk of post-occlusion impotence seems real to us. In our experience, the presence of selectively non-catheterizable prostatic branches in the context of type III penile vascularization in young subjects wishing to preserve their sexual activity is the only situation contraindicating embolization.
3. Perspective, Evolution, and Discussion about PAE
3.1. PAE Safety and Complications
3.2. PAE Limitations
3.3. Embolization Agent
3.4. Particle Size
3.5. Peripheral vs. Central Prostate
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Berry, S.J.; Coffey, D.S.; Walsh, P.C.; Ewing, L.L. The Development of Human Benign Prostatic Hyperplasia with Age. J. Urol. 1984, 132, 474–479. [Google Scholar] [CrossRef] [PubMed]
- Ahyai, S.A.; Gilling, P.; Kaplan, S.A.; Kuntz, R.M.; Madersbacher, S.; Montorsi, F.; Speakman, M.J.; Stief, C.G. Meta-analysis of Functional Outcomes and Complications Following Transurethral Procedures for Lower Urinary Tract Symptoms Resulting from Benign Prostatic Enlargement. Eur. Urol. 2010, 58, 384–397. [Google Scholar] [CrossRef] [PubMed]
- Reich, O.; Gratzke, C.; Bachmann, A.; Seitz, M.; Schlenker, B.; Hermanek, P.; Lack, N.; Stief, C.G. Urology Section of the Bavarian Working Group for Quality Assurance† Morbidity, Mortality and Early Outcome of Transurethral Resection of the Prostate: A Prospective Multicenter Evaluation of 10,654 Patients. J. Urol. 2008, 180, 246–249. [Google Scholar] [CrossRef] [PubMed]
- Cornelis, F.H.; Bilhim, T.; Hacking, N.; Sapoval, M.; Tapping, C.R.; Carnevale, F.C. CIRSE Standards of Practice on Prostatic Artery Embolisation. Cardiovasc. Intervent. Radiol. 2020, 43, 176–185. [Google Scholar] [CrossRef] [PubMed]
- Malde, S.; Umbach, R.; Wheeler, J.R.; Lytvyn, L.; Cornu, J.-N.; Gacci, M.; Gratzke, C.; Herrmann, T.R.W.; Mamoulakis, C.; Rieken, M.; et al. A Systematic Review of Patients’ Values, Preferences, and Expectations for the Diagnosis and Treatment of Male Lower Urinary Tract Symptoms. Eur. Urol. 2021, 79, 796–809. [Google Scholar] [CrossRef]
- de Assis, A.M.; Moreira, A.M.; de Paula Rodrigues, V.C.; Harward, S.H.; Antunes, A.A.; Srougi, M.; Carnevale, F.C. Pelvic Arterial Anatomy Relevant to Prostatic Artery Embolisation and Proposal for Angiographic Classification. Cardiovasc. Intervent. Radiol. 2015, 38, 855–861. [Google Scholar] [CrossRef]
- Bilhim, T.; Pisco, J.; Pinheiro, L.C.; Rio Tinto, H.; Fernandes, L.; Pereira, J.A. The Role of Accessory Obturator Arteries in Prostatic Arterial Embolization. J. Vasc. Interv. Radiol. 2014, 25, 875–879. [Google Scholar] [CrossRef]
- du Pisanie, J.; Abumoussa, A.; Donovan, K.; Stewart, J.; Bagla, S.; Isaacson, A. Predictors of Prostatic Artery Embolization Technical Outcomes: Patient and Procedural Factors. J. Vasc. Interv. Radiol. 2019, 30, 233–240. [Google Scholar] [CrossRef]
- Bagla, S.; Isaacson, A.J. Tips and Tricks for Difficult Prostatic Artery Embolization. Semin. Interv. Radiol. 2016, 33, 236–239. [Google Scholar] [CrossRef][Green Version]
- Bhatia, S.; Harward, S.H.; Sinha, V.K.; Narayanan, G. Prostate Artery Embolization via Transradial or Transulnar versus Transfemoral Arterial Access: Technical Results. J. Vasc. Interv. Radiol. 2017, 28, 898–905. [Google Scholar] [CrossRef]
- Dudeck, O. Safety and Efficacy of Target Vessel Catheterization with the New Steerable Microcatheter Direxion Compared with a Standard Microcatheter: A Prospective, Preclinical Trial. Cardiovasc. Intervent. Radiol. 2014, 37, 1041–1046. [Google Scholar] [CrossRef]
- Picel, A.C.; Hsieh, T.-C.; Shapiro, R.M.; Vezeridis, A.M.; Isaacson, A.J. Prostatic Artery Embolization for Benign Prostatic Hyperplasia: Patient Evaluation, Anatomy, and Technique for Successful Treatment. RadioGraphics 2019, 39, 1526–1548. [Google Scholar] [CrossRef]
- Bilhim, T.; Pisco, J.M.; Rio Tinto, H.; Fernandes, L.; Pinheiro, L.C.; Furtado, A.; Casal, D.; Duarte, M.; Pereira, J.; Oliveira, A.G.; et al. Prostatic Arterial Supply: Anatomic and Imaging Findings Relevant for Selective Arterial Embolization. J. Vasc. Interv. Radiol. 2012, 23, 1403–1415. [Google Scholar] [CrossRef]
- Maclean, D.; Vigneswaran, G.; Maher, B.; Hadi, M.; Harding, J.; Harris, M.; Bryant, T.; Hacking, N.; Modi, S. The effect of protective coil embolization of penile anastomoses during prostatic artery embolization on erectile function: A propensity-matched analysis. J. Vasc. Interv. Radiol. 2022, 33, S1051044322012787. [Google Scholar] [CrossRef]
- Henry, B.M.; Pękala, P.A.; Vikse, J.; Sanna, B.; Skinningsrud, B.; Saganiak, K.; Walocha, J.A.; Tomaszewski, K.A. Variations in the Arterial Blood Supply to the Penis and the Accessory Pudendal Artery: A Meta-Analysis and Review of Implications in Radical Prostatectomy. J. Urol. 2017, 198, 345–353. [Google Scholar] [CrossRef]
- Abt, D.; Hechelhammer, L.; Müllhaupt, G.; Markart, S.; Güsewell, S.; Kessler, T.M.; Schmid, H.-P.; Engeler, D.S.; Mordasini, L. Comparison of prostatic artery embolisation (PAE) versus transurethral resection of the prostate (TURP) for benign prostatic hyperplasia: Randomised, open label, non-inferiority trial. BMJ 2018, 361, k2338. [Google Scholar] [CrossRef]
- Carnevale, F.C.; Iscaife, A.; Yoshinaga, E.M.; Moreira, A.M.; Antunes, A.A.; Srougi, M. Transurethral Resection of the Prostate (TURP) Versus Original and PErFecTED Prostate Artery Embolization (PAE) Due to Benign Prostatic Hyperplasia (BPH): Preliminary Results of a Single Center, Prospective, Urodynamic-Controlled Analysis. Cardiovasc. Intervent. Radiol. 2016, 39, 44–52. [Google Scholar] [CrossRef]
- Insausti, I.; Sáez de Ocáriz, A.; Galbete, A.; Capdevila, F.; Solchaga, S.; Giral, P.; Bilhim, T.; Isaacson, A.; Urtasun, F.; Napal, S. Randomized Comparison of Prostatic Artery Embolization versus Transurethral Resection of the Prostate for Treatment of Benign Prostatic Hyperplasia. J. Vasc. Interv. Radiol. 2020, 31, 882–890. [Google Scholar] [CrossRef]
- Pisco, J.M.; Bilhim, T.; Costa, N.V.; Torres, D.; Pisco, J.; Pinheiro, L.C.; Oliveira, A.G. Randomised Clinical Trial of Prostatic Artery Embolisation Versus a Sham Procedure for Benign Prostatic Hyperplasia. Eur. Urol. 2020, 77, 354–362. [Google Scholar] [CrossRef]
- Ray, A.F.; Powell, J.; Speakman, M.J.; Longford, N.T.; DasGupta, R.; Bryant, T.; Modi, S.; Dyer, J.; Harris, M.; Carolan-Rees, G.; et al. Efficacy and safety of prostate artery embolization for benign prostatic hyperplasia: An observational study and propensity-matched comparison with transurethral resection of the prostate (the UK-ROPE study). BJU Int. 2018, 122, 270–282. [Google Scholar] [CrossRef]
- Russo, G.I.; Kurbatov, D.; Sansalone, S.; Lepetukhin, A.; Dubsky, S.; Sitkin, I.; Salamone, C.; Fiorino, L.; Rozhivanov, R.; Cimino, S.; et al. Prostatic Arterial Embolization vs Open Prostatectomy: A 1-Year Matched-pair Analysis of Functional Outcomes and Morbidities. Urology 2015, 86, 343–348. [Google Scholar] [CrossRef] [PubMed]
- Salem, R.; Hairston, J.; Hohlastos, E.; Riaz, A.; Kallini, J.; Gabr, A.; Ali, R.; Jenkins, K.; Karp, J.; Desai, K.; et al. Prostate Artery Embolization for Lower Urinary Tract Symptoms Secondary to Benign Prostatic Hyperplasia: Results From a Prospective FDA-Approved Investigational Device Exemption Study. Urology 2018, 120, 205–210. [Google Scholar] [CrossRef] [PubMed]
- Knight, G.M.; Talwar, A.; Salem, R.; Mouli, S. Systematic Review and Meta-analysis Comparing Prostatic Artery Embolization to Gold-Standard Transurethral Resection of the Prostate for Benign Prostatic Hyperplasia. Cardiovasc. Intervent. Radiol. 2021, 44, 183–193. [Google Scholar] [CrossRef] [PubMed]
- Bilhim, T.; Costa, N.V.; Torres, D.; Pinheiro, L.C.; Spaepen, E. Long-Term Outcome of Prostatic Artery Embolization for Patients with Benign Prostatic Hyperplasia: Single-Centre Retrospective Study in 1072 Patients Over a 10-Year Period. Cardiovasc. Intervent. Radiol. 2022, 45, 1324–1336. [Google Scholar] [CrossRef] [PubMed]
- Moulin, B.; Hakime, A.; Kuoch, V. Percutaneous Prostatic Artery Embolization with Absolute Alcohol: A Case Report. J. Vasc. Interv. Radiol. 2022, 33, 1008–1010. [Google Scholar] [CrossRef] [PubMed]
- Chau, Y.; Rambaud-Collet, C.; Durand, M.; Léna, P.; Raffaelli, C.; Brunner, P.; Quintens, H.; Sédat, J. Prostatic Artery Embolization with Ethylene Vinyl Alcohol Copolymer: A 3-Patient Series. J. Vasc. Interv. Radiol. 2018, 29, 1333–1336. [Google Scholar] [CrossRef]
- Salet, E.; Crombé, A.; Grenier, N.; Marcelin, C.; Lebras, Y.; Jambon, E.; Coussy, A.; Cornelis, F.H.; Petitpierre, F. Prostatic Artery Embolization for Benign Prostatic Obstruction: Single-Centre Retrospective Study Comparing Microspheres Versus n-Butyl Cyanoacrylate. Cardiovasc. Intervent. Radiol. 2022, 45, 814–823. [Google Scholar] [CrossRef]
- Torres, D.; Costa, N.V.; Pisco, J.; Pinheiro, L.C.; Oliveira, A.G.; Bilhim, T. Prostatic Artery Embolization for Benign Prostatic Hyperplasia: Prospective Randomized Trial of 100–300 μm versus 300–500 μm versus 100- to 300-μm + 300- to 500-μm Embospheres. J. Vasc. Interv. Radiol. 2019, 30, 638–644. [Google Scholar] [CrossRef]
- Wang, M.Q.; Zhang, J.L.; Xin, H.N.; Yuan, K.; Yan, J.; Wang, Y.; Zhang, G.D.; Fu, J.X. Comparison of Clinical Outcomes of Prostatic Artery Embolization with 50-μm Plus 100-μm Polyvinyl Alcohol (PVA) Particles versus 100-μm PVA Particles Alone: A Prospective Randomized Trial. J. Vasc. Interv. Radiol. 2018, 29, 1694–1702. [Google Scholar] [CrossRef]
- Anract, J.; Amouyal, G.; Peyromaure, M.; Zerbib, M.; Sapoval, M.; Barry Delongchamps, N. Study of the intra-prostatic arterial anatomy and implications for arterial embolization of benign prostatic hyperplasia. Prog. Urol. 2019, 29, 263–269. [Google Scholar] [CrossRef]
| Study | Pisco, 2019 [19] | Insauti, 2020 [18] | Abt, 2018 [16] | Carnevale, 2015 [17] | Russo, 2015 [21] | Ray, 2018 [20] | Salem, 2018 [22] |
|---|---|---|---|---|---|---|---|
| Patient Number | n = 78 | n = 23 | n = 48 | n = 15 | n = 80 | n = 199 | n = 45 |
| Design | RCT, PAE vs. Sham | RCT, PAE vs. TURP | RCT, PAE vs. TURP | RCT, PAE vs. TURP | RCT, PAE vs. prostatectomy | Registry-based study | Prospective, PAE only |
| Total adverse event, n (%) | 25 (32.0) | 15 (65.2) | 36 (75) | 4 (46.7) | 7 (8.7) | 136 (68.3) | 26 (57.8) |
| Clavien Dindo grade | |||||||
| grade I | 21 (26.9) | 4 (17.3) | 54% | 6 (7.5) | 134 (67.3) | 24 (53.3) | |
| grade II | 3 (3.8) | 11 (47.8) | 17% | 1 (1.3) | 2 (1) | 2 (4.4) | |
| grade III | 1 (1.3) | 0 | 4.30% | 0 | 0 | ||
| grade IV | 0 | 0 | 0 | 0 | |||
| grade V | 0 | 0 | 0 | 0 | |||
| Description (number, %) | |||||||
| Urinary frequency and urgency | 3 (6.6) | ||||||
| Burning perineal pain | 1 (1.3) | 1 (4.3) | 15 (31.3) | ||||
| Burning urethral pain | 3 (3.8) | 4 (17.3) | |||||
| Dysuria | 3 (3.8) | 5 (6.3) | 13 (28.9) | ||||
| Ecchymosis | 2 (2.6) | ||||||
| Haematospermia | 7 (9.0) | 1 (6.7) | 1 (1.3) | 25 (12.6) | 2 (4.4) | ||
| Haematuria | 5 (6.4) | 1 (4.3) | 4 (8.3) | 2 (13.3) | 37 (18.6) | 6 (13.3) | |
| Inguinal haematoma | 4 (5.1) | 4 (2) | |||||
| Penile ulcer | 2 (1) | ||||||
| Artery dissection | 4 (2.0) | ||||||
| Acute urinary retention | 5 (21.7) | 1 (2.1) | 2 (4.4) | ||||
| Radiodermitis | 1 (4.3) | ||||||
| Erectile dysfunction | 1 (4.3) | ||||||
| Change in ejaculation volume | 1 (4.3) | 2 (13.3) | 48 (24.1) | ||||
| Incontinence | 2 (1) | ||||||
| Prostate fragment expelled | 1 (1.3) | ||||||
| Rectorrhagia/rectal ischemia | 2 (2.6) | 1 (4.3) | 1 (6.7) | ||||
| Urinary tract infection | 1 (1.3) | 10 (20.1) | 1 (1.3) | 14 (7.0) | |||
| Other | 6 (12.5) | 1 (6.7) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Moulin, B.; Di Primio, M.; Vignaux, O.; Sarrazin, J.L.; Angelopoulos, G.; Hakime, A. Prostate Artery Embolization: Challenges, Tips, Tricks, and Perspectives. J. Pers. Med. 2023, 13, 87. https://doi.org/10.3390/jpm13010087
Moulin B, Di Primio M, Vignaux O, Sarrazin JL, Angelopoulos G, Hakime A. Prostate Artery Embolization: Challenges, Tips, Tricks, and Perspectives. Journal of Personalized Medicine. 2023; 13(1):87. https://doi.org/10.3390/jpm13010087
Chicago/Turabian StyleMoulin, Benjamin, Massimiliano Di Primio, Olivier Vignaux, Jean Luc Sarrazin, Georgios Angelopoulos, and Antoine Hakime. 2023. "Prostate Artery Embolization: Challenges, Tips, Tricks, and Perspectives" Journal of Personalized Medicine 13, no. 1: 87. https://doi.org/10.3390/jpm13010087
APA StyleMoulin, B., Di Primio, M., Vignaux, O., Sarrazin, J. L., Angelopoulos, G., & Hakime, A. (2023). Prostate Artery Embolization: Challenges, Tips, Tricks, and Perspectives. Journal of Personalized Medicine, 13(1), 87. https://doi.org/10.3390/jpm13010087







