Effectiveness of Augmented and Virtual Reality-Based Interventions in Improving Knowledge, Attitudes, Empathy and Stigma Regarding People with Mental Illnesses—A Scoping Review
Abstract
1. Introduction
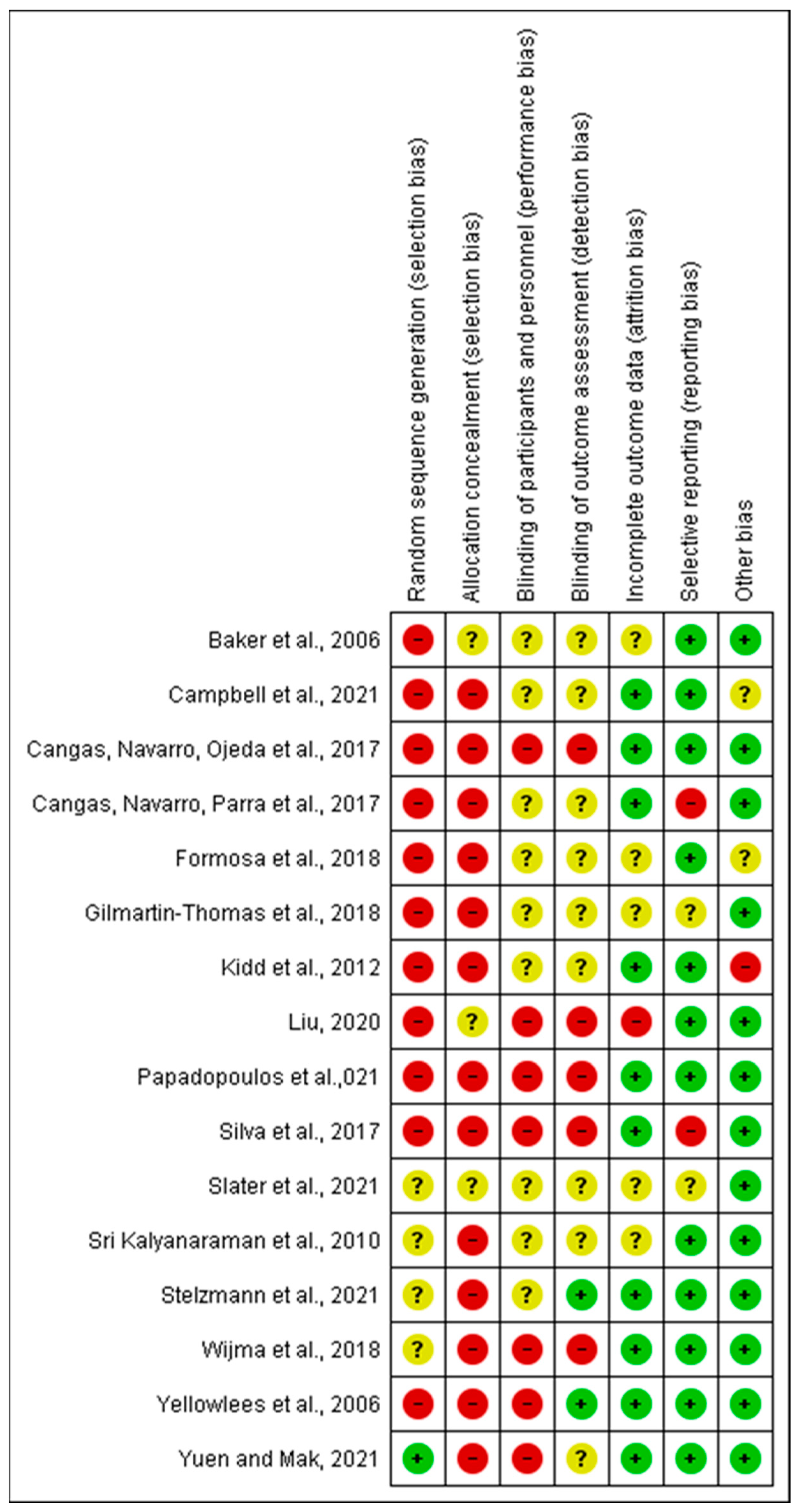
2. Methodology
3. Results
3.1. Description of Studies
3.2. Knowledge about Mental Illnesses
3.3. Attitudes toward People with Mental Illnesses
3.4. Empathy
3.5. Stigma Regarding People with Mental Illnesses
4. Discussion
4.1. Knowledge about Mental Illnesses
4.2. Attitude towards People with Mental Illnesses
4.3. Empathy
4.4. Stigma
5. Limitations and Future Research Directions
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A
References
- Dattani, S.; Ritchie, H.; Roser, M. Mental Health. Available online: https://ourworldindata.org/mental-health (accessed on 18 November 2021).
- GBD Mental Disorders Collaborators. Global, regional, and national burden of 12 mental disorders in 204 countries and territories, 1990–2019: A systematic analysis for the Global Burden of Disease Study 2019. Lancet Psychiatry 2022, 9, 137–150. [Google Scholar] [CrossRef]
- Pescosolido, B.A.; Jensen, P.S.; Martin, J.K.; Perry, B.L.; Olafsdottir, S.; Fettes, D. Public knowledge and assessment of child mental health problems: Findings from the National Stigma Study-Children. J. Am. Acad. Child Adolesc. Psychiatry 2008, 47, 339–349. [Google Scholar] [CrossRef]
- Furnham, A.; Swami, V. Mental health literacy: A review of what it is and why it matters. Int. Perspect. Psychol. 2018, 7, 240–257. [Google Scholar] [CrossRef]
- Jorm, A.F.; Korten, A.E.; Jacomb, P.A.; Christensen, H.; Rodgers, B.; Pollitt, P. “Mental health literacy”: A survey of the public’s ability to recognise mental disorders and their beliefs about the effectiveness of treatment. Med. J. Aust. 1997, 166, 182–186. [Google Scholar] [CrossRef] [PubMed]
- Cheng, H.L.; Wang, C.; McDermott, R.C.; Kridel, M.; Rislin, J.L. Self-stigma, mental health literacy, and attitudes toward seeking psychological help. J. Couns. Dev. 2018, 96, 64–74. [Google Scholar] [CrossRef]
- Tay, J.L.; Tay, Y.F.; Klainin-Yobas, P. Effectiveness of information and communication technologies interventions to increase mental health literacy: A systematic review. Early Interv. Psychiatry 2018, 12, 1024–1037. [Google Scholar] [CrossRef]
- Błądziński, P.; Kalisz, A.; Adamczyk, P.; Arciszewska, A.; Mętel, D.; Daren, A.; Cechnicki, A. Associations of insight and treatment adherence with employment status of people with schizophrenia. Postępy Psychiatrii Neurologii Adv. Psychiatry Neurol. 2019, 28, 21–33. [Google Scholar] [CrossRef]
- Garcia-Cabeza, I.; Victor, F.; de Portugal, E. Relationship between insight, adherence and disability in the diagnose of paranoid schizophrenia. J. Ment. Health Clin. Psychol. 2018, 2, 6–10. [Google Scholar] [CrossRef]
- Novick, D.; Montgomery, W.; Treuer, T.; Aguado, J.; Kraemer, S.; Haro, J.M. Relationship of insight with medication adherence and the impact on outcomes in patients with schizophrenia and bipolar disorder: Results from a 1-year European outpatient observational study. BMC Psychiatry 2015, 15, 1–8. [Google Scholar] [CrossRef]
- Moudatsou, M.; Stavropoulou, A.; Philalithis, A.; Koukouli, S. The role of empathy in health and social care professionals. Healthcare 2020, 8, 26. [Google Scholar] [CrossRef]
- Hecht, M.; Kloß, A.; Bartsch, A. Stopping the Stigma. How Empathy and Reflectiveness Can Help Reduce Mental Health Stigma. Media Psychol. 2021, 25, 367–386. [Google Scholar] [CrossRef]
- Henderson, C.; Gronholm, P.C. Mental health related stigma as a ‘wicked problem’: The need to address stigma and consider the consequences. Int. J. Environ. Res. Public Health 2018, 15, 1158. [Google Scholar] [CrossRef] [PubMed]
- Squire, K.; Klopfer, E. Augmented reality simulations on handheld computers. J. Learn. Sci. 2007, 16, 371–413. [Google Scholar] [CrossRef]
- Chong, Y.; Sethi, D.K.; Loh, C.H.Y.; Lateef, F. Going forward with pokemon go. J. Emergencies Trauma Shock 2018, 11, 243. [Google Scholar]
- Lee, E.A.-L.; Wong, K.W.; Fung, C.C. How does desktop virtual reality enhance learning outcomes? A structural equation modeling approach. Comput. Educ. 2010, 55, 1424–1442. [Google Scholar]
- Wu, Y.; Zhang, M.; Li, X.; Gan, Y.; Zhao, C. Augment Reality-Based Teaching Practice. Biomed. Eng. Educ. 2021, 1, 237–241. [Google Scholar] [CrossRef] [PubMed]
- Hamilton, D.; McKechnie, J.; Edgerton, E.; Wilson, C. Immersive virtual reality as a pedagogical tool in education: A systematic literature review of quantitative learning outcomes and experimental design. J. Comput. Educ. 2021, 8, 1–32. [Google Scholar] [CrossRef]
- Rizzo, A.S. Clinical virtual reality in mental health and rehabilitation: A brief review of the future! In Proceedings of the SPIE 11002, Infrared Technology and Applications XLV 2019, Baltimore, MD, USA, 14–18 April 2019; pp. 150–158. [Google Scholar]
- Almurashi, H.; Bouaziz, R.; Alharthi, W.; Al-Sarem, M.; Hadwan, M.; Kammoun, S. Augmented reality, serious games and picture exchange communication system for people with ASD: Systematic literature review and future directions. Sensors 2022, 22, 1250. [Google Scholar] [CrossRef]
- Barba, M.C.; Covino, A.; De Luca, V.; De Paolis, L.T.; D’Errico, G.; Di Bitonto, P.; Di Gestore, S.; Magliaro, S.; Nunnari, F.; Paladini, G.I. BRAVO: A gaming environment for the treatment of ADHD. In Proceedings of the International Conference on Augmented Reality, Virtual Reality and Computer Graphics, Santa Maria al Bagno, Italy, 24–27 June 2019; pp. 394–407. [Google Scholar]
- Goharinejad, S.; Goharinejad, S.; Hajesmaeel-Gohari, S.; Bahaadinbeigy, K. The usefulness of virtual, augmented, and mixed reality technologies in the diagnosis and treatment of attention deficit hyperactivity disorder in children: An overview of relevant studies. BMC Psychiatry 2022, 22, 1–13. [Google Scholar] [CrossRef]
- Karami, B.; Koushki, R.; Arabgol, F.; Rahmani, M.; Vahabie, A.-H. Effectiveness of Virtual/Augmented Reality-based therapeutic interventions on individuals with autism spectrum disorder: A comprehensive meta-analysis. Front. Psychiatry 2021, 12, 887. [Google Scholar] [CrossRef]
- Albakri, G.; Bouaziz, R.; Alharthi, W.; Kammoun, S.; Al-Sarem, M.; Saeed, F.; Hadwan, M. Phobia Exposure Therapy Using Virtual and Augmented Reality: A Systematic Review. Appl. Sci. 2022, 12, 1672. [Google Scholar] [CrossRef]
- Caponnetto, P.; Triscari, S.; Maglia, M.; Quattropani, M.C. The Simulation Game—Virtual Reality Therapy for the Treatment of Social Anxiety Disorder: A Systematic Review. Int. J. Environ. Res. Public Health 2021, 18, 13209. [Google Scholar] [CrossRef]
- Hinze, J.; Röder, A.; Menzie, N.; Müller, U.; Domschke, K.; Riemenschneider, M.; Noll-Hussong, M. Spider Phobia: Neural Networks Informing Diagnosis and (Virtual/Augmented Reality-Based) Cognitive Behavioral Psychotherapy—A Narrative Review. Front. Psychiatry 2021, 12, 704174. [Google Scholar] [CrossRef]
- Ma, L.; Mor, S.; Anderson, P.L.; Baños, R.M.; Botella, C.; Bouchard, S.; Cárdenas-López, G.; Donker, T.; Fernández-Álvarez, J.; Lindner, P. Integrating virtual realities and psychotherapy: SWOT analysis on VR and MR based treatments of anxiety and stress-related disorders. Cogn. Behav. Ther. 2021, 50, 509–526. [Google Scholar] [CrossRef]
- Cullen, A.J.; Dowling, N.L.; Segrave, R.; Carter, A.; Yücel, M. Exposure therapy in a virtual environment: Validation in obsessive compulsive disorder. J. Anxiety Disord. 2021, 80, 102404. [Google Scholar] [CrossRef]
- Dehghan, B.; Saeidimehr, S.; Sayyah, M.; Rahim, F. The Effect of Virtual Reality on Emotional Response and Symptoms Provocation in Patients with OCD: A Systematic Review and Meta-Analysis. Front. Psychiatry 2021, 12, 733584. [Google Scholar] [CrossRef]
- García-Batista, Z.E.; Guerra-Peña, K.; Alsina-Jurnet, I.; Cano-Vindel, A.; Cantisano-Guzmán, L.M.; Nazir-Ferreiras, A.; Moretti, L.S.; Medrano, L.A.; Garrido, L.E. Design and Validation of Augmented Reality Stimuli for the Treatment of Cleaning Obsessive-Compulsive Disorder. Front. Psychol. 2021, 12, 618874. [Google Scholar] [CrossRef]
- Eshuis, L.; van Gelderen, M.; van Zuiden, M.; Nijdam, M.; Vermetten, E.; Olff, M.; Bakker, A. Efficacy of immersive PTSD treatments: A systematic review of virtual and augmented reality exposure therapy and a meta-analysis of virtual reality exposure therapy. J. Psychiatr. Res. 2021, 143, 516–527. [Google Scholar] [CrossRef]
- Georgiev, D.D.; Georgieva, I.; Gong, Z.; Nanjappan, V.; Georgiev, G.V. Virtual reality for neurorehabilitation and cognitive enhancement. Brain Sci. 2021, 11, 221. [Google Scholar] [CrossRef]
- Sejunaite, K.; Lanza, C.; Ganders, S.; Iljaitsch, A.; Riepe, M. Augmented reality: Sustaining autonomous way-finding in the community for older persons with cognitive impairment. J. Frailty Aging 2017, 6, 206–211. [Google Scholar] [CrossRef]
- Formosa, N.J.; Morrison, B.W.; Hill, G.; Stone, D. Testing the efficacy of a virtual reality-based simulation in enhancing users’ knowledge, attitudes, and empathy relating to psychosis. Aust. J. Psychol. 2018, 70, 57–65. [Google Scholar] [CrossRef]
- Gilmartin-Thomas, J.F.-M.; McNeil, J.; Powell, A.; Malone, D.T.; Wolfe, R.; Larson, I.C.; O’Reilly, C.L.; Kirkpatrick, C.M.; Kipen, E.; Petrovich, T. Impact of a virtual dementia experience on medical and pharmacy students’ knowledge and attitudes toward people with dementia: A controlled study. J. Alzheimer’s Dis. 2018, 62, 867–876. [Google Scholar] [CrossRef]
- Cangas, A.J.; Navarro, N.; Parra, J.; Ojeda, J.J.; Cangas, D.; Piedra, J.A.; Gallego, J. Stigma-Stop: A serious game against the stigma toward mental health in educational settings. Front. Psychol. 2017, 8, 1385. [Google Scholar] [CrossRef]
- Liu, J. VR-Assisted Curriculum on Depression for Stigma Reduction. Available online: https://clinicaltrials.gov/ct2/show/study/NCT03912597 (accessed on 8 November 2021).
- Peters, M.D.; Godfrey, C.M.; McInerney, P.; Soares, C.B.; Khalil, H.; Parker, D. The Joanna Briggs Institute Reviewers’ Manual 2015: Methodology for JBI Scoping Reviews. Available online: https://nursing.lsuhsc.edu/jbi/docs/reviewersmanuals/scoping-.pdf (accessed on 1 December 2021).
- Levac, D.; Colquhoun, H.; O’Brien, K.K. Scoping studies: Advancing the methodology. Implement. Sci. 2010, 5, 1–9. [Google Scholar] [CrossRef]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. Ann. Intern. Med. 2009, 151, 264–269. [Google Scholar] [CrossRef]
- Sri Kalyanaraman, S.; Penn, D.L.; Ivory, J.D.; Judge, A. The Virtual Doppelganger: Effects of a Virtual Reality Simulator on Perceptions of Schizophrenia. J. Nerv. Ment. Dis. 2010, 198, 437–443. [Google Scholar] [CrossRef]
- Stelzmann, D.; Toth, R.; Schieferdecker, D. Can intergroup contact in virtual reality (VR) reduce stigmatization against people with schizophrenia? J. Clin. Med. 2021, 10, 2961. [Google Scholar] [CrossRef]
- Yuen, A.S.; Mak, W.W. The effects of immersive virtual reality in reducing public stigma of mental illness in the university population of Hong Kong: Randomized controlled trial. J. Med. Internet Res. 2021, 23, e23683. [Google Scholar] [CrossRef]
- Kidd, L.I.; Knisley, S.J.; Morgan, K.I. Effectiveness of a Second Life® simulation as a teaching strategy for undergraduate mental health nursing students. J. Psychosoc. Nurs. Ment. Health Serv. 2012, 50, 28–37. [Google Scholar] [CrossRef]
- Liu, W. The Effects of Virtual Simulation on Undergraduate Nursing Students’ Mental Health Literacy: A Prospective Cohort Study. Issues Ment. Health Nurs. 2020, 42, 239–248. [Google Scholar] [CrossRef]
- Silva, R.D.D.C.; Albuquerque, S.G.; Muniz, A.D.V.; Ribeiro, S.; Pinheiro, P.R.; Albuquerque, V.H.C. Reducing the schizophrenia stigma: A new approach based on augmented reality. Comput. Intell. Neurosci. 2017, 2017, 2721846. [Google Scholar] [CrossRef]
- Campbell, D.; Lugger, S.; Sigler, G.S.; Turkelson, C. Increasing awareness, sensitivity, and empathy for Alzheimer’s dementia patients using simulation. Nurse Educ. Today 2021, 98, 104764. [Google Scholar] [CrossRef]
- Slater, P.; Hasson, F.; Moore, K.; Sharkey, F. Simulated Based Dementia Training: Impact on Empathic Understanding and Behaviour Among Professionals and Carers. Clin. Simul. Nurs. 2021, 55, 43–51. [Google Scholar] [CrossRef]
- Cangas, A.J.; Navarro, N.; Ojeda, J.J.; Cangas, D.; Piedra, J.A.; Gallego, J. Assessment of the usefulness and appeal of stigma-stop by psychology students: A serious game designed to reduce the stigma of mental illness. Mental Health 2017, 2, 5. [Google Scholar] [CrossRef]
- Papadopoulos, C.; Kenning, G.; Bennett, J.; Kuchelmeister, V.; Ginnivan, N.; Neidorf, M. A visit with Viv: Empathising with a digital human character embodying the lived experiences of dementia. Dementia 2021, 20, 2462–2477. [Google Scholar] [CrossRef]
- Baker, E.K.; Kurtz, M.; Astur, R.S. Virtual reality assessment of medication compliance in patients with schizophrenia. CyberPsychol. Behav. 2006, 9, 224–229. [Google Scholar] [CrossRef]
- Yellowlees, P.M.; Cook, J.N. Education about hallucinations using an internet virtual reality system: A qualitative survey. Acad. Psychiatry 2006, 30, 534–539. [Google Scholar] [CrossRef]
- Wijma, E.M.; Veerbeek, M.A.; Prins, M.; Pot, A.M.; Willemse, B.M. A virtual reality intervention to improve the understanding and empathy for people with dementia in informal caregivers: Results of a pilot study. Aging Ment. Health 2018, 22, 1121–1129. [Google Scholar] [CrossRef]
- Smith, F. Information literacy instruction using virtual reality. In Beyond Reality: Augmented, Virtual, and Mixed Reality in the Library; ALA Editions: Chicago, IL, USA, 2019; pp. 87–98. [Google Scholar]
- Freina, L.; Ott, M. A literature review on immersive virtual reality in education: State of the art and perspectives. In Proceedings of the International Scientific Conference Elearning and Software for Education, Bucharest, Romania, 23–24 April 2015; Volume 1, pp. 1000–1007. [Google Scholar]
- Pantelidis, V.S. Reasons to use virtual reality in education and training courses and a model to determine when to use virtual reality. Themes Sci. Technol. Educ. 2010, 2, 59–70. [Google Scholar]
- Webster, R. Declarative knowledge acquisition in immersive virtual learning environments. Interact. Learn. Environ. 2016, 24, 1319–1333. [Google Scholar] [CrossRef]
- Alfalah, S.F.; Falah, J.F.; Alfalah, T.; Elfalah, M.; Muhaidat, N.; Falah, O. A comparative study between a virtual reality heart anatomy system and traditional medical teaching modalities. Virtual Real. 2019, 23, 229–234. [Google Scholar] [CrossRef]
- Fertleman, C.; Aubugeau-Williams, P.; Sher, C.; Lim, A.-N.; Lumley, S.; Delacroix, S.; Pan, X. A discussion of virtual reality as a new tool for training healthcare professionals. Front. Public Health 2018, 6, 44. [Google Scholar] [CrossRef] [PubMed]
- Pillai, A.S.; Mathew, P.S. Impact of virtual reality in healthcare: A review. In Virtual and Augmented Reality in Mental Health Treatment; IGI Global: Hershey, PA, USA, 2019; pp. 17–31. [Google Scholar]
- Plotzky, C.; Lindwedel, U.; Sorber, M.; Loessl, B.; König, P.; Kunze, C.; Kugler, C.; Meng, M. Virtual reality simulations in nurse education: A systematic mapping review. Nurse Educ. Today 2021, 101, 104868. [Google Scholar] [CrossRef] [PubMed]
- Wan, W.H.; Lam, A.H.Y. The effectiveness of virtual reality-based simulation in health professions education relating to mental illness: A literature review. Health 2019, 11, 646–660. [Google Scholar] [CrossRef]
- Tsai, C.-F.; Yeh, S.-C.; Huang, Y.; Wu, Z.; Cui, J.; Zheng, L. The effect of augmented reality and virtual reality on inducing anxiety for exposure therapy: A comparison using heart rate variability. J. Healthc. Eng. 2018, 2018, 6357351. [Google Scholar] [CrossRef]
- Geraets, C.N.; Van der Stouwe, E.C.; Pot-Kolder, R.; Veling, W. Advances in immersive virtual reality interventions for mental disorders: A new reality? Curr. Opin. Psychol. 2021, 41, 40–45. [Google Scholar] [CrossRef]
- Bell, I.H.; Nicholas, J.; Alvarez-Jimenez, M.; Thompson, A.; Valmaggia, L. Virtual reality as a clinical tool in mental health research and practice. Dialogues Clin. Neurosci. 2020, 22, 169. [Google Scholar] [CrossRef]
- Han, S. An integrative review on augmented reality/virtual reality simulation programs in the mental health area for health professionals. Int. J. Contents 2019, 15, 36–43. [Google Scholar]
- Jones, C.; Jones, D.; Moro, C. Use of virtual and augmented reality-based interventions in health education to improve dementia knowledge and attitudes: An integrative review. BMJ Open 2021, 11, e053616. [Google Scholar] [CrossRef]
- Herrera, F.; Bailenson, J.; Weisz, E.; Ogle, E.; Zaki, J. Building long-term empathy: A large-scale comparison of traditional and virtual reality perspective-taking. PLoS ONE 2018, 13, e0204494. [Google Scholar] [CrossRef]
- Pan, X.; Gillies, M.; Slater, M. Virtual character personality influences participant attitudes and behavior–an interview with a virtual human character about her social anxiety. Front. Robot. AI 2015, 2, 1. [Google Scholar] [CrossRef]
- Hoppe, M.; Baumann, A.; Tamunjoh, P.C.; Machulla, T.-K.; Woźniak, P.W.; Schmidt, A.; Welsch, R. There Is No First- or Third-Person View in Virtual Reality: Understanding the Perspective Continuum. In Proceedings of the CHI Conference on Human Factors in Computing Systems, New Orleans, LA, USA, 30 April–5 May 2022; pp. 1–13. [Google Scholar]
- McCall, C.; Singer, T. Empathy and the brain. In Understanding other Minds: Perspectives from Developmental Social Neuroscience; Oxford University Press: Oxford, UK, 2013; pp. 194–209. [Google Scholar]
- Ventura, S.; Badenes-Ribera, L.; Herrero, R.; Cebolla, A.; Galiana, L.; Baños, R. Virtual reality as a medium to elicit empathy: A meta-analysis. Cyberpsychology Behav. Soc. Netw. 2020, 23, 667–676. [Google Scholar] [CrossRef] [PubMed]
- Dyer, E.; Swartzlander, B.J.; Gugliucci, M.R. Using virtual reality in medical education to teach empathy. J. Med. Libr. Assoc. JMLA 2018, 106, 498. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Z.; Sun, K.; Jatchavala, C.; Koh, J.; Chia, Y.; Bose, J.; Li, Z.; Tan, W.; Wang, S.; Chu, W. Overview of stigma against psychiatric illnesses and advancements of anti-stigma activities in six Asian societies. Int. J. Environ. Res. Public Health 2020, 17, 280. [Google Scholar] [CrossRef]
- Gunasekaran, S.; Tan, G.T.H.; Shahwan, S.; Goh, C.M.J.; Ong, W.J.; Subramaniam, M. The perspectives of healthcare professionals in mental health settings on stigma and recovery—A qualitative inquiry. BMC Health Serv. Res. 2022, 22, 1–16. [Google Scholar] [CrossRef] [PubMed]
- Martingano, A.J.; Hererra, F.; Konrath, S. Virtual reality improves emotional but not cognitive empathy: A meta-analysis. Technol. Mind Behav. 2021, 2, 1–15. [Google Scholar] [CrossRef]
- Ando, S.; Clement, S.; Barley, E.A.; Thornicroft, G. The simulation of hallucinations to reduce the stigma of schizophrenia: A systematic review. Schizophr. Res. 2011, 133, 8–16. [Google Scholar] [CrossRef]

| Author Country/Setting | Design/ Participant | Intervention | Control | Outcome Measures | Knowledge | Attitudes | Empathy | Stigma |
|---|---|---|---|---|---|---|---|---|
| [51] United States | 2 arm quasi-experimental Patients with schizophrenia and healthy control | G1: Patients with schizophrenia, n = 25 - Participants interact with surroundings, objects in a virtual environment using mouse. They were asked to take pills with virtual distractions (siren, ringing doorbells). | G2: Healthy control, n = 16 - same intervention | Pre - The Medication Management Ability Assessment (MMAA) - Continuous Performance Test | ↑ Better pill selection, less time discrepancy when taking medications and greater MMAA score with reminder notes, clock | Nil | Nil | Nil |
| [47] United States | Pre, post single group quasi-experimental Nursing under-graduates from 3 classes | G1: Virtual Dementia Tour, n = 163 - equipment that altered participants’ vision, hearing and touch - complete 5 tasks - 10 min | Pre group | Pre, post - Dementia Attitudes Scale - Knowledge about Memory Loss and Care - Healthcare tour survey Post only - Students’ reflection | ↑ Improvement noted post-test although it did not reach significant levels | ↑ Significant improvement at post-intervention | ↑ Students’ reflection highlighted that patients with dementia required empathy and sensitivity. Students affirmed the need to support caregivers and families. | Nil |
| [49] Spain | Post only single group quasi- experimental Psychology under-graduates aged 18 to 28 | G1: Stigma-Stop, n = 26 | Nil | Post only - Open ended questions and the following questions rated ‘yes’ and ‘no’: (1) Whether character is emotionally well? (2) Whether participant can help the character? (3) Whether participant had similar experience? | -- Most participants rated characters as emotionally unwell: a. 96%- panic disorder with agoraphobia b. 96% for schizophrenia c. 73% for bipolar disorder d. 100% for depression | -- Most participants felt they could help the character: a. 100%- panic disorder with agoraphobia b. 88% for schizophrenia c. 79% for bipolar disorder d. 92% for depression | Nil | ↓ Participants’ open-ended answers showed reduction of stigma. |
| [36] Spain | 2 arm pre post RCT High school students aged 14–18, from 24 classes | G1: Stigma-Stop, n = 484 from 21 classes - Non immersive virtual reality game presenting four characters experiencing depression, bipolar disorder, schizophrenia, panic disorder with agoraphobia. | G2: n = 68 from 3 classes | Pre, post - Student Attitudes toward Schizophrenia measures stereotypes and other aggressiveness | -- Most participants rated characters as emotionally unwell: a. 96.8%- panic disorder with agoraphobia b. 86.8% for schizophrenia c. 61.8% for bipolar disorder d. 96.1% for depression | -- About half to most of the participants felt they could help the character: a. 82.4%- panic disorder with agoraphobia b. 62.5% for schizophrenia c. 53% for bipolar disorder d. 90% for depression | Nil | ↓ Stigma-Stop group had significantly lower stigma |
| [34] Australia | Pre-post single group quasi- experimental Public and psychology under-graduates | G1: VR, n = 50 - with head mounted display, headphones and Xbox controller, - virtual environment with VH environmental sounds and voices suggestive of danger - 10–15 min | Pre group | Pre, post - Knowledge * about psychosis - Attitude ^ by Reavley and Jorm (2011) - Empathy by clinical empathy scale | ↑ Significant improvement at post-test | ↑ Significant improvement in attitude scores at post-test | ↑ Significant improvement in empathy scores at post-test | Nil |
| [35] Australia | Pre-post 2 arm quasi-experimental Medicine and pharmacy under-graduates | G1: Australia Vic Virtual Dementia Experience, n= 80 - multisensory, virtual simulation to allow participants to experience perceptual and cognitive difficulties by patients - 1.5 h | G2: Waitlist control group, n = 198 - curriculum as usual | Pre post - Dementia Attitudes Scale | Nil | ↑ Intervention group had significantly better attitude scores at post-test | Nil | Nil |
| [44] United States | Descriptive study Nursing students, n = 126 | G1: VR condition, n = 126 - Students viewed virtual neighbourhood with two houses: one belonged to someone with schizophrenia, another with depression. Students enter house and interact with patient. - Students were given case studies on the patients. - 45–60 min | Nil | Post only - * 35-item Second Life (SL) Simulation Evaluation Survey - Two open-ended questions regarding feedback about stimulation | ↑ Second Life Simulation, as a teaching modality, was moderately effective. | Nil | Nil | Nil |
| [45] United States | Pre- and post-intervention study 4th year nursing undergraduates | G1: VR, n = 149 - one virtual simulation case study weekly on depression, bipolar disorder, anxiety, alcohol withdrawal and schizophrenia - 30 min, student can repeat simulation | G2: Non-simulation group, n = 150 | Post only - Two vignettes, schizophrenia and depression. Participants answer about their perception of helpfulness of certain people (including healthcare workers, traditional healers, family and friends), specific medications and interventions (e.g., physical activity, massage, relaxation, specific therapies). | ↑ For perceived helpfulness of pharmacological interventions, intervention group was less likely to rate antipsychotics and sleeping pills as ‘do not know’ for the depression vignette. Control group was more likely than G1 to rate psychiatric hospital admission and electroconvulsive therapy as ‘do not know’. | -- Both groups agreed solving the problem by self as unhelpful. | Nil | Nil |
| [50] Australia | Pre post single group quasi-experimental Students and public | G1: Visit with Viv, n = 35: - VR about Viv, who recounts her experiences of dementia > life-size in art gallery, > Occulus Quest VR headset in university, n = 36 - 15–20 min | Pre group | Pre post - comprehensive state empathy scale - Change in emotional distance scale | Nil | Nil | ↑ Significant improvement in empathy scores from pre-test | ↓ Significant reduction in stigma levels at post-test |
| [46] Brazil | Pre post single group quasi-experimental Medical students from 3 universities | G1: AR, n = 21 - figures and voices from narratives of three patients with schizophrenia - voices included whispers, commanding and threatening speech - 3 min | Pre group | Pre post - Schizophrenia stigma * Post only - Evaluate environment simulation | Nil | ↑ Significant increase in the average score of help-giving at post-test | ↑ Increase in empathy | ↑ Increase in stigma especially in fear, pity and segregation. |
| [48] Ireland | Pre post repeated single group quasi-experimental Health professionals, voluntary groups and public | G1: Virtual Dementia Tour + watching another group doing distortion session, n = 240 - 2 h - 10 min of sensory distortion - 30 min debriefing | Pre group | Pre post, follow up at 3 months * Tool that measures empathy, understanding of behaviours and role of the person in care decisions. | ↑ Significant improvement in understanding of behavioural impact of dementia across time points | Nil | ↑ Significant improvement in empathy across time | Nil |
| [41] United States | 4 arm post only RCT Psychology research participant pool and university community | G1: VR condition, n = 26 - Participant plays the character of someone experiencing schizophrenia, visiting a pharmacist asking for prescription refill. - 4.5 min G2: Empathy condition, n = 26 - Participants were asked to pen their thoughts about experiencing VH and AH while getting prescription - 1 min G3: VR+ empathy condition, n = 26 - Empathy before VR condition | G4: control, n = 26 No intervention control group | Post only - Empathy 12-items - Social Distance Scale - Attitudes Toward People with Schizophrenia, 7 items - Evaluation of simulation - Pre-existing attitudes towards people with schizophrenia, 8 items | Nil | ↑ Intervention group had better attitudes but this did not reach significant levels | ↑ Significant improvement in empathy in intervention groups using VR | ↓ VR group had significantly lower stigma |
| [42] Germany | 3 arm post only RCT Majority are students from university, n = 114 | G1: VR, n = 31 - Young male actor speaking about his experiences with schizophrenia, including how his loved ones cope with it. G2: regular video, n = 45 - Similar as the VR but fixed perspective | G3: No intervention control group, n = 38 | Post only - Stigma with four related constructs: anxiety *, social proximity ^, empathy (by Kinnebrock et al., 2010, - Benevolence (using Community-Attitudes-Toward-the-Mentally Ill Inventory) | Nil | Nil | Nil | ↑ VR contact did not decrease stigmatization compared with control but had increased stigmatization compared with video. |
| [53] The Netherlands Alzheimer’s Society | Pre post single group quasi-experimental Informal caregivers caring for those with dementia | G1: VR, n = 35 360-degree simulation movie on virtual reality (first person view) and e-course, n = 42- different scenes of interactions e.g., confronted by daughter about remote control in cupboard and she talks to people on the phone about you - 13 min | Pre group | Pre, post - Empathy measured by Person-centeredness subscale of Approach to Dementia questionnaire and ‘perspective-taking’ subscale of Interpersonal Reactivity Index | Nil | Nil | ↑ Significant improvement using the perspective-taking subscale | Nil |
| [52] United States | Post only single group quasi- experimental Second Life Users | G1: Second Life VR, n = 579 - Character toured environment, experiencing hallucinations including voices, posters changing text to profanities, floor that fall away, TV that encourage suicide and gun with voices telling character to commit suicide, and own reflection with bleeding eyes. | Nil | Post only - Questions about understanding of hallucinations | -- Intervention group had improvements of understanding of (1) AH- 76.86% (2) VH- 69.91% (3) Schizophrenia- 73.9% | Nil | Nil | Nil |
| [43] Hong Kong | 3 arm pre post RCT University students 18 years old and above | G1: Immersive animation, n = 82 Participants played a character, Yan, who had mixed anxiety and depression, and who was speaking with an uncle. Pop up messages illustrated problems in Uncle’s communication. G2: Text condition, n = 80 Participants read same story in 2D effect, without immersive experience. All 3 groups: 10 min, had VR headset, Oculus Go. | G3: Control, n = 82 Exoplanet VR video, 360° | Pre, post, 1 week follow up: - Stigma by 21-item Public Stigma and Acceptance Scale - 7-item Sense of Embodiment Scale * - Story Transportation | Nil | Nil | Nil | ↓ Immersive animation and text condition had significantly lower public stigma at post-test and follow up compared with the control group. Immersive animation vs. text condition did not have significantly different stigma levels between them. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tay, J.L.; Xie, H.; Sim, K. Effectiveness of Augmented and Virtual Reality-Based Interventions in Improving Knowledge, Attitudes, Empathy and Stigma Regarding People with Mental Illnesses—A Scoping Review. J. Pers. Med. 2023, 13, 112. https://doi.org/10.3390/jpm13010112
Tay JL, Xie H, Sim K. Effectiveness of Augmented and Virtual Reality-Based Interventions in Improving Knowledge, Attitudes, Empathy and Stigma Regarding People with Mental Illnesses—A Scoping Review. Journal of Personalized Medicine. 2023; 13(1):112. https://doi.org/10.3390/jpm13010112
Chicago/Turabian StyleTay, Jing Ling, Huiting Xie, and Kang Sim. 2023. "Effectiveness of Augmented and Virtual Reality-Based Interventions in Improving Knowledge, Attitudes, Empathy and Stigma Regarding People with Mental Illnesses—A Scoping Review" Journal of Personalized Medicine 13, no. 1: 112. https://doi.org/10.3390/jpm13010112
APA StyleTay, J. L., Xie, H., & Sim, K. (2023). Effectiveness of Augmented and Virtual Reality-Based Interventions in Improving Knowledge, Attitudes, Empathy and Stigma Regarding People with Mental Illnesses—A Scoping Review. Journal of Personalized Medicine, 13(1), 112. https://doi.org/10.3390/jpm13010112