Nomogram for Predicting Semen Parameters Improvement after Microscopic Varicocelectomy in Infertile Men with Abnormal Semen Parameters
Abstract
1. Introduction
2. Methods
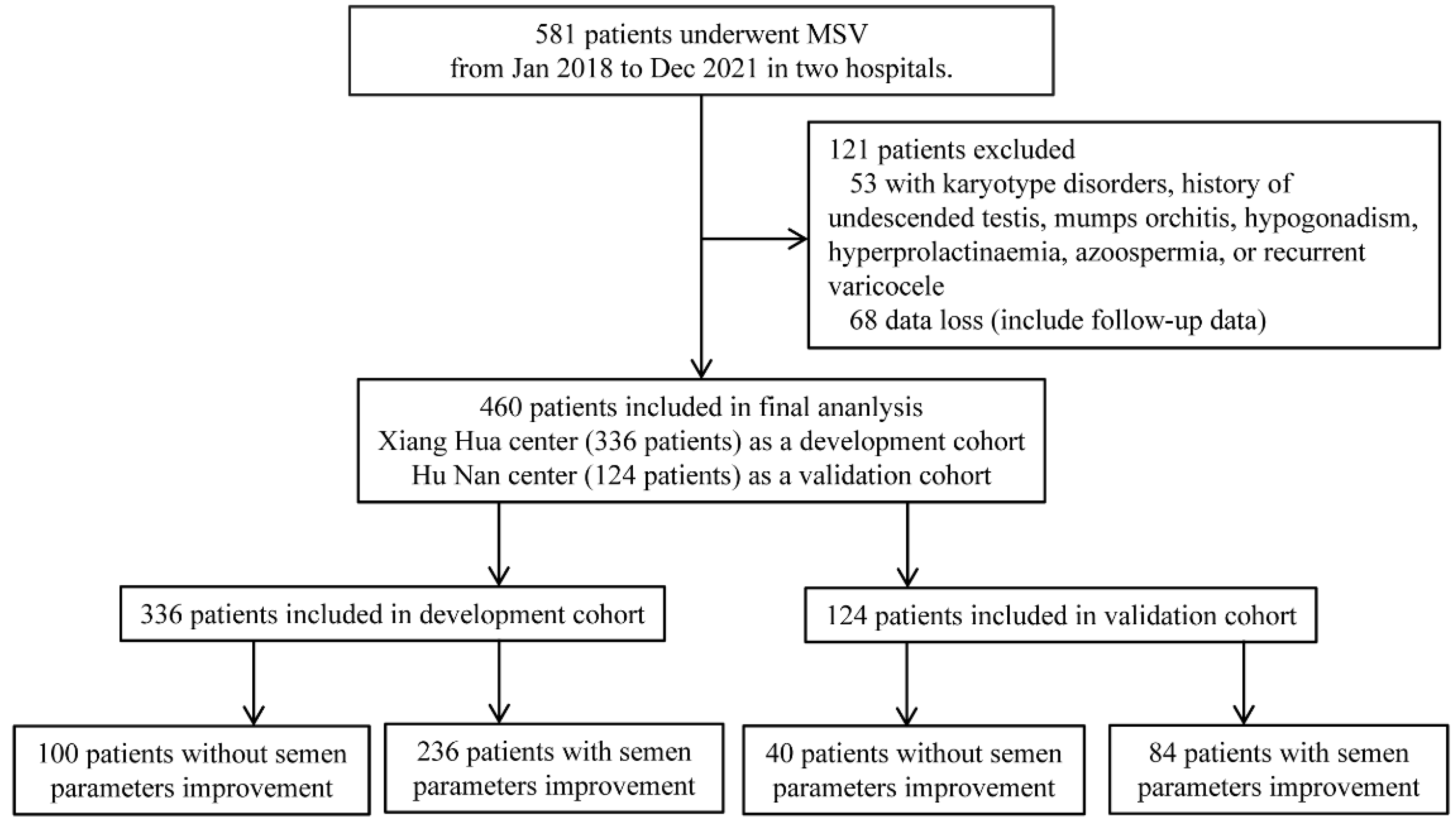
2.1. Study Design
2.2. Inclusion and Exclusion Criteria
2.3. Measurement of Characteristics and Follow-Up
2.4. Statistical Analysis
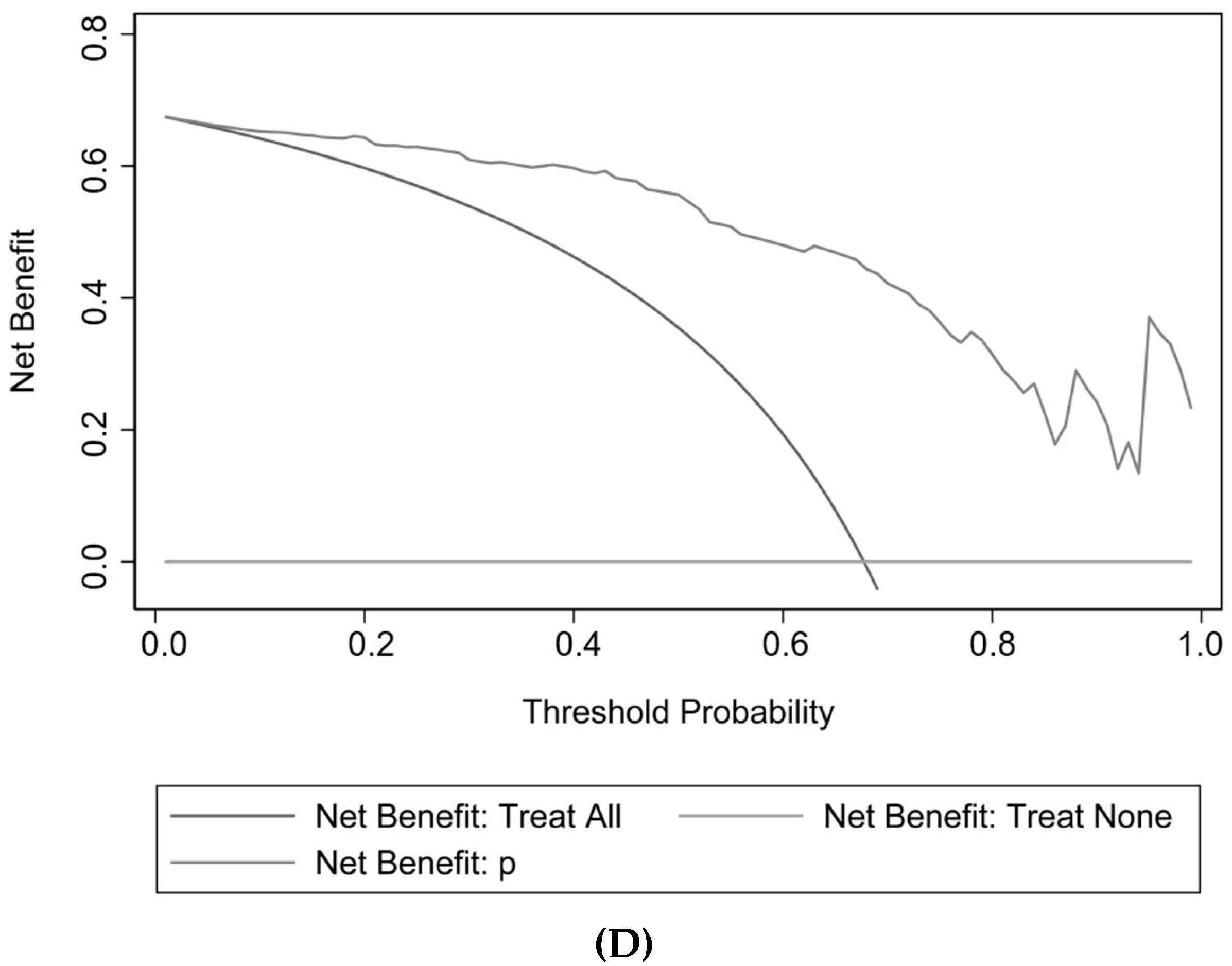
3. Results
4. Discussion
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
References
- Damsgaard, J.; Joensen, U.N.; Carlsen, E.; Erenpreiss, J.; Jensen, M.B.; Matulevicius, V.; Zilaitiene, B.; Olesen, I.A.; Perheentupa, A.; Punab, M.; et al. Varicocele is associated with impaired semen quality and reproductive hormone levels: A study of 7035 healthy young men from six European countries. Eur. Urol. 2016, 70, 1019–1029. [Google Scholar] [CrossRef]
- Jensen, C.F.S.; Østergren, P.; Dupree, J.M.; Ohl, D.A.; Sønksen, J.; Fode, M. Varicocele and male infertility. Nat. Rev. Urol. 2017, 14, 523–533. [Google Scholar] [CrossRef] [PubMed]
- Baazeem, A.; Belzile, E.; Ciampi, A.; Dohle, G.; Jarvi, K.; Salonia, A.; Weidner, W.; Zini, A. Varicocele and male factor infertility treatment: A new meta-analysis and review of the role of varicocele repair. Eur. Urol. 2011, 60, 796–808. [Google Scholar] [CrossRef] [PubMed]
- Dubin, J.M.; Greer, A.B.; Kohn, T.P.; Masterson, T.A.; Ji, L.; Ramasamy, R. Men with severe oligospermia appear to benefit from varicocele repair: A cost-effectiveness analysis of assisted reproductive technology. Urology 2018, 111, 99–103. [Google Scholar] [CrossRef] [PubMed]
- Kohn, T.P.; Kohn, J.R.; Pastuszak, A.W. Varicocelectomy before assisted reproductive technology: Are outcomes improved? Fertil. Steril. 2017, 108, 385–391. [Google Scholar] [CrossRef] [PubMed]
- Ding, H.; Tian, J.; Du, W.; Zhang, L.; Wang, H.; Wang, Z. Open non-microsurgical, laparoscopic or open microsurgical varicocelectomy for male infertility: A meta-analysis of randomized controlled trials. BJU Int. 2012, 110, 1536–1542. [Google Scholar] [CrossRef]
- Wang, H.; Ji, Z.G. Microsurgery versus laparoscopic surgery for varicocele: A meta-analysis and systematic review of randomized controlled trials. J. Investig. Surg. 2020, 33, 40–48. [Google Scholar] [CrossRef]
- Bryniarski, P.; Taborowski, P.; Rajwa, P.; Kaletka, Z.; Życzkowski, M.; Paradysz, A. The comparison of laparoscopic and microsurgical varicocoelectomy in infertile men with varicocoele on paternity rate 12 months after surgery: A prospective randomized controlled trial. Andrology 2017, 5, 445–450. [Google Scholar] [CrossRef]
- Pan, F.; Pan, L.; Zhang, A.; Liu, Y.; Zhang, F.; Dai, Y. Comparison of two approaches in microsurgical varicocelectomy in Chinese infertile males. Urol. Int. 2013, 90, 443–448. [Google Scholar] [CrossRef]
- Almekaty, K.; Zahran, M.H.; Zoeir, A.; Minhas, S.; Salem, K. The role of artery-preserving varicocelectomy in subfertile men with severe oligozoospermia: A randomized controlled study. Andrology 2019, 7, 193–198. [Google Scholar] [CrossRef]
- Bozhedomov, V.A.; Lipatova, N.A.; Alexeev, R.A.; Alexandrova, L.M.; Nikolaeva, M.A.; Sukhikh, G.T. The role of the antisperm antibodies in male infertility assessment after microsurgical varicocelectomy. Andrology 2014, 2, 847–855. [Google Scholar] [CrossRef]
- Huang, H.C.; Huang, S.T.; Chen, Y.; Hsu, Y.C.; Chang, P.C.; Hsieh, M.L. Prognostic factors for successful varicocelectomy to treat varicocele-associated male infertility. Reprod. Fertil. Dev. 2014, 26, 485–490. [Google Scholar] [CrossRef]
- Palmisano, F.; Moreno-Mendoza, D.; Ievoli, R.; Veber-Moisés-Da Silva, G.; Gasanz-Serrano, C.; Villegas-Osorio, J.F.; Peraza-Godoy, M.F.; Vives, Á.; Bassas, L.; Montanari, E.; et al. Clinical factors affecting semen improvement after microsurgical subinguinal varicocelectomy: Which subfertile patients benefit from surgery? Ther. Adv. Urol. 2019, 11, 1756287219887656. [Google Scholar] [CrossRef]
- Shabana, W.; Teleb, M.; Dawod, T.; Elsayed, E.; Desoky, E.; Shahin, A.; Eladl, M.; Sorour, W. Predictors of improvement in semen parameters after varicocelectomy for male subfertility: A prospective study. Can. Urol. Assoc. J. 2015, 9, E579–E582. [Google Scholar] [CrossRef]
- Ok, F.; Erdogan, O.; Durmus, E. Can preoperative gonadotropin and testosterone levels predict the success of varicocelectomy? Andrologia 2020, 52, e13887. [Google Scholar] [CrossRef]
- World Health Organization. WHO Laboratory Manual for the Examination and Processing of Human Semen, 5th ed.; WHO Press: Geneva, Switzerland, 2010; pp. 1–286. Available online: https://www.who.int/docs/default-source/reproductive-health/srhr-documents/infertility/examination-and-processing-of-human-semen-5ed-eng.pdf (accessed on 7 November 2022).
- Collins, G.S.; Reitsma, J.B.; Altman, D.G.; Moons, K.G. Transparent reporting of a multivariable prediction model for individual prognosis or diagnosis (TRIPOD): The TRIPOD statement. BMJ 2015, 350, g7594. [Google Scholar] [CrossRef]
- Sauerbrei, W.; Boulesteix, A.L.; Binder, H. Stability investigations of multivariable regression models derived from low- and high-dimensional data. J. Biopharm. Stat. 2011, 21, 1206–1231. [Google Scholar] [CrossRef]
- Abdel-Meguid, T.A.; Al-Sayyad, A.; Tayib, A.; Farsi, H.M. Does varicocele repair improve male infertility? An evidence-based perspective from a randomized, controlled trial. Eur. Urol. 2011, 59, 455–461. [Google Scholar] [CrossRef]
- Samplaski, M.K.; Lo, K.C.; Grober, E.D.; Zini, A.; Jarvi, K.A. Varicocelectomy to “upgrade” semen quality to allow couples to use less invasive forms of assisted reproductive technology. Fertil. Steril. 2017, 108, 609–612. [Google Scholar] [CrossRef]
- Wang, Q.; Yu, Y.; Liu, Y.; Wang, L. Outcome of varicocelectomy on different degrees of total motile sperm count: A systematic review and meta-analysis. Syst. Biol. Reprod. Med. 2019, 65, 430–436. [Google Scholar] [CrossRef]
- Al-Adl, A.M.; El-Karamany, T.; Issa, H.; Zaazaa, M. The influence of antisperm antibodies, intratesticular haemodynamics and the surgical approach to varicocelectomy on seminal variables. Arab J. Urol. 2014, 12, 309–317. [Google Scholar] [CrossRef] [PubMed]
- Seiler, F.; Kneissl, P.; Hamann, C.; Jünemann, K.P.; Osmonov, D. Laparoscopic varicocelectomy in male infertility: Improvement of seminal parameters and effects on spermatogenesis. Wien. Klin. Wochenschr. 2022, 34, 51–55. [Google Scholar] [CrossRef] [PubMed]
| Variables | Development Cohort | Validation Cohort |
|---|---|---|
| Number of patients (%) | 336 (100) | 124 (100) |
| Demographic characteristics | ||
| Age (years) | 31.64 ± 4.28 | 31.44 ± 4.26 |
| BMI (kg/m2) | 25.32 ± 3.78 | 24.92 ± 3.80 |
| Infertility duration (months) | 24 (12, 36) | |
| Dietary habits | ||
| Smoke (never vs. current or former) | 246 (73.2)/90 (26.8) | 93 (75.0)/31 (25.0) |
| Varicocele | ||
| Surgical side (left vs. bilateral) | 186 (55.4)/150 (44.6) | 75 (60.5)/49 (39.5) |
| Grade of palpation (left, II vs. III) | 156 (46.4)/180 (53.6) | 55 (44.4)/69 (60.5) |
| Diameter of veins (left, mm) | 3.33 ± 0.56 | 3.29 ± 0.56 |
| Testicualr volume (left, mL) | 15.34 ± 3.50 | 15.06 ± 3.54 |
| Semen parameters before MSV | ||
| Baseline TPMSC (106) | 13.82 ± 3.83 | 13.84 ± 3.72 |
| Sperm concentration (106/mL) | 15.89 ± 2.87 | 15.31 ± 2.75 |
| Morphology (normal forms, %) | 2.84 ± 2.63 | 3.17 + 2.62 |
| Intraoperative data | ||
| Surgical approach (subinguinal vs. inguinal) | 234 (69.6)/102 (30.4) | 84 (67.7)/40 (32.3) |
| Ligated veins (number) | 13.51 ± 4.36 | 13.08 ± 4.44 |
| Development Cohort 336 (100.00) | Validation Cohort 124 (100.00) | |||||
|---|---|---|---|---|---|---|
| Variables | No Improvement | Improvement | p Value | No Improvement | Improvement | p Value |
| Number of patients (%) | 100 (29.8) | 236 (70.2) | 40 (32.3) | 84 (67.7) | ||
| Demographic characteristics | ||||||
| Age (years) | 31.72 ± 3.71 | 31.61 ± 4.51 | 0.830 | 31.33 ± 3.72 | 31.49 ± 4.38 | 0.839 |
| BMI (kg/m2) | 25.09 ± 4.11 | 25.07 ± 3.62 | 0.064 | 24.51 ± 4.13 | 25.11 ± 3.64 | 0.412 |
| Infertility duration (months) | 24 (24, 36) | 24 (12, 36) | 0.832 | 24 (24, 36) | 24 (12, 36) | 0.225 |
| Dietary habits | ||||||
| Smoke (never vs. current or former) | 70 (70.0)/30 (30.0) | 176 (74.6)/60 (25.4) | 0.386 | 26 (65.0)/14 (35.0) | 67 (79.8)/17 (20.2) | 0.076 |
| Varicocele | ||||||
| Surgical side (left vs. bilateral) | 54 (54.0)/46 (46.0) | 132 (55.9)/104 (44.1) | 0.745 | 21 (52.5)/19 (47.5) | 54 (64.3)/30 (35.7) | 0.210 |
| Grade of palpation (left, II vs. III) | 44 (44.0)/56 (56.0) | 112 (47.5)/124 (52.5) | 0.561 | 18 (45.0)/22 (55.0) | 37 (44.0)/47 (56.0) | 0.921 |
| Diameter of veins (left, mm) | 3.15 ± 0.49 | 3.41 ± 0.57 | <0.001 | 3.13 ± 0.38 | 3.36 ± 0.62 | 0.033 |
| Testicualr volume (left, mL) | 14.82 ± 3.33 | 15.56 ± 3.55 | 0.076 | 14.00 ± 2.84 | 15.57 ± 3.74 | 0.020 |
| Semen parameters before MSV | ||||||
| Baseline TPMSC (106) | 9.82 ± 2.33 | 15.51 ± 2.98 | <0.001 | 10.25 ± 2.25 | 15.55 ± 2.99 | <0.001 |
| Sperm concentration (106/mL) | 15.44 ± 2.79 | 16.08 ± 2.89 | 0.062 | 14.83 ± 2.32 | 15.55 ± 2.92 | 0.140 |
| Morphology (normal forms, %) | 2.60 ± 2.51 | 2.94 ± 2.68 | 0.279 | 3.02 ± 2.77 | 2.24 ± 2.56 | 0.674 |
| Intraoperative data | ||||||
| Surgical approach (subinguinal vs. inguinal) | 72 (72.0)/28 (28.0) | 162 (68.6)/74 (31.4) | 0.541 | 28 (70.0)/12 (30.0) | 56 (66.7)/28 (33.3) | 0.711 |
| Ligated veins (number) | 13.34 ± 4.38 | 13.58 ± 4.49 | 0.650 | 13.10 ± 4.13 | 13.07 ± 4.60 | 0.973 |
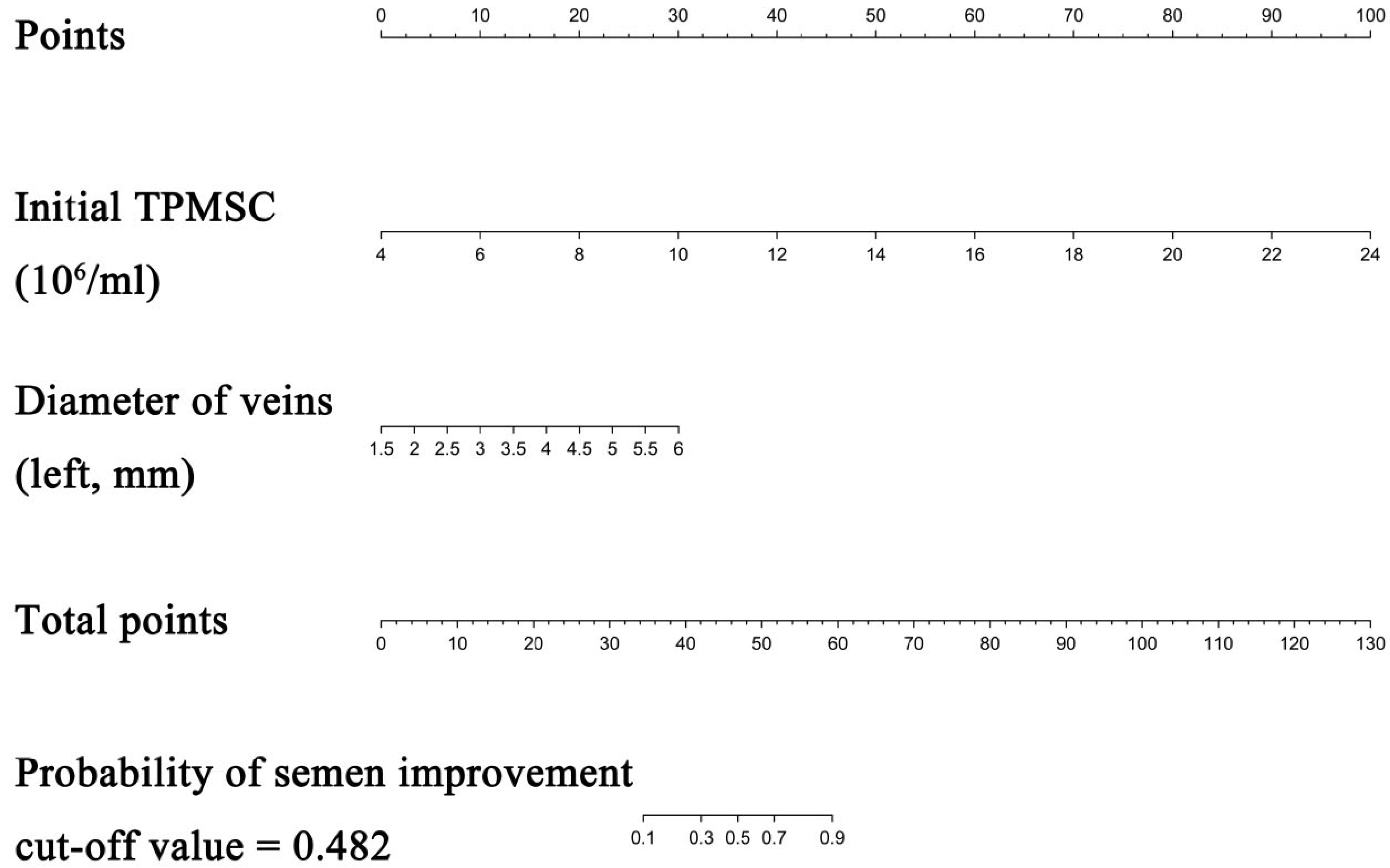
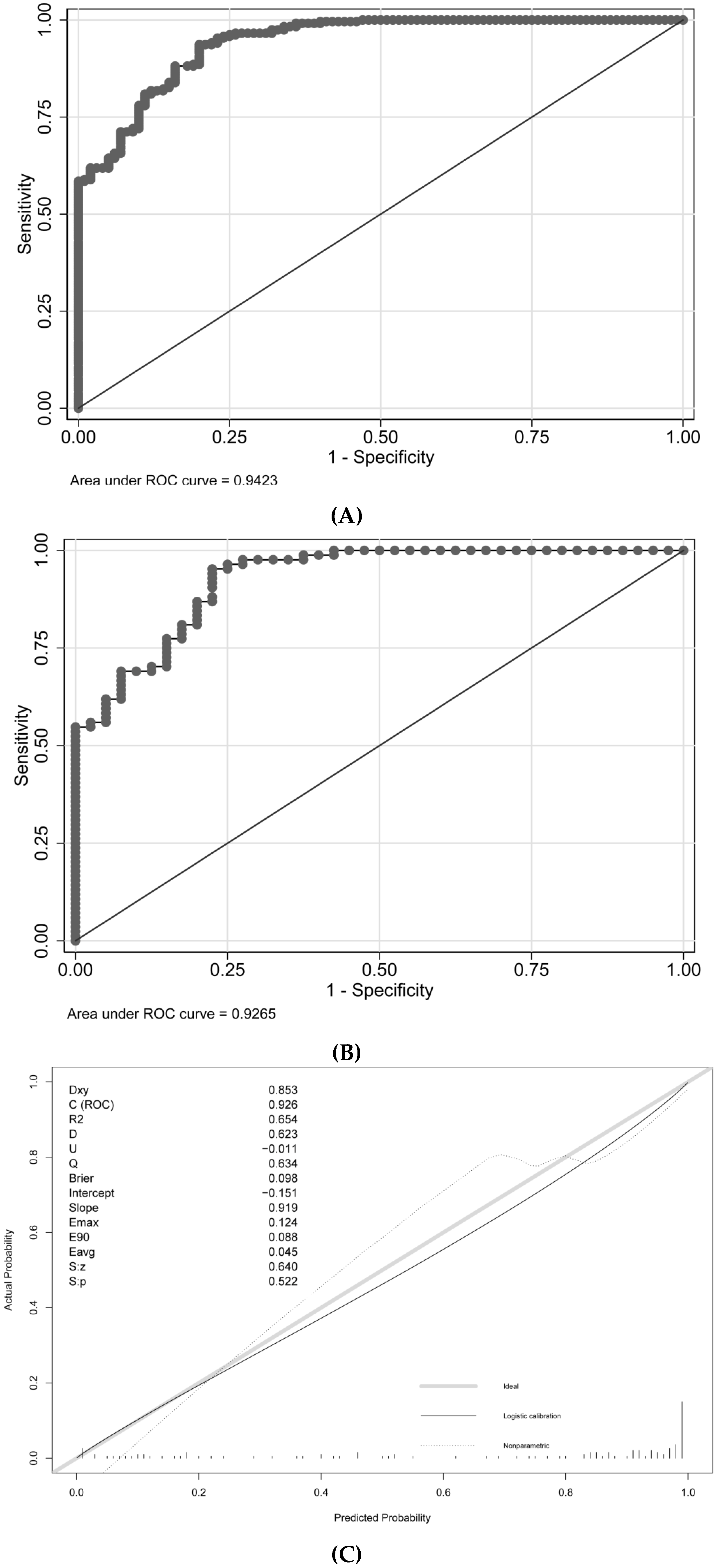
| Intercept and Variable | β | 95% CI | OR | 95% CI | p |
|---|---|---|---|---|---|
| Intercept | −13.598 | −17.261, −9.934 | 1.24 × 10−6 | 3.19 × 10−8, 0.0000485 | <0.001 |
| Diameter of veins (left, mm) | 1.181 | 0.382, 1.980 | 3.258 | 1.465, 7.242 | 0.004 |
| Baseline TPMSC (106) | 0.885 | 0.682, 1.090 | 2.422 | 1.978, 2.966 | <0.001 |
| Area under ROC curve | |||||
| Development Dataset | 0.942 | 0.918, 0.967 | p < 0.001 | ||
| Validation Dataset | 0.927 | 0.879, 0.974 | p < 0.001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Liu, X.; Liu, D.; Pan, C.; Su, H. Nomogram for Predicting Semen Parameters Improvement after Microscopic Varicocelectomy in Infertile Men with Abnormal Semen Parameters. J. Pers. Med. 2023, 13, 11. https://doi.org/10.3390/jpm13010011
Liu X, Liu D, Pan C, Su H. Nomogram for Predicting Semen Parameters Improvement after Microscopic Varicocelectomy in Infertile Men with Abnormal Semen Parameters. Journal of Personalized Medicine. 2023; 13(1):11. https://doi.org/10.3390/jpm13010011
Chicago/Turabian StyleLiu, Xiuping, Dongmei Liu, Chunyu Pan, and Hui Su. 2023. "Nomogram for Predicting Semen Parameters Improvement after Microscopic Varicocelectomy in Infertile Men with Abnormal Semen Parameters" Journal of Personalized Medicine 13, no. 1: 11. https://doi.org/10.3390/jpm13010011
APA StyleLiu, X., Liu, D., Pan, C., & Su, H. (2023). Nomogram for Predicting Semen Parameters Improvement after Microscopic Varicocelectomy in Infertile Men with Abnormal Semen Parameters. Journal of Personalized Medicine, 13(1), 11. https://doi.org/10.3390/jpm13010011







