Mathematical Model of Interaction of Therapist and Patients with Bipolar Disorder: A Systematic Literature Review
Abstract
1. Introduction
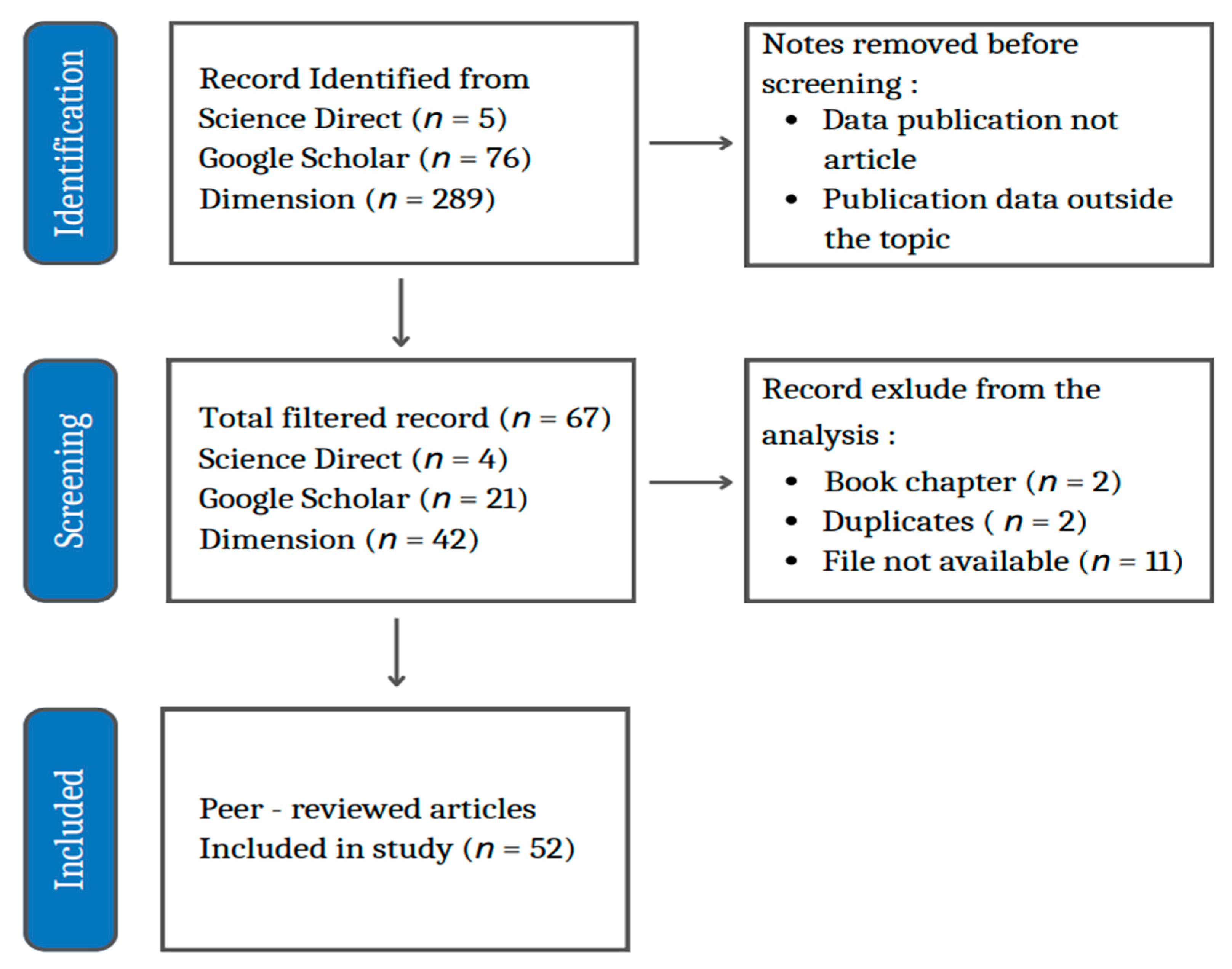
2. Materials and Methods
2.1. Scientific Article Data
2.2. Selection of Literature Database
2.3. Systematic Data Analysis and Methods
3. Results
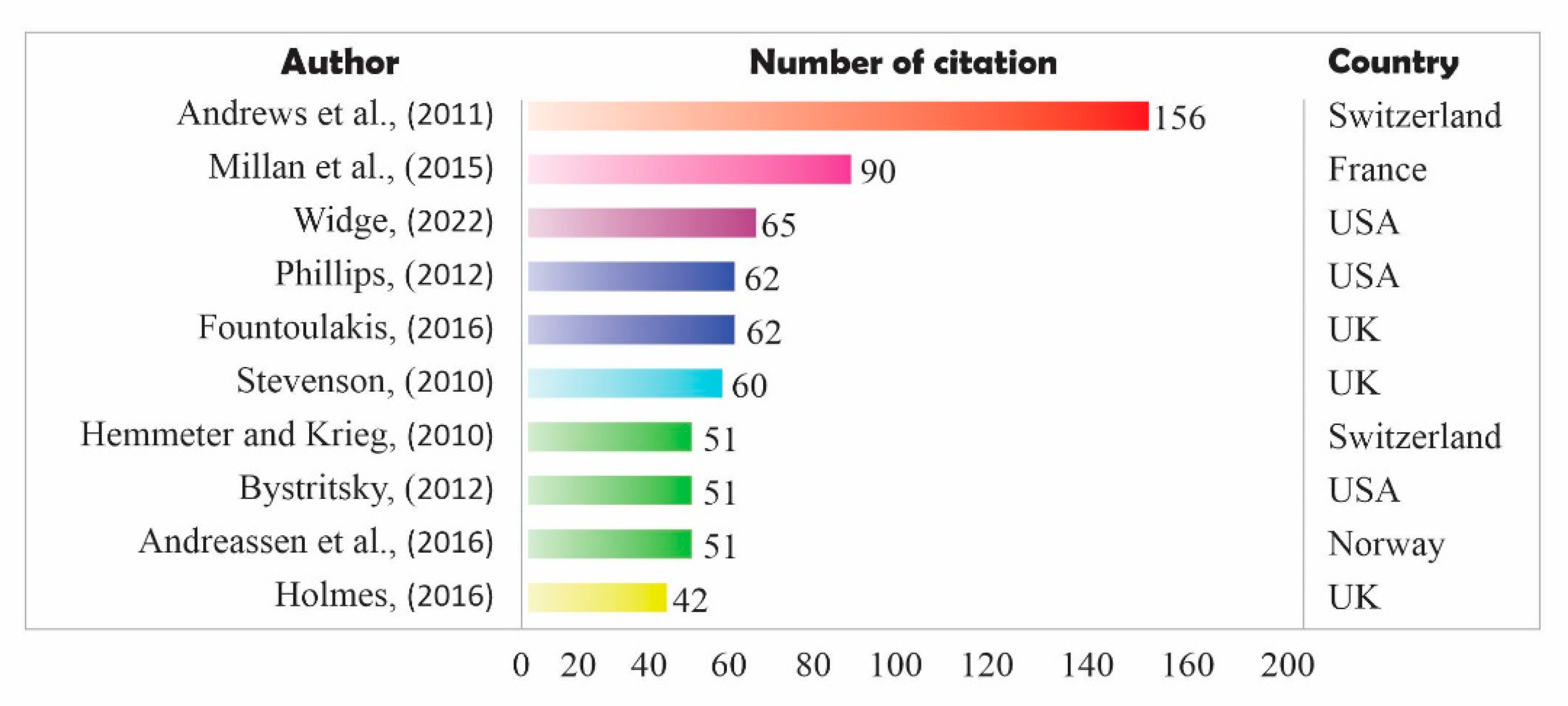
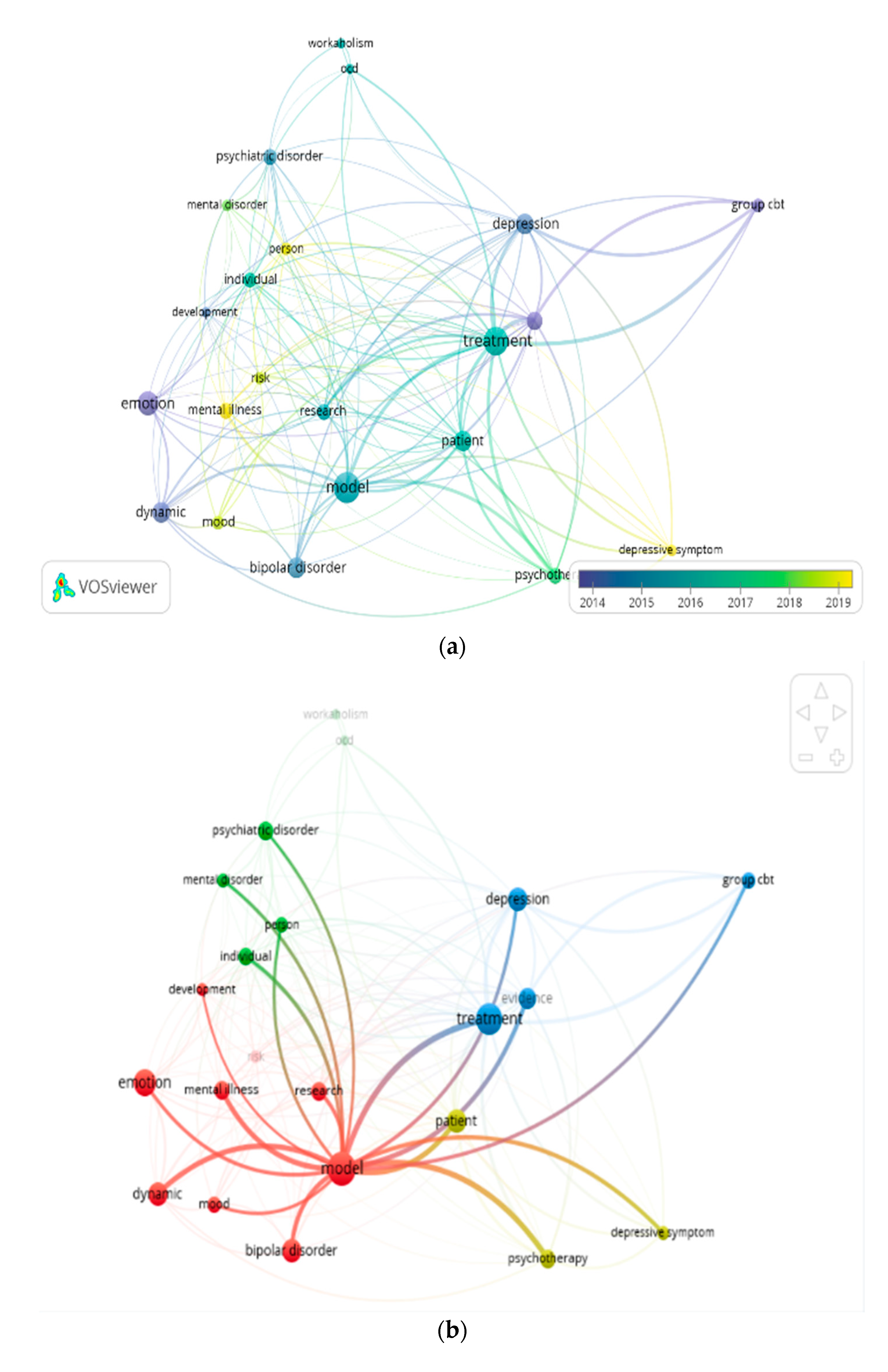
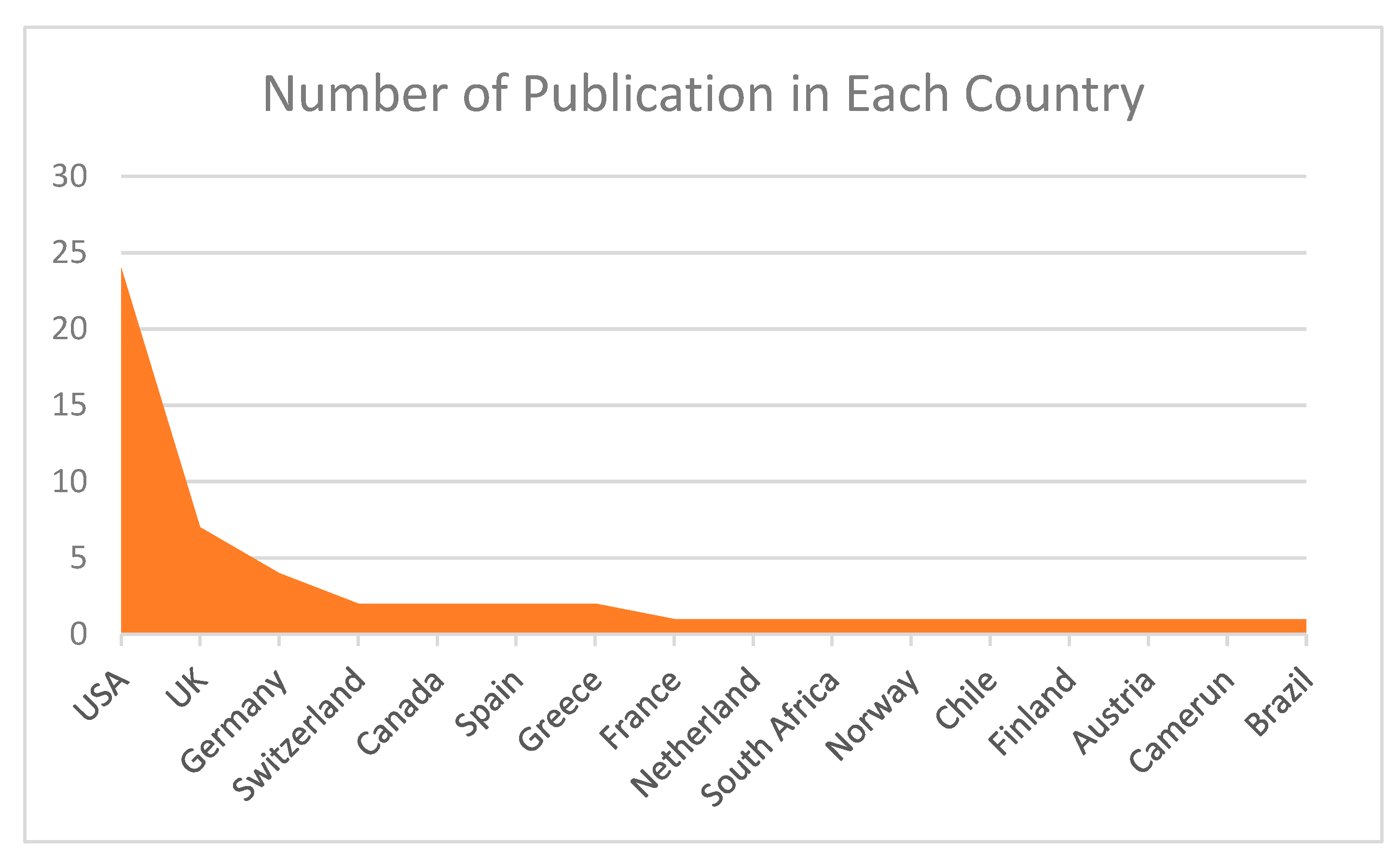
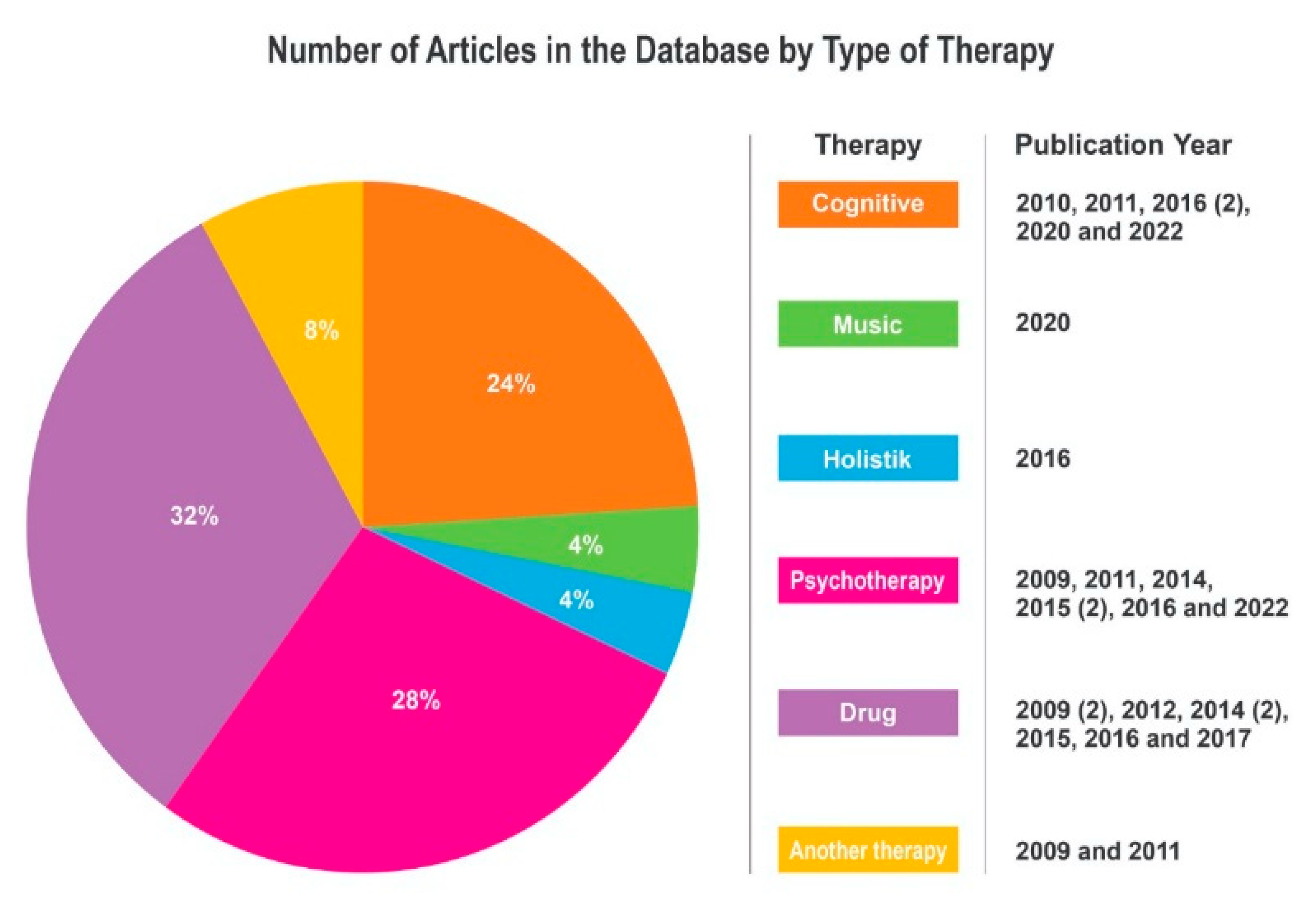
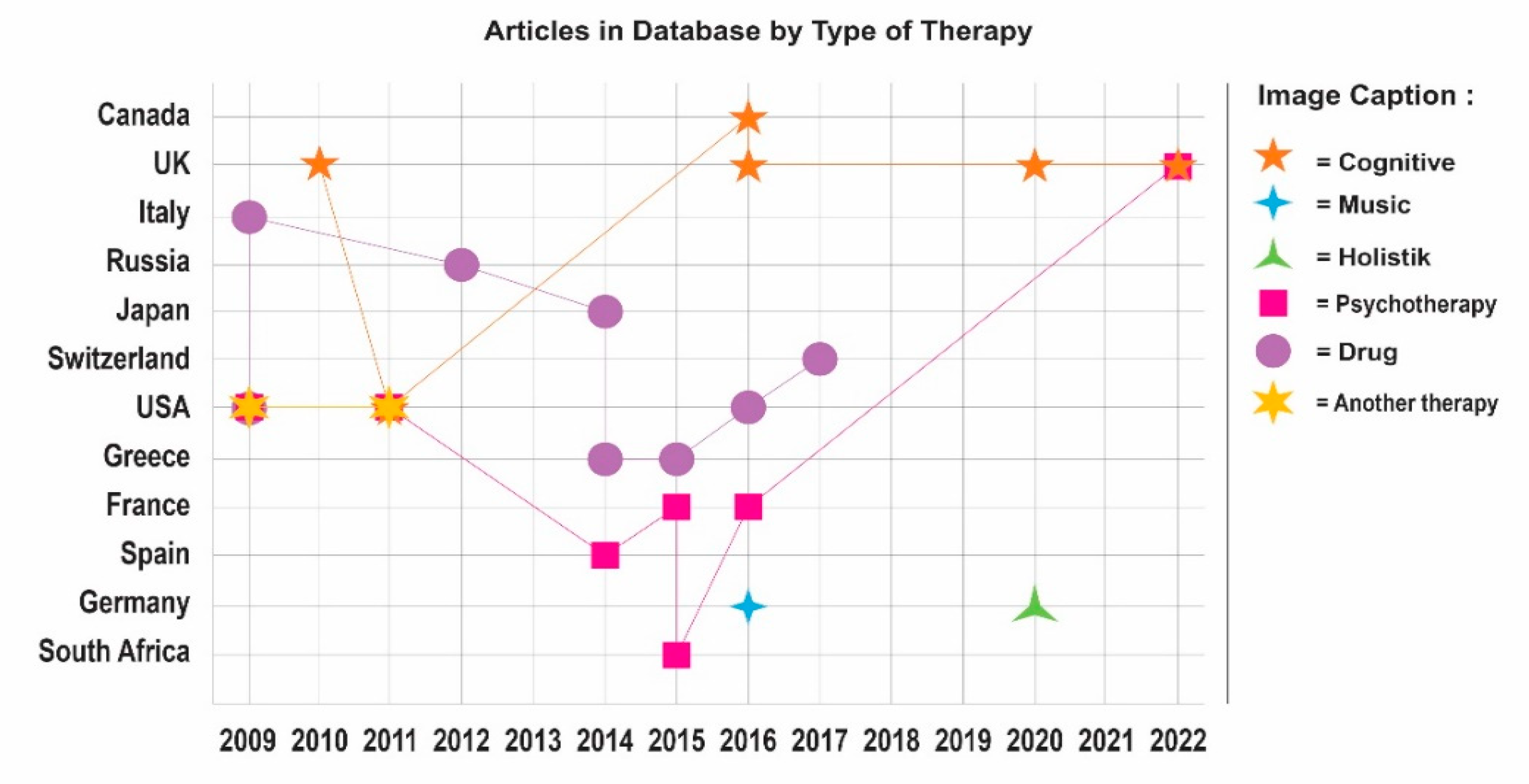
3.1. Article Data Visualization
3.2. BD Therapy Mathematical Model Development
3.3. Types of Therapy in Psychiatry
3.4. Methodology Used in Types of Therapy
4. Discussion
4.1. Research Trends in Mathematical Models of Interaction of BD and Therapists
4.2. Therapeutic Analysis and Psychiatric Diagnosis
4.3. Research Development in Mathematical Models of Interaction of BD and Therapists
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Widge, A.S.; Ellard, K.K.; Paulk, A.C.; Basu, I.; Yousefi, A.; Zorowitz, S.; Gilmour, A.; Afzal, A.; Deckersbach, T.; Cash, S.S.; et al. Treating Refractory Mental Illness With Closed-Loop Brain Stimulation: Progress Towards a Patient-Specific Transdiagnostic Approach. Focus 2022, 20, 137–151. [Google Scholar] [CrossRef] [PubMed]
- Demic, S.; Cheng, S. Modeling the dynamics of disease states in depression. PLoS ONE 2014, 9, e110358. [Google Scholar] [CrossRef]
- Lobban, F.; Solis-Trapala, I.; Tyler, E.; Chandler, C.; Morriss, R.K. The role of beliefs about mood swings in determining outcome in bipolar disorder. Cognit. Ther. Res. 2013, 37, 51–60. [Google Scholar] [CrossRef]
- Akers, N.; Lobban, F.; Hilton, C.; Panagaki, K.; Jones, S.H. Measuring social and occupational functioning of people with bipolar disorder: A systematic review. Clin. Psychol. Rev. 2019, 74, 101782. [Google Scholar] [CrossRef] [PubMed]
- Carlborg, A.; Ferntoft, L.; Thuresson, M.; Bodegard, J. Population study of disease burden, management, and treatment of bipolar disorder in Sweden: A retrospective observational registry study. Bipolar Disord. 2015, 17, 76–85. [Google Scholar] [CrossRef]
- Johnson, S.L.; Murray, G.; Fredrickson, B.; Youngstrom, E.A.; Hinshaw, S.; Bass, J.M.; Deckersbach, T.; Schooler, J.; Salloum, I. Creativity and bipolar disorder: Touched by fire or burning with questions? Clin. Psychol. Rev. 2012, 32, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Allen, C.B.T.-P. A first-rate madness: Uncovering the links between leadership and mental illness. Choice Rev. Online 2011, 49, 49–1764. [Google Scholar]
- Phillips, J.; Frances, A.; Cerullo, M.A.; Chardavoyne, J.; Decker, H.S.; First, M.B.; Ghaemi, N.; Greenberg, G.; Hinderliter, A.C.; Kinghorn, W.A.; et al. The six most essential questions in psychiatric diagnosis: A pluralogue part 1: Conceptual and definitional issues in psychiatric diagnosis. Philos. Ethics Humanit. Med. 2012, 7, 3. [Google Scholar] [CrossRef]
- Hafeez, H.Y.; Ndikilar, C.E.; Isyaku, S. Analytical Study of the Van der Pol Equation in the Autonomous Regime. Prog. Phys. Issue 2015, 11, 1–4. [Google Scholar]
- Daugherty, D.; Roque-Urrea, T.; Urrea-Roque, J.; Troyer, J.; Wirkus, S.; Porter, M.A. Mathematical models of bipolar disorder. Commun. Nonlinear Sci. Numer. Simul. 2009, 14, 2897–2908. [Google Scholar] [CrossRef][Green Version]
- Wei, S.Y.; Tseng, H.H.; Chang, H.H.; Lu, T.H.; Chang, W.H.; Chiu, N.T.; Yang, Y.K.; Chen, P.S. Dysregulation of oxytocin and dopamine in the corticostriatal circuitry in bipolar II disorder. Transl. Psychiatry 2020, 10, 281. [Google Scholar] [CrossRef] [PubMed]
- Pisanu, C.; Papadima, E.M.; Del Zompo, M.; Squassina, A. Understanding the molecular mechanisms underlying mood stabilizer treatments in bipolar disorder: Potential involvement of epigenetics. Neurosci. Lett. 2018, 669, 24–31. [Google Scholar] [CrossRef] [PubMed]
- Alloy, L.B.; Ng, T.H.; Titone, M.K.; Boland, E.M. Circadian Rhythm Dysregulation in Bipolar Spectrum Disorders. Curr. Psychiatry Rep. 2017, 19, 21. [Google Scholar] [CrossRef]
- Hellevik, K.; Gudmestad, O.T. Limit cycle oscillations at resonances. IOP Conf. Ser. Mater. Sci. Eng. 2017, 276, 1–9. [Google Scholar] [CrossRef]
- Vaidyanathan, S. Output regulation of the forced Van der Pol chaotic oscillator via adaptive control method. Int. J. PharmTech Res. 2015, 8, 106–116. [Google Scholar]
- MacCabe, J.H.; Lambe, M.P.; Cnattingius, S.; Sham, P.C.; David, A.S.; Reichenberg, A.; Murray, R.M.; Hultman, C.M. Excellent school performance at age 16 and risk of adult bipolar disorder: National cohort study. Br. J. Psychiatry 2010, 196, 109–115. [Google Scholar] [CrossRef] [PubMed]
- Karpinski, R.I.; Kinase Kolb, A.M.; Tetreault, N.A.; Borowski, T.B. High intelligence: A risk factor for psychological and physiological overexcitabilities. Intelligence 2016, 66, 8–23. [Google Scholar] [CrossRef]
- Webster, C.R.; Mahaffy, P.R.; Atreya, S.K.; Flesch, G.J. Low upper limit to methane abundance on Mars. Science 2013, 342, 355–357. [Google Scholar] [CrossRef] [PubMed]
- Durach, C.F.; Wieland, A. A New Paradigm for Systematic Literature Reviews in Supply Chain Management at Berlin. J. Supply Chain. Manag. 2017, 53, 67–85. [Google Scholar] [CrossRef]
- Riaman; Sukono; Supian, S.; Ismail, N. Mapping in the Topic of Mathematical Model in Paddy Agricultural Insurance Based on Bibliometric Analysis: A Systematic Review Approach. Computation 2022, 10, 50. [Google Scholar]
- Kalfin; Sukon; Supian, S.; Mamat, M. Insurance as an Alternative for Sustainable Economic Recovery after Natural Disasters: A Systematic Literature Review. Sustainability 2022, 14, 1–18. [Google Scholar]
- Firdaniza, F.; Ruchjana, B.N.; Chaerani, D.; Radianti, J. Information Diffusion Model in Twitter: A Systematic Literature Review. Information 2022, 13, 13. [Google Scholar] [CrossRef]
- Boell, S.K.; Cecez-kecmanovic, D. On being ‘systematic’ in literature reviews in IS. J. Inf. Technol. 2015, 2015, 161–173. [Google Scholar] [CrossRef]
- Torrent, C.; Mar Bonnin, C.D.; Martínez-Arán, A.; Valle, J.; Amann, B.L.; González-Pinto, A.; Crespo, J.M.; Ibáñez, Á.; Garcia-Portilla, M.P.; Tabarés-Seisdedos, R.; et al. Efficacy of functional remediation in bipolar disorder: A multicenter randomized controlled study. Am. J. Psychiatry 2013, 170, 852–859. [Google Scholar] [CrossRef]
- Fristad, M.A.; Davidson, K.H.; Leffler, J.M. Journal of Family Thinking-Feeling-Doing: A Therapeutic Technique for Children with Bipolar Disorder and Their Parents. J. Fam. Psychother. 2007, 18, 81–103. [Google Scholar] [CrossRef]
- Zubrick, S.R.; Hafekost, J.; Johnson, S.E.; Sawyer, M.G.; Patton, G.; Lawrence, D. The continuity and duration of depression and its relationship to non-suicidal self-harm and suicidal ideation and behavior in adolescents 12–17. J. Affect. Disord. 2017, 220, 49–56. [Google Scholar] [CrossRef]
- Newman, C.F. Reducing the risk of suicide in patients with bipolar disorder: Interventions and safeguards. Cogn. Behav. Pract. 2005, 12, 76–88. [Google Scholar] [CrossRef]
- Brereton, P.; Kitchenham, B.A.; Budgen, D.; Turner, M.; Khalil, M. Lessons from applying the systematic literature review process within the software engineering domain. J. Syst. Softw. 2007, 80, 571–583. [Google Scholar] [CrossRef]
- Priharsari, D. Systematic Literature Review Di Bidang Sistem Informasi Dan Systematic Literature Review in Information Systems and Computer Engineering: A Guideline. J. Teknol. Inf. Dan Ilmu Komput. 2022, 9, 263–268. [Google Scholar]
- van Eck, N.J.; Waltman, L. Citation-based clustering of publications using CitNetExplorer and VOSviewer. Scientometrics 2017, 111, 1053–1070. [Google Scholar] [CrossRef]
- Meng, L.; Wen, K.H.; Brewin, R.; Wu, Q. Knowledge atlas on the relationship between urban street space and residents’ health-a bibliometric analysis based on vos viewer and cite space. Sustainability 2020, 12, 2384. [Google Scholar] [CrossRef]
- Andrews, P.W.; Kornstein, S.G.; Halberstadt, L.J.; Gardner, C.O.; Neale, M.C. Blue Again: Perturbational Effects of Antidepressants Suggest Monoaminergic Homeostasis in Major Depression. Front. Psychol. 2011, 2, 159. [Google Scholar] [CrossRef] [PubMed]
- Millan, M.J.; Goodwin, G.M.; Meyer-Lindenberg, A.; Ögren, S.O. Learning from the past and looking to the future: Emerging perspectives for improving the treatment of psychiatric disorders. Eur. Neuropsychopharmacol. 2015, 25, 599–656. [Google Scholar] [CrossRef] [PubMed]
- Fountoulakis, K.N.; Yatham, L.; Grunze, H.; Vieta, E.; Young, A.; Blier, P.; Kasper, S.; Moeller, H.J. The International College of Neuro-Psychopharmacology (CINP) Treatment Guidelines for Bipolar Disorder in Adults (CINP-BD-2017), Part 2: Review, Grading of the Evidence, and a Precise Algorithm. Int. J. Neuropsychopharmacol. 2016, 20, 121–179. [Google Scholar] [CrossRef] [PubMed]
- Stevenson, M.D.; Scope, A.; Sutcliffe, P.A.; Booth, A.; Slade, P.; Parry, G.; Saxon, D.; Kalthenthaler, E. Group cognitive behavioural therapy for postnatal depression: A systematic review of clinical effectiveness, cost effectiveness and value of information analyses. Health Technol. Assess. (Rockv.) 2010, 14, 1–135. [Google Scholar] [CrossRef]
- Hemmeter, U.-M.; Hemmeter-Spernal, J.; Krieg, J.-C. Sleep deprivation in depression. Expert Rev. Neurother. 2010, 10, 1101–1115. [Google Scholar] [CrossRef] [PubMed]
- Bystritsky, A.; Nierenberg, A.A.; Feusner, J.D.; Rabinovich, M. Computational non-linear dynamical psychiatry: A new methodological paradigm for diagnosis and course of illness. J. Psychiatr. Res. 2012, 46, 428–435. [Google Scholar] [CrossRef]
- Andreassen, C.S.; Griffiths, M.D.; Sinha, R.; Hetland, J.; Pallesen, S. The Relationships between Workaholism and Symptoms of Psychiatric Disorders: A Large-Scale Cross-Sectional Study. PLoS ONE 2016, 11, e0152978. [Google Scholar] [CrossRef]
- Holmes, E.A.; Bonsall, M.B.; Hales, S.A.; Mitchell, H.; Renner, F.; Blackwell, S.E.; Watson, P.; Goodwin, G.M.; Di Simplicio, M. Applications of time-series analysis to mood fluctuations in bipolar disorder to promote treatment innovation: A case series. Transl. Psychiatry 2016, 6, e720. [Google Scholar] [CrossRef] [PubMed]
- Spina, E.; Arrigo, C.D.; Santoro, V.; Muscatello, M.R.; Pandolfo, G.; Zoccali, R.; Diaz, F.J.; de Leon, J. Effect of valproate on olanzapine plasma concentrations in patients with bipolar or schizoaffective disorder. Ther. Drug 2009, 31, 758–763. Available online: https://journals.lww.com/drug-653monitoring/Fulltext/2009/12000/Plasma_Concentrations_of_Risperidone_and.15.aspx (accessed on 19 June 2022). [CrossRef] [PubMed]
- Camara, N.F.; Binyet, E. Are Mental Disorders Brain Diseases and What Does This Mean? Brain Disord. Ther. 2017, 6, 1–5. [Google Scholar] [CrossRef]
- Stawarz, K.; Preist, C.; Tallon, D.; Wiles, N.; Kessler, D. Design considerations for the integrated delivery of cognitive behavioral therapy for depression: User-centered design study. JMIR Mental 2020, 7, e15927. Available online: https://mental.jmir.org/2020/9/e15972 (accessed on 5 July 2022). [CrossRef] [PubMed]
- Fuhr, K.; Werle, D.; Batra, A. How does early symptom change predict subsequent course of depressive symptoms during psychotherapy? Psychol. Psychother. Theory Res. Pract. 2022, 95, 137–154. [Google Scholar] [CrossRef]
- Kazdin, A.E. Evidence-based psychotherapies II: Changes in models of treatment and treatment delivery. S. Afr. J. Psychol. 2014, 45, 3–21. [Google Scholar] [CrossRef]
- Liebovitch, L.S.; Peluso, P.R.; Norman, M.D.; Su, J.; Gottman, J.M. Mathematical model of the dynamics of psychotherapy. Cogn. Neurodyn. 2011, 5, 265–275. [Google Scholar] [CrossRef] [PubMed]
- Gaebel, C.; Rittner, S.; Stoffel, M.; Jarczok, M.N.; Aguilar-Raab, C.; Ditzen, B.; Warth, M. Study protocol of the MUSED study: A randomized controlled trial to evaluate the psychobiological effects of group music therapy in women with depression. Nord. J. Music Ther. 2020, 30, 131–156. [Google Scholar] [CrossRef]
- Moore, P.J. Mathematical Modelling, Forecasting and Telemonitoring of Mood in Bipolar Disorder. 2014. Available online: http://www.maxlittle.net/students/thesis_moore.pdf (accessed on 7 June 2021).
- Baldessarini, R.J.; Tondo, L.; Visioli, C. First-episode types in bipolar disorder: Predictive associations with later illness. Acta Psychiatr. Scand. 2014, 129, 383–392. [Google Scholar] [CrossRef] [PubMed]
- Swartz, H.A.; Levenson, J.C.; Frank, E. Psychotherapy for Bipolar II Disorder: The Role of Interpersonal and Social Rhythm Therapy. Prof. Psychol. Res. Pr. 2012, 43, 145–153. [Google Scholar] [CrossRef]
- Dome, P.; Rihmer, Z.; Gonda, X. Suicide risk in bipolar disorder: A brief review. Medicina 2019, 55, 403. [Google Scholar] [CrossRef] [PubMed]
- Esaki, Y.; Obayashi, K.; Saeki, K.; Fujita, K.; Iwata, N.; Kitajima, T. Higher prevalence of intentional self-harm in bipolar disorder with evening chronotype: A finding from the APPLE cohort study. J. Affect. Disord. 2020, 277, 727–732. [Google Scholar] [CrossRef] [PubMed]
- Chatterton, M.L.; Ke, X.; Lewis, B.E.; Rajagopalan, K.; Lazarus, A. Impact of bipolar disorder on the family: Utilization and cost of health care resources. P T 2008, 33, 15–34. [Google Scholar]
- Swartz, H.A.; Swanson, J. Psychotherapy for Bipolar Disorder in Adults. Focus 2014, 12, 251–266. [Google Scholar] [CrossRef] [PubMed]
- Hoberg, A.A.; Ponto, J.; Nelson, P.J.; Frye, M.A. Group Interpersonal and Social Rhythm Therapy for Bipolar Depression. Perspect. Psychiatr. Care 2013, 49, 226–234. [Google Scholar] [CrossRef] [PubMed]
- Mayer, E.A.; Knight, R.; Mazmanian, S.K.; Cryan, J.F.; Tillisch, K. Gut microbes and the brain: Paradigm shift in neuroscience. J. Neurosci. 2014, 34, 15490–15496. [Google Scholar] [CrossRef]
- Baldessarini, R.J.; Tondo, L.; Vázquez, G.H. Pharmacological treatment of adult bipolar disorder. Mol. Psychiatry 2019, 24, 198–217. [Google Scholar] [CrossRef]
- Xue, S.; Husain, M.I.; Ortiz, A.; Husain, M.O.; Daskalakis, Z.J.; Mulsant, B.H. COVID-19: Implications for bipolar disorder clinical care and research. SAGE Open Med. 2020, 8, 205031212098117. [Google Scholar] [CrossRef] [PubMed]
- Data, O. World in Number of People with Bipolar Disorder 1990 to 2019. Available online: https://ourworldindata.org/grapher/number-with-bipolar-disorder-country?tab=chart&country=NOR~USA~England~FRA~CHE (accessed on 17 July 2022).
- Magioncalda, P.; Martino, M. A unified model of the pathophysiology of bipolar disorder. Mol. Psychiatry 2022, 27, 202–211. [Google Scholar] [CrossRef] [PubMed]
- Fountoulakis, K.N.; Siamouli, M. Re: How well do psychosocial interventions work in bipolar disorder? Can. J. Psychiatry. 2009, 54, 578. [Google Scholar] [CrossRef] [PubMed]
- Borsboom, D. A network theory of mental disorders. World Psychiatry 2017, 16, 5–13. [Google Scholar] [CrossRef] [PubMed]
- Avasthi, A.; Varma, S.C.; Kulhara, P.; Nehra, R.; Grover, S.; Sharma, S. Diagnosis of common mental disorders by using PRIME-MD Patient Health Questionnaire. Indian J. Med. Res. 2008, 127, 159–164. [Google Scholar]

| Keywords Screening | Type | Science Direct | Dimensions | Google Scholar |
|---|---|---|---|---|
| Keyword 1 | MM and BD | 149 | 2086 | 1960 |
| Keyword 2 | MM and BD and T | 6 | 305 | 96 |
| Keyword 3 | MM and BD and T and I | 5 | 289 | 76 |
| Author | Indexed | Keywords | Citation | Focus |
|---|---|---|---|---|
| PW Andrews, et al. (2011) [32] | Scopus Q1 | Major depressive disorder, neurochemical disorder, antidepressant drug therapy, meta-analysis of studies | 156 | tested the prediction of revival of depressive symptoms comparable to the effect of ADM disorder by conducting a meta-analysis of ADM discontinuation studies. |
| MJ Millan, et al. (2015) [33] | Scopus Q1 | Neuropsychopharmacology, pharmacotherapy, therapy | 92 | Neuropsychopharmacology enhancement increased prevention and assistance of psychiatric disorders. |
| AS Wedge et al. (2022) [1] | Scopus Q1 | Deep brain stimulation, Psychiatric illness, Psychiatric diagnosis, Functional imaging, Anxiety disorders, Electrophysiology, Modeling, Local field potential, Mood disorders. | 65 | developed a closed-loop DBS system by correcting dysfunctional activity in the brain circuits underlying the domain. |
| J. Phillips et al. (2012) [8] | Scopus Q1 | Diagnostic and Statistical Manual of Mental Disorders, diagnostic category | 62 | Development of DSM and DSM-5 in mental disorder and diagnostic category |
| KN Fountoulakis et al. (2016) [34] | Scopus Q1 | Bipolar disorder; Anticonvulsants; Antidepressants; Treatments; Clinical; Clinical trials | 62 | systematic literature search, detailed presentation of results, and assessment of treatment options in terms of efficacy and tolerability/safety BD. |
| MD Stevenson et al. (2010) [35] | Scopus Q1 | Group cognitive behavioral therapy, postnatal depression, clinical effectiveness, cost-effectiveness, value of information analyses | 60 | support the use of cognitive behavior therapy (CBT) in the treatment of depression, and psychological therapies as a first-line treatment for PND. |
| U.-M. Hemmeter, et al. (2010) [36] | Scopus Q1 | depression, dopamine, GABA, microsleep, naps, neuroimaging, serotonin, sleep deprivation, sleep EEG, sleep endocrinoloy, sleep regulation | 51 | sleep deprivation problems in depressed patients and the use of antidepressant drugs as well as neurobiological aspects of sleep and SD (sleep EEG, neuroendocrinology, neurochemistry, and chronobiology.) |
| Bystritsky, A (2012) [37] | Scopus Q1 | Phenomenology, Mathematical models, Non-linear dynamics, Winner less competition Psychopathology | 51 | highlights the significant potential benefits of applying computational mathematical models to the field of psychiatry, particularly in relation to diagnostic conceptualization. |
| CS Andreassen, et al. (2016) [38] | Scopus Q1 | Workaholism, a cross-sectional survey based on the web, Symptoms of Psychiatric Disorders | 51 | assessing symptoms of psychiatric disorders and work addiction. |
| EA Holmes et al. (2016) [39] | Scopus Q1 | BD, mood fluctuations, treatment innovation, MAPP; Mood Action Psychology Program | 42 | Innovative treatment for bipolar disorder. |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Nursuprianah, I.; Anggriani, N.; Nuraini, N.; Rosandi, Y. Mathematical Model of Interaction of Therapist and Patients with Bipolar Disorder: A Systematic Literature Review. J. Pers. Med. 2022, 12, 1469. https://doi.org/10.3390/jpm12091469
Nursuprianah I, Anggriani N, Nuraini N, Rosandi Y. Mathematical Model of Interaction of Therapist and Patients with Bipolar Disorder: A Systematic Literature Review. Journal of Personalized Medicine. 2022; 12(9):1469. https://doi.org/10.3390/jpm12091469
Chicago/Turabian StyleNursuprianah, Indah, Nursanti Anggriani, Nuning Nuraini, and Yudi Rosandi. 2022. "Mathematical Model of Interaction of Therapist and Patients with Bipolar Disorder: A Systematic Literature Review" Journal of Personalized Medicine 12, no. 9: 1469. https://doi.org/10.3390/jpm12091469
APA StyleNursuprianah, I., Anggriani, N., Nuraini, N., & Rosandi, Y. (2022). Mathematical Model of Interaction of Therapist and Patients with Bipolar Disorder: A Systematic Literature Review. Journal of Personalized Medicine, 12(9), 1469. https://doi.org/10.3390/jpm12091469