Corrected Allele Frequency of BRCA1/2 Mutations Is an Independent Prognostic Factor for Treatment Response to PARP-Inhibitors in Ovarian Cancer Patients
Abstract
1. Introduction
2. Materials and Methods
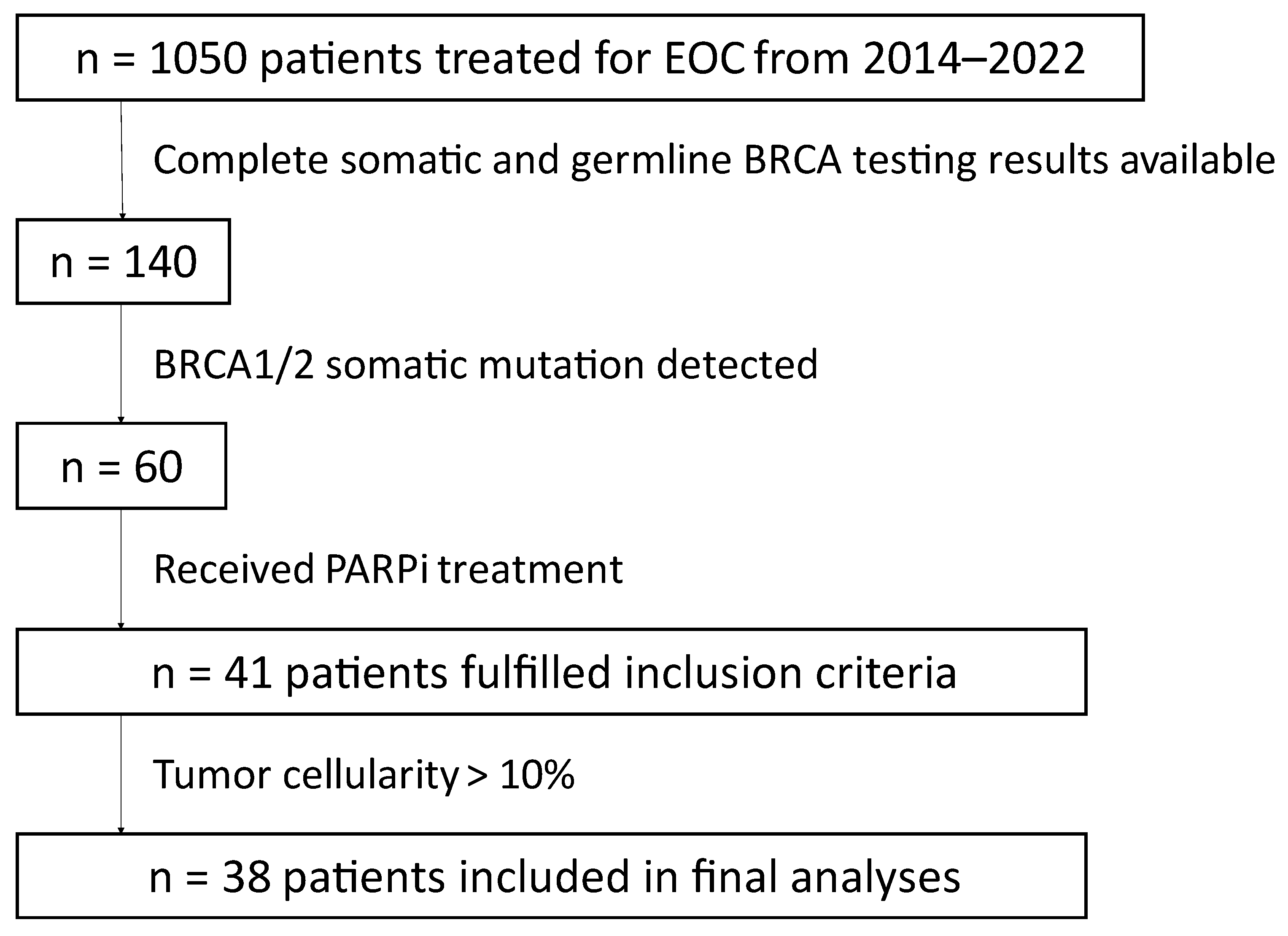
2.1. Study Population
2.2. BRCA Germline Testing
2.3. BRCA Tumor Testing
2.4. Calculation of Corrected Allele Frequency
2.5. Statistical Analysis
3. Results
3.1. Patient Characteristics
3.2. BRCA Testing
3.3. PARPi Treatment
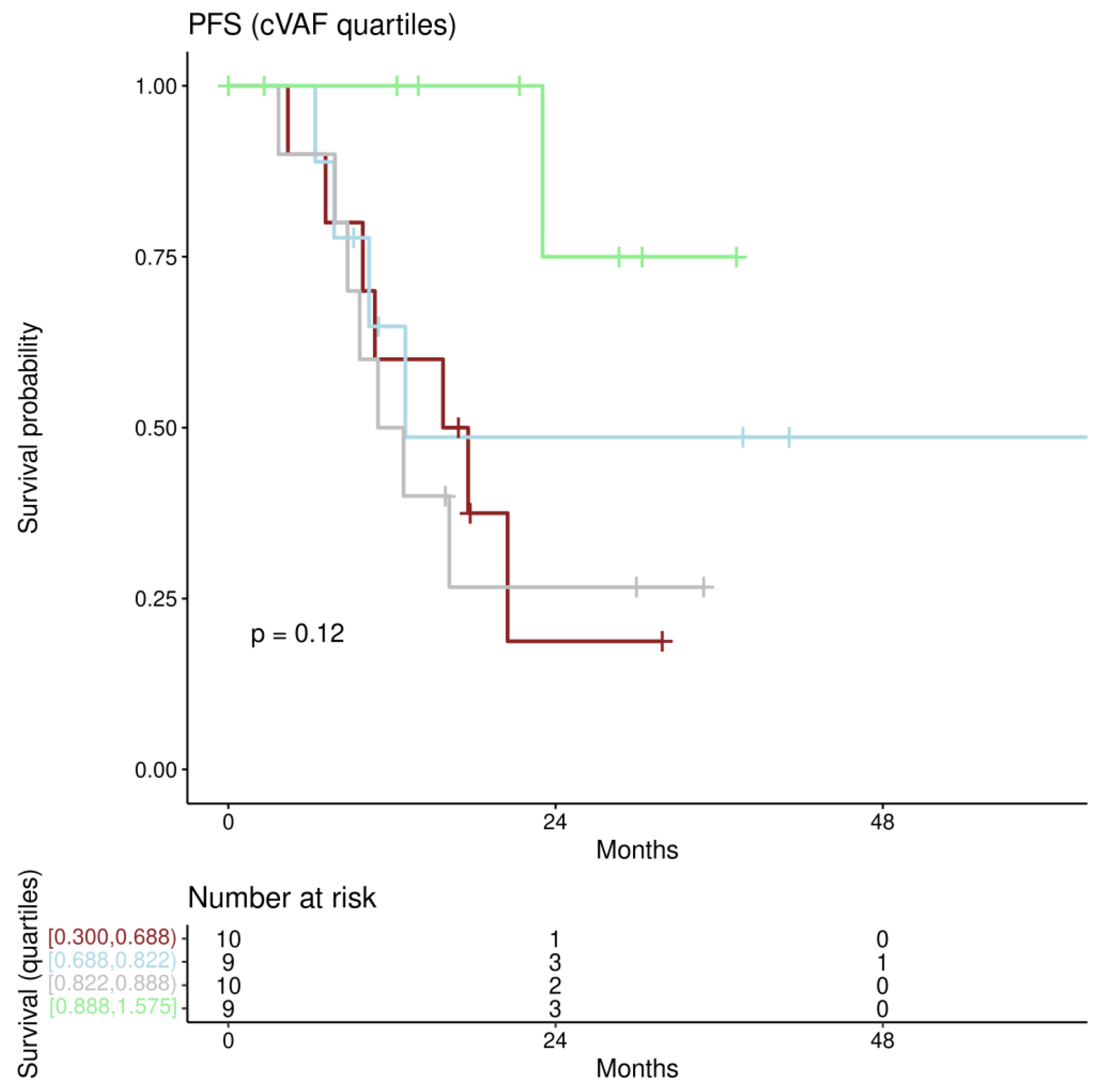
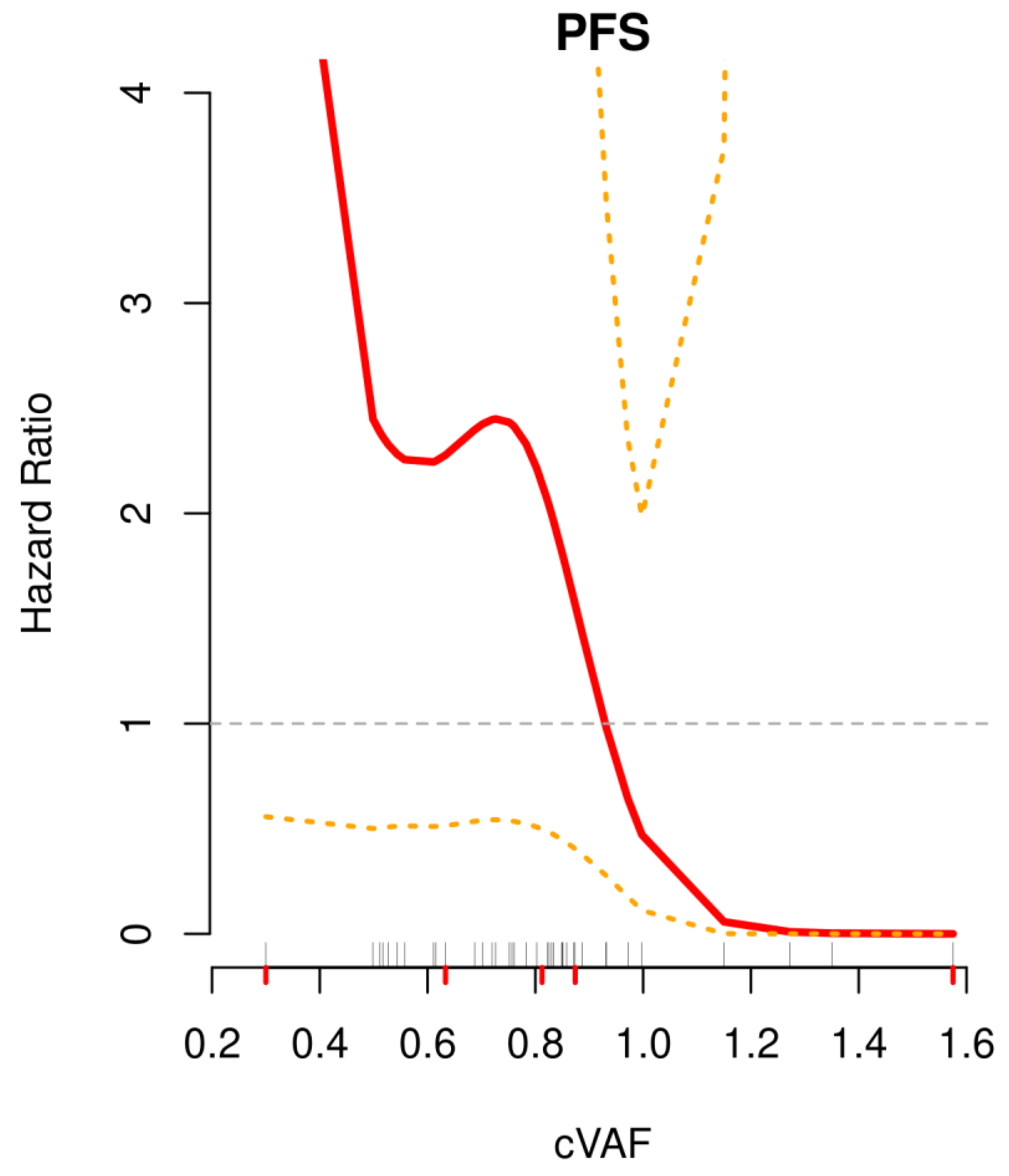
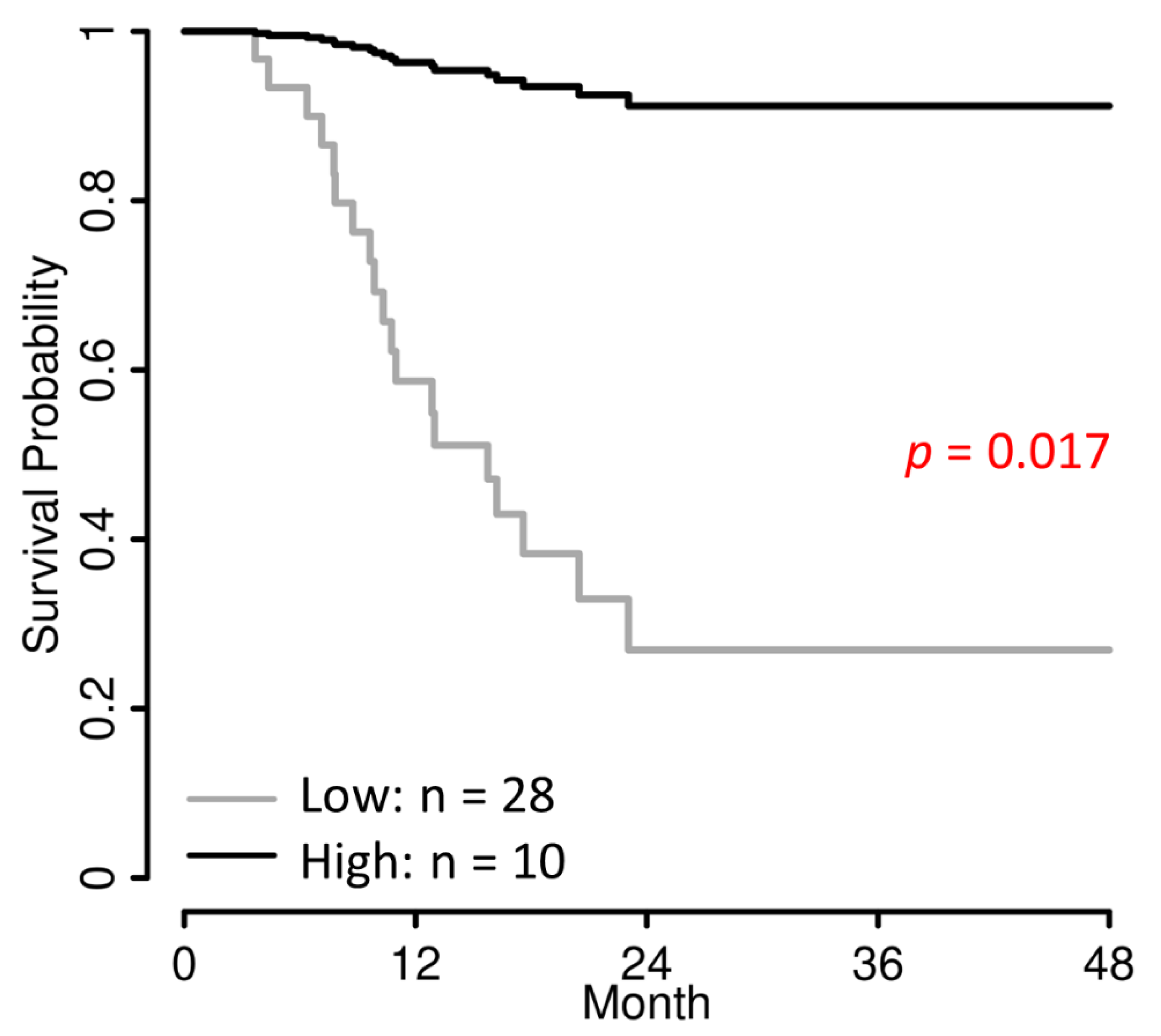
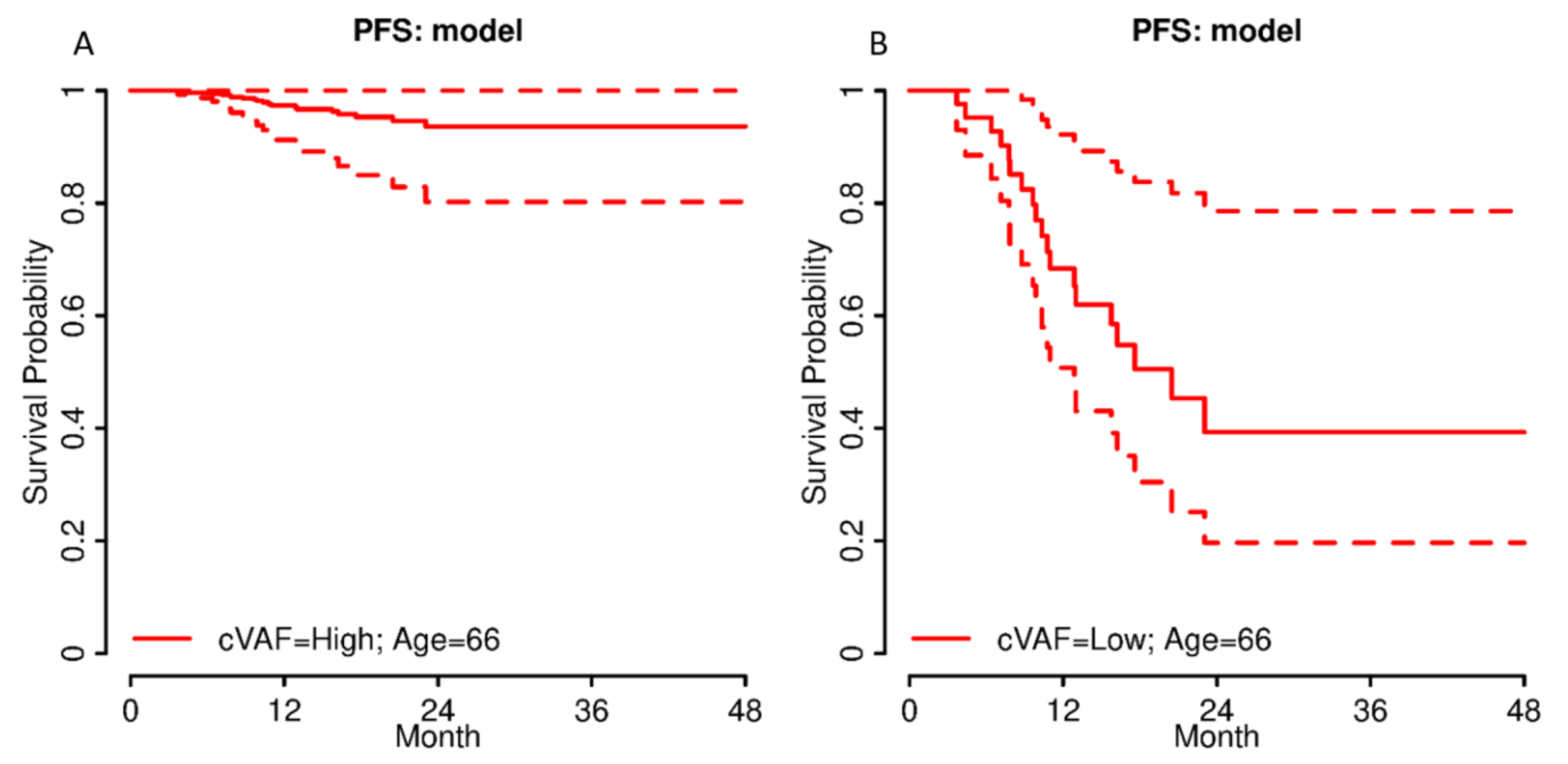
3.4. Progression-Free Survival
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Siegel, R.L.; Miller, K.D.; Jemal, A. Cancer Statistics. CA Cancer J. Clin. 2020, 70, 7–30. [Google Scholar] [CrossRef]
- Antoniou, A.; Pharoah, P.D.; Narod, S.; Risch, H.A.; Eyfjord, J.E.; Hopper, J.L.; Loman, N.; Olsson, H.; Johannsson, O.; Borg, Å.; et al. Average risks of breast and ovarian cancer associated with BRCA1 or BRCA2 mutations detected in case Series unselected for family history: A combined analysis of 22 studies. Am. J. Hum. Genet. 2003, 72, 1117–1130. [Google Scholar] [CrossRef]
- Sowter, H.M.; Ashworth, A. BRCA1 and BRCA2 as ovarian cancer susceptibility genes. Carcinogenesis 2005, 26, 1651–1656. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Norquist, B.M.; Harrell, M.I.; Brady, M.F.; Walsh, T.; Lee, M.K.; Gulsuner, S.; Bernards, S.S.; Casadei, S.; Yi, Q.; Burger, R.A.; et al. Inherited Mutations in Women with Ovarian Carcinoma. JAMA Oncol. 2016, 2, 482–490. [Google Scholar] [CrossRef] [PubMed]
- Zhang, S.; Royer, R.; Li, S.; McLaughlin, J.R.; Rosen, B.; Risch, H.A.; Fan, I.; Bradley, L.; Shaw, P.A.; Narod, S.A. Frequencies of BRCA1 and BRCA2 mutations among 1342 unselected patients with invasive ovarian cancer. Gynecol. Oncol. 2011, 121, 353–357. [Google Scholar] [CrossRef] [PubMed]
- Turashvili, G.; Lazaro, C.; Ying, S.; Charames, G.; Wong, A.; Hamilton, K.; Yee, D.; Agro, E.; Chang, M.; Pollett, A.; et al. Tumor BRCA Testing in High Grade Serous Carcinoma: Mutation Rates and Optimal Tissue Requirements. Cancers 2020, 12, 3468. [Google Scholar] [CrossRef]
- Weren, R.D.; Mensenkamp, A.R.; Simons, M.; Eijkelenboom, A.; Sie, A.S.; Ouchene, H.; van Asseldonk, M.; Gomez-Garcia, E.B.; Blok, M.J.; de Hullu, J.A.; et al. Novel BRCA1 and BRCA2 Tumor Test as Basis for Treatment Decisions and Referral for Genetic Counselling of Patients with Ovarian Carcinomas. Hum. Mutat. 2016, 38, 226–235. [Google Scholar] [CrossRef] [PubMed]
- Rezaei, N.; Hedayat, M. Allele Frequency. In Brenner’s Encyclopedia of Genetics, 2nd ed.; Maloy, S., Hughes, K., Eds.; Academic Press: Cambridge, MA, USA, 2013; pp. 77–78. [Google Scholar]
- Moore, K.; Colombo, N.; Scambia, G.; Kim, B.-G.; Oaknin, A.; Friedlander, M.; Lisyanskaya, A.; Floquet, A.; Leary, A.; Sonke, G.S.; et al. Maintenance Olaparib in Patients with Newly Diagnosed Advanced Ovarian Cancer. N. Engl. J. Med. 2018, 379, 2495–2505. [Google Scholar] [CrossRef] [PubMed]
- González-Martín, A.; Pothuri, B.; Vergote, I.; DePont Christensen, R.; Graybill, W.; Mirza, M.R.; McCormick, C.; Lorusso, D.; Hoskins, P.; Freyer, G.; et al. Niraparib in Patients with Newly Diagnosed Advanced Ovarian Cancer. N. Engl. J. Med. 2019, 381, 2391–2402. [Google Scholar] [CrossRef] [PubMed]
- Fong, P.C.; Yap, T.A.; Boss, D.S.; Carden, C.P.; Mergui-Roelvink, M.; Gourley, C.; De Greve, J.; Lubinski, J.; Shanley, S.; Messiou, C.; et al. Poly(ADP)-ribose polymerase inhibition: Frequent durable responses in BRCA carrier ovarian cancer correlating with platinum-free interval. J. Clin. Oncol. 2010, 28, 2512–2519. [Google Scholar] [CrossRef]
- Penson, R.T.; Valencia, R.V.; Cibula, D.; Colombo, N.; Leath, C.A., 3rd; Bidzinski, M.; Kim, J.W.; Nam, J.H.; Madry, R.; Hernandez, C.; et al. Olaparib Versus Nonplatinum Chemotherapy in Patients with Platinum-Sensitive Relapsed Ovarian Cancer and a Germline BRCA1/2 Mutation (SOLO3): A Randomized Phase III Trial. J. Clin. Oncol. 2020, 38, 1164–1174. [Google Scholar] [CrossRef] [PubMed]
- Oza, A.M.; Tinker, A.V.; Oaknin, A.; Shapira-Frommer, R.; McNeish, I.A.; Swisher, E.M.; Ray-Coquard, I.; Bell-McGuinn, K.; Coleman, R.L.; O’Malley, D.M.; et al. Antitumor activity and safety of the PARP inhibitor rucaparib in patients with high-grade ovarian carcinoma and a germline or somatic BRCA1 or BRCA2 mutation: Integrated analysis of data from Study 10 and ARIEL2. Gynecol. Oncol. 2017, 147, 267–275. [Google Scholar] [CrossRef]
- Li, H.; Liu, Z.-Y.; Wu, N.; Chen, Y.-C.; Cheng, Q.; Wang, J. PARP inhibitor resistance: The underlying mechanisms and clinical implications. Mol. Cancer 2020, 19, 107. [Google Scholar] [CrossRef]
- Janysek, D.C.; Kim, J.; Duijf, P.H.; Dray, E. Clinical use and mechanisms of resistance for PARP inhibitors in homologous recombination-deficient cancers. Transl. Oncol. 2021, 14, 101012. [Google Scholar] [CrossRef]
- Wolford, J.E.; Bai, J.; Moore, K.N.; Kristeleit, R.; Monk, B.J.; Tewari, K.S. Cost-effectiveness of niraparib, rucaparib, and olaparib for treatment of platinum-resistant, recurrent ovarian carcinoma. Gynecol. Oncol. 2020, 157, 500–507. [Google Scholar] [CrossRef] [PubMed]
- Muston, D.; Hettle, R.; Monberg, M.; McLaurin, K.K.; Gao, W.; Swallow, E.; Zhang, S.; Kalemaj, I.; Signorovitch, J.; Moore, K. Cost-effectiveness of olaparib as a maintenance treatment for women with newly diagnosed advanced ovarian cancer and BRCA1/2 mutations in the United States. Gynecol. Oncol. 2020, 159, 491–497. [Google Scholar] [CrossRef] [PubMed]
- Bitler, B.G.; Watson, Z.L.; Wheeler, L.J.; Behbakht, K. PARP inhibitors: Clinical utility and possibilities of overcoming resistance. Gynecol. Oncol. 2017, 147, 695–704. [Google Scholar] [CrossRef] [PubMed]
- LaFargue, C.J.; Molin, G.Z.D.; Sood, A.K.; Coleman, R.L. Exploring and comparing adverse events between PARP inhibitors. Lancet Oncol. 2019, 20, e15–e28. [Google Scholar] [CrossRef]
- Morice, P.-M.; Leary, A.; Dolladille, C.; Chrétien, B.; Poulain, L.; González-Martín, A.; Moore, K.; O’Reilly, E.M.; Ray-Coquard, I.; Alexandre, J. Myelodysplastic syndrome and acute myeloid leukaemia in patients treated with PARP inhibitors: A safety meta-analysis of randomised controlled trials and a retrospective study of the WHO pharmacovigilance database. Lancet Haematol. 2021, 8, e122–e134. [Google Scholar] [CrossRef]
- Bekos, C.; Grimm, C.; Kranawetter, M.; Polterauer, S.; Oberndorfer, F.; Tan, Y.; Müllauer, L.; Singer, C. Reliability of Tumor Testing Compared to Germline Testing for Detecting BRCA1 and BRCA2 Mutations in Patients with Epithelial Ovarian Cancer. J. Pers. Med. 2021, 11, 593. [Google Scholar] [CrossRef] [PubMed]
- Kanchi, K.L.; Johnson, K.J.; Lu, C.; McLellan, M.D.; Leiserson, M.D.M.; Wendl, M.C.; Zhang, Q.; Koboldt, D.C.; Xie, M.; Kandoth, C.; et al. Integrated analysis of germline and somatic variants in ovarian cancer. Nat. Commun. 2014, 5, 3156. [Google Scholar] [CrossRef]
- Li, X.-M.; Yang, J.-J.; Wu, Y.-L. Association of allele frequency of EGFR mutation with efficacy of EGFR TKIs in advanced non-small cell lung cancer. J. Clin. Oncol. 2019, 37, e20678. [Google Scholar] [CrossRef]
- Al-Dherasi, A.; Liao, Y.; Al-Mosaib, S.; Hua, R.; Wang, Y.; Yu, Y.; Zhang, Y.; Zhang, X.; Jalayta, R.; Mousa, H.; et al. Allele frequency deviation (AFD) as a new prognostic model to predict overall survival in lung adenocarcinoma (LUAD). Cancer Cell Int. 2021, 21, 451. [Google Scholar] [CrossRef] [PubMed]
- Ma, J.; Fu, Y.; Tu, Y.-Y.; Liu, Y.; Tan, Y.-R.; Ju, W.-T.; Pickering, C.R.; Myers, J.N.; Zhang, Z.-Y.; Zhong, L.-P. Mutation allele frequency threshold does not affect prognostic analysis using next-generation sequencing in oral squamous cell carcinoma. BMC Cancer 2018, 18, 758. [Google Scholar] [CrossRef] [PubMed]
- Tian, J.; Geng, Y.; Lv, D.; Li, P.; Cordova-Delgado, M.; Liao, Y.; Tian, X.; Zhang, X.; Zhang, Q.; Zou, K.; et al. Using plasma cell-free DNA to monitor the chemoradiotherapy course of cervical cancer. Int. J. Cancer 2019, 145, 2547–2557. [Google Scholar] [CrossRef]
- Stagni, C.; Zamuner, C.; Elefanti, L.; Zanin, T.; Del Bianco, P.; Sommariva, A.; Fabozzi, A.; Pigozzo, J.; Mocellin, S.; Montesco, M.C.; et al. BRAF Gene Copy Number and Mutant Allele Frequency Correlate with Time to Progression in Metastatic Melanoma Patients Treated with MAPK Inhibitors. Mol. Cancer Ther. 2018, 17, 1332–1340. [Google Scholar] [CrossRef]
- Friedlaender, A.; Tsantoulis, P.; Chevallier, M.; De Vito, C.; Addeo, A. The Impact of Variant Allele Frequency in EGFR Mutated NSCLC Patients on Targeted Therapy. Front. Oncol. 2021, 11, 644472. [Google Scholar] [CrossRef]
- Zheng, Q.; Hong, S.; Huang, Y.; Zhao, H.; Yang, Y.; Hou, X.; Zhao, Y.; Ma, Y.; Zhou, T.; Zhang, Y.; et al. EGFR T790M relative mutation purity predicts osimertinib treatment efficacy in non-small cell lung cancer patients. Clin. Transl. Med. 2020, 9, 17. [Google Scholar] [CrossRef] [PubMed]
- Berrino, E.; Balsamo, A.; Pisacane, A.; Gallo, S.; Becco, P.; Miglio, U.; Caravelli, D.; Poletto, S.; Paruzzo, L.; Debernardi, C.; et al. High BRAF variant allele frequencies are associated with distinct pathological features and responsiveness to target therapy in melanoma patients. ESMO Open 2021, 6, 100133. [Google Scholar] [CrossRef]
- Mohyuddin, G.R.; Aziz, M.; Britt, A.; Wade, L.; Sun, W.; Baranda, J.; Al-Rajabi, R.; Saeed, A.; Kasi, A. Similar response rates and survival with PARP inhibitors for patients with solid tumors harboring somatic versus Germline BRCA mutations: A Meta-analysis and systematic review. BMC Cancer 2020, 20, 507. [Google Scholar] [CrossRef]
- Francis, K.; Kim, S.; Friedlander, M.; Gebski, V.; Ray-Coquard, I.; Clamp, A.; Penson, R.; Oza, A.; Perri, T.; Huzarski, T.; et al. The impact of olaparib dose reduction and treatment interruption on treatment outcome in the SOLO2/ENGOT-ov21 platinum-sensitive recurrent ovarian cancer. Ann. Oncol. 2022, 33, 593–601. [Google Scholar] [CrossRef] [PubMed]
- Norquist, B.; Wurz, K.A.; Pennil, C.C.; Garcia, R.; Gross, J.; Sakai, W.; Karlan, B.Y.; Taniguchi, T.; Swisher, E.M. Secondary somatic mutations restoring BRCA1/2 predict chemotherapy resistance in hereditary ovarian carcinomas. J. Clin. Oncol. 2011, 29, 3008–3015. [Google Scholar] [CrossRef]
- Swisher, E.M.; Sakai, W.; Karlan, B.Y.; Wurz, K.; Urban, N.; Taniguchi, T. Secondary BRCA1 mutations in BRCA1-mutated ovarian carcinomas with platinum resistance. Cancer Res. 2008, 68, 2581–2586. [Google Scholar] [CrossRef] [PubMed]
- Sakai, W.; Swisher, E.M.; Karlan, B.Y.; Agarwal, M.K.; Higgins, J.; Friedman, C.; Villegas, E.; Jacquemont, C.; Farrugia, D.J.; Couch, F.J.; et al. Secondary mutations as a mechanism of cisplatin resistance in BRCA2-mutated cancers. Nature 2008, 451, 1116–1120. [Google Scholar] [CrossRef] [PubMed]

| Parameter | Variable | n (%) |
|---|---|---|
| Histology | Serous | 35 (92.1%) |
| Endometrioid | 3 (7.9%) | |
| Grade | high-grade | 38 (100.0%) |
| FIGO stage at initial diagnosis | II | 1 (2.6%) |
| III | 27 (71.1%) | |
| IV | 10 (26.3%) | |
| Primary treatment | NACT + IDS | 13 (34.2%) |
| PDS + adj. CHT | 25 (65.8%) | |
| PARPi | Olaparib | 32 (84.2%) |
| Niraparib | 4 (10.5%) | |
| Rucaparib | 2 (5.3%) | |
| PARPi Treatment line | 1 | 12 (31.6%) |
| 2 | 20 (52.6%) | |
| 3 | 1 (2.6%) | |
| 4 | 3 (7.9%) | |
| 5 | 2 (5.3%) |
| Germline Mutation | Germline Wild-Type | |||
|---|---|---|---|---|
| BRCA1 | BRCA2 | |||
| Somatic mutation | BRCA1 (n = 25) | 22 | 0 | 3 |
| BRCA2 (n = 13) | 0 | 10 | 3 | |
| 22 | 10 | 6 | ||
| Parameters (n = 38, 19 Events) | Univariate HR [95% CI] | p-Value | Multiple HR [95% CI] | p-Value |
|---|---|---|---|---|
| cVAF | 0.11 [0.02–0.86] | 0.035 | 0.07 [0.01–0.63] | 0.017 |
| Age 1 | 0.99 [0.96–1.03] | 0.733 | 0.96 [0.91–1.01] | 0.145 |
| Therapy-line | 1.21 [0.83–1.78] | 0.327 | - 4 | - |
| FIGO at initial diagnosis 2 | 1.02 [0.37–2.86] | 0.964 | - 4 | - |
| Histology 3 | 0.43 [0.05–3.49] | 0.428 | - 4 | - |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Grech, C.T.; Pils, D.; Aust, S.; Grimm, C.; Polterauer, S.; Reinthaller, A.; Müllauer, L.; Reischer, T.; Bekos, C. Corrected Allele Frequency of BRCA1/2 Mutations Is an Independent Prognostic Factor for Treatment Response to PARP-Inhibitors in Ovarian Cancer Patients. J. Pers. Med. 2022, 12, 1467. https://doi.org/10.3390/jpm12091467
Grech CT, Pils D, Aust S, Grimm C, Polterauer S, Reinthaller A, Müllauer L, Reischer T, Bekos C. Corrected Allele Frequency of BRCA1/2 Mutations Is an Independent Prognostic Factor for Treatment Response to PARP-Inhibitors in Ovarian Cancer Patients. Journal of Personalized Medicine. 2022; 12(9):1467. https://doi.org/10.3390/jpm12091467
Chicago/Turabian StyleGrech, Christina T., Dietmar Pils, Stefanie Aust, Christoph Grimm, Stephan Polterauer, Alexander Reinthaller, Leonhard Müllauer, Theresa Reischer, and Christine Bekos. 2022. "Corrected Allele Frequency of BRCA1/2 Mutations Is an Independent Prognostic Factor for Treatment Response to PARP-Inhibitors in Ovarian Cancer Patients" Journal of Personalized Medicine 12, no. 9: 1467. https://doi.org/10.3390/jpm12091467
APA StyleGrech, C. T., Pils, D., Aust, S., Grimm, C., Polterauer, S., Reinthaller, A., Müllauer, L., Reischer, T., & Bekos, C. (2022). Corrected Allele Frequency of BRCA1/2 Mutations Is an Independent Prognostic Factor for Treatment Response to PARP-Inhibitors in Ovarian Cancer Patients. Journal of Personalized Medicine, 12(9), 1467. https://doi.org/10.3390/jpm12091467










