Comparison of the Post-Surgical Position of the Temporomandibular Joint after Orthognathic Surgery in Skeletal Class III Patients and Patients with Cleft Lip and Palate
Abstract
:1. Introduction
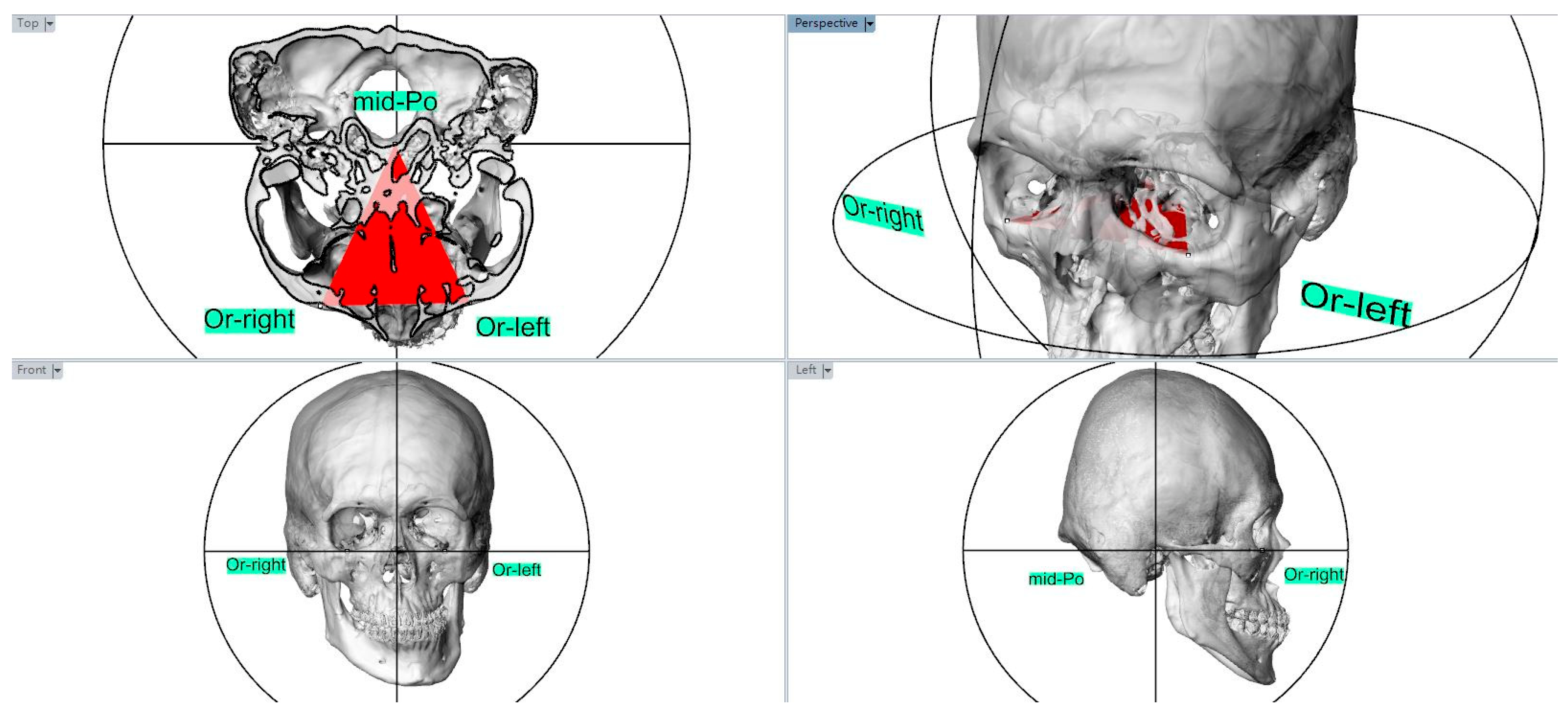
2. Materials and Methods
Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Vandeput, A.S.; Verhelst, P.J.; Jacobs, R.; Shaheen, E.; Swennen, G.; Politis, C. Condylar changes after orthognathic surgery for class III dentofacial deformity: A systematic review. Int. J. Oral Maxillofac. Surg. 2019, 48, 193–202. [Google Scholar] [CrossRef] [PubMed]
- Hoppenreijs, T.J.; Freihofer, H.P.M.; Stoelinga, P.J.; Tuinzing, D.B.; van’t Hof, M.A. Condylar remodelling and resorption after Le Fort I and bimaxillary osteotomies in patients with anterior open bite. A clinical and radiological study. Int. J. Oral Maxillofac. Surg. 1998, 27, 81–91. [Google Scholar] [CrossRef]
- Arnett, G.W.; Milam, S.B.; Gottesman, L. Progressive mandibular retrusion—Idiopathic condylar resorption. Part I. Am. J. Orthod Dentofac. Orthop. 1996, 110, 8–15. [Google Scholar] [CrossRef]
- Sanromán, J.F.; Gonzalez, J.G.; Del Hoyo, J.A.; Gil, F.M. Morphometric and morphological changes in the temporomandibular joint after orthognathic surgery: A magnetic resonance imaging and computed tomography prospective study. J. Cranio-Maxillofac. Surg. 1997, 25, 139–148. [Google Scholar] [CrossRef]
- Thongdee, P.; Samman, N. Stability of Maxillary Surgical Movement in Unilateral Cleft Lip and Palate with Preceding Alveolar Bone Grafting. Cleft Palate-Craniofacial J. 2005, 42, 664–674. [Google Scholar] [CrossRef] [PubMed]
- Daimaruya, T.; Imai, Y.; Kochi, S.; Tachi, M.; Takano-Yamamoto, T. Midfacial changes through distraction osteogenesis using a rigid external distraction system with retention plates in cleft lip and palate patients. J. Oral Maxillofac. Surg. 2010, 68, 1480–1486. [Google Scholar] [CrossRef] [PubMed]
- Chua, H.D.P.; Hägg, M.B.; Cheung, L.K. Cleft maxillary distraction versus orthognathic surgery—Which one is more stable in 5 years? Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endodontology 2010, 109, 803–814. [Google Scholar] [CrossRef] [PubMed]
- Hirano, A.; Suzuki, H. Factors Related to Relapse after Le Fort I Maxillary Advancement Osteotomy in Patients with Cleft Lip and Palate. Cleft Palate-Craniofacial J. 2001, 38, 1–10. [Google Scholar] [CrossRef]
- Heliövaara, A.; Ranta, R.; Hukki, J.; Rintala, A. Skeletal stability of Le Fort I osteotomy in patients with isolated cleft palate and bilateral cleft lip and palate. Int. J. Oral Maxillofac. Surg. 2002, 31, 358–363. [Google Scholar] [CrossRef]
- Park, Y.H.; Seo, J.H.; Yang, I.H.; Choi, J.Y.; Lee, J.H.; Kim, M.J.; Baek, S.H. What Are the Contributing Factors for Postsurgical Relapse After Two-Jaw Surgery in Patients with Cleft Lip and Palate. J. Craniofac. Surg. 2017, 28, 1071–1077. [Google Scholar] [CrossRef]
- Saltaji, H.; Major, M.P.; Alfakir, H.; Al-Saleh, M.A.; Flores-Mir, C. Maxillary advancement with conventional orthognathic surgery in patients with cleft lip and palate: Is it a stable technique? J. Oral Maxillofac. Surg. 2012, 70, 2859–2866. [Google Scholar] [CrossRef] [PubMed]
- Chang, Y.J.; Ruellas, A.C.O.; Yatabe, M.S.; Westgate, P.M.; Cevidanes, L.H.; Huja, S.S. Soft Tissue Changes Measured with Three-Dimensional Software Provides New Insights for Surgical Predictions. J. Oral Maxillofac. Surg. 2017, 75, 2191–2201. [Google Scholar] [CrossRef] [PubMed]
- Ruellas, A.C.; Tonello, C.; Gomes, L.R.; Yatabe, M.S.; Macron, L.; Lopinto, J.; Cevidanes, L.H. Common 3-dimensional coordinate system for assessment of directional changes. Am. J. Orthod Dentofac. Orthop. 2016, 149, 645–656. [Google Scholar] [CrossRef] [PubMed]
- Wang, L.C.; Lee, Y.H.; Tsai, C.Y.; Wu, T.J.; Teng, Y.Y.; Lai, J.P.; Lin, S.S.; Chang, Y.J. Postsurgical Stability of Temporomandibular Joint of Skeletal Class III Patients Treated with 2-Jaw Orthognathic Surgery via Computer-Aided Three-Dimensional Simulation and Navigation in Orthognathic Surgery (CASNOS). BioMed Res. Int. 2021, 2021, 1563551. [Google Scholar] [CrossRef]
- An, S.B.; Park, S.B.; Kim, Y.I.; Son, W.S. Effect of post-orthognathic surgery condylar axis changes on condylar morphology as determined by 3-dimensional surface reconstruction. Angle Orthod. 2014, 84, 316–321. [Google Scholar] [CrossRef]
- Ha, M.H.; Kim, Y.I.; Park, S.B.; Kim, S.S.; Son, W.S. Cone-beam computed tomographic evaluation of the condylar remodeling occurring after mandibular set-back by bilateral sagittal split ramus osteotomy and rigid fixation. Korean J. Orthod. 2013, 43, 263–270. [Google Scholar] [CrossRef]
- Park, S.B.; Yang, Y.M.; Kim, Y.I.; Cho, B.H.; Jung, Y.H.; Hwang, D.S. Effect of bimaxillary surgery on adaptive condylar head remodeling: Metric analysis and image interpretation using cone-beam computed tomography volume superimposition. J. Oral Maxillofac. Surg. 2012, 70, 1951–1959. [Google Scholar] [CrossRef]
- Katsumata, A.; Nojiri, M.; Fujishita, M.; Ariji, Y.; Ariji, E.; Langlais, R.P. Condylar head remodeling following mandibular setback osteotomy for prognathism: A comparative study of different imaging modalities. Oral Surg. Oral Med. Oral Pathol Oral Radiol. Endod. 2006, 101, 505–514. [Google Scholar] [CrossRef]
- Hochban, W.; Ganß, C.; Austermann, K.H. Long-Term Results after Maxillary Advancement in Patients with Clefts. Cleft Palate-Craniofacial J. 1993, 30, 237–243. [Google Scholar] [CrossRef]
- Figueroa, A.A.; Polley, J.W.; Friede, H.; Ko, E.W. Long-term skeletal stability after maxillary advancement with distraction osteogenesis using a rigid external distraction device in cleft maxillary deformities. Plast. Reconstr. Surg. 2004, 114, 1382–1392. [Google Scholar] [CrossRef]
- Chen, S.; Lei, J.; Wang, X.; Fu, K.Y.; Farzad, P.; Yi, B. Short- and Long-Term Changes of Condylar Position After Bilateral Sagittal Split Ramus Osteotomy for Mandibular Advancement in Combination with Le Fort I Osteotomy Evaluated by Cone-Beam Computed Tomography. J. Oral Maxillofac. Surg. 2013, 71, 1956–1966. [Google Scholar] [CrossRef] [PubMed]
- Harris, M.D.; Van Sickels, J.R.; Alder, M. Factors influencing condylar position after the bilateral sagittal split osteotomy fixed with bicortical screws. J. Oral Maxillofac. Surg. 1999, 57, 650–654. [Google Scholar] [CrossRef]



| Group 1 | Group 2 | ||||
|---|---|---|---|---|---|
| Sex | Amount | Mean Age (years) | Sex | Amount | Mean Age (years) |
| Male | 11 | 24.9 ± 4.5 years (range: 20~33 years) | Male | 14 | 19.5 ± 2.5 years (range: 18~21 years) |
| Female | 12 | 23.92 ± 5.2 years (range: 19~36 years) | Female | 6 | 19.2 ± 2.3 years (range: 19~22 years) |
| Total | 23 | 24.39 ± 4.8 years (range: 19~36 years) | Total | 20 | 20.25 ± 3.8 years (range: 18~22 years) |
| Group 1 | Group 2 | ||||
|---|---|---|---|---|---|
| Measurement | Mean Value ± SD Pre-Surgery | Mean Value ± SD Post-Surgery | Measurement | Mean Value ± SD Pre-Surgery | Mean Value ± SD Post-Surgery |
| SNA | 79.3 ± 1.5° | 83.7 ± 1.3° | SNA | 76.1 ± 4.1° | 79.7 ± 3.8° |
| SNB | 86.1 ± 1.5° | 81.1 ± 1.3° | SNB | 80.9 ± 4.1° | 78.8 ± 4.1° |
| ANB | −6.2 ± 1.9° | 2.3 ± 1.5° | ANB | −4.9 ± 3.1° | 0.9 ± 2.6° |
| A-Nv | 0.5 ± 1.6 mm | 2.5 ± 1.2 mm | A-Nv | −7.1 ± 4.4 mm | −2.6 ± 4.2 mm |
| Pog-Nv | 10.7 ± 3.7 mm | 1.3 ± 0.6 mm | Pog-Nv | −1.8 ± 10.8 mm | −5.9 ± 7.5 mm |
| Parameter | Group 1 | Group 2 | ||
|---|---|---|---|---|
| Discrepancy of Condylar Point | Mean Discrepancy | Discrepancy of Condylar Point | Mean Discrepancy | p-Value |
| RL-RL’ | 1.23 ± 0.47 mm | RL-RL’ | 2.53 ± 0.82 mm | <0.001 * |
| LL-LL’ | 1.14 ± 0.33 mm | LL-LL’ | 2.37 ± 0.71 mm | <0.001 * |
| RM-RM’ | 1.09 ± 0.23 mm | RM-RM’ | 2.86 ± 1.02 mm | <0.001 * |
| LM-LM’ | 0.95 ± 0.15 mm | LM-LM’ | 2.42 ± 0.85 mm | <0.001 * |
| Parameter | Group 1 | Group 2 | |||
|---|---|---|---|---|---|
| Intercondylar Angles | Mean Value ± SD | p-value | Intercondylar Angles | Mean Value ± SD | p-Value |
| Preoperative | 161.75 ± 5.18° | Preoperative | 171.47 ± 6.38° | ||
| Postoperative | 159.36 ± 4.75° | <0.001 * | Postoperative | 165.38 ± 5.23° | <0.001 * |
| Alteration of intercondylar angles | 2.33 ± 1.34° | <0.001 * | Alteration of intercondylar angles | 6.30 ± 2.22° | <0.001 * |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lee, Y.-H.; Tsai, C.-Y.; Wang, L.-C.; Lai, U.-K.; Lai, J.-P.; Lin, S.-S.; Chang, Y.-J. Comparison of the Post-Surgical Position of the Temporomandibular Joint after Orthognathic Surgery in Skeletal Class III Patients and Patients with Cleft Lip and Palate. J. Pers. Med. 2022, 12, 1437. https://doi.org/10.3390/jpm12091437
Lee Y-H, Tsai C-Y, Wang L-C, Lai U-K, Lai J-P, Lin S-S, Chang Y-J. Comparison of the Post-Surgical Position of the Temporomandibular Joint after Orthognathic Surgery in Skeletal Class III Patients and Patients with Cleft Lip and Palate. Journal of Personalized Medicine. 2022; 12(9):1437. https://doi.org/10.3390/jpm12091437
Chicago/Turabian StyleLee, Yi-Hao, Chi-Yu Tsai, Ling-Chun Wang, U-Kei Lai, Jui-Pin Lai, Shiu-Shiung Lin, and Yu-Jen Chang. 2022. "Comparison of the Post-Surgical Position of the Temporomandibular Joint after Orthognathic Surgery in Skeletal Class III Patients and Patients with Cleft Lip and Palate" Journal of Personalized Medicine 12, no. 9: 1437. https://doi.org/10.3390/jpm12091437
APA StyleLee, Y.-H., Tsai, C.-Y., Wang, L.-C., Lai, U.-K., Lai, J.-P., Lin, S.-S., & Chang, Y.-J. (2022). Comparison of the Post-Surgical Position of the Temporomandibular Joint after Orthognathic Surgery in Skeletal Class III Patients and Patients with Cleft Lip and Palate. Journal of Personalized Medicine, 12(9), 1437. https://doi.org/10.3390/jpm12091437






