Retrospective Analysis for Dose Reduction to Organs at Risk with New Personalized Breast Holder (PERSBRA) in Left Breast IMRT
Abstract
:1. Introduction
2. Materials and Methods
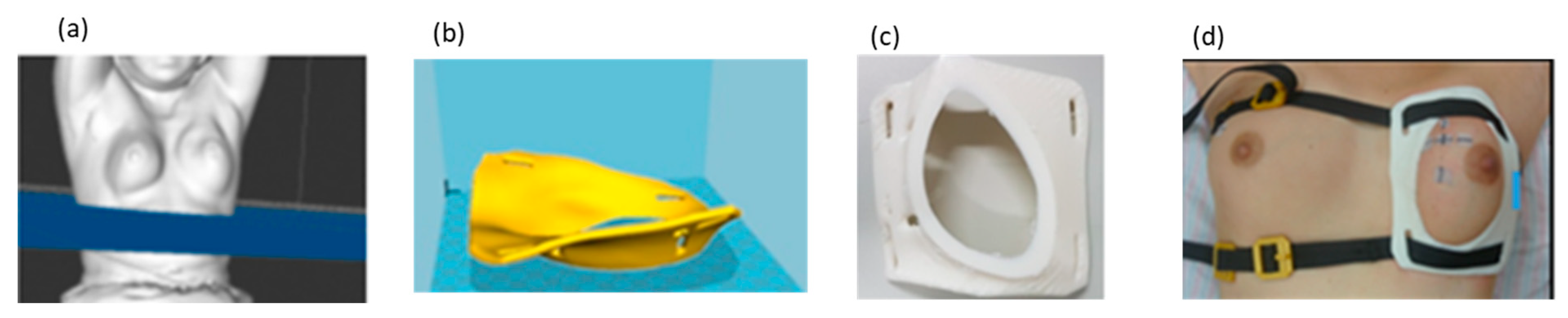
2.1. PERSBRA Design
2.2. Patient Selection
2.3. Delineation of Target Volume and Organs at Risk
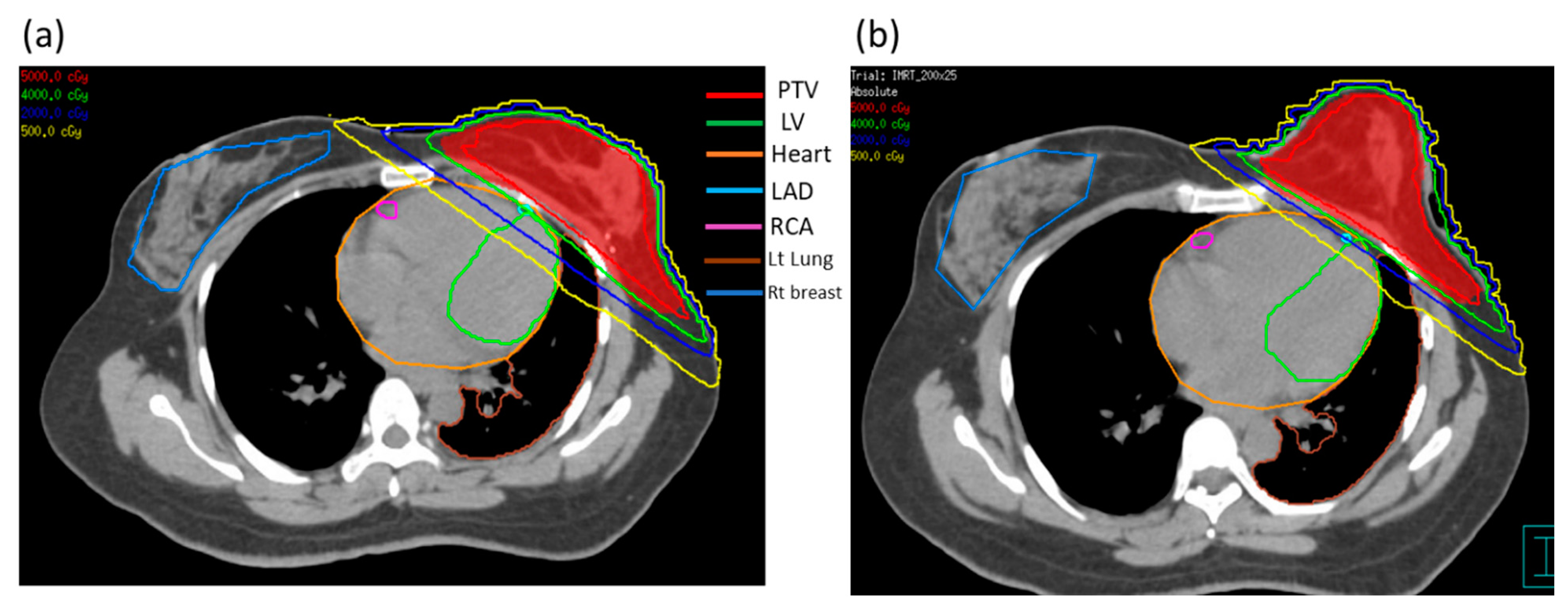
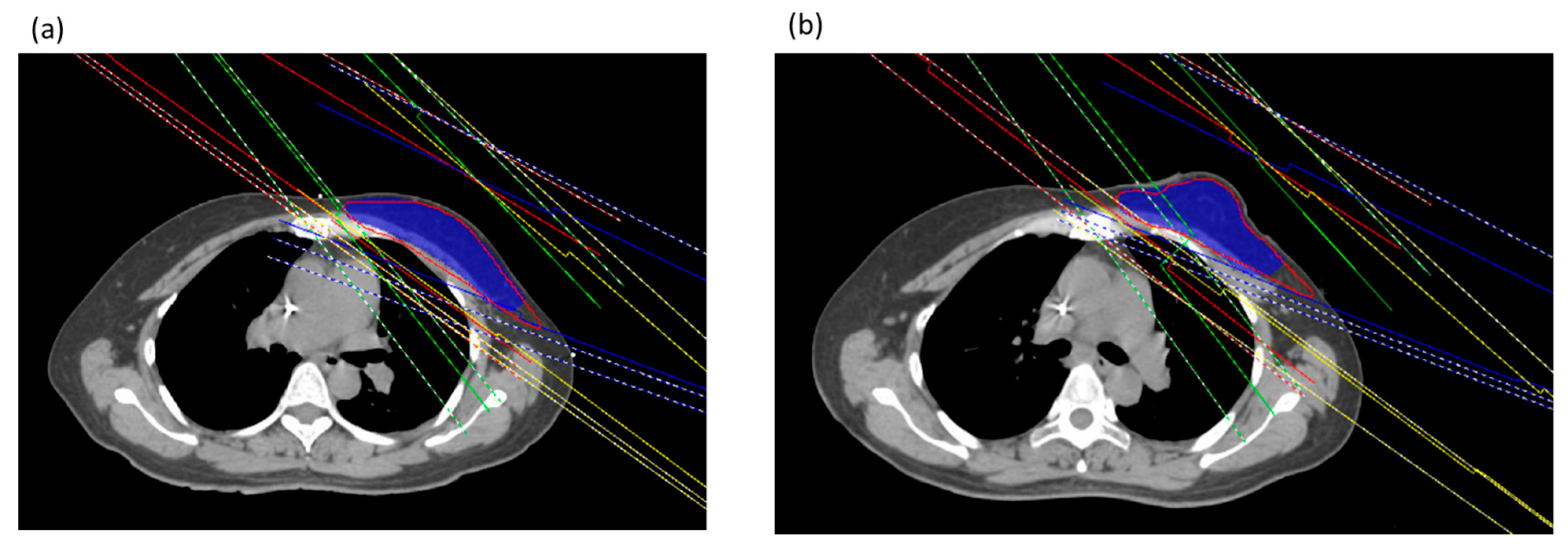
2.4. Treatment Planning
2.5. Plan Evaluation Parameters
2.6. Statistical Analyses
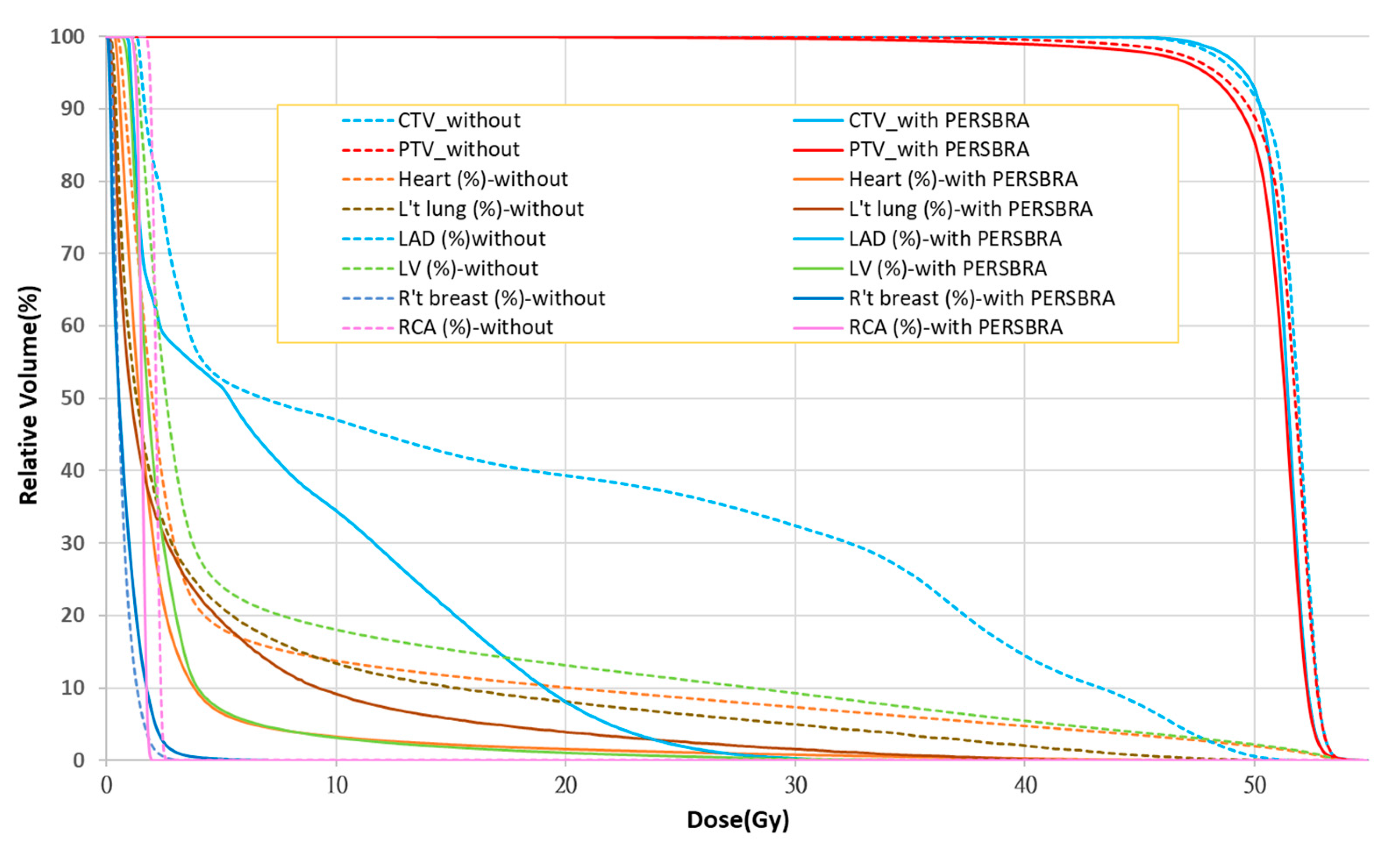
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Sung, H.; Ferlay, J.; Siegel, R.L.; Laversanne, M.; Soerjomataram, I.; Jemal, A.; Bray, F. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA A Cancer J. Clin. 2021, 71, 209–249. [Google Scholar] [CrossRef] [PubMed]
- Darby, S.; McGale, P.; Correa, C.; Taylor, C.; Arriagada, R.; Clarke, M.; Cutter, D.; Davies, C.; Ewertz, M.; Godwin, J.; et al. Effect of radiotherapy after breast-conserving surgery on 10-year recurrence and 15-year breast cancer death: Meta-analysis of individual patient data for 10,801 women in 17 randomised trials. Lancet 2011, 378, 1707–1716. [Google Scholar] [PubMed]
- Wennstig, A.K.; Wadsten, C.; Garmo, H.; Fredriksson, I.; Blomqvist, C.; Holmberg, L.; Nilsson, G.; Sund, M. Long-term risk of ischemic heart disease after adjuvant radiotherapy in breast. Breast Cancer Res. 2020, 22, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Lind, P.A.; Pagnanelli, R.; Marks, L.B.; Borges-Neto, S.; Hu, C.; Zhou, S.M.; Light, K.; Hardenbergh, P.H. Myocardial perfusion changes in patients irradiated for left sided breast cancer and correlation with coronary artery distribution. Int. J. Radiat. Oncol. Biol. Phys. 2003, 55, 914–920. [Google Scholar] [CrossRef]
- Darby, S.C.; Ewertz, M.; McGale, P.; Bennet, A.M.; Blom-Goldman, U.; Brønnum, D.; Correa, C.; Cutter, D.; Gagliardi, G.; Gigante, B.; et al. Risk of ischemic heart disease in women after radiotherapy for breast cancer. N. Engl. J. Med. 2013, 368, 987–998. [Google Scholar] [CrossRef]
- Taylor, C.; Correa, C.; Duane, F.K.; Aznar, M.C.; Anderson, S.J.; Bergh, J.; Dodwell, D.; Ewertz, M.; Gray, R.; Jagsi, R.; et al. Estimating the Risks of Breast Cancer Radiotherapy: Evidence From Modern Radiation Doses to the Lungs and Heart and From Previous Randomized Trials. J. Clin. Oncol. Off. J. Am. Soc. Clin. Oncol. 2017, 35, 1641–1649. [Google Scholar] [CrossRef] [PubMed]
- Omarini, C.; Thanopoulou, E.; Johnston, S.R. Johnston, pneumonitis and pulmonary fibrosis associated with breast cancer treatments. Breast Cancer Res. Treat. 2014, 146, 245–258. [Google Scholar] [CrossRef]
- Song, J.; Tang, T.; Caudrelier, J.M.; Bélec, J.; Chan, J.; Lacasse, P.; Aldosary, G.; Nair, V. Dose-sparing effect of deep inspiration breath hold technique on coronary artery and left ventricle segments in treatment of breast cancer. Radiother. Oncol. J. Eur. Soc. Ther. Radiol. Oncol. 2021, 154, 101–109. [Google Scholar] [CrossRef]
- Koivumäki, T.; Fogliata, A.; Zeverino, M.; Boman, E.; Sierpowska, J.; Moeckli, R.; Vallet, V.; Cozzi, L.; Heikkilä, J.; Väänänen, A.; et al. Dosimetric evaluation of modern radiation therapy techniques for left breast in deep-inspiration breath-hold. Phys. Med. 2018, 45, 82–87. [Google Scholar] [CrossRef] [PubMed]
- Yao, S.; Zhang, Y.; Nie, K.; Liu, B.; Haffty, B.G.; Ohri, N.; Yue, N.J. Setup uncertainties and the optimal imaging schedule in the prone position whole breast radiotherapy. Radiat. Oncol. 2019, 14, 76. [Google Scholar] [CrossRef] [Green Version]
- Saini, A.S.; Hwang, C.S.; Biagioli, M.C.; Das, I.J. Evaluation of sparing organs at risk (OARs) in left-breast irradiation in the supine and prone positions and with deep inspiration breath-hold. J. Appl. Clin. Med. Phys. 2018, 19, 195–204. [Google Scholar] [CrossRef] [PubMed]
- Kirby, A.M.; Evans, P.M.; Helyer, S.J.; Donovan, E.M.; Convery, H.M.; Yarnold, J.R. A randomised trial of supine veusus prone breast radiotherapy. Radiat. Oncol. 2011, 100, 22–226. [Google Scholar]
- Bergom, C.; Currey, A.; Desai, N.; Tai, A.; Strauss, J.B. DIBH techniques and advantages for cardiac sparing during breast cancer irradiation. Front. Oncol. 2018, 8, 87. [Google Scholar] [CrossRef] [PubMed]
- Gaál, S.; Kahán, Z.; Paczona, V.; Kószó, R.; Drencsényi, R.; Szabó, J.; Rónai, R.; Antal, T.; Deák, B.; Varga, Z. Deep-inspirational breath-hold (DIBH) technique in left-sided breast cancer: Various aspects of clinical utility. Radiat. Oncol. 2021, 16, 89. [Google Scholar] [CrossRef]
- Chen, T.H.; Chung, M.Y.; Tien, D.C.; Wang, R.Y.; Chiou, J.F.; Chen, K.H.; Tseng, K.H.; Lu, L.S. Personalized Breast Holder (PERSBRA): A New Cardiac Sparing Technique for Left-sided Whole Breast Irradiation. Int. J. Radiat. Oncol. Biol. Phys. 2017, 99, E646. [Google Scholar] [CrossRef]
- Keller, L.M.; Sopka, D.M.; Li, T.; Klayton, T.; Li, J.; Anderson, P.R.; Bleicher, R.J.; Sigurdson, E.R.; Freedman, G.M. Five year results of whole breast imrt for the treatment of early stage breast cancer. Int. J. Radiat. Oncol. Biol. Phys. 2012, 84, 881–887. [Google Scholar] [CrossRef]
- Schubert, L.K.; Gondi, V.; Sengbusch, E.; Westerly, D.C.; Soisson, E.T.; Paliwal, B.R.; Mackie, T.R.; Mehta, M.P.; Patel, R.R.; Tomé, W.A.; et al. Dosimetric comparison of left-sided whole breast irradiation with 3DCRT, forward-planned IMRT, inverse-planned IMRT, helical tomotherapy, and topotherapy. Radiother. Oncol. J. Eur. Soc. Ther. Radiol. Oncol. 2011, 100, 241–246. [Google Scholar] [CrossRef]
- Huang, J.H.; Wu, X.X.; Lin, X.; Shi, J.T.; Ma, Y.J.; Duan, S.; Huang, X.B. Evaluation of fixed-jaw IMRT and tangential partial-VMAT radiotherapy plans for synchronous bilateral breast cancer irradiation based on a dosimetric study. J. Appl. Clin. Med. Phys. 2019, 20, 31–41. [Google Scholar] [CrossRef]
- Yeung, R.; Conroy, L.; Long, K.; Walrath, D.; Li, H.; Smith, W.; Hudson, A.; Phan, T. Cardiac dose reduction with deep inspiration breath hold for left-sided breast cancer radiotherapy patients with and without regional nodal irradiation. Radiat. Oncol. 2015, 10, 200. [Google Scholar] [CrossRef]
- Aznar, M.C.; Korreman, S.S.; Pedersen, A.N.; Persson, G.F.; Josipovic, M.; Specht, L. Evaluation of dose to cardiac structures during breast irradiation. Br. J. Radiol. 2011, 84, 743–746. [Google Scholar] [CrossRef]
- Yamauchi, R.; Mizuno, N.; Itazawa, T.; Saitoh, H.; Kawamori, J. Dosimetric evaluation of deep inspiration breath hold for left-sided breast cancer: Analysis of patient-specific parameters related to heart dose reduction. J. Radiat. Res. 2020, 61, 447–456. [Google Scholar] [CrossRef] [Green Version]
- Chen, C.P.; Lin, C.Y.; Kuo, C.C.; Chen, T.H.; Lin, S.C.; Tseng, K.H.; Cheng, H.W.; Chao, H.L.; Yen, S.H.; Lin, R.Y.; et al. Skin Surface Dose for Whole Breast Radiotherapy Using Personalized Breast Holder: Comparison with Various Radiotherapy Techniques and Clinical Experiences. Cancers 2022, 14, 3205. [Google Scholar] [CrossRef] [PubMed]
- Offersen, B.V.; Boersma, L.J.; Kirkove, C.; Hol, S.; Aznar, M.C.; Biete Sola, A.; Kirova, Y.M.; Pignol, J.P.; Remouchamps, V.; Verhoeven, K.; et al. ESTRO consensus guideline on target volume delineation for elective radiation therapy of early stage breast cancer. Radiother. Oncol. J. Eur. Soc. Ther. Radiol. Oncol. 2015, 114, 3–10. [Google Scholar] [CrossRef] [PubMed]
- Feng, M.; Moran, J.M.; Koelling, T.; Chughtai, A.; Chan, J.L.; Freedman, L.; Hayman, J.A.; Jagsi, R.; Jolly, S.; Larouere, J.; et al. Development and validation of a heart atlas to study cardiac exposure to radiation following treatment for breast cancer. Int. J. Radiat. Oncol. Biol. Phys. 2011, 79, 10–18. [Google Scholar] [CrossRef] [PubMed]
- Gradishar, W.J.; Anderson, B.O.; Abraham, J.; Aft, R.; Agnese, D.; Allison, K.H.; Blair, S.L.; Burstein, H.J.; Dang, C.; Elias, A.D.; et al. Breast Cancer, Version 3.2020, NCCN Clinical Practice Guidelines in Oncology. J. Natl. Compr. Cancer Netw. 2020, 18, 452–478. [Google Scholar] [CrossRef]
- Rudra, S.; Al-Hallaq, H.A.; Feng, C.; Chmura, S.J.; Hasan, Y. Effect of RTOG breast guidelines on dose-volume histogram parameters. J. Appl. Clin. Med. Phys. 2014, 15, 127–137. [Google Scholar] [CrossRef] [PubMed]
- Nithya, L.; Goel, V.; Sharma, D.; Vittal, K.; Marjara, N. Dosimetric comparison of different planning techniques in left sided whole breast irradiation: A planning study. J. Med. Phys. 2020, 45, 148. [Google Scholar] [CrossRef]
- Wu, Q.; Mohan, R.; Morris, M.; Lauve, A.; Schmidt-Ullrich, R. Simultaneous integrated boost intensity-modulated radiotherapy for locally advanced head-and-neck squamous cell carcinomas. I: Dosimetric results. Int. J. Radiat. Oncol. Biol. Phys. 2003, 56, 573–585. [Google Scholar] [CrossRef]
- Wambersie, A.; Landberg, T.G.; Chavaudra, J.; Dobbs, J.; Hanks, G.; Johansson, K.A.; Moller, T.; Purdy, J.; Akanuma, A.; Gerard, J.P.; et al. Prescribing, Recording, And Reporting Photon Beam Therapy Presentation Of The ICRU Report # 50. J. Med. Phys. 1992, 17, 5–7. [Google Scholar]
- Yan, L.; Xu, Y.; Chen, X.; Xie, X.; Liang, B.; Dai, J. A new homogeneity index definition for evaluation of radiotherapy plans. J. Appl. Clin. Med. Phys. 2019, 20, 50–56. [Google Scholar] [CrossRef]
- Stovall, M.; Smith, S.A.; Langholz, B.M.; Boice Jr, J.D.; Shore, R.E.; Andersson, M.; Buchholz, T.A.; Capanu, M.; Bernstein, L.; Lynch, C.F.; et al. Dose to the contralateral breast from radiotherapy and risk of second primary breast cancer in the wecare study. Int. J. Radiat. Oncol. Biol. Phys. 2008, 72, 1021–1030. [Google Scholar] [CrossRef] [PubMed]
- Swanson, T.; Grills, I.S.; Ye, H.; Entwistle, A.; Teahan, M.; Letts, N.; Yan, D.; Duquette, J.; Vicini, F.A. Six-year experience routinely using moderate deep inspiration breath-hold for the reduction of cardiac dose in left-sided breast irradiation for patients with early-stage or locally advanced breast cancer. Am. J. Clin. Oncol. 2013, 36, 24–30. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Graham, P. Cardiac dosimetry for adjuvant left-sided breast radiotherapy: Patterns with 2D- vs. 3D-era planning and correlates of coronary dose with maximum depth of myocardial exposure. J. Med. Imaging Radiat. Oncol. 2014, 58, 517–522. [Google Scholar] [CrossRef]
- Chi, F.; Wu, S.; Zhou, J.; Li, F.; Sun, J.; Lin, Q.; Lin, H.; Guan, X.; He, Z. Dosimetric comparison of moderate deep inspiration breath-hold and free-breathing intensity-modulated radiotherapy for left-sided breast cancer. Cancer Radiother. J. De La Soc. Fr. De Radiother. Oncol. 2015, 19, 180–186. [Google Scholar] [CrossRef] [PubMed]
- Lakosi, F.; Gulyban, A.; Janvary, L.; Simoni, S.B.; Jansen, N.; Seidel, L.; Kovacs, A.; Vavassis, P.; Coucke, P. Respiratory Motion, Anterior Heart Displacement and Heart Dosimetry: Comparison Between Prone (Pr) and Supine (Su) Whole Breast Irradiation. Pathol. Oncol. Res. POR 2015, 21, 1051–1058. [Google Scholar] [CrossRef] [PubMed]
- Lin, L.L.; Vennarini, S.; Dimofte, A.; Ravanelli, D.; Shillington, K.; Batra, S.; Tochner, Z.; Both, S.; Freedman, G. Proton beam versus photon beam dose to the heart and left anterior descending artery for left-sided breast cancer. Acta Oncol. 2015, 54, 1032–1039. [Google Scholar] [CrossRef]
- Jacob, S.; Camilleri, J.; Derreumaux, S.; Walker, V.; Lairez, O.; Lapeyre, M.; Bruguière, E.; Pathak, A.; Bernier, M.O.; Laurier, D.; et al. Is mean heart dose a relevant surrogate parameter of left ventricle and coronary arteries exposure during breast cancer radiotherapy: A dosimetric evaluation based on individually-determined radiation dose (BACCARAT study). Radiat. Oncol. 2019, 14, 29. [Google Scholar] [CrossRef]
- Carosi, A.; Ingrosso, G.; Turturici, I.; Valeri, S.; Barbarino, R.; Di Murro, L.; Bottero, M.; Lancia, A.; Ponti, E.; Bruni, A.; et al. Whole breast external beam radiotherapy in elderly patients affected by left-sided early breast cancer: A dosimetric comparison between two simple free-breathing techniques. Aging Clin. Exp. Res. 2020, 32, 1335–1341. [Google Scholar] [CrossRef]
- Duma, M.N.; Baumann, R.; Budach, W.; Dunst, J.; Feyer, P.; Fietkau, R.; Haase, W.; Harms, W.; Hehr, T.; Krug, D.; et al. Heart-sparing radiotherapy techniques in breast cancer patients: A recommendation of the breast cancer expert panel of the German society of radiation oncology (DEGRO). Strahlenther. Und Onkol. Organ Der Dtsch. Rontgenges. 2019, 195, 861–871. [Google Scholar] [CrossRef]
- Marks, L.B.; Bentzen, S.M.; Deasy, J.O.; Kong, F.M.; Bradley, J.D.; Vogelius, I.S.; El Naqa, I.; Hubbs, J.L.; Lebesque, J.V.; Timmerman, R.D.; et al. Radiation dose-volume effects in the lung. Int. J. Radiat. Oncol. Biol. Phys. 2010, 76 (Suppl. S3), S70–S76. [Google Scholar] [CrossRef]
- Lingos, T.I.; Recht, A.; Vicini, F.; Abner, A.; Silver, B.; Harris, J.R. Radiation pneumonitis in breast cancer patients treated with conservative surgery and radiaton therapy. Int. J. Radiat. Oncol. Biol. Phys. 1991, 21, 355–360. [Google Scholar] [CrossRef]
- Varga, Z.; Cserháti, A.; Rárosi, F.; Boda, K.; Gulyás, G.; Együd, Z.; Kahán, Z. Individualized positioning for maximum heart protection during breast irradiation. Acta Oncol. 2014, 53, 58–64. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lin, C.H.; Lin, L.C.; Que, J.; Ho, C.H. A seven-year experience of using moderate deep inspiration breath-hold for patients with early-stage breast cancer and dosimetric comparison. Medicine 2019, 98, e15510. [Google Scholar] [CrossRef] [PubMed]
- Byun, H.K.; Chang, J.S.; Choi, M.S.; Chun, J.; Jung, J.; Jeong, C.; Kim, J.S.; Chang, Y.; Chung, S.Y.; Lee, S.; et al. Evaluation of deep learning-based autosegmentation in breast cancer radiotherapy. Radiat. Oncol. 2021, 16, 203. [Google Scholar] [CrossRef] [PubMed]

| Without PERSBRA-IMRT | With PERSBRA-IMRT | |
|---|---|---|
| Mean ± SD (Range) | Mean ± SD (Range) | |
| Age (in years) | 51.7 ± 11.0 (35–82) | |
| CTV | ||
| Volume (cc) | 385.0 ± 134.6 (247.2–676.0) | 388.1 ± 145.3 (223.7–719.3) |
| PTV | ||
| Volume (cc) | 538.0 ± 158.1 (367.4–816.2) | 520.2 ± 162.5 (328.1–869.7) |
| Heart | ||
| Volume (cc) | 476.7 ± 64.1 (354.8–595.3) | 471.7 ± 61.5 (379.8–598.3) |
| Without PERSBRA-IMRT | With PERSBRA-IMRT | |
|---|---|---|
| Mean ± SD | Mean ± SD | |
| PTV D95(%) | 95.94 ± 1.12 | 95.76 ± 1.11 |
| PTV CI | 1.34 ± 0.11 | 1.28 ± 0.15 |
| PTV HI | 0.148 ± 0.03 | 0.169 ± 0.05 |
| Organ at Risk Mean ± sd | Without PERABRA-IMRT | With PERSBRA-IMRT | Reduction (%) |
|---|---|---|---|
| Heart Dmean (cGy) | 382.3 ± 100.5 | 221.8 ± 33.9 | 42.0% |
| LAD | |||
| Dmax (cGy) | 4903.9 ± 419.4 | 3608.2 ± 665.2 | 26.4% |
| Dmean (cGy) | 1621.6 ± 511.8 | 859.0 ± 154.8 | 47.0% |
| LV | |||
| Dmean (cGy) | 604.3 ± 163.1 | 277.5 ± 43.0 | 54.1% |
| Left lung | |||
| V20 (%) | 17.1 ± 5.3 | 13.2 ± 4.5 | 22.8% |
| V10 (%) | 24.8 ± 6.2 | 19.9 ± 5.2 | 19.8% |
| V5 (%) | 34.3 ± 7.3 | 28.9 ± 5.1 | 15.7% |
| Dmean (cGy) | 946.1 ± 268.9 | 725.2 ± 181.4 | 23.3% |
| Metric | Without PERSBRA-IMRT | With PERSBRA-IMRT | p-Value |
|---|---|---|---|
| Median (IQR) | Median (IQR) | ||
| CTV | |||
| Volume (cc) | 329.3 (176.6) | 358.9 (162.2) | 0.992 |
| PTV | |||
| Volume (cc) | 471.8 (228.7) | 495 (208.8) | 0.617 |
| Heart | |||
| Dmean (cGy) | 335.1 (155.5) | 218.5 (35.6) | <0.001 * |
| Volume (cc) | 472.7 (86.4) | 453.6 (98.8) | 0.721 |
| LAD | |||
| Dmax (cGy) | 5068.6 (502.9) | 3716.4 (679.1) | <0.001 * |
| Dmean (cGy) | 1684.7 (556.4) | 873.7 (137.8) | <0.001 * |
| V30 (%) | 28.7 (17.6) | 1.6 (3.8) | <0.001 * |
| V40 (%) | 12.1 (11.7) | 0 (0) | <0.001 * |
| LV | |||
| Dmean (cGy) | 536.1 (300.2) | 277 (42.3) | <0.001 * |
| V5 (%) | 22.3 (6.4) | 8.1 (2.2) | <0.001 * |
| V23 (%) | 6.7 (7) | 0.9 (1) | <0.001 * |
| RCA | |||
| Dmax (cGy) | 190.6 (50.3) | 189.4 (41.1) | 0.665 |
| Dmean (cGy) | 133.2 (23.9) | 130.2 (32.9) | 0.452 |
| Right breast | |||
| Dmax (cGy) | 358.5 (203.8) | 345 (146.1) | 0.798 |
| Dmean (cGy) | 46.0 (22.2) | 57.8 (18.4) | 0.032 * |
| Left lung | |||
| V20 (%) | 18.2 (7.7) | 14.7(7.4) | 0.006 * |
| V10 (%) | 25.3 (8.2) | 21.7(7.8) | 0.004 * |
| V5 (%) | 34.6 (9.9) | 30.7 (7) | 0.007 * |
| Dmean (cGy) | 984.8 (392.9) | 797.2 (296) | 0.002 * |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chen, C.-P.; Chen, T.-H.; Chiou, J.-F.; Chen, Y.-J.; Kuo, C.-C.; Tseng, K.-H.; Chung, M.-Y.; Chen, C.-Y.; Wu, J.-Y.; Lu, L.-S.; et al. Retrospective Analysis for Dose Reduction to Organs at Risk with New Personalized Breast Holder (PERSBRA) in Left Breast IMRT. J. Pers. Med. 2022, 12, 1368. https://doi.org/10.3390/jpm12091368
Chen C-P, Chen T-H, Chiou J-F, Chen Y-J, Kuo C-C, Tseng K-H, Chung M-Y, Chen C-Y, Wu J-Y, Lu L-S, et al. Retrospective Analysis for Dose Reduction to Organs at Risk with New Personalized Breast Holder (PERSBRA) in Left Breast IMRT. Journal of Personalized Medicine. 2022; 12(9):1368. https://doi.org/10.3390/jpm12091368
Chicago/Turabian StyleChen, Chiu-Ping, Tung-Ho Chen, Jeng-Fong Chiou, Yi-Ju Chen, Chia-Chun Kuo, Kuo-Hsiung Tseng, Meng-Yun Chung, Chun-You Chen, Jeng-You Wu, Long-Sheng Lu, and et al. 2022. "Retrospective Analysis for Dose Reduction to Organs at Risk with New Personalized Breast Holder (PERSBRA) in Left Breast IMRT" Journal of Personalized Medicine 12, no. 9: 1368. https://doi.org/10.3390/jpm12091368
APA StyleChen, C.-P., Chen, T.-H., Chiou, J.-F., Chen, Y.-J., Kuo, C.-C., Tseng, K.-H., Chung, M.-Y., Chen, C.-Y., Wu, J.-Y., Lu, L.-S., & Hsu, S.-M. (2022). Retrospective Analysis for Dose Reduction to Organs at Risk with New Personalized Breast Holder (PERSBRA) in Left Breast IMRT. Journal of Personalized Medicine, 12(9), 1368. https://doi.org/10.3390/jpm12091368






