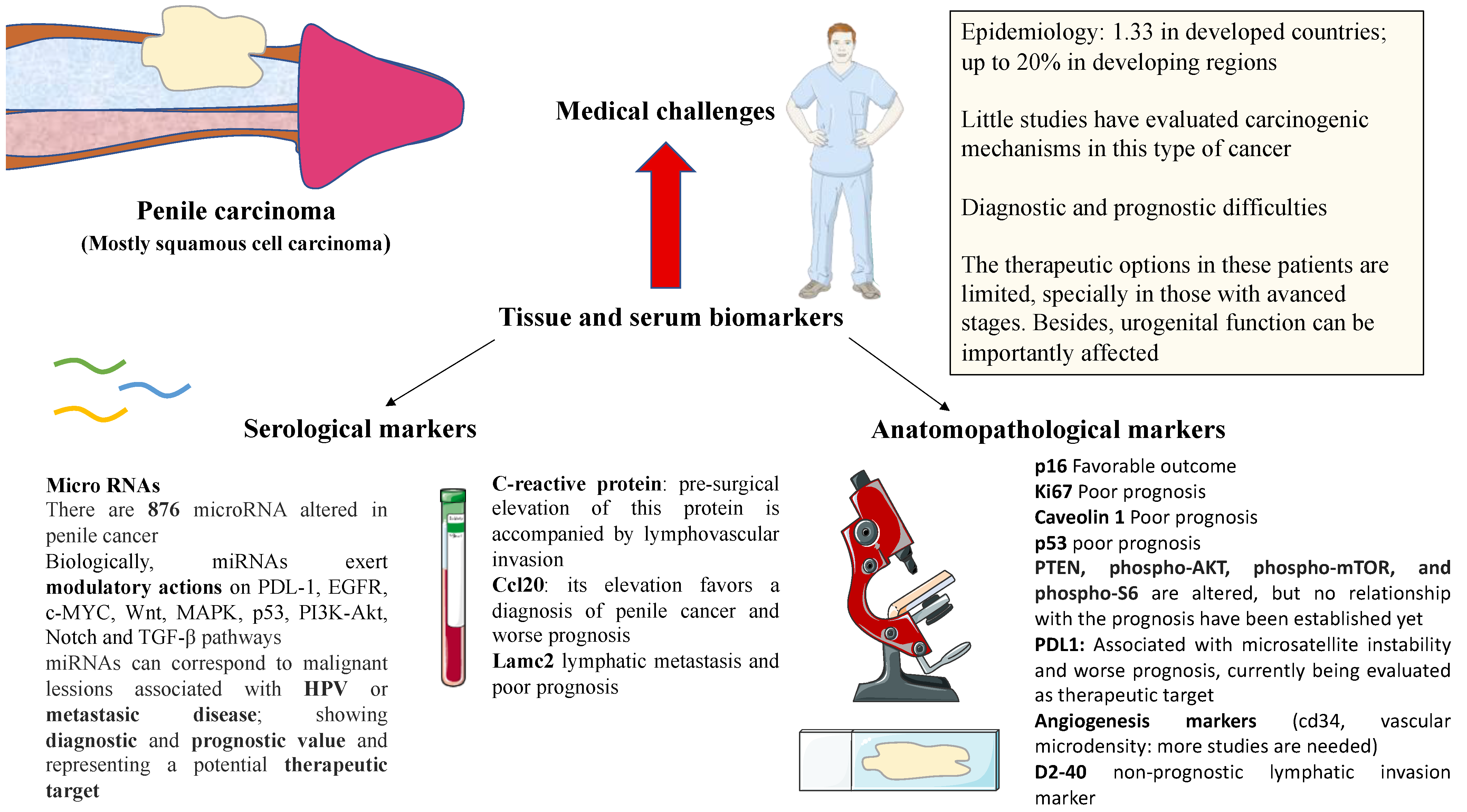
Clinical and Novel Biomarkers in Penile Carcinoma: A Prospective Review
Abstract
1. Introduction
2. Histological Markers
3. Serological Markers
4. MicroRNA
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Douglawi, A.; Masterson, T.A. Updates on the epidemiology and risk factors for penile cancer. Transl. Androl. Urol. 2017, 6, 785–790. [Google Scholar] [CrossRef] [PubMed]
- Montes Cardona, C.E.; García-Perdomo, H.A. Incidence of penile cancer worldwide: Systematic review and meta-analysis. Rev. Panam. Salud Pública 2017, 41, e117. [Google Scholar] [CrossRef] [PubMed]
- Vieira, C.B.; Feitoza, L.; Pinho, J.; Teixeira-Júnior, A.; Lages, J.; Calixto, J.; Coelho, R.; Nogueira, L.; Cunha, I.; Soares, F.; et al. Profile of patients with penile cancer in the region with the highest worldwide incidence. Sci. Rep. 2020, 10, 2965. [Google Scholar] [CrossRef] [PubMed]
- Engelsgjerd, J.S. Penile Cancer—StatPearls—NCBI Bookshelf. National Center for Biotechnology Information. Available online: https://www.ncbi.nlm.nih.gov/books/NBK499930/ (accessed on 6 August 2022).
- Morrison, B. Risk Factors and Prevalence of Penile Cancer. West Indian Med. J. 2018, 63, 559–560. [Google Scholar] [CrossRef][Green Version]
- Olesen, T.B.; Sand, F.L.; Rasmussen, C.L.; Albieri, V.; Toft, B.G.; Norrild, B.; Munk, C.; Kjær, S.K. Prevalence of human papillomavirus DNA and p16INK4a in penile cancer and penile intraepithelial neoplasia: A systematic review and meta-analysis. Lancet Oncol. 2019, 20, 145–158. [Google Scholar] [CrossRef]
- Pal, A.; Kundu, R. Human Papillomavirus E6 and E7: The Cervical Cancer Hallmarks and Targets for Therapy. Front. Microbiol. 2020, 10, 3116. [Google Scholar] [CrossRef]
- Djajadiningrat, R.S.; Jordanova, E.S.; Kroon, B.K.; van Werkhoven, E.; De Jong, J.; Pronk, D.T.; Snijders, P.J.; Horenblas, S.; Heideman, D.A. Human Papillomavirus Prevalence in Invasive Penile Cancer and Association with Clinical Outcome. J. Urol. 2015, 193, 526–531. [Google Scholar] [CrossRef]
- Sand, F.L.; Rasmussen, C.L.; Frederiksen, M.H.; Andersen, K.K.; Kjaer, S.K. Prognostic Significance of HPV and p16 Status in Men Diagnosed with Penile Cancer: A Systematic Review and Meta-analysis. Cancer Epidemiol. Biomark. Prev. 2018, 27, 1123–1132. [Google Scholar] [CrossRef]
- Marth, C.; Landoni, F.; Mahner, S.; McCormack, M.; Gonzalez-Martin, A.; Colombo, N. Cervical cancer: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann. Oncol. 2017, 28, iv72–iv83. [Google Scholar] [CrossRef]
- Bleeker, M.C.G.; Heideman, D.A.M.; Snijders, P.J.F.; Horenblas, S.; Dillner, J.; Meijer, C.J.L.M. Penile cancer: Epidemiology, pathogenesis and prevention. World J. Urol. 2008, 27, 141–150. [Google Scholar] [CrossRef] [PubMed]
- Shabbir, M.; Minhas, S.; Muneer, A. Diagnosis and management of premalignant penile lesions. Ther. Adv. Urol. 2011, 3, 151–158. [Google Scholar] [CrossRef]
- Hoekstra, R.J.; Trip, E.J.; Kate, F.J.T.; Horenblas, S.; Lock, M.T. Penile intraepithelial neoplasia: Nomenclature, incidence and progression to malignancy in the Netherlands. Int. J. Urol. 2018, 26, 353–357. [Google Scholar] [CrossRef] [PubMed]
- Iorga, L.; Marcu, R.D.; Diaconu, C.C.; Stanescu, A.M.A.; Stoian, A.P.; Mischianu, D.L.D.; Surcel, M.; Bungau, S.; Constantin, T.; Boda, D.; et al. Penile carcinoma and HPV infection (Review). Exp. Ther. Med. 2019, 20, 91–96. [Google Scholar] [CrossRef] [PubMed]
- Hakenberg, O.W.; Dräger, D.L.; Erbersdobler, A.; Naumann, C.M.; Jünemann, K.-P.; Protzel, C. The Diagnosis and Treatment of Penile Cancer. Dtsch. Ärzteblatt Int. 2018, 115, 646–652. [Google Scholar] [CrossRef] [PubMed]
- Krishna, S.; Shanbhogue, K.P.; Schieda, N.; Morbeck, F.; Hadas, B.; Kulkarni, G.; McInnes, M.D.; Baroni, R.H. Role of MRI in Staging of Penile Cancer. J. Magn. Reson. Imaging 2020, 51, 1612–1629. [Google Scholar] [CrossRef] [PubMed]
- Sadeghi, R.; Gholami, H.; Zakavi, S.R.; Kakhki, V.R.D.; Tabasi, K.T.; Horenblas, S. Accuracy of Sentinel Lymph Node Biopsy for Inguinal Lymph Node Staging of Penile Squamous Cell Carcinoma: Systematic Review and Meta-Analysis of the Literature. J. Urol. 2012, 187, 25–31. [Google Scholar] [CrossRef]
- Spiess, P.E.; Hernandez, M.S.; Pettaway, C.A. Contemporary inguinal lymph node dissection: Minimizing complications. World J. Urol. 2008, 27, 205–212. [Google Scholar] [CrossRef]
- Galgano, S.J.; Norton, J.C.; Porter, K.K.; West, J.T.; Rais-Bahrami, S. Imaging for the Initial Staging and Post-Treatment Surveillance of Penile Squamous Cell Carcinoma. Diagnostics 2022, 12, 170. [Google Scholar] [CrossRef]
- Bansal, H.; Chaudhary, A.; Batra, D.; Jindal, R. Metastasis from Penile Squamous Cell Carcinoma to Brain: A Case Report and Review of Literature. Indian J. Neurosurg. 2017, 7, 164–167. [Google Scholar] [CrossRef]
- Yuvaraja, T.B.; Waigankar, S.; Dharmadhikari, N.; Pednekar, A. Organ Preservation Surgery for Carcinoma Penis. Indian J. Surg. Oncol. 2016, 8, 59–63. [Google Scholar] [CrossRef]
- Zukiwskyj, M.; Daly, P.; Chung, E. Penile cancer and phallus preservation strategies: A review of current literature. BJU Int. 2013, 112, 21–26. [Google Scholar] [CrossRef] [PubMed]
- Ornellas, A.A.; Chin, E.W.K.; Nóbrega, B.L.B.; Wisnescky, A.; Koifman, N.; Quirino, R. Surgical treatment of invasive squamous cell carcinoma of the penis: Brazilian national cancer institute long-term experience. J. Surg. Oncol. 2008, 97, 487–495. [Google Scholar] [CrossRef] [PubMed]
- Qi, F.; Wei, X.; Zheng, Y.; Ren, X.; Li, X.; Zhao, E. Incidence trends and survival outcomes of penile squamous cell carcinoma: Evidence from the Surveillance, Epidemiology and End Results population-based data. Ann. Transl. Med. 2020, 8, 1428. [Google Scholar] [CrossRef] [PubMed]
- Solsona, E.; Bahl, A.; Brandes, S.B.; Dickerson, D.; Puras-Baez, A.; van Poppel, H.; Watkin, N.A. New Developments in the Treatment of Localized Penile Cancer. Urology 2010, 76, S36–S42. [Google Scholar] [CrossRef]
- Sun, M.; Djajadiningrat, R.S.; Alnajjar, H.M.; Trinh, Q.-D.; Graafland, N.M.; Watkin, N.; Karakiewicz, P.I.; Horenblas, S. Development and external validation of a prognostic tool for prediction of cancer-specific mortality after complete loco-regional pathological staging for squamous cell carcinoma of the penis. BJU Int. 2015, 116, 734–743. [Google Scholar] [CrossRef]
- Ficarra, V.; Akduman, B.; Bouchot, O.; Palou, J.; Tobias-Machado, M. Prognostic Factors in Penile Cancer. Urology 2010, 76, S66–S73. [Google Scholar] [CrossRef]
- Velazquez, E.F.; Ayala, G.; Liu, H.; Chaux, A.; Zanotti, M.; Torres, J.; Cho, S.I.; Barreto, J.E.; Soares, F.; Cubilla, A.L. Histologic Grade and Perineural Invasion are More Important Than Tumor Thickness as Predictor of Nodal Metastasis in Penile Squamous Cell Carcinoma Invading 5 to 10 mm. Am. J. Surg. Pathol. 2008, 32, 974–979. [Google Scholar] [CrossRef]
- Hakenberg, O.W.; Protzel, C. Chemotherapy in penile cancer. Ther. Adv. Urol. 2012, 4, 133–138. [Google Scholar] [CrossRef]
- Rieken, M.; Djajadiningrat, R.S.; Kluth, L.A.; Favaretto, R.L.; Xylinas, E.; Guimaraes, G.C.; Soares, F.A.; Kent, M.; Sjoberg, D.D.; Horenblas, S.; et al. Predictors of Cancer-specific Mortality After Disease Recurrence in Patients with Squamous Cell Carcinoma of the Penis. Eur. Urol. 2014, 66, 811–814. [Google Scholar] [CrossRef]
- Theodore, C.; Skoneczna, I.; Bodrogi, I.; Leahy, M.; Kerst, J.M.; Collette, L.; Ven, K.; Marréaud, S.; Oliver, R.D.T. A phase II multicentre study of irinotecan (CPT 11) in combination with cisplatin (CDDP) in metastatic or locally advanced penile carcinoma (EORTC PROTOCOL 30992). Ann. Oncol. 2008, 19, 1304–1307. [Google Scholar] [CrossRef]
- Duffy, M.J. Tumor Markers in Clinical Practice: A Review Focusing on Common Solid Cancers. Med. Princ. Pract. 2012, 22, 4–11. [Google Scholar] [CrossRef] [PubMed]
- Mehra, N.S.; Ho, T.P.; Hernandez, L.H.; Quevedo, J.F.; Costello, B.A.; Pagliaro, L.C. Penile cancer with visceral metastasis and p16/human papillomavirus positivity: An unusual case of long-term survival. Urol. Case Rep. 2020, 33, 101278. [Google Scholar] [CrossRef] [PubMed]
- Munger, K.; Gwin, T.K.; McLaughlin-Drubin, M.E. p16 in HPV-associated cancers. Oncotarget 2013, 4, 1864–1865. [Google Scholar] [CrossRef]
- Fischer, C.A.; Kampmann, M.; Zlobec, I.; Green, E.; Tornillo, L.; Lugli, A.; Wolfensberger, M.; Terracciano, L.M. p16 expression in oropharyngeal cancer: Its impact on staging and prognosis compared with the conventional clinical staging parameters. Ann. Oncol. 2010, 21, 1961–1966. [Google Scholar] [CrossRef]
- Zhang, J.; Zhang, H.; Xiu, Y.; Cheng, H.; Gu, M.; Song, N. Prognostic Significance of Expression in Penile Squamous Cell Carcinoma: A Meta-Analysis with Trial Sequential Analysis. BioMed Res. Int. 2018, 2018, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Proetzel. Expression of proliferation marker Ki67 correlates to occurrence of metastasis and prognosis, histological subtypes and HPV DNA detection in penile carcinomas. Histol. Histopathol. 2007, 1197–1204. [Google Scholar] [CrossRef]
- Panic, A.; Reis, H.; Wittka, A.; Darr, C.; Hadaschik, B.; Jendrossek, V.; Klein, D. The Biomarker Potential of Caveolin-1 in Penile Cancer. Front. Oncol. 2021, 11, 606122. [Google Scholar] [CrossRef]
- Gunia, S.; Kakies, C.; Erbersdobler, A.; Hakenberg, O.W.; Koch, S.; May, M. Expression of p53, p21 and cyclin D1 in penile cancer: p53 predicts poor prognosis. J. Clin. Pathol. 2011, 65, 232–236. [Google Scholar] [CrossRef]
- Prapiska, F.F.; Warli, S.M. P53 and Survival Rate in Penile Cancer. Open Access Maced. J. Med. Sci. 2019, 7, 1170–1173. [Google Scholar] [CrossRef]
- Chaux, A.; Munari, E.; Cubilla, A.L.; Hicks, J.; Lecksell, K.; Burnett, A.L.; Netto, G.J. Immunohistochemical expression of the mammalian target of rapamycin pathway in penile squamous cell carcinomas: A tissue microarray study of 112 cases. Histopathology 2014, 64, 863–871. [Google Scholar] [CrossRef]
- Davidsson, S.; Carlsson, J.; Giunchi, F.; Harlow, A.; Kirrander, P.; Rider, J.; Fiorentino, M.; Andrén, O. PD-L1 Expression in Men with Penile Cancer and its Association with Clinical Outcomes. Eur. Urol. Oncol. 2019, 2, 214–221. [Google Scholar] [CrossRef]
- Evaluation of microvascular density in tumors: Pro and contra. Histol. Histopathol. 2008, 601–607. [CrossRef]
- Goddard, J.C.; Sutton, C.; Berry, D.; O’Byrne, K.; Kockelbergh, R. The use of microvessel density in assessing human urological tumours. BJU Int. 2001, 87, 866–875. [Google Scholar] [CrossRef] [PubMed]
- Al-Najar, A.; Al-Sanabani, S.; Korda, J.B.; Hegele, A.; Bolenz, C.; Herbst, H.; Jönemann, K.-P.; Naumann, C.M. Microvessel density as a prognostic factor in penile squamous cell carcinoma. Urol. Oncol. Semin. Orig. Investig. 2012, 30, 325–329. [Google Scholar] [CrossRef]
- Arora, A.; Bansal, A. The importance of microvessel density in predicting cancer progression in patients with penile squamous cell carcinoma. Int. Urol. Nephrol. 2017, 49, 1007–1014. [Google Scholar] [CrossRef] [PubMed]
- Copland, I.; Sharma, K.; Lejeune, L.; Eliopoulos, N.; Stewart, D.; Liu, P.; Lachapelle, K.; Galipeau, J. CD34 expression on murine marrow-derived mesenchymal stromal cells: Impact on neovascularization. Exp. Hematol. 2008, 36, 93–103. [Google Scholar] [CrossRef]
- Minardi, D.; D’Anzeo, G.; Lucarini, G.; Filosa, A.; Zizzi, A.; Simonetti, O.; Polito, M.; Offidani, A.M.; Di Primio, R.; Montironi, R.; et al. D2-40 immunoreactivity in penile squamous cell carcinoma: A marker of aggressiveness. Hum. Pathol. 2011, 42, 1596–1602. [Google Scholar] [CrossRef]
- Charkhchi, P.; Cybulski, C.; Gronwald, J.; Wong, F.O.; Narod, S.A.; Akbari, M.R. CA125 and Ovarian Cancer: A Comprehensive Review. Cancers 2020, 12, 3730. [Google Scholar] [CrossRef] [PubMed]
- Poruk, K.E.; Gay, D.Z.; Brown, K.; Mulvihill, J.D.; Boucher, K.M.; Scaife, C.L.; Firpo, M.A.; Mulvihill, S.J. The Clinical Utility of CA 19-9 in Pancreatic Adenocarcinoma: Diagnostic and Prognostic Updates. Curr. Mol. Med. 2013, 13, 340–351. [Google Scholar] [CrossRef]
- Gopalakrishna, A.; Longo, T.A.; Fantony, J.J.; Owusu, R.; Foo, W.-C.; Dash, R.; Inman, B.A. The diagnostic accuracy of urine-based tests for bladder cancer varies greatly by patient. BMC Urol. 2016, 16, 30. [Google Scholar] [CrossRef]
- Hegarty, P.K.; Kayes, O.; Freeman, A.; Christopher, N.; Ralph, D.J.; Minhas, S. A prospective study of 100 cases of penile cancer managed according to European Association of Urology guidelines. BJU Int. 2006, 98, 526–531. [Google Scholar] [CrossRef]
- Ghoshal, A.; Garmo, H.; Arthur, R.; Hammar, N.; Jungner, I.; Malmström, H.; Lambe, M.; Walldius, G.; Van Hemelrijck, M. Serum biomarkers to predict risk of testicular and penile cancer in AMORIS. Ecancermedicalscience 2017, 11, 762. [Google Scholar] [CrossRef] [PubMed]
- Al Ghazal, A.; Steffens, S.; Steinestel, J.; Lehmann, R.; Schnoeller, T.J.; Schulte-Hostede, A.; Wegener, G.; Jentzmik, F.; Schrader, M.; A Kuczyk, M.; et al. Elevated C-reactive protein values predict nodal metastasis in patients with penile cancer. BMC Urol. 2013, 13, 53. [Google Scholar] [CrossRef] [PubMed]
- Mo, M.; Tong, S.; Huang, W.; Cai, Y.; Zu, X.; Hu, X. High serum CCL20 is associated with tumor progression in penile cancer. J. Cancer 2020, 11, 6812–6822. [Google Scholar] [CrossRef] [PubMed]
- Zhou, Q.-H.; Deng, C.-Z.; Chen, J.-P.; Huang, K.-B.; Liu, T.-Y.; Yao, K.; Liu, Z.-W.; Qin, Z.-K.; Li, Y.-H.; Guo, S.-J.; et al. Elevated serum LAMC2 is associated with lymph node metastasis and predicts poor prognosis in penile squamous cell carcinoma. Cancer Manag. Res. 2018, 10, 2983–2995. [Google Scholar] [CrossRef] [PubMed]
- Peng, Y.; Croce, C.M. The role of MicroRNAs in human cancer. Signal Transduct. Target. Ther. 2016, 1, 15004. [Google Scholar] [CrossRef] [PubMed]
- Zirak, R.G.; Tajik, H.; Asadi, J.; Hashemian, P.; Javid, H. The Role of Micro RNAs in Regulating PI3K/AKT Signaling Pathways in Glioblastoma. Iran. J. Pathol. 2022, 17, 122–136. [Google Scholar] [CrossRef] [PubMed]
- Reddy, K.B. MicroRNA (miRNA) in cancer. Cancer Cell Int. 2015, 15, 38. [Google Scholar] [CrossRef] [PubMed]
- Emmanuel, A.; Nettleton, J.; Watkin, N.; Berney, D.M. The molecular pathogenesis of penile carcinoma—current developments and understanding. Virchows Arch. 2019, 475, 397–405. [Google Scholar] [CrossRef]
- Ayoubian, H.; Heinzelmann, J.; Hölters, S.; Khalmurzaev, O.; Pryalukhin, A.; Loertzer, P.; Heinzelbecker, J.; Lohse, S.; Geppert, C.; Loertzer, H.; et al. miRNA Expression Characterizes Histological Subtypes and Metastasis in Penile Squamous Cell Carcinoma. Cancers 2021, 13, 1480. [Google Scholar] [CrossRef]
- Hartz, J.M.; Engelmann, D.; Fürst, K.; Marquardt, S.; Spitschak, A.; Goody, D.; Protzel, C.; Hakenberg, O.W.; Pützer, B.M. Integrated Loss of miR-1/miR-101/miR-204 Discriminates Metastatic from Nonmetastatic Penile Carcinomas and Can Predict Patient Outcome. J. Urol. 2016, 196, 570–578. [Google Scholar] [CrossRef]
- Pinho, J.D.; Silva, G.E.B.; Júnior, A.A.L.T.; Belfort, M.R.D.C.; Macedo, J.M.; Da Cunha, I.W.; Quintana, L.G.; Calixto, J.D.R.R.; Nogueira, L.R.; Coelho, R.W.P.; et al. MIR-107, MIR-223-3P and MIR-21-5P Reveals Potential Biomarkers in Penile Cancer. Asian Pac. J. Cancer Prev. 2020, 21, 391–397. [Google Scholar] [CrossRef] [PubMed]
- Pinho, J.D.; Silva, G.E.B.; Júnior, A.A.L.T.; Belfort, M.R.D.C.; Mendes, J.M.M.; Calixto, J.D.R.R.; Nogueira, L.R.; Burbano, R.R.; Khayat, A.S. Downregulation of miR-145 is associated with perineural invasion in penile carcinoma. Transl. Androl. Urol. 2021, 10, 2019–2026. [Google Scholar] [CrossRef] [PubMed]
- Kuasne, H.; Barros-Filho, M.C.; Busso-Lopes, A.; Marchi, F.A.; Pinheiro, M.; Muñoz, J.J.M.; Scapulatempo-Neto, C.; Faria, E.F.; Guimarães, G.C.; Lopes, A.; et al. Integrative miRNA and mRNA analysis in penile carcinomas reveals markers and pathways with potential clinical impact. Oncotarget 2017, 8, 15294–15306. [Google Scholar] [CrossRef] [PubMed]
- Zhang, L.; Wei, P.; Shen, X.; Zhang, Y.; Xu, B.; Zhou, J.; Fan, S.; Hao, Z.; Shi, H.; Zhang, X.; et al. MicroRNA Expression Profile in Penile Cancer Revealed by Next-Generation Small RNA Sequencing. PLoS ONE 2015, 10, e0131336. [Google Scholar] [CrossRef]
- Crocetto, F.; Arcaniolo, D.; Napolitano, L.; Barone, B.; La Rocca, R.; Capece, M.; Caputo, V.F.; Imbimbo, C.; De Sio, M.; Calace, F.P.; et al. Impact of Sexual Activity on the Risk of Male Genital Tumors: A Systematic Review of the Literature. Int. J. Environ. Res. Public Health 2021, 18, 8500. [Google Scholar] [CrossRef]
| Biomarker | Type | Utility | Reference |
|---|---|---|---|
| p16 | Immunohistochemical | Better prognosis in patients with elevated expression | [8,35] |
| Ki67 | Immunohistochemical | Higher expression is accompanied by a worse prognosis | [37] |
| Caveolin 1 | Immunohistochemical | Higher expression is accompanied by a worse prognosis | [38] |
| p53 | Immunohistochemical | Higher expression is accompanied by a worse prognosis | [39,40] |
| PDL-1 | Immunohistochemical | Higher expression is accompanied by a worse prognosis; possible therapeutic target in penile carcinoma (NCT04224740) | [42] |
| D2-40 | Density of lymphatic vessels. Immunohistochemistry. | High intratumoral lymphatic density major 2 had a sensitivity of 83.3% and a specificity of 78% in predicting lymphatic metastasis invasion. | [48] |
| CRP, albumin, and haptoglobin | Serological | No utility was found when used as serological markers in penile carcinoma. | [53] |
| CRP | Serological | Preoperative elevation of CRP is accompanied by lymphovascular invasion. | [54] |
| CCL20 (chemokine C-C ligands) | Serological | Preoperative serological levels were elevated compared to healthy controls: ROC of 0.855, sensitivity of 72.4%, and specificity of 93.5%. | [55] |
| laminin gamma 2 (LAMC2) | Serological | Serological elevation is accompanied by a greater presence of lymphatic metastases and worse survival. | [56] |
| miR-211-5p y miR-181d-5p | microRNA | Association with HPV-associated malignant lesions such as basaloid and verrucous carcinomas | [61] |
| Infraexpresión de miR-137 y miR-328-3p | microRNA | Association with metastatic disease | [61] |
| miR 138-5p | microRNA | Association with PDL1 expression in patients with carcinoma of the penis | [61] |
| miR-1, miR-101, and miR-204 | microRNA | Underexpression is associated with lymphovascular and metastatic invasion in addition to presenting a worse prognosis. | [62] |
| miR-223-3p, miR-107, and miR-21-5p | microRNA | More frequent in carcinoma of the penis compared to non-tumorous tissue | [63] |
| miR-223-3p | microRNA | Overexpression is associated with a worse prognosis. | [63] |
| miR-145 | microRNA | Underexpression is associated with perineural invasion. | [64] |
| miR-31-5p, miR-224-5p, and miR-223-3p | microRNA | ROC curves 0.861, 0.739, and 0.733, respectively, for differentiating penile carcinoma from non-tumorous tissue | [65] |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pekarek, L.; Ortega, M.A.; Fraile-Martinez, O.; García-Montero, C.; Casanova, C.; Saez, M.A.; García-Honduvilla, N.; Alvarez-Mon, M.; Buján, J.; Diez-Nicolas, V.; et al. Clinical and Novel Biomarkers in Penile Carcinoma: A Prospective Review. J. Pers. Med. 2022, 12, 1364. https://doi.org/10.3390/jpm12091364
Pekarek L, Ortega MA, Fraile-Martinez O, García-Montero C, Casanova C, Saez MA, García-Honduvilla N, Alvarez-Mon M, Buján J, Diez-Nicolas V, et al. Clinical and Novel Biomarkers in Penile Carcinoma: A Prospective Review. Journal of Personalized Medicine. 2022; 12(9):1364. https://doi.org/10.3390/jpm12091364
Chicago/Turabian StylePekarek, Leonel, Miguel A. Ortega, Oscar Fraile-Martinez, Cielo García-Montero, Carlos Casanova, Miguel A. Saez, Natalio García-Honduvilla, Melchor Alvarez-Mon, Julia Buján, Victor Diez-Nicolas, and et al. 2022. "Clinical and Novel Biomarkers in Penile Carcinoma: A Prospective Review" Journal of Personalized Medicine 12, no. 9: 1364. https://doi.org/10.3390/jpm12091364
APA StylePekarek, L., Ortega, M. A., Fraile-Martinez, O., García-Montero, C., Casanova, C., Saez, M. A., García-Honduvilla, N., Alvarez-Mon, M., Buján, J., Diez-Nicolas, V., Burgos, J. F., & Gomez Dos Santos, V. (2022). Clinical and Novel Biomarkers in Penile Carcinoma: A Prospective Review. Journal of Personalized Medicine, 12(9), 1364. https://doi.org/10.3390/jpm12091364










