The Impact of the Laterality on Radiographic Outcomes of the Bernese Periacetabular Osteotomy
Abstract
:1. Introduction
2. Materials and Methods
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
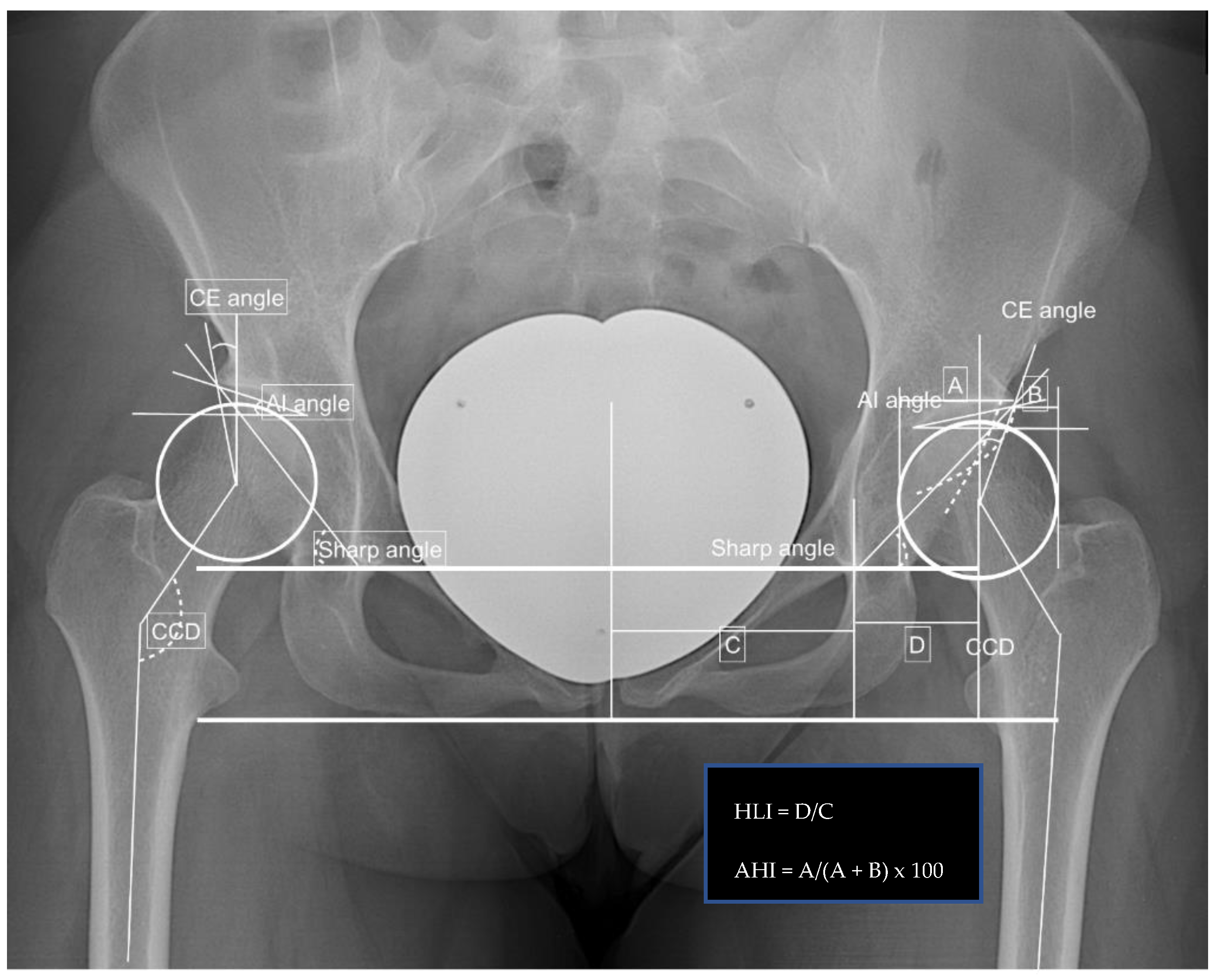
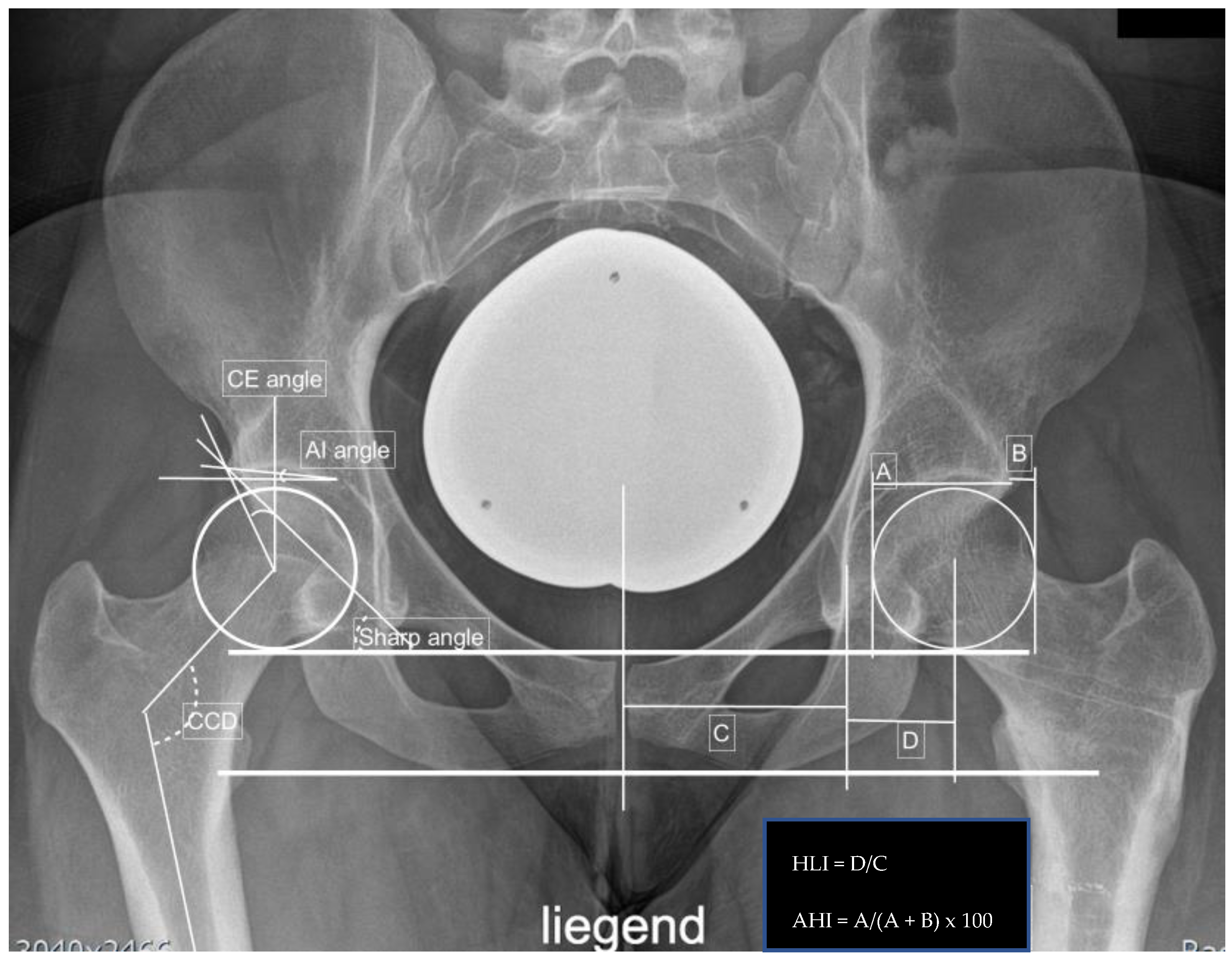
Appendix A
References
- Aronson, J. Osteoarthritis of the young adult hip: Etiology and treatment. Instr. Course Lect. 1986, 35, 119–128. [Google Scholar] [PubMed]
- Leunig, M.; Siebenrock, K.A.; Ganz, R. Rationale of periacetabular osteotomy and background work. J. Bone Jt. Surg. 2001, 83, 438. [Google Scholar] [CrossRef]
- Jakobsen, S.S.; Overgaard, S.; Søballe, K.; Ovesen, O.; Mygind-Klavsen, B.; Dippmann, C.A.; Jensen, M.U.; Stürup, J.; Retpen, J. The interface between periacetabular osteotomy, hip arthroscopy and total hip arthroplasty in the young adult hip. EFORT Open Rev. 2018, 3, 408–417. [Google Scholar] [CrossRef] [PubMed]
- Hayashi, S.; Hashimoto, S.; Matsumoto, T.; Takayama, K.; Kamenaga, T.; Niikura, T.; Kuroda, R. Overcorrection of the acetabular roof angle or anterior center-edge angle may cause decrease of range of motion after curved periacetabular osteotomy. J. Hip Preserv. Surg. 2020, 7, 583–590. [Google Scholar] [CrossRef] [PubMed]
- Hartig-Andreasen, C.; Troelsen, A.; Thillemann, T.M.; Søballe, K. What factors predict failure 4 to 12 years after periacetabular osteotomy? Clin. Orthop. Relat. Res. 2012, 470, 2978–2987. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Clohisy, J.C.; Schutz, A.L.; St. John, L.; Schoenecker, P.L.; Wright, R.W. Periacetabular Osteotomy: A Systematic Literature Review. Clin. Orthop. Relat. Res. 2009, 467, 2041–2052. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Biedermann, R.; Donnan, L.; Gabriel, A.; Wachter, R.; Krismer, M.; Behensky, H. Complications and patient satisfaction after periacetabular pelvic osteotomy. Int. Orthop. 2007, 32, 611–617. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Siebenrock, K.A.; Scholl, E.; Lottenbach, M.; Ganz, R. Bernese periacetabular osteotomy. Clin. Orthop. Relat. Res. 1999, 9–20. [Google Scholar] [CrossRef]
- Davey, J.P.; Santore, R.F. Complications of Periacetabular Osteotomy. Clin. Orthop. Relat. Res. 1999, 363, 33–37. [Google Scholar] [CrossRef]
- Mayo, K.A.; Trumble, S.J.; Mast, J.W. Results of Periacetabular Osteotomy in Patients with Previous Surgery for Hip Dysplasia. Clin. Orthop. Relat. Res. 1999, 363, 73–80. [Google Scholar] [CrossRef]
- Kong, X.; Yang, M.; Li, X.; Ni, M.; Zhang, G.; Chen, J.; Chai, W. Impact of surgeon handedness in manual and robot-assisted total hip arthroplasty. J. Orthop. Surg. Res. 2020, 15, 159. [Google Scholar] [CrossRef] [Green Version]
- Pennington, N.; Redmond, A.; Stewart, T.; Stone, M. The impact of surgeon handedness in total hip replacement. Ann. R. Coll. Surg. Engl. 2014, 96, 437–441. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tannast, M.; Hanke, M.S.; Zheng, G.; Steppacher, S.D.; Siebenrock, K.A. What are the radiographic reference values for acetabular under- and overcoverage? Clin. Orthop. Relat. Res. 2015, 473, 1234–1246. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Clohisy, J.C.; Barrett, S.E.; Gordon, J.E.; Delgado, E.; Schoenecker, P.L. Periacetabular osteotomy for the treatment of severe acetabular dysplasia. J. Bone Jt. Surg. 2005, 87, 254–259. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ahmad, S.S.; Giebel, G.M.; Perka, C.; Meller, S.; Pumberger, M.; Hardt, S.; Stöckle, U.; Konrads, C. Survival of the dysplastic hip after periacetabular osteotomy: A meta-analysis. HIP Int. 2021, 11207000211048425. [Google Scholar] [CrossRef]
- Imai, H.; Kamada, T.; Takeba, J.; Shiraishi, Y.; Mashima, N.; Miura, H. Anterior coverage after eccentric rotational acetabular osteotomy for the treatment of developmental dysplasia of the hip. J. Orthop. Sci. 2014, 19, 762–769. [Google Scholar] [CrossRef] [Green Version]
- Moloney, D.; Bishay, M.; Ivory, J.; Pozo, J. Failure of the sliding hip screw in the treatment of femoral neck fractures: ‘Left-handed surgeons for left-sided hips’. Injury 1994, 25, SB9–SB13. [Google Scholar] [CrossRef]
- Crawford, D.A.; Adams, J.B.; Hobbs, G.R.; Lombardi, A.J.V.; Berend, K.R. Surgical Approach and Hip Laterality Affect Accuracy of Acetabular Component Placement in Primary Total Hip Arthroplasty. Surg. Technol. Int. 2019, 35, 377–385. [Google Scholar] [PubMed]
- Siebenrock, K.A.; Leunig, M.; Ganz, R. Periacetabular osteotomy: The Bernese experience. Instr. Course Lect. 2001, 50, 239–245. [Google Scholar] [CrossRef]
- Kamath, A.F. Bernese periacetabular osteotomy for hip dysplasia: Surgical technique and indications. World J. Orthop. 2016, 7, 280–286. [Google Scholar] [CrossRef]



| Observation | Overall | Left Hip | Right Hip | p-Value |
|---|---|---|---|---|
| Numbers (%) | 41 (100) | 16 (39.0) | 25 (61.0) | |
| Dysplastic hips (%) | 13 (31.7) | 4 (25.0) | 9 (36.0) | 0.236 |
| Age (mean age) | 28.6 ± 7.4 | 29.4 ± 7.7 | 28.1 ± 7.1 | 0.288 |
| Follow up in days | 267.5 ± 208.5 | 222.7 ± 251.0 | 296.7 ± 169.0 | 0.149 |
| Gender (female) n (%) | 37 (90.1) | 16 (100) | 21 (80.8) | 0.048 |
| Body height (cm) | 169.7 ± 8.3 | 168.1 ± 7.6 | 170.7 ± 8.5 | 0.178 |
| Body weight (kg) | 68.0 ± 11.7 | 65.6 ± 9.3 | 69.6 ± 12.7 | 0.159 |
| Body mass index (kg/m2) | 23.6 ± 3.8 | 23.5 ± 3.1 | 23.7 ± 4.2 | 0.450 |
| Mental disorders, Depression n (%) | 7 (17.1) | 3 (18.8) | 4 (16.0) | 0.412 |
| Fixation (screws) n (%) | 35 (85.4) | 14 (87.5) | 21 (84.0) | 0.382 |
| Rotational Values | Overall | Left Hip | Right Hip | p-Value |
|---|---|---|---|---|
| Acetabular torsion (°) | 18.8 ± 6.9 | 18.8 ± 6.9 | 19.3 ± 5.6 | 0.388 |
| Femoral torsion (°) | 30.5 ± 12.9 | 27.7 ± 14.1 | 13.3 ± 18.8 | 0.139 |
| Tibial torsion (°) | 37.4 ± 11.0 | 37.0 ± 7.6 | 41.8 ± 8.8 | 0.433 |
| Femorotibial torsion (°) | 6.2 ± 5.4 | −6.6 ± 11.1 | 7.8 ± 3.6 | 0.082 |
| X-ray Measurements | Preoperatively | Postoperatively | Difference | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Overall | Left Hip | Right Hip | p-Value | Overall | Left Hip | Right Hip | p-Value | p-Value | |
| CE angle (°) | 22.0 ± 6.2 | 24.1 ± 5.2 | 20.7 ± 6.5 | 0.045 | 38.5 ± 8.9 | 37.8 ± 6.1 | 39.0 ± 10.3 | 0.340 | <0.001 |
| AIA (°) | 11.7 ± 5.7 | 10.6 ± 4.4 | 12.4 ± 6.3 | 0.172 | −0.02 ± 6.1 | −2.6 ± 4.3 | 1.6 ± 6.5 | 0.016 | <0.001 |
| Sharp angle (°) | 42.9 ± 3.8 | 41.7 ± 3.3 | 43.6 ± 3.9 | 0.069 | 30.1 ± 5.0 | 29.3 ± 5.9 | 30.7 ± 4.3 | 0.194 | <0.001 |
| Hip lateralization | 0.56 ± 0.07 | 0.55 ± 0.06 | 0.56 ± 0.07 | 0.363 | 0.62 ± 0.07 | 0.60 ± 0.05 | 0.62 ± 0.09 | 0.179 | <0.001 |
| Anterior hip index | 75.5 ± 7.5 | 77.4 ± 6.4 | 74.3 ± 7.8 | 0.100 | 89.7 ± 6.8 | 90.8 ± 6.2 | 89.1 ± 7.0 | 0.229 | <0.001 |
| CCD angle (°) | 134.1 ± 6.0 | 133.0 ± 4.8 | 134.8 ± 6.5 | 0.182 | 136.5 ± 6.8 | 134.6 ± 4.9 | 137.7 ± 7.5 | 0.083 | 0.047 |
| CAM FAI n (%) | 17 (41.5) | 6 (37.5) | 11 (44.0) | 0.345 | |||||
| Pincer FAI | 2 (4.9) | 0 (0) | 2 (8.0) | 0.128 | |||||
| Crossing-over sign | 14 (34.1) | 5 (31.3) | 9 (36.0) | 0.381 | |||||
| Kellgren-Lawrence score 0 | 25 (61.0) | 10 (62.5) | 15 (60.0) | 0.294 | |||||
| Kellgren-Lawrence score 1 | 14 (34.1) | 6 (37.5) | 8 (32.0) | ||||||
| Kellgren-Lawrence score 2 | 2 (4.9) | 0 (0) | 2 (8.0) | ||||||
| Alpha angle (°) | 100.7 ± 10.7 | 97.0 ± 9.5 | 103.4 ± 10.7 | 0.034 | 90.9 ± 12.9 | 92.1 ± 17.8 | 90.4 ± 9.9 | 0.422 | 0.005 |
| Beta angle (°) | 57.5 ± 7.4 | 56.5 ± 7.0 | 58.3 ± 7.6 | 0.234 | 59.4 ± 5.7 | 60.4 ± 4.4 | 59.0 ± 6.2 | 0.355 | 0.210 |
| X-ray Measurements | Change | |||
|---|---|---|---|---|
| Overall | Left Hip | Right Hip | p-Value | |
| CE angle (°) | 16.6 ± 7.1 | 13.7 ± 5.5 | 18.4 ± 7.3 | 0.021 |
| AIA (°) | −11.7 ± 5.7 | −13.2 ± 6.0 | −10.7 ± 5.2 | 0.093 |
| Sharp angle (°) | −12.7 ± 4.0 | −12.5 ± 4.7 | −12.9 ± 3.5 | 0.381 |
| Hip lateralization | 0.06 ± 0.06 | 0.05 ± 0.05 | 0.06 ± 0.06 | 0.213 |
| Anterior hip index | 14.2 ± 5.2 | 13.4 ± 5.0 | 14.8 ± 5.2 | 0.195 |
| Alpha angle (°) | −3.6 ± 30.3 | −0.5 ± 16.5 | −4.9 ± 34.24 | 0.412 |
| Beta angle (°) | 4.7 ± 18.5 | 2.3 ± 6.1 | 5.7 ± 21.4 | 0.386 |
| Complications | Overall | Left Side | Right Side | p-Value |
|---|---|---|---|---|
| Transfusion (%) | 7 (17.1) | 1 (6.3) | 6 (24.0) | 0.07 |
| Hypesthesia of lateral cutaneous femoral nerve (%) | 37 (90.2) | 14 (87.5) | 22 (88.0) | 0.482 |
| Implant migration (%) | 2 (4.9) | 1 (6.3) | 1 (4.0) | 0.376 |
| Peroneal communis nerve palsy (%) | 1 (2.4) | 0 (0) | 1 (4.0) | <0.001 |
| Wound infection (%) | 1 (2.4) | 0 (0) | 1 (4.0) | <0.001 |
| Hardware removal (%) | 10 (24.4) | 1 (6.3) | 9 (36.0) | 0.015 |
| Demographic Data | Overall | Left Hip | Right Hip | p-Value | |||||
|---|---|---|---|---|---|---|---|---|---|
| Age (mean age) | 29.1 ± 6.9 | 28.9 ± 6.9 | 29.3 ± 6.9 | 0.460 | |||||
| Follow up in days | 303.6 ± 243.2 | 271.4 ± 312.7 | 335.9 ± 135.7 | 0.312 | |||||
| Body height (cm) | 167.7 ± 6.1 | 167.8 ± 6.2 | 167.6 ± 6.1 | 0.485 | |||||
| Body weight (kg) | 67.7 ± 7.2 | 68.1 ± 7.6 | 67.3 ± 6.7 | 0.411 | |||||
| Body mass index (kg/m2) | 24.1 ± 2.8 | 24.3 ± 2.9 | 24.0 ± 2.7 | 0.432 | |||||
| Comparison | Preoperatively | Postoperatively | Difference | ||||||
| Overall | Left Hip | Right Hip | p-Value | Overall | Left Hip | Right Hip | p-Value | p-Value | |
| CE angle (°) | 20.7 ± 5.8 | 23.0 ± 5.0 | 18.4 ± 5.6 | 0.063 | 39.2 ± 8.6 | 38.7 ± 5.0 | 39.8 ± 11.0 | 0.413 | <0.001 |
| AIA (°) | 13.6 ± 4.4 | 11.8 ± 4.0 | 15.4 ± 3.9 | 0.056 | −0.11 ± 4.8 | −2.8 ± 4.0 | 2.6 ± 4.0 | 0.013 | <0.001 |
| Sharp angle (°) | 43.1 ± 4.2 | 41.5 ± 3.3 | 44.7 ± 4.4 | 0.072 | 30.1 ± 4.5 | 28.3 ± 4.0 | 31.9 ± 4.2 | 0.060 | <0.001 |
| Hip lateralization | 0.556 ± 0.07 | 0.56 ± 0.08 | 0.55 ± 0.06 | 0.386 | 0.59 ± 0.05 | 0.60 ± 0.04 | 0.59 ± 0.05 | 0.384 | 0.043 |
| Anterior hip index | 73.7 ± 6.4 | 76.6 ± 5.9 | 70.8 ± 5.5 | 0.039 | 90.1 ± 5.7 | 92.7 ± 4.9 | 87.5 ± 5.2 | 0.037 | <0.001 |
| Change in Radiographic Parameters | |||||||||
| CE angle (°) | 18.5 ± 6.9 | 15.7 ± 4.7 | 21.3 ± 7.5 | 0.057 | |||||
| AIA (°) | −13.7 ± 5.3 | −14.6 ± 5.9 | −12.8 ± 4.5 | 0.268 | |||||
| Sharp angle (°) | −13.0 ± 3.8 | −13.2 ± 3.7 | −12.8 ± 3.9 | 0.416 | |||||
| Hip lateralization | 0.04 ± 0.06 | 0.04 ± 0.05 | 0.04 ± 0.07 | 0.452 | |||||
| Anterior hip index | 16.4 ± 4.2 | 16.1 ± 4.9 | 16.7 ± 3.2 | 0.396 | |||||
| Complications | |||||||||
| Transfusion (%) | 2 (12.5) | 0 (0) | 2 (25.0) | 0.074 | |||||
| Hypesthesia of lateral cutaneous femoral nerve (%) | 16 (100) | 8 (100) | 8 (100) | 1.000 | |||||
| Implant migration (%) | 2 (12.5) | 1 (12.5) | 1 (12.5) | 1.000 | |||||
| Hardware removal (%) | 2 (12.5) | 0 (0) | 2 (25) | 0.074 | |||||
| Operative Time | |||||||||
| Surgical time (min) | 93 ± 36 | 89 ± 25 | 97 ± 44 | 0.340 | |||||
| Anaesthesia time (min) | 152 ± 46 | 147 ± 31 | 157 ± 57 | 0.355 | |||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Heimer, C.Y.W.; Wu, C.H.; Perka, C.; Hardt, S.; Göhler, F.; Bäcker, H.C. The Impact of the Laterality on Radiographic Outcomes of the Bernese Periacetabular Osteotomy. J. Pers. Med. 2022, 12, 1072. https://doi.org/10.3390/jpm12071072
Heimer CYW, Wu CH, Perka C, Hardt S, Göhler F, Bäcker HC. The Impact of the Laterality on Radiographic Outcomes of the Bernese Periacetabular Osteotomy. Journal of Personalized Medicine. 2022; 12(7):1072. https://doi.org/10.3390/jpm12071072
Chicago/Turabian StyleHeimer, Carsten Y. W., Chia H. Wu, Carsten Perka, Sebastian Hardt, Friedemann Göhler, and Henrik C. Bäcker. 2022. "The Impact of the Laterality on Radiographic Outcomes of the Bernese Periacetabular Osteotomy" Journal of Personalized Medicine 12, no. 7: 1072. https://doi.org/10.3390/jpm12071072
APA StyleHeimer, C. Y. W., Wu, C. H., Perka, C., Hardt, S., Göhler, F., & Bäcker, H. C. (2022). The Impact of the Laterality on Radiographic Outcomes of the Bernese Periacetabular Osteotomy. Journal of Personalized Medicine, 12(7), 1072. https://doi.org/10.3390/jpm12071072







