More than Meets the Eye: Using Textural Analysis and Artificial Intelligence as Decision Support Tools in Prostate Cancer Diagnosis—A Systematic Review
Abstract
:1. Introduction
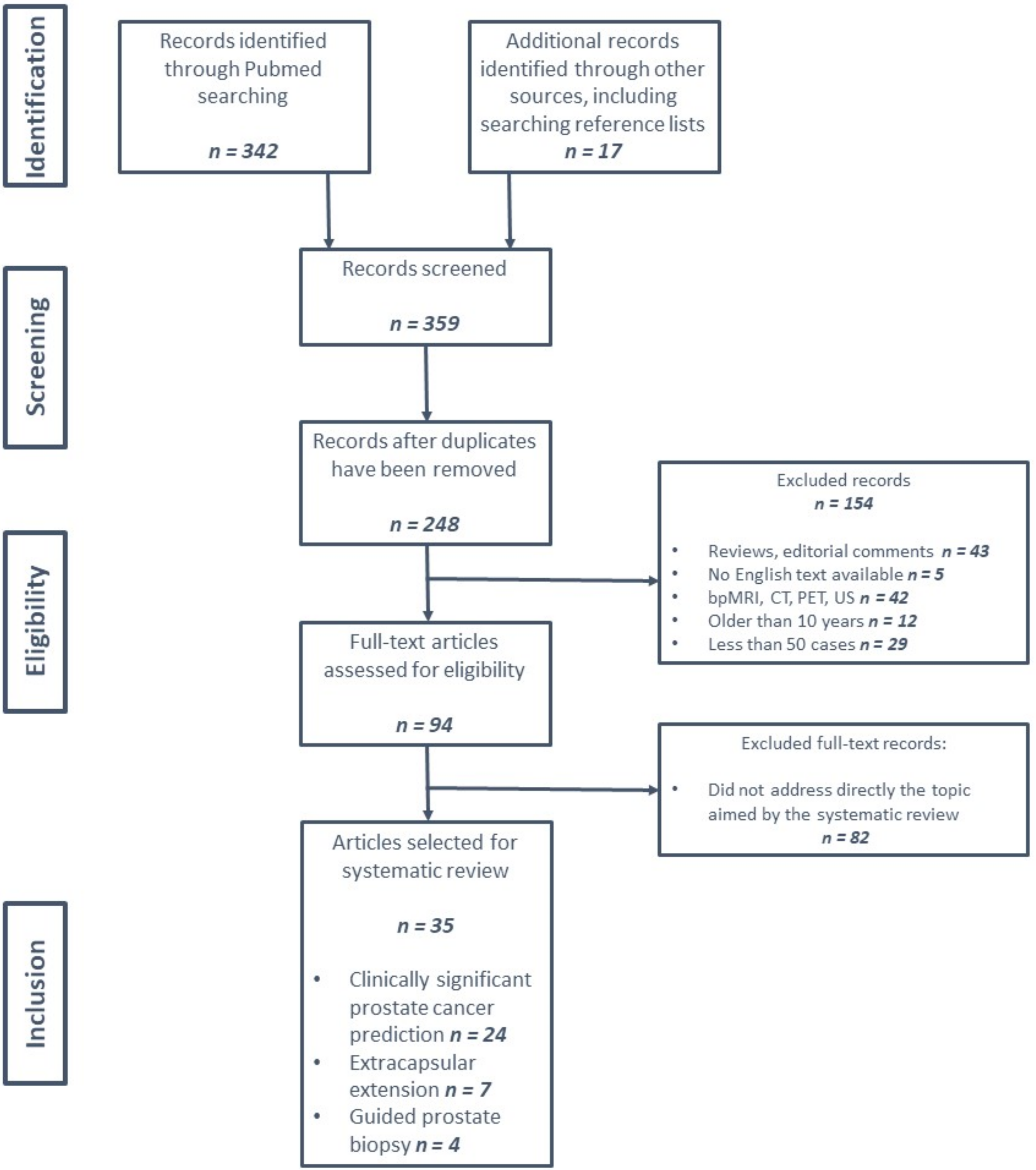
2. Materials and Methods
- Only original research papers were considered;
- Decision support tools trained and validated on at least 50 cases;
- Imagistic technique employed: mpMRI, with specified field strength (1.5 or 3 T);
- Analytical observational studies, written in English and published in the last 10 years;
- Focus on clinical aspects.
- Exclusion criteria:
- Study population under 50 cases;
- Other imagistic methods used, including biparametric MRI (bpMRI);
- Papers designed as systematic reviews, meta-analyses, comments, letters to editor, case reports and clinical practice guidelines;
- Articles focusing on the technical aspects of MRI, textural analysis and artificial intelligence, without a well-established clinical application;
- Studies based on public datasets or carried out on animal subjects or phantom substitutes.
3. Results
3.1. Diagnostic Accuracy and Prediction of PCa Aggressiveness
3.1.1. General Data
3.1.2. AI-Based Automatic Detection of PCa
3.1.3. Prostate Cancer Aggressiveness
3.1.4. Decision Support Tools’ Accuracy Compared to Radiologists’ Interpretation
3.2. Diagnostic Accuracy and Prediction of Extracapsular Extension (ECE)
3.2.1. General Data
3.2.2. AI-Based Tools for Automatic Detection of ECE
3.2.3. Radiomic and Texture Analysis-Based Prediction of ECE
3.2.4. The Accuracy of the Decision Support Tool Compared to the Interpretation of the Radiologist
3.3. Artificial Intelligence-Assisted Targeted Prostate Biopsy
3.3.1. General Data
3.3.2. Accuracy and csPCa Detection Rate of AI-Assisted Targeted Prostate Biopsy
4. Discussion
4.1. PCa Detection and Aggressiveness
4.2. Extracapsular Extension Assessment
4.3. AI-Assisted Targeted Prostate Biopsy
4.4. Limitations of the Review Process
4.5. Implications for Clinical Practice and Future Research
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Siegel, R.L.; Miller, K.D.; Jemal, A. Cancer statistics, 2020. CA Cancer J. Clin. 2020, 70, 7–30. [Google Scholar] [CrossRef] [PubMed]
- Catalona, W.J. Prostate Cancer Screening. Med. Clin. N. Am. 2018, 102, 199–214. [Google Scholar] [CrossRef] [PubMed]
- Turkbey, B.; Rosenkrantz, A.B.; Haider, M.A.; Padhani, A.R.; Villeirs, G.; Macura, K.J.; Tempany, C.M.; Choyke, P.L.; Cornud, F.; Margolis, D.J.; et al. Prostate Imaging Reporting and Data System Version 2.1: 2019 Update of Prostate Imaging Reporting and Data System Version 2. Eur. Urol. 2019, 76, 340–351. [Google Scholar] [CrossRef] [PubMed]
- Flood, T.F.; Pokharel, S.S.; Patel, N.U.; Clark, T.J. Accuracy and Interobserver Variability in Reporting of PI-RADS Version 2. J. Am. Coll. Radiol. 2017, 14, 1202–1205. [Google Scholar] [CrossRef] [PubMed]
- Coker, M.A.; Glaser, Z.A.; Gordetsky, J.B.; Thomas, J.V.; Rais-Bahrami, S. Targets missed: Predictors of MRI-targeted biopsy failing to accurately localize prostate cancer found on systematic biopsy. Prostate Cancer Prostatic Dis. 2018, 21, 549–555. [Google Scholar] [CrossRef]
- Kam, J.; Yuminaga, Y.; Krelle, M.; Gavin, D.; Koschel, S.; Aluwihare, K.; Sutherland, T.; Skinner, S.; Brennan, J.; Wong, L.M.; et al. Evaluation of the accuracy of multiparametric MRI for predicting prostate cancer pathology and tumour staging in the real world: An multicentre study. BJU Int. 2019, 124, 297–301. [Google Scholar] [CrossRef] [PubMed]
- Lambin, P.; Rios-Velazquez, E.; Leijenaar, R.; Carvalho, S.; van Stiphout, R.G.; Granton, P.; Zegers, C.M.; Gillies, R.; Boellard, R.; Dekker, A.; et al. Radiomics: Extracting more information from medical images using advanced feature analysis. Eur. J. Cancer 2012, 48, 441–446. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nketiah, G.; Elschot, M.; Kim, E.; Teruel, J.R.; Scheenen, T.W.; Bathen, T.F.; Selnæs, K.M. T2 weighted MRI derived textural features reflect prostate cancer aggressiveness: Preliminary results. Eur. Radiol. 2017, 27, 3050–3059. [Google Scholar] [CrossRef]
- Kelcz, F.; Jarrard, D.F. Prostate cancer: The applicability of textural analysis of MRI for grading. Nature reviews. Urology 2016, 13, 185–186. [Google Scholar] [CrossRef]
- Zhang, L.; Jiang, D.; Chen, C.; Yang, X.; Lei, H.; Kang, Z.; Huang, H.; Pang, J. Development and validation of a multiparametric MRI-based radiomics signature for distinguishing between indolent and aggressive prostate cancer. Br. J. Radiol. 2021, 95, 20210191. [Google Scholar] [CrossRef]
- Bonekamp, D.; Kohl, S.; Wiesenfarth, M.; Schelb, P.; Radtke, J.P.; Götz, M.; Kickingereder, P.; Yaqubi, K.; Hitthaler, B.; Gählert, N.; et al. Radiomic Machine Learning for Characterization of Prostate Lesions with MRI: Comparison to ADC Values. Radiology 2018, 289, 128–137. [Google Scholar] [CrossRef] [PubMed]
- Hectors, S.J.; Chen, C.; Chen, J.; Wang, J.; Gordon, S.; Yu, M.; Al Hussein Al Awamlh, B.; Sabuncu, M.R.; Margolis, D.J.A.; Hu, J.C. Magnetic Resonance Imaging Radiomics-Based Machine Learning Prediction of Clinically Significant Prostate Cancer in Equivocal PI-RADS 3 Lesions. J. Magn. Reson. Imaging 2021, 54, 1466–1473. [Google Scholar] [CrossRef] [PubMed]
- Zhang, H.; Li, X.; Zhang, Y.; Huang, C.; Wang, Y.; Yang, P.; Duan, S.; Mao, N.; Xie, H. Diagnostic nomogram based on intralesional and perilesional radiomics features and clinical factors of clinically significant prostate cancer. J. Magn. Reson. Imaging 2021, 53, 1550–1558. [Google Scholar] [CrossRef] [PubMed]
- Giannini, V.; Mazzetti, S.; Defeudis, A.; Stranieri, G.; Calandri, M.; Bollito, E.; Bosco, M.; Porpiglia, F.; Manfredi, M.; de Pascale, A.; et al. A Fully Automatic Artificial Intelligence System Able to Detect and Characterize Prostate Cancer Using Multiparametric MRI: Multicenter and Multi-Scanner Validation. Front. Oncol. 2021, 11, 718155. [Google Scholar] [CrossRef]
- Parra, N.A.; Lu, H.; Choi, J.; Gage, K.; Pow-Sang, J.; Gillies, R.J.; Balagurunathan, Y. Habitats in DCE-MRI to Predict Clinically Significant Prostate Cancers. Tomography 2019, 5, 68–76. [Google Scholar] [CrossRef]
- Winkel, D.J.; Breit, H.C.; Block, T.K.; Boll, D.T.; Heye, T.J. High spatiotemporal resolution dynamic contrast-enhanced MRI improves the image-based discrimination of histopathology risk groups of peripheral zone prostate cancer: A supervised machine learning approach. Eur. Radiol. 2020, 30, 4828–4837. [Google Scholar] [CrossRef]
- Han, C.; Ma, S.; Liu, X.; Liu, Y.; Li, C.; Zhang, Y.; Zhang, X.; Wang, X. Radiomics Models Based on Apparent Diffusion Coefficient Maps for the Prediction of High-Grade Prostate Cancer at Radical Prostatectomy: Comparison with Preoperative Biopsy. J. Magn. Reson. Imaging 2021, 54, 1892–1901. [Google Scholar] [CrossRef]
- Li, M.; Yang, L.; Yue, Y.; Xu, J.; Huang, C.; Song, B. Use of Radiomics to Improve Diagnostic Performance of PI-RADS v2.1 in Prostate Cancer. Front. Oncol. 2021, 10, 631831. [Google Scholar] [CrossRef]
- Zhang, K.S.; Schelb, P.; Kohl, S.; Radtke, J.P.; Wiesenfarth, M.; Schimmöller, L.; Kuder, T.A.; Stenzinger, A.; Hohenfellner, M.; Schlemmer, H.P.; et al. Improvement of PI-RADS-dependent prostate cancer classification by quantitative image assessment using radiomics or mean ADC. Magn. Reson. Imaging 2021, 82, 9–17. [Google Scholar] [CrossRef]
- Wang, J.; Wu, C.J.; Bao, M.L.; Zhang, J.; Wang, X.N.; Zhang, Y.D. Machine learning-based analysis of MR radiomics can help to improve the diagnostic performance of PI-RADS v2 in clinically relevant prostate cancer. Eur. Radiol. 2017, 27, 4082–4090. [Google Scholar] [CrossRef]
- Hou, Y.; Bao, M.L.; Wu, C.J.; Zhang, J.; Zhang, Y.D.; Shi, H.B. A radiomics machine learning-based redefining score robustly identifies clinically significant prostate cancer in equivocal PI-RADS score 3 lesions. Abdom. Radiol. 2020, 45, 4223–4234. [Google Scholar] [CrossRef]
- Castillo, T.J.M.; Starmans, M.P.A.; Arif, M.; Niessen, W.J.; Klein, S.; Bangma, C.H.; Schoots, I.G.; Veenland, J.F. A Multi-Center, Multi-Vendor Study to Evaluate the Generalizability of a Radiomics Model for Classifying Prostate cancer: High Grade vs. Low Grade. Diagnostics 2021, 11, 369. [Google Scholar] [CrossRef] [PubMed]
- Khosravi, P.; Lysandrou, M.; Eljalby, M.; Li, Q.; Kazemi, E.; Zisimopoulos, P.; Sigaras, A.; Brendel, M.; Barnes, J.; Ricketts, C.; et al. A Deep Learning Approach to Diagnostic Classification of Prostate Cancer Using Pathology-Radiology Fusion. J. Magn. Reson. Imaging 2021, 54, 462–471. [Google Scholar] [CrossRef] [PubMed]
- Chen, T.; Li, M.; Gu, Y.; Zhang, Y.; Yang, S.; Wei, C.; Wu, J.; Li, X.; Zhao, W.; Shen, J. Prostate Cancer Differentiation and Aggressiveness: Assessment with a Radiomic-Based Model vs. PI-RADS v2. J. Magn. Reson. Imaging 2019, 49, 875–884. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- He, X.; Xiong, H.; Zhang, H.; Liu, X.; Zhou, J.; Guo, D. Value of MRI texture analysis for predicting new Gleason grade group. Br. J. Radiol. 2021, 94, 20210005. [Google Scholar] [CrossRef] [PubMed]
- Cuocolo, R.; Stanzione, A.; Ponsiglione, A.; Romeo, V.; Verde, F.; Creta, M.; La Rocca, R.; Longo, N.; Pace, L.; Imbriaco, M. Clinically significant prostate cancer detection on MRI: A radiomic shape features study. Eur. J. Radiol. 2019, 116, 144–149. [Google Scholar] [CrossRef]
- Damascelli, A.; Gallivanone, F.; Cristel, G.; Cava, C.; Interlenghi, M.; Esposito, A.; Brembilla, G.; Briganti, A.; Montorsi, F.; Castiglioni, I.; et al. Advanced Imaging Analysis in Prostate MRI: Building a Radiomic Signature to Predict Tumor Aggressiveness. Diagnostics 2021, 11, 594. [Google Scholar] [CrossRef]
- Min, X.; Li, M.; Dong, D.; Feng, Z.; Zhang, P.; Ke, Z.; You, H.; Han, F.; Ma, H.; Tian, J.; et al. Multi-parametric MRI-based radiomics signature for discriminating between clinically significant and insignificant prostate cancer: Cross-validation of a machine learning method. Eur. J. Radiol. 2019, 115, 16–21. [Google Scholar] [CrossRef] [Green Version]
- Xiong, H.; He, X.; Guo, D. Value of MRI texture analysis for predicting high-grade prostate cancer. Clin. Imaging 2021, 72, 168–174. [Google Scholar] [CrossRef]
- Liu, Y.; Zheng, H.; Liang, Z.; Miao, Q.; Brisbane, W.G.; Marks, L.S.; Raman, S.S.; Reiter, R.E.; Yang, G.; Sung, K. Textured-Based Deep Learning in Prostate Cancer Classification with 3T Multiparametric MRI: Comparison with PI-RADS-Based Classification. Diagnostics 2021, 11, 1785. [Google Scholar] [CrossRef]
- Sanford, T.; Harmon, S.A.; Turkbey, E.B.; Kesani, D.; Tuncer, S.; Madariaga, M.; Yang, C.; Sackett, J.; Mehralivand, S.; Yan, P.; et al. Deep-Learning-Based Artificial Intelligence for PI-RADS Classification to Assist Multiparametric Prostate MRI Interpretation: A Development Study. J. Magn. Reson. Imaging 2020, 52, 1499–1507. [Google Scholar] [CrossRef] [PubMed]
- Schelb, P.; Kohl, S.; Radtke, J.P.; Wiesenfarth, M.; Kickingereder, P.; Bickelhaupt, S.; Kuder, T.A.; Stenzinger, A.; Hohenfellner, M.; Schlemmer, H.P.; et al. Classification of Cancer at Prostate MRI: Deep Learning versus Clinical PI-RADS Assessment. Radiology 2019, 293, 607–617. [Google Scholar] [CrossRef] [PubMed]
- Peng, T.; Xiao, J.; Li, L.; Pu, B.; Niu, X.; Zeng, X.; Wang, Z.; Gao, C.; Li, C.; Chen, L.; et al. Can machine learning-based analysis of multiparameter MRI and clinical parameters improve the performance of clinically significant prostate cancer diagnosis? Int. J. Comput. Assist. Radiol. Surg. 2021, 16, 2235–2249. [Google Scholar] [CrossRef] [PubMed]
- Patel, N.U.; Lind, K.E.; Garg, K.; Crawford, D.; Werahera, P.N.; Pokharel, S.S. Assessment of PI-RADS v2 categories ≥ 3 for diagnosis of clinically significant prostate cancer. Abdom. Radiol. 2019, 44, 705–712. [Google Scholar] [CrossRef] [PubMed]
- Hou, Y.; Zhang, Y.H.; Bao, J.; Bao, M.L.; Yang, G.; Shi, H.B.; Song, Y.; Zhang, Y.D. Artificial intelligence is a promising prospect for the detection of prostate cancer extracapsular extension with mpMRI: A two-center comparative study. Eur. J. Nucl. Med. Mol. Imaging 2021, 48, 3805–3816. [Google Scholar] [CrossRef]
- Cuocolo, R.; Stanzione, A.; Faletti, R.; Gatti, M.; Calleris, G.; Fornari, A.; Gentile, F.; Motta, A.; Dell’Aversana, S.; Creta, M.; et al. MRI index lesion radiomics and machine learning for detection of extraprostatic extension of disease: A multicenter study. Eur. Radiol. 2021, 31, 7575–7583. [Google Scholar] [CrossRef]
- Bai, H.; Xia, W.; Ji, X.; He, D.; Zhao, X.; Bao, J.; Zhou, J.; Wei, X.; Huang, Y.; Li, Q.; et al. Multiparametric Magnetic Resonance Imaging-Based Peritumoral Radiomics for Preoperative Prediction of the Presence of Extracapsular Extension with Prostate Cancer. J. Magn. Reson. Imaging 2021, 54, 1222–1230. [Google Scholar] [CrossRef]
- He, D.; Wang, X.; Fu, C.; Wei, X.; Bao, J.; Ji, X.; Bai, H.; Xia, W.; Gao, X.; Huang, Y.; et al. MRI-based radiomics models to assess prostate cancer, extracapsular extension and positive surgical margins. Cancer Imaging 2021, 21, 46. [Google Scholar] [CrossRef]
- Xu, L.; Zhang, G.; Zhao, L.; Mao, L.; Li, X.; Yan, W.; Xiao, Y.; Lei, J.; Sun, H.; Jin, Z. Radiomics Based on Multiparametric Magnetic Resonance Imaging to Predict Extraprostatic Extension of Prostate Cancer. Front. Oncol. 2020, 10, 940. [Google Scholar] [CrossRef]
- Ma, S.; Xie, H.; Wang, H.; Han, C.; Yang, J.; Lin, Z.; Li, Y.; He, Q.; Wang, R.; Cui, Y.; et al. MRI-Based Radiomics Signature for the Preoperative Prediction of Extracapsular Extension of Prostate Cancer. J. Magn. Reason. Imaging 2019, 50, 1914–1925. [Google Scholar] [CrossRef]
- Ma, S.; Xie, H.; Wang, H.; Yang, J.; Han, C.; Wang, X.; Zhang, X. Preoperative Prediction of Extracapsular Extension: Radiomics Signature Based on Magnetic Resonance Imaging to Stage Prostate Cancer. Mol. Imaging Biol. 2020, 22, 711–721. [Google Scholar] [CrossRef] [PubMed]
- Soerensen, S.J.C.; Fan, R.E.; Seetharaman, A.; Chen, L.; Shao, W.; Bhattacharya, I.; Kim, Y.H.; Sood, R.; Borre, M.; Chung, B.I.; et al. Deep Learning Improves Speed and Accuracy of Prostate Gland Segmentations on Magnetic Resonance Imaging for Targeted Biopsy. J. Urol. 2021, 206, 604–612. [Google Scholar] [CrossRef] [PubMed]
- Van de Ven, W.J.; Hulsbergen-van de Kaa, C.A.; Hambrock, T.; Barentsz, J.O.; Huisman, H.J. Simulated required accuracy of image registration tools for targeting high-grade cancer components with prostate biopsies. Eur. Radiol. 2013, 23, 1401–1407. [Google Scholar] [CrossRef] [PubMed]
- Campa, R.; del Monte, M.; Barchetti, G.; Pecoraro, M.; Salvo, V.; Ceravolo, I.; Indino, E.L.; Ciardi, A.; Catalano, C.; Panebianco, V. Improvement of prostate cancer detection combining a computer-aided diagnostic system with TRUS-MRI targeted biopsy. Abdom. Radiol. 2019, 44, 264–271. [Google Scholar] [CrossRef] [PubMed]
- Ferriero, M.; Anceschi, U.; Bove, A.M.; Bertini, L.; Flammia, R.S.; Zeccolini, G.; de Concilio, B.; Tuderti, G.; Mastroianni, R.; Misuraca, L.; et al. Fusion US/MRI prostate biopsy using a computer aided diagnostic (CAD) system. Minerva Urol. Nephrol. 2021, 73, 616–624. [Google Scholar] [CrossRef]
- Ytre-Hauge, S.; Dybvik, J.A.; Lundervold, A.; Salvesen, Ø.O.; Krakstad, C.; Fasmer, K.E.; Werner, H.M.; Ganeshan, B.; Høivik, E.; Bjørge, L.; et al. Preoperative tumor texture analysis on MRI predicts high-risk disease and reduced survival in endometrial cancer. J. Magn. Reason. Imaging 2018, 48, 1637–1647. [Google Scholar] [CrossRef]
- Israël, B.; Leest, M.V.; Sedelaar, M.; Padhani, A.R.; Zámecnik, P.; Barentsz, J.O. Multiparametric Magnetic Resonance Imaging for the Detection of Clinically Significant Prostate Cancer: What Urologists Need to Know. Part 2: Interpretation. Eur. Urol. 2020, 77, 469–480. [Google Scholar] [CrossRef]
- Hambrock, T.; Vos, P.C.; Hulsbergen-van de Kaa, C.A.; Barentsz, J.O.; Huisman, H.J. Prostate cancer: Computer-aided diagnosis with multiparametric 3-T MR imaging—Effect on observer performance. Radiology 2013, 266, 521–530. [Google Scholar] [CrossRef] [Green Version]
- Naji, L.; Randhawa, H.; Sohani, Z.; Dennis, B.; Lautenbach, D.; Kavanagh, O.; Bawor, M.; Banfield, L.; Profetto, J. Digital Rectal Examination for Prostate Cancer Screening in Primary Care: A Systematic Review and Meta-Analysis. Ann. Fam. Med. 2018, 16, 149–154. [Google Scholar] [CrossRef]
- Soeterik, T.F.W.; van Melick, H.H.E.; Dijksman, L.M.; Biesma, D.H.; Witjes, J.A.; van Basten, J.A. Multiparametric Magnetic Resonance Imaging Should Be Preferred Over Digital Rectal Examination for Prostate Cancer Local Staging and Disease Risk Classification. Urology 2021, 147, 205–212. [Google Scholar] [CrossRef]
- Song, J.; Yin, Y.; Wang, H.; Chang, Z.; Liu, Z.; Cui, L. A review of original articles published in the emerging field of radiomics. Eur. J. Radiol. 2020, 127, 108991. [Google Scholar] [CrossRef] [PubMed]
- Malik, N.; Geraghty, B.; Dasgupta, A.; Maralani, P.J.; Sandhu, M.; Detsky, J.; Tseng, C.L.; Soliman, H.; Myrehaug, S.; Husain, Z.; et al. MRI radiomics to differentiate between low grade glioma and glioblastoma peritumoral region. J. Neurooncol. 2021, 155, 181–191. [Google Scholar] [CrossRef] [PubMed]
- Priya, S.; Agarwal, A.; Ward, C.; Locke, T.; Monga, V.; Bathla, G. Survival prediction in glioblastoma on post-contrast magnetic resonance imaging using filtration based first-order texture analysis: Comparison of multiple machine learning models. Neuroradiol. J. 2021, 34, 355–362. [Google Scholar] [CrossRef] [PubMed]
- Lupean, R.A.; Ștefan, P.A.; Csutak, C.; Lebovici, A.; Măluțan, A.M.; Buiga, R.; Melincovici, C.S.; Mihu, C.M. Differentiation of Endometriomas from Ovarian Hemorrhagic Cysts at Magnetic Resonance: The Role of Texture Analysis. Medicina 2020, 56, 487. [Google Scholar] [CrossRef]
| No. | Study | No. of Centers | Total Cases | Study Protocol | mpMRI Field Power (T) | Sequences Used for Features Extraction | Segmentation | Ground Truth | Focus Region |
|---|---|---|---|---|---|---|---|---|---|
| 1. | Zhang et al., 2021 [10] | Unicentric | 139 | Training n = 93 Testing n = 46 | 3 | T2WI DWI | Manual | Systematic prostate biopsy | PZ |
| 2. | Bonekamp et al., 2018 [11] | Unicentric | 316 | Training n = 183 Testing n = 133 | 3 | T2WI ADC | Manual | Targeted prostate biopsy | PZ + TZ |
| 3. | Hectors et al., 2021 [12] | Unicentric | 240 | Training n = 188 Testing n = 52 | 3 | T2WI | Manual | Targeted prostate biopsy | PZ + TZ (Same protocol) |
| 4. | Zhang et al., 2021 [13] | Unicentric | 140 | Training n = 105 Testing n = 35 | 3 | T2WI ADC DCE | Manual | Systematic prostate biopsy Radical prostatectomy specimen | WG |
| 5. | Giannini et al., 2021 [14] | Multicentric | 149 | Training n = 81 Testing n = 38 Validation n = 30 | 1.5 | T2WI ADC | Automated | Radical prostatectomy specimen | PZ |
| 6. | Parra et al., 2019 [15] | Unicentric | 72 | Single cohort | 1.5/3 | DCE | Manual | Systematic prostate biopsy | PZ + TZ |
| 7. | Winkel et al., 2020 [16] | Unicentric | 402 | Benign n = 201 Low risk n = 57 Intermediate risk n = 97 High risk n = 47 | 3 | DCE | Manual | Targeted prostate biopsy | PZ |
| 8. | Han et al., 2021 [17] | Unicentric | 176 | Training n = 123 Testing n = 53 | 3 | ADC | Automated versus Manual | Radical prostatectomy specimen | WG |
| 9. | Li et al., 2021 [18] | Unicentric | 203 | Training n = 141 Testing n = 62 | 3 | T2WI ADC DWI DCE | Manual | Systematic prostate biopsy Radical prostatectomy specimen | PZ + TZ |
| 10. | Zhang et al., 2021 [19] | Unicentric | 316 | Training n = 183 Testing n = 133 | 3 | ADC | Manual | Targeted prostate biopsy | PZ |
| 11. | Wang et al., 2017 [20] | Unicentric | 54 | Single cohort | 3 | T2WI DWI | Manual | Radical prostatectomy specimen | PZ + TZ |
| 12. | Hou et al., 2020 [21] | Unicentric | 263 | Single cohort | 3 | T2WI ADC DWI | Manual | Systematic prostate biopsy Radical prostatectomy specimen | PZ + TZ (Same protocol) |
| 13. | Castillo et al., 2021 [22] | Multicentric | 204 | Training n = 48 Testing n = 84 Validation n = 72 | 1.5/3 | T2WI ADC DWI | Manual | Radical prostatectomy specimen | PZ + TZ |
| 14. | Khosravi et al., 2021 [23] | Multicentric | 400 | Training n = 95 Testing n = 305 | 1.5/3 | T2WI | Automated | Targeted prostate biopsy Radical prostatectomy specimen | PZ |
| 15. | Chen et al., 2019 [24] | Unicentric | 381 | Benign n = 266 Malignant n = 115 | 3 | T2WI ADC | Manual | Systematic prostate biopsy | PZ + TZ (Same protocol) |
| 16. | He et al., 2021 [25] | Unicentric | 58 | Single cohort | 1.5 | T2WI ADC | Manual | Systematic prostate biopsy | PZ |
| 17. | Cuocolo et al., 2019 [26] | Unicentric | 75 | Single cohort | 3 | T2WI ADC | Manual | Targeted prostate biopsy | PZ |
| 18. | Damascelli et al., 2021 [27] | Unicentric | 62 | Single cohort | 1.5 | T2WI ADC | Semiautomated | Radical prostatectomy specimen | PZ + TZ (Same protocol) |
| 19. | Min et al., 2019 [28] | Unicentric | 280 | Training n = 187 Testing n = 93 | 3 | T2WI ADC DWI | Manual | Targeted prostate biopsy | PZ + TZ |
| 20. | Xiong et al., 2020 [29] | Unicentric | 85 | Single cohort | 1.5 | T2WI ADC | Manual | Systematic prostate biopsy | PZ + TZ (Same protocol) |
| 21. | Liu et al., 2021 [30] | Unicentric | 466 | Training and testing n = 324 Validation n = 142 | 3 | T2WI ADC | Manual | Radical prostatectomy specimen | PZ + TZ + AFMS |
| 22. | Sanford et al., 2020 [31] | Multicentric | 1034 | Training n = 727 Testing n = 212 Validation n = 95 | 3 | T2WI ADC DWI | Manual | Targeted prostate biopsy | PZ + TZ |
| 23. | Schleb et al., 2019 [32] | Unicentric | 457 | Training n = 369 Testing n = 88 | 3 | T2WI ADC DWI | Manual | Targeted prostate biopsy | PZ + TZ |
| 24. | Peng et al., 2021 [33] | Multicentric | 252 | Training n = 135 Testing n = 59 Validation n = 58 | 1.5 | T2WI DCE | Manual | Targeted prostate biopsy | PZ |
| No. | Study | No. of Centers | Total Cases | Study Protocol | mpMRI Field Power (T) | Sequences Used for Features Extraction | Segmentation | Main Goal |
|---|---|---|---|---|---|---|---|---|
| 1. | Ying Hou et al., 2021 [35] | Multicentric | 849 | Training n = 596 Testing n = 150 External validation n = 103 | 3 | T2WI DWI ADC | Automated | Develop and validate an AI based tool to preoperatively assess ECE of localized PCa |
| 2. | Cuocolo et al., 2021 [36] | Multicentric | 193 | Training n = 104 External validation 1 n = 43 External validation 2 n = 46 | 1.5/3 (2 vendors) | T2WI ADC | Manual | Build an ML model to detect ECE based on radiomics |
| 3. | Bai et al., 2021 [37] | Multicentric | 284 | Training n = 158 Internal validation n = 68 External validation n = 58 | 3 (3 vendors) | T2WI ADC | Manual | Preoperative prediction of ECE using peritumoral radiomics |
| 4. | He et al., 2021 [38] | Unicentric | 273 | Training n = 192 Testing n = 81 | 3 | T2WI ADC | Manual | Radiomics model for predicting ECE and PSM |
| 5. | Xu et al., 2020 [39] | Unicentric | 115 | Training n = 82 (35 ECE and 47 non-ECE) Testing n = 33 (14 ECE and 19 non-ECE) | 3 | T2WI DWI ADC DCE | Manual | Preoperative prediction of ECE using radiomics signature |
| 6. | Ma et al., 2019 [40] | Unicentric | 210 | Training n = 143 Validation n = 67 | 3 (2 vendors) | T2WI | Manual | Preoperative prediction of ECE using radiomics signature, compared to radiologists’ interpretation |
| 7. | Ma et al., 2019 [41] | Unicentric | 119 | Training n = 74 (148 bilateral samples) Validation n = 45 (90 bilateral samples) | 3 (2 vendors) | T2WI | Manual | Preoperative prediction of side specific ECE status using radiomics signature |
| No. | Study | No. of Centers | Total Cases | mpMRI Field Power (T) | Sequences Used for Features Extraction | Aim of the Study |
|---|---|---|---|---|---|---|
| 1. | Soerensen et al., 2021 [42] | Multicentric | 916 Training n = 805 Testing n = 111 | 1.5/3 (3 vendors) | T2WI | Deep-learning automatic segmentation of the prostate |
| 2. | van de Ven et al., 2013 [43] | Multicentric | 62 | 3 | ADC | Assessing the required spatial alignment accuracy at MRI—guided biopsies |
| 3. | Campa et al., 2018 [44] | Unicentric | 63 | 3 | T2WI DWI DCE | Defining the accuracy of targeted cores sampled using RAD, CAD and TiT prediction |
| 4. | Ferriero et al., 2021 [45] | Multicentric | 183 Fusion biopsy n = 94 CAD assisted n = 89 | 3 | T2WI | Comparing the csPCA detection rate of CAD-assisted targeted biopsies versus stand-alone fusion biopsies |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Telecan, T.; Andras, I.; Crisan, N.; Giurgiu, L.; Căta, E.D.; Caraiani, C.; Lebovici, A.; Boca, B.; Balint, Z.; Diosan, L.; et al. More than Meets the Eye: Using Textural Analysis and Artificial Intelligence as Decision Support Tools in Prostate Cancer Diagnosis—A Systematic Review. J. Pers. Med. 2022, 12, 983. https://doi.org/10.3390/jpm12060983
Telecan T, Andras I, Crisan N, Giurgiu L, Căta ED, Caraiani C, Lebovici A, Boca B, Balint Z, Diosan L, et al. More than Meets the Eye: Using Textural Analysis and Artificial Intelligence as Decision Support Tools in Prostate Cancer Diagnosis—A Systematic Review. Journal of Personalized Medicine. 2022; 12(6):983. https://doi.org/10.3390/jpm12060983
Chicago/Turabian StyleTelecan, Teodora, Iulia Andras, Nicolae Crisan, Lorin Giurgiu, Emanuel Darius Căta, Cosmin Caraiani, Andrei Lebovici, Bianca Boca, Zoltan Balint, Laura Diosan, and et al. 2022. "More than Meets the Eye: Using Textural Analysis and Artificial Intelligence as Decision Support Tools in Prostate Cancer Diagnosis—A Systematic Review" Journal of Personalized Medicine 12, no. 6: 983. https://doi.org/10.3390/jpm12060983
APA StyleTelecan, T., Andras, I., Crisan, N., Giurgiu, L., Căta, E. D., Caraiani, C., Lebovici, A., Boca, B., Balint, Z., Diosan, L., & Lupsor-Platon, M. (2022). More than Meets the Eye: Using Textural Analysis and Artificial Intelligence as Decision Support Tools in Prostate Cancer Diagnosis—A Systematic Review. Journal of Personalized Medicine, 12(6), 983. https://doi.org/10.3390/jpm12060983







