Educational Intervention in Rehabilitation to Improve Functional Capacity after Hip Arthroplasty: A Scoping Review
Abstract
:1. Introduction
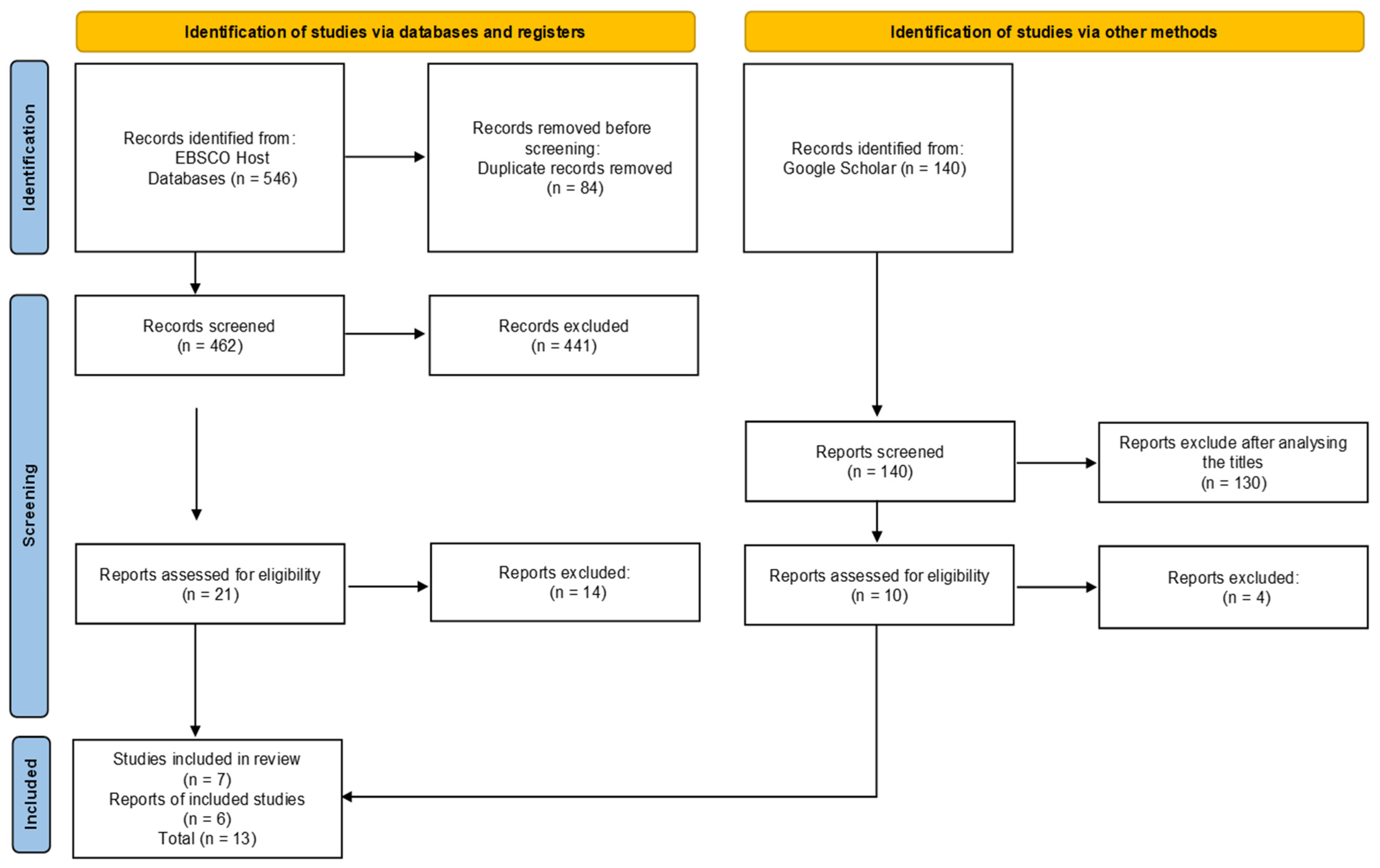
2. Materials and Methods
2.1. Study Design
2.2. Elegibility Criteria
- P—(Population) adults and older persons’ who underwent hip arthroplasty;
- C—(Concept) educational rehabilitation interventions;
- C—(Context) hospital and rehabilitation units.
2.3. Data Collection
2.4. Data Processing and Analysis
3. Results
4. Discussion
Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Esquenazi, D.; Silva, S.; Guimarães, M. Pathophysiological aspects of human aging and falls in the elderly. Rev. Hosp. Univ. Pedro Ernesto 2014, 13, 11–20. [Google Scholar] [CrossRef] [Green Version]
- Barnes, R.Y.; Bodenstein, K.; Human, N.; Raubenheimer, J.; Dawkins, J.; Jacobs, J.; Van der Linde, J.; Venter, R. Preoperative education in the hip and knee arthroplasty patients in Bloemfontein. S. Afr. J. Physiother. 2018, 74, 1–7. [Google Scholar] [CrossRef] [Green Version]
- Sousa, L.; Carvalho, M. Pessoa com Osteoartrose na Anca e Joelho em Contexto de Internamento em Ortopedia. In C. Marques-Vieira e L. Sousa, Cuidados de Enfermagem de Reabilitação à pessoa ao Longo da Vida; Lusodidacta: Loures, Portugal, 2017; pp. 405–420. [Google Scholar]
- Júnior, D.; Castro, A.; Fonseca, E.; Baptista, E.; Padial, M.; Rosemberg, L. Main complications of hip arthroplasty: Pictorial essay. Radiol. Bras. 2020, 53, 56–62. [Google Scholar] [CrossRef] [PubMed]
- Pinto, V.M.P. Efeitos de um Programa de Reabilitação Instituído a Pessoas Submetidas a Artroplastia Total da Anca. Master’s Thesis, Instituto Politécnico de Bragança, Bragança, Portugal, 2016. Available online: https://bibliotecadigital.ipb.pt/handle/10198/13077 (accessed on 10 December 2021).
- Violante, A. Efetividade de Ensino Pré-operatório em Doentes Submetidos a Artroplastia Total da Anca. Master’s Thesis, Escola Superior de Enfermagem de Coimbra, Coimbra, Portugal, 2014. Available online: https://scholar.google.pt/scholar?q=).+Efetividade+de+Ensino+Pr%C3%A9-operat%C3%B3rio+em+Doentes+Submetidos+a+Artroplastia+Total+da+Anca.&hl=pt-PT&as_sdt=0&as_vis=1&oi=scholart (accessed on 10 December 2021).
- Yeh, M.-L.; Chen, H.-H.; Liu, P.-H. Effects of multimedia with printed nursing guide in education on self-efficacy and functional activity and hospitalization in patients with hip replacement. Patient Educ. Couns. 2005, 57, 217–224. [Google Scholar] [CrossRef] [PubMed]
- Thawanna, J.B.G.; Ferreira, B.A.S.; Baixinho, C.L.; Ferreira, O.M.R. Algorithm for transitional care for dependent elderly caregivers: Validation study. Rev. Bras. Enferm. 2021, 74, e20200625. [Google Scholar] [CrossRef]
- Olsson, L.E.; Karlsson, J.; Berg, U.; Kärrholm, J.; Hansson, E. Person-centred care compared with standardized care for patients undergoing total hip arthroplasty—A quasi-experimental study. J. Orthop. Surg. Res. 2014, 9, 95. [Google Scholar] [CrossRef] [Green Version]
- Arksey, H.; O’Malley, L. Scoping studies: Towards a methodological framework. Int. J. Soc. Res. Methodol. 2005, 8, 19–32. [Google Scholar] [CrossRef] [Green Version]
- Munn, Z.; Peters, M.D.J.; Stern, C.; Tufanaru, C.; McArthur, A.; Aroamtaris, E. Systematic review or scoping review? Guidance for authors when choosing between a systematic or scoping review approach. BMC Med. Res. Methodol. 2018, 18, 143. [Google Scholar] [CrossRef]
- Tricco, A.C.; Lillie, E.; Zarin, W.; O’Brien, K.K.; Colquhoun, H.; Levac, D.; Moher, D.; Peters, M.D.; Horsley, T.; Weeks, L.; et al. PRISMA extension for scoping reviews (PRISMA-ScR): Checklist and explanation. Ann. Intern. Med. 2018, 169, 467–473. [Google Scholar] [CrossRef] [Green Version]
- Apóstolo, J. Síntese da Evidência no Contexto da Translação da Ciência; Escola Superior de Enfermagem de Coimbra: Coimbra, Portugal, 2017. [Google Scholar]
- Roos, E. Effectiveness and practice variation of rehabilitation after joint replacement. Curr. Opin. Rheumatol. 2003, 15, 160–162. [Google Scholar] [CrossRef]
- Froehlig, P.; Le Mouel, S.; Coudeyre, E.; Revel, M.; Rannou, F. What is the interest of early mobilization after total hip arthroplasty? Development of French guidelines for clinical practice. Ann. Readapt. Med. Phys. 2008, 51, 212–217. [Google Scholar] [CrossRef] [PubMed]
- Götz, J.; Leiss, F.; Maderbacher, G.; Meyer, M.; Reinhard, J.; Zeman, F.; Grifka, J.; Greimel, F. Implementing fast-track in total hip arthroplasty: Rapid mobilization with low need for pain medication and low pain values: Retrospective analysis of 102 consecutive patients. Z. Rheumatol. 2021, 81, 253–262. [Google Scholar] [CrossRef] [PubMed]
- Raphael, M.; Jaeger, M.; van Vlymen, J. Easily adoptable total joint arthroplasty program allows discharge home in two days. Can. J. Anaesth. 2021, 58, 902–910. [Google Scholar] [CrossRef] [Green Version]
- Smith, T.; McCabe, C.; Lister, S.; Christie, S.; Cross, J. Rehabilitation implications during the development of the Norwich Enhanced Recovery Programme (NERP) for patients following total knee and total hip arthroplasty. Orthop. Traumatol. Surg. Res. 2012, 98, 499–505. [Google Scholar] [CrossRef] [PubMed]
- Musumeci, A.; Pranovi, G.; Masiero, S. Patient education and rehabilitation after hip arthroplasty in an Italian spa center: A pilot study on its feasibility. Int. J. Biometeorol. 2018, 62, 1489–1496. [Google Scholar] [CrossRef] [PubMed]
- Ninlerd, C.; Dungkong, S.; Phuangphay, G.; Amornsupak, C.; Narkbunnam, R. Effect of Home-Based Rehabilitation Exercise Program for Elderly Patients with Femoral Neck Fracture after Bipolar Hemiarthroplasty. Siriraj Med. J. 2019, 72, 315–320. [Google Scholar] [CrossRef]
- Dong, R.; Chen, H. Application of Functional Exercise Nursing Plan Based on Evidence-based Nursing after Hip Replacement. J. Clin. Nurs. Res. 2020, 4, 25–28. Available online: http://ojs.bbwpublisher.com/index.php/JCNR/article/view/1210 (accessed on 10 December 2021). [CrossRef]
- Holsgaard-Larsen, A.; Hermann, A.; Zerahn, B.; Mejdahl, S.; Overgaard, S. Effects of progressive resistance training prior to total HIP arthroplasty—A secondary analysis of a randomized controlled trial. Osteoarthr. Res. Soc. Int. 2020, 28, 1038–1045. [Google Scholar] [CrossRef]
- Hua-ping, S. An Analysis for the application of rapid rehabilitation surgery concept in the nursing satisfaction of the perioperative period of the elderly’s hip arthroplasty. Med. Res. 2020, 2, 21–25. [Google Scholar] [CrossRef]
- Mehta, S.; Hume, E.; Troxel, A.; Reitz, C.; Norton, L.; Lacko, H.; McDonald, C.; Freeman, J.; Marcus, N.; Volpp, K.G.; et al. Effect of Remote Monitoring on Discharge to Home, Return to Activity, and Rehospitalization after Hip and Knee Arthroplasty. A Randomized Clinical Trial. JAMA Netw. Open 2020, 3, e2028328. [Google Scholar] [CrossRef]
- Saraiva, P.; Anunciação, S.; Pontinha, C.; Neves, I.; Batista, A.; Monteiro, G. Gains in functional independence as a promoter of quality of life. Millenium 2020, 2, 225–231. [Google Scholar] [CrossRef]
- Jordan, Z.; Lockwood, C.; Munn, Z.; Aromataris, E. The updated Joanna Briggs Institute Model of Evidence-Based Healthcare. Int. J. Evid. Based Healthc. 2019, 17, 58–71. [Google Scholar] [CrossRef] [PubMed]
- Sousa, L.; Martins, M.M.; Novo, A. A Enfermagem de Reabilitação no Empoderamento e Capacitação da Pessoa em Processos de Transição saúde-Doença. Rev. Port. Enferm. Reabil. 2020, 3, 64–69. [Google Scholar] [CrossRef]
- Calle Jimenez, T.; Sanchez Gordon, S.; Rybarczyk, Y.; Jadán, J.; Villarreal, S.; Esparza, W.; Acosta Vargas, P.; Guevara, C.; Nunes, I.L. Analysis and Improvement of the web accessibility of a telerehabilitation platform for hip arthroplasty patients. In Advances in Human Factors and Systems Interaction; AHFE 2018. Advances in Intelligent Systems and Computing; Nunes, I., Ed.; Springer: Orlando, FL, USA, 2019; Volume 781, pp. 233–245. [Google Scholar] [CrossRef]
- Saunders, R.; Seaman, K.; Ashford, C.; Sullivan, T.; McDowall, J.; Whitehead, L.; Ewens, B.; Pedler, K.; Gullick, K. An eHealth program for patients undergoing a total hip arthroplasty: Protocol for a randomized controlled trial. JMIR Res. Protoc. 2018, 7, e137. Available online: http://www.researchprotocols.org/2018/6/e137/ (accessed on 10 December 2021). [CrossRef] [PubMed]
- Suso Martí, L.; La Touche, R.; Herranz Gómez, A.; Angulo Díaz Parreño, S.; Paris Alemany, A.; Cuenca Martinez, F. Effectiveness of telerehabilitation in Physical Therapy Practice: Na Umbrella and Mapping Review with Meta–Meta–Analisys. Phys. Ther. 2021, 101, pzab075. [Google Scholar] [CrossRef] [PubMed]
- Vesterby, M.; Pedersen, P.; Laursen, M.; Mikkersen, S.; Larsen, J.; Soballe, K.; Jorgensen, B. Telemedicine support shortens length of stay after fast-track hip replacement. Acta Orthop. 2017, 88, 41–47. Available online: https://pubmed.ncbi.nlm.nih.gov/28097941/ (accessed on 10 December 2021). [CrossRef] [Green Version]
- Padovan, A.; Kuvacic, G.; Gulotta, F.; Sellami, M.; Bruno, C.; Isoardi, M.; De Giorgio, A. A new integrative approach to increase quality of life by reducing pain and fear of movement in patients undergoing total hip arthroplasty: The IARA model. Psychol. Health Med. 2018, 23, 1223–1230. [Google Scholar] [CrossRef]
- Zhao, J.; Davis, S.P. Na integrative review of multimodel pain manegement on patient recovery after total hip and knee arthroplasty. Int. J. Nurs. Stud. 2019, 96, 94–106. [Google Scholar] [CrossRef]
- Barros, E.; Cambruzzi, G.; Souza, J.; Barroso, J.; Silva, L. Cuidados e Orientações ao Paciente Submetido a Artroplastia de Quadril; Perse: Florianópolis, Brazil, 2017; Available online: http://www.cefid.udesc.br/?id=120 (accessed on 10 December 2021).
- Christelis, N.; Wallace, S.; Sage, C.; Babitu, U.; Liew, S.; Dugal, J.; Nyulasi, I.; Mutalima, N.; Tran, T.; Myles, P. An enhanced recovery after surgery program for hip and knee arthroplasty. Med. J. Aust. 2015, 202, 363–369. [Google Scholar] [CrossRef] [Green Version]
- Zhu, S.; Qian, W.; Jiang, C.; Ye, C.; Chen, X. Enhanced recovery after surgery for hip and knee arthroplasty: A systematic review and meta-analysis. Postgrad. Med. J. 2017, 93, 736–742. [Google Scholar] [CrossRef]
- Ripollés-Melchor, J.; Abad-Motos, A.; Díez-Remesal, Y.; Aseguinolaza-Pagola, M.; Padin-Barreiro, L.; Sánchez-Martín, R.; Logroño-Egea, M.; Catalá-Bauset, J.C.; García-Orallo, S.; Bisbe, E.; et al. Association between Use of Enhanced Recovery after Surgery Protocol and Postoperative Complications in Total Hip and Knee Arthroplasty in the Postoperative Outcomes within Enhanced Recovery after Surgery Protocol in Elective Total Hip and Knee Arthroplasty Study (Power2). JAMA Surg. 2020, 155, e196024. [Google Scholar] [CrossRef] [PubMed]
- Baixinho, C.L.; Presado, M.H.; Ribeiro, J. Qualitative research and the transformation of public health. Cien. Saude Colet. 2019, 24, 1583. [Google Scholar] [CrossRef] [Green Version]
- Wainwright, T.; Gill, M.; McDonald, D.; Middleton, R.; Reed, M.; Sahota, O.; Yates, P.; Ljungqvist, O. Consensus statement for perioperative care in total hip replacement and total knee replacement surgery: Enhanced Recovery after Surgery (ERAS) Society recommendations. Acta Orthop. 2020, 91, 3–19. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wilson, A. Assistive devices, hip precautions, environmental modifications and training to prevent dislocation and improve function after hip arthroplasty: A Cochrane review summary. Int. J. Nurs. Stud. 2018, 79, 165–166. [Google Scholar] [CrossRef]
- Gogineni, H.C.; Gray, C.F.; Prieto, H.A.; Deen, J.T.; Boezaart, A.P.; Parvataneni, H.K. Transition to outpatient total hip and knee arthroplasty: Experience at an academic tertiary care center. Arthroplast. Today 2018, 5, 100–105. [Google Scholar] [CrossRef] [Green Version]
- Churchil, L.; Pollock, M.; Lebedeva, Y.; Pasic, N.; Bryant, D.; Howard, J.; Lanting, B.; Rudman, D.L. Optimizing outpatient total hip arthroplasty: Perspectives of keys stakeholders. Can. J. Surg. 2018, 61, 370–376. Available online: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6281453/ (accessed on 10 December 2021). [CrossRef] [Green Version]
- Ko, Y.; Lee, Y.; Oh, E.; Choi, M.; Kim, C.; Sung, K.; Baek, S. Older adults with hip arthroplasty: An individualized transitional care program. Rehabil. Nurs. 2019, 44, 203–212. [Google Scholar] [CrossRef] [Green Version]
- Ferreira, E.; Lourenço, O.; Costa, P.; Pinto, S.; Gomes, C.; Oliveira, A.; Ferreira, Ó.; Baixinho, C. Active Life: A project for a safe hospital-community transition after arthroplasty. Rev. Bras. Enferm. 2019, 72, 147–153. [Google Scholar] [CrossRef]
- Ferreira, B.A.L.S.; Gomes, T.J.B.; Baixinho, C.R.S.L.; Ferreira, O.M.R. Transitional care to caregivers of dependent older people: An integrative literature review. Rev. Bras. Enferm. 2020, 73, e20200394. [Google Scholar] [CrossRef]
| Database | Syntax Adopted |
|---|---|
| Medline | (((((((hip arthroplasty[Title/Abstract]) OR (hip replace*[Title/Abstract])) OR (hip[Title/Abstract])) OR (arthroplasty[Title/Abstract])) OR (surger*[Title/Abstract])) OR (arthroplasties, hip replacement[MeSH Terms])) AND ((((((((educational rehabilitation interventions[Title/Abstract]) OR (educ*[Title/Abstract])) OR (reab*[Title/Abstract])) OR (intervent*[Title/Abstract])) OR (activities, educational[MeSH Terms])) OR (health education[MeSH Terms])) OR (care, self rehabilitation[MeSH Terms])) OR (early intervention education[MeSH Terms]))) AND (((((hospital[Title/Abstract]) OR (rehabilitation units[Title/Abstract]))) OR (center, rehabilitation[MeSH Terms])) OR (hospitalization[MeSH Terms])) |
| CINAHL | (TI (“hip arthroplasty” or hip*) and (“Nursing care” or “Rehabilitation” or “Nurs*” and (“Patient education” or “mobilization”) (TI hip arthroplasty OR hip replace OR hip OR arthroplasty OR surger*) OR (AB hip arthroplasty OR hip replace OR hip OR arthroplasty OR surger*) OR (MM “Arthroplasty, Replacement, Hip”)) OR (MM “Hip Surgery”) AND (TI educational rehabilitation interventions OR educ* OR intervent*) OR (AB educational rehabilitation interventions OR educ* OR intervent*) OR ((MH “Nursing Interventions”) OR (MM “Outcomes of Education”) OR (MM “Rehabilitation, Geriatric”)) OR (MM “Nursing Care”) OR (MM “Patient Education”)) AND (TI hospital OR rehabilitation units) OR (AB hospital OR rehabilitation units) OR (MH “Hospital Programs”)) OR (MM “Rehabilitation”)). |
| Cochrane | (“hip arthroplasty” OR hip*) AND (“Nursing care” OR “Rehabilitation” OR “Nurs*” OR “Patient education” OR “mobilization”) AND (Hospital OR Rehabilitation unit) |
| MedicLatina | (“hip arthroplasty” OR hip*) AND (“Nursing care” OR “Rehabilitation” OR “Nurs*” AND (“Patient education” OR “mobilization”) AND (Hospital OR Rehabilitation unit) |
| Google academic | (“hip arthroplasty” OR hip*) AND (“Nursing care” OR “Rehabilitation” OR “Nurs*” OR “Patient education” OR “mobilization”) AND (Hospital OR Rehabilitation unit) |
| Reference | Level of Evidence [26] | Country |
|---|---|---|
| [7] | 2.c—Quasi-experimental study | Taiwan |
| [14] | 2.b—Systematic review of quasi-experimental studies | Sweden |
| [15] | 2.b—Systematic review of quasi-experimental studies | France |
| [16] | 3.c—Retrospective cohort study | Germany |
| [17] | 3.c—Cohort study | Canada |
| [18] | 2.c—Quasi-experimental study | United Kingdom |
| [19] | 2.c—Quasi-experimental study | Italy |
| [20] | Prospective cohort study | Thailand |
| [21] | 1.c—Randomised controlled study | China |
| [22] | 1.c—Randomised controlled study | Denmark |
| [23] | 1.c—Randomised controlled study | China |
| [24] | 1.c—Randomised controlled study | USA |
| [25] | 4—Descriptive, retrospective study of a quantitative nature | Portugal |
| Study/Sample | Study Design and Aim | Intervention | Results |
|---|---|---|---|
| [7] 33 people in the control group and 33 people in the experimental group | Quasi-experimental study. To examine the effects of multimedia with printed nursing guides in the education of the person with hip arthroplasty, on the improvement of self-efficacy, functional activity, and length of hospital stay. | The control group received standard care, which included individual education with leaflets during hospitalisation. The experimental group received a nursing guide in CD and printed forms, with video and audio nursing instructions that addressed aspects about articulation, preparation for surgery, use of assistive devices, and rehabilitation. | The results showed that the experimental group, which received education through multimedia CD and printed nursing guides, showed statistically better self-efficacy and functional activity, and shorter hospital stay than the control group. |
| [14] | Systematic review. To know the exercise-based treatments applied during the postoperative period and the possible implications for discharge destination and health outcomes. | Instruction for early mobilisation is the gold standard for achieving functional mobility, including sufficient range of motion. Exercise improves physical activity-related outcomes after hip arthroplasty. | Patients can achieve similar pain relief and functional capacity when discharged home with therapeutic exercise supervision compared to discharge to a rehabilitation facility. Exercise produces long-term benefits regarding physical function in elderly, improving strength, balance, and other neuromuscular aspects, facilitating functional activities and potentially preventing adverse outcomes such as falls. |
| [15] 200 expert professionals | Systematic review. Developing clinical practice guidelines for early mobilisation following total hip arthroplasty. | Education addresses early mobilisation, transfer, walking, and prevention of dislocating movements. Early mobilisation after hip arthroplasty is an integral part of post-operative management, in the approach to the person and the operated hip. | This early mobilisation plays a crucial role in the person’s initial functional mobilisation, as well as an important role in the prevention of thromboembolic diseases. After this initial period (3 to 4 days), the attention is focused on the prevention of movements with risk of dislocation, the functional transference, and the beginning of gait. |
| [16] 102 people submitted to the rapid treatment programme in hip arthroplasty | Retrospective cohort study. Assessment of function, mobilisation, and pain scores during hospitalisation (6 postoperative days) and 4 weeks after fast-track treatment in hip arthroplasty. | Conducting a multidisciplinary lecture preoperatively and gait training with crutches for all persons, administration of preventive non-steroidal anti-inflammatory drug one hour before the intervention, minimally invasive anterolateral approach under spinal anaesthesia, administration of intravenous dexamethasone, placement of uncemented implants, infiltration of analgesia in the peri-acetabular and femoral region, and administration of tranexamic acid. | The application of a fast-track programme was effective regarding function and mobilisation, as well as pain relief and gait recovery speed. |
| [17] 100 people treated in a fast-track programme compared with 100 people treated before the introduction of this programme | Cohort study. Primary aim: to determine whether a fast-track care model can reduce the length of hospital stay following hip and knee arthroplasty while maintaining the person’s safety. Secondary aim: to compare the incidence of clinically significant outcomes of the fast-track programme with the previous common care programme. | The fast-track programme emphasises pre- and postoperative education, postoperative analgesia with periarticular injection, early mobilisation, and discharge home with an outpatient rehabilitation programme. All were contacted by the nurse 2 to 3 days after discharge for symptom assessment and recovery. | The fast-track programme can reduce postoperative length of stay while maintaining appropriate pain management and safeguarding the person′s satisfaction and safety. All people reported a good surgical and hospital experience. |
| [18] The first 95 consecutive people who underwent total hip arthroplasty or total knee arthroplasty | Quasi-experimental study. To report the outcomes of rehabilitation following a Norwich Enhanced Recovery Programme (NERP) in terms of function and pain at discharge, length of stay, need for rehabilitation services after discharge, and complications during the first 6 weeks after total hip and knee arthroplasty. | All participated in a preoperative educational session that included information on the route within the hospital, postoperative exercises, and advice on physical abilities expected postoperatively; people who were to undergo THA were also taught about care to prevent prosthesis dislocation. In THA surgeries, all implants were cemented, local anaesthetic was injected into the operative wound, and a catheter was placed in the wound for infiltration of local anaesthetic on the first 12 h; no drains were used. Approximately 4 h after surgery, with the local anaesthetic still effective, an assessment was made with the intention of starting the exercises; to do the lifting; and, with a gait aid, to do gait training. | The results of this study indicate that the development of the Norwich Enhanced Recovery Programme (NERP) was a successful rehabilitation regime for patients undergoing total hip arthroplasty (THA) and total knee arthroplasty (TKA), facilitating early and safe discharge with minimal complications. This suggests that initiating mobilisation within 4 h of surgery was important in improving initial functionality outcomes, as well as reducing pain levels and length of stay. |
| [19] 12 consecutive people submitted to total hip arthroplasty | Quasi-experimental study. To evaluate the feasibility and effectiveness of an intensive rehabilitation programme after hip arthroplasty in an Italian spa centre. | All people underwent a 2-week thermo-multimodal rehabilitation programme, which consisted of educational and physical rehabilitation measures. The rehabilitation treatment consisted of six sessions/week of rehabilitation, gait training and balance strategies, kinesiotherapy, and hydro kinesiotherapy in thermal pool. The educational programme was conducted for the people and their families. | The study showed that this intensive treatment was feasible in a thermal spa and was effective, producing good results in terms of pain relief, improving motor and functional capacity, and improving people′s perception of quality of life. Thermal centres with a vocation for rehabilitation can provide various types of rehabilitation procedures, such as physical therapies (electrical, ultrasound, among others) and various forms of kinesiotherapy and functional training, such as passive/active mobilisation, hydro kinesiotherapy, respiratory training, balance and gait training, and health prevention programmes, in addition to traditional thermal therapy. |
| [20] 41 people submitted to cementless bipolar hemiarthroplasty after femoral neck fracture | Prospective cohort study. To investigate the effectiveness of a home-based rehabilitation programme, examining recovery time, risk of falling, improvement in mobility, and improvement in quality of life. | After surgery, participants received instructions on how to perform a home rehabilitation programme. They had to perform exercises every day for 6 months, 10–15 repetitions, 2 sets/3 × a day, including lying down and standing position exercises. The lying down exercises consisted of hip abduction and hip flexion. The standing exercises included hip abduction, extension, and flexion. | The home rehabilitation programme in this study was found to be safe and effective in improving the recovery of people undergoing hip hemiarthroplasty in physical performance and quality of life. All participants were able to return to their pre-injury status within six months. |
| [21] 150 patients who were divided into a control group (75) and an experimental group (75) | Randomised controlled trial. To explore the effect of a functional exercise nursing plan in patients following hip replacement. | The control group received conventional rehabilitation treatment. The experimental group underwent a specific functional exercise nursing plan based on relevant evidence, studies, and methods from the literature, combined with the person′s particular situation and guided by nursing. | The results obtained show that a functional exercise nursing plan based on existing literature and studies in people after hip arthroplasty has a significant effect. It promotes their recovery, improves their quality of life, and reduces the length of hospital stay and the incidence of postoperative complications. |
| [22] 80 patients who were divided into a control group (40) and an experimental group (40) | Randomised controlled study. To investigate the postoperative effect at 12 months of preoperative resistance training in patients undergoing hip arthroplasty on activity and function and expected outcomes on muscle strength and physical performance. | The experimental group participated in a preoperative training program, performed in sessions of 1 h, 2 times a week for 10 weeks. Each session included 10 m warm-up followed by a sequence of 4 exercises performed on training machines (hip extension, knee extension/flexion, and leg press); the exercises were performed at moderate to high intensity in 3 sets of 8 to 12 repetitions with a load adjusted to each person, not causing any pain. The control group received exercises to perform at home, of low intensity without specific resistance exercises. | The results obtained showed that after 12 months of surgery, the preoperative resistance training programme did not provide additional benefit regarding muscle strength and additional tests; however, it provided accelerated rehabilitation by 3 months. Therefore, intensive preoperative training is a viable complement to achieve the earliest onset of postoperative functional recovery after hip arthroplasty. |
| [23] 58 patients divided into a control group (29) and an experimental group (29) | Randomised controlled trial. To explore the application of the concept of rapid rehabilitation surgery and patient satisfaction with nursing care in the perioperative period of hip arthroplasty in the elderly. | The people in the control group received as peri-operative nursing care: orientation in preoperative exams and health education. After surgery, they were instructed to engage in early rehabilitation training according to their existing limitations to promote their recovery. | The results obtained showed that the recovery of hip function, surgery time, and hospital stay were significantly better in the experimental group than in the control group, as well as the satisfaction regarding nursing care. |
| [24] 242 patients divided into a control group (124) and an experimental group (118) | Randomised controlled study. To evaluate the effect of activity monitoring and text messaging on the rate of discharge to home and clinical outcomes in patients after hip or knee arthroplasty. | The control group received “usual care”. The intervention group received a physical activity monitor, daily pain tracking through text messages about post-surgery milestones and access to the doctor whenever needed. In this group, there was one branch that also received feedback with motivational messages, with goal setting and gamification. The remote monitoring and text messaging activities started at hospital discharge. | Results showed that activity monitoring and text messaging did not increase the rate of discharge home after hip and knee arthroplasty and that gamification and social support did not significantly increase physical activity. Remote monitoring demonstrated better care to people undergoing hip and knee arthroplasty by providing a direct mean of communication for the assessment of urgent problems, which translated into a significant reduction in the rate of readmissions. |
| [25] 144 people undergoing scheduled THA and TKA | A descriptive, retrospective, quantitative study. To analyse the gains in functional independence in patients submitted to a post-surgery motor rehabilitation programme. | The “Enable” project was created in the service, which aims to systematically promote the teaching, instruction, and training of patients who have undergone THA and TKA. In this project, the intervention of rehabilitation nursing began at home, with the correct identification of support devices, adaptive equipment, and people′s perception of their abilities. The identification of the characteristics of the home is important for the ADL training to be performed as close as possible to reality. | The results obtained in the assessment of the programme reveal an unequivocal recovery of functional independence after surgery. Thus, we can conclude that the implementation of the “Enable” project has allowed empowering the patients who underwent the post-surgery motor rehabilitation programme, THA, and TKA, as early as possible, with translation of the gains acquired in functional independence, and consequently facilitating their reintegration into society. |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Nicolau, C.; Mendes, L.; Ciríaco, M.; Ferreira, B.; Baixinho, C.L.; Fonseca, C.; Ferreira, R.; Sousa, L. Educational Intervention in Rehabilitation to Improve Functional Capacity after Hip Arthroplasty: A Scoping Review. J. Pers. Med. 2022, 12, 656. https://doi.org/10.3390/jpm12050656
Nicolau C, Mendes L, Ciríaco M, Ferreira B, Baixinho CL, Fonseca C, Ferreira R, Sousa L. Educational Intervention in Rehabilitation to Improve Functional Capacity after Hip Arthroplasty: A Scoping Review. Journal of Personalized Medicine. 2022; 12(5):656. https://doi.org/10.3390/jpm12050656
Chicago/Turabian StyleNicolau, Célia, Liliana Mendes, Mário Ciríaco, Bruno Ferreira, Cristina Lavareda Baixinho, César Fonseca, Rogério Ferreira, and Luís Sousa. 2022. "Educational Intervention in Rehabilitation to Improve Functional Capacity after Hip Arthroplasty: A Scoping Review" Journal of Personalized Medicine 12, no. 5: 656. https://doi.org/10.3390/jpm12050656
APA StyleNicolau, C., Mendes, L., Ciríaco, M., Ferreira, B., Baixinho, C. L., Fonseca, C., Ferreira, R., & Sousa, L. (2022). Educational Intervention in Rehabilitation to Improve Functional Capacity after Hip Arthroplasty: A Scoping Review. Journal of Personalized Medicine, 12(5), 656. https://doi.org/10.3390/jpm12050656









