A Holistic Approach for the Identification of Success Factors in Secondary Cleft Osteoplasty
Abstract
:1. Introduction
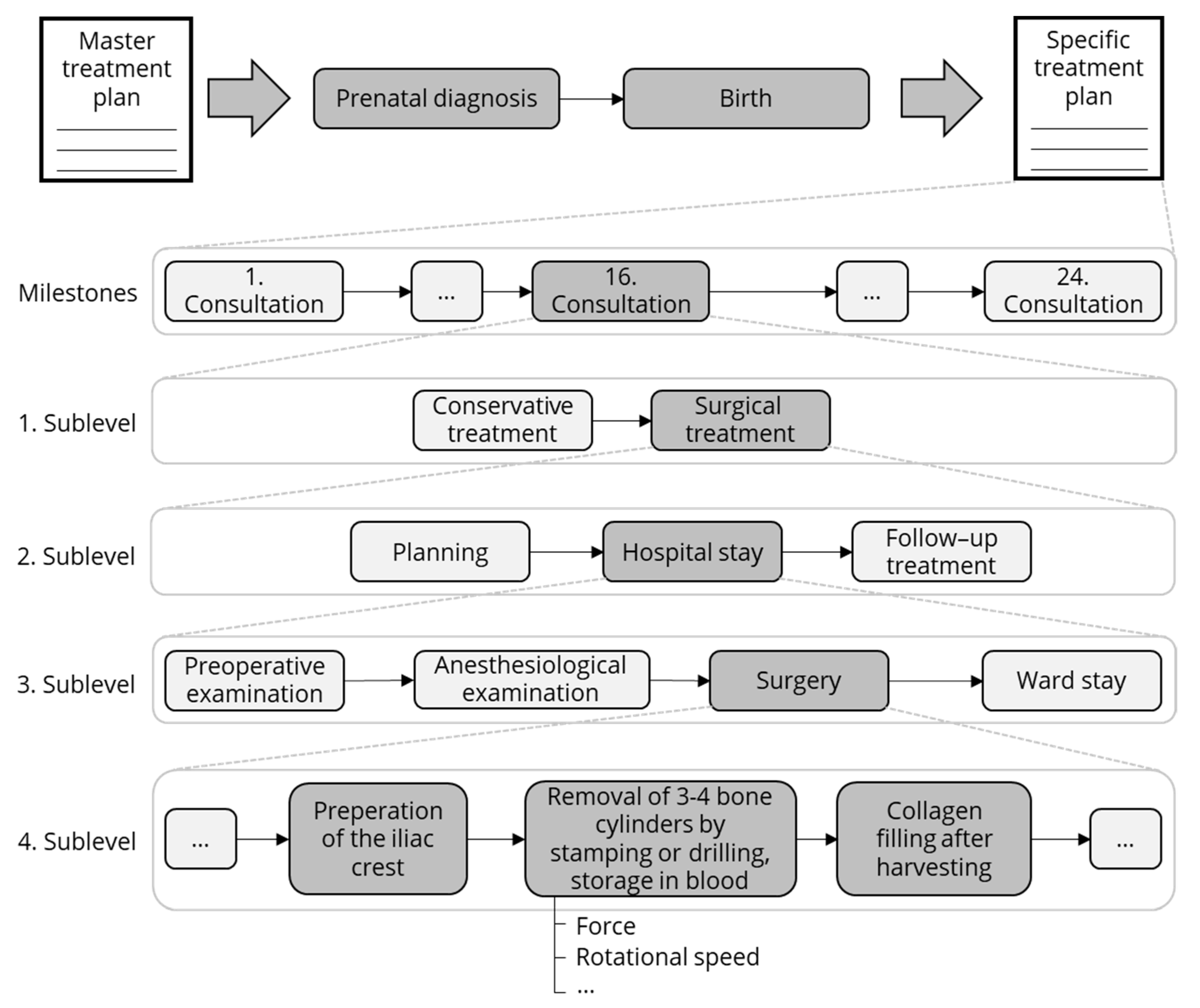
2. Materials and Methods
2.1. Analysis of Retrospective Data
- General procedures, which are performed regardless of the cleft type;
- Procedures that are performed to treat the cleft lip;
- Procedures that are specific to the cleft palate;
- Procedures that are specific to the alveolar cleft.
2.2. Analysis and Definition of Process Parameters for Quantitative Measurement
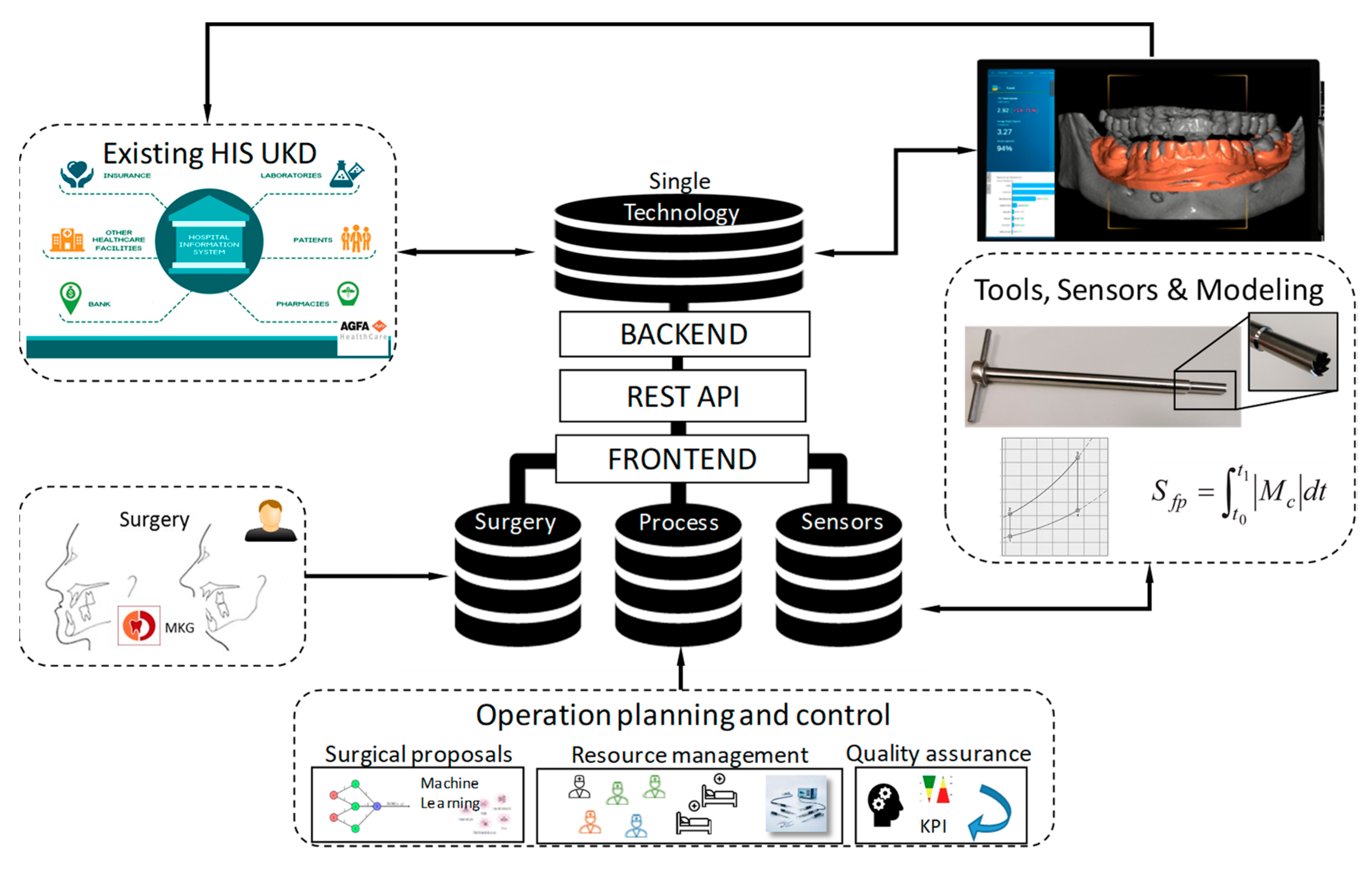
2.3. Method to Integrate Data from Different Sources
- A physician familiar with clinical data management (Faculty of Health Sciences);
- A research scientist assigned as the DTS administrator (Faculty of Health Sciences);
- A computer scientist with experience in production, for software and server support (Information Engineering).
3. Results
3.1. Analysis Medical Data
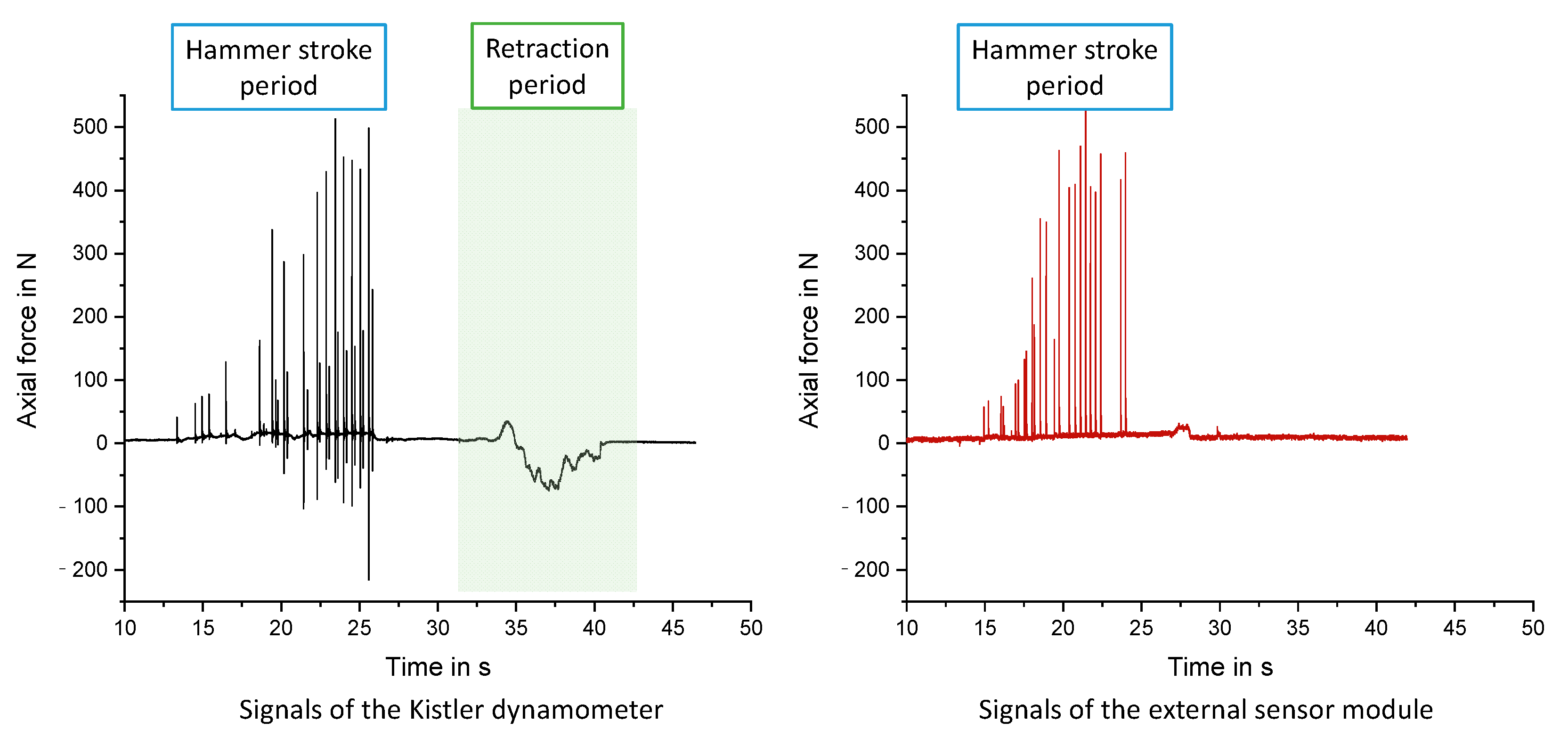
3.2. Sensory Concept for In Vitro Experiments
3.3. Specification of Dental Tech Space Software
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Dixon, M.J.; Marazita, M.L.; Beaty, T.H.; Murray, J.C. Cleft lip and palate: Understanding genetic and environmental influences. Nat. Rev. Genet. 2011, 12, 167–178. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Seifeldin, S.A. Is alveolar cleft reconstruction still controversial? (Review of literature). Saudi Dent. J. 2016, 28, 3–11. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Santiago, P.E.; Schuster, L.A.; Levy-Bercowski, D. Management of the Alveolar Cleft. Clin. Plast. Surg. 2014, 41, 219–232. [Google Scholar] [CrossRef] [PubMed]
- Shetye, P.R. Update on treatment of patients with cleft—Timing of orthodontics and surgery. Semin. Orthod. 2016, 22, 45–51. [Google Scholar] [CrossRef]
- Goodacre, T.; Swan, M.C. Cleft lip and palate: Current management. Paediatr. Child Health 2012, 22, 160–168. [Google Scholar] [CrossRef]
- Myeroff, C.; Archdeacon, M. Autogenous bone graft: Donor sites and techniques. J. Bone Jt. Surg. Am. 2011, 93, 2227–2236. [Google Scholar] [CrossRef] [PubMed]
- Kamal, M.; Ziyab, A.H.; Bartella, A.; Mitchell, D.; Al-Asfour, A.; Hölzle, F.; Kessler, P.; Lethaus, B. Volumetric comparison of autogenous bone and tissue-engineered bone replacement materials in alveolar cleft repair: A systematic review and meta-analysis. Br. J. Oral Maxillofac. Surg. 2018, 56, 453–462. [Google Scholar] [CrossRef] [PubMed]
- Schönmeyr, B.; Wendby, L.; Campbell, A. Early Surgical Complications after Primary Cleft Lip Repair: A Report of 3108 Consecutive Cases. Cleft Palate-Craniofacial J. 2015, 52, 706–710. [Google Scholar] [CrossRef] [PubMed]
- Terheyden, H.; Müller, A.; Dunsche, A.; Härle, F. Comparison of secondary and tertiary cleft jaw osteoplasty. 20 year analysis. Mund. Kiefer. Gesichtschir. 2002, 6, 134–139. [Google Scholar] [CrossRef] [PubMed]
- Nagy, K.; Mommaerts, M.Y. Postoperative Wound Management after Cleft Lip Surgery. Cleft Palate-Craniofacial J. 2011, 48, 584–586. [Google Scholar] [CrossRef] [PubMed]
- Subramanyam, D. An insight of the cleft lip and palate in pediatric dentistry—A Review. J. Dent. Oral. Biol. 2020, 5, 1164. [Google Scholar]
- de Ladeira, P.R.S.; Alonso, N. Protocols in cleft lip and palate treatment: Systematic review. Plast. Surg. Int. 2012, 2012, 562892. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Teicher, U.; Ben Achour, A.; Nestler, A.; Brosius, A.; Lauer, G. Process based analysis of manually controlled drilling processes for bone. AIP Conf. Proc. 2018, 070025, 1960. [Google Scholar] [CrossRef]
- Kozak, K.; Seidel, A.; Matvieieva, N.; Neupetsch, C.; Teicher, U.; Lemme, G.; Achour, A.B.; Barth, M.; Ihlenfeldt, S.; Drossel, W.G. Unique Device Identification Based Linkage of Hierarchically Accessible Data Domains in Prospective Hospital Data Ecosystems. arXiv 2022, arXiv:2202.13215. [Google Scholar]
- Pradel, W.; Lauer, G. Tissue-engineered bone grafts for osteoplasty in patients with cleft alveolus. Ann. Anat.-Anat. Anz. 2012, 194, 545–548. [Google Scholar] [CrossRef] [PubMed]
- Shaye, D.; Liu, C.C.; Tollefson, T.T. Cleft Lip and Palate. Facial Plast. Surg. Clin. N. Am. 2015, 23, 357–372. [Google Scholar] [CrossRef] [PubMed]
- Kalaaji, A.; Lilja, J.; Friede, H.; Elander, A. Bone grafting in the mixed and permanent dentition in cleft lip and palate patients: Long-term results and the role of the surgeon’s experience. J. Cranio-Maxillofac. Surg. 1996, 24, 29–35. [Google Scholar] [CrossRef]
- Klijn, R.J.; Meijer, G.J.; Bronkhorst, E.M.; Jansen, J.A. Sinus Floor Augmentation Surgery Using Autologous Bone Grafts from Various Donor Sites: A Meta-Analysis of the Total Bone Volume. Tissue Eng. Part B Rev. 2010, 16, 295–303. [Google Scholar] [CrossRef] [PubMed]
- Tai, C.-C.E.; Sutherland, I.S.; McFadden, L. Prospective analysis of secondary alveolar bone grafting using computed tomography. J. Oral Maxillofac. Surg. 2000, 58, 1241–1249. [Google Scholar] [CrossRef] [PubMed]
- Feichtinger, M.; Mossböck, R.; Kärcher, H. Assessment of Bone Resorption after Secondary Alveolar Bone Grafting Using Three-Dimensional Computed Tomography: A Three-Year Study. Cleft Palate-Craniofacial J. 2007, 44, 142–148. [Google Scholar] [CrossRef] [PubMed]
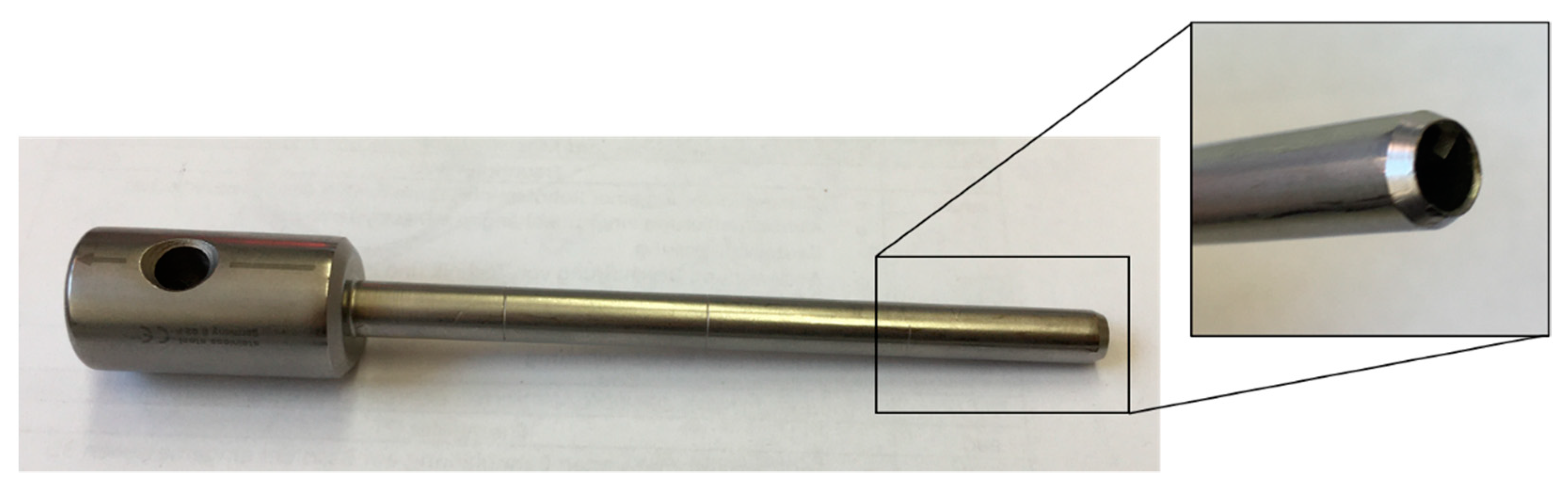
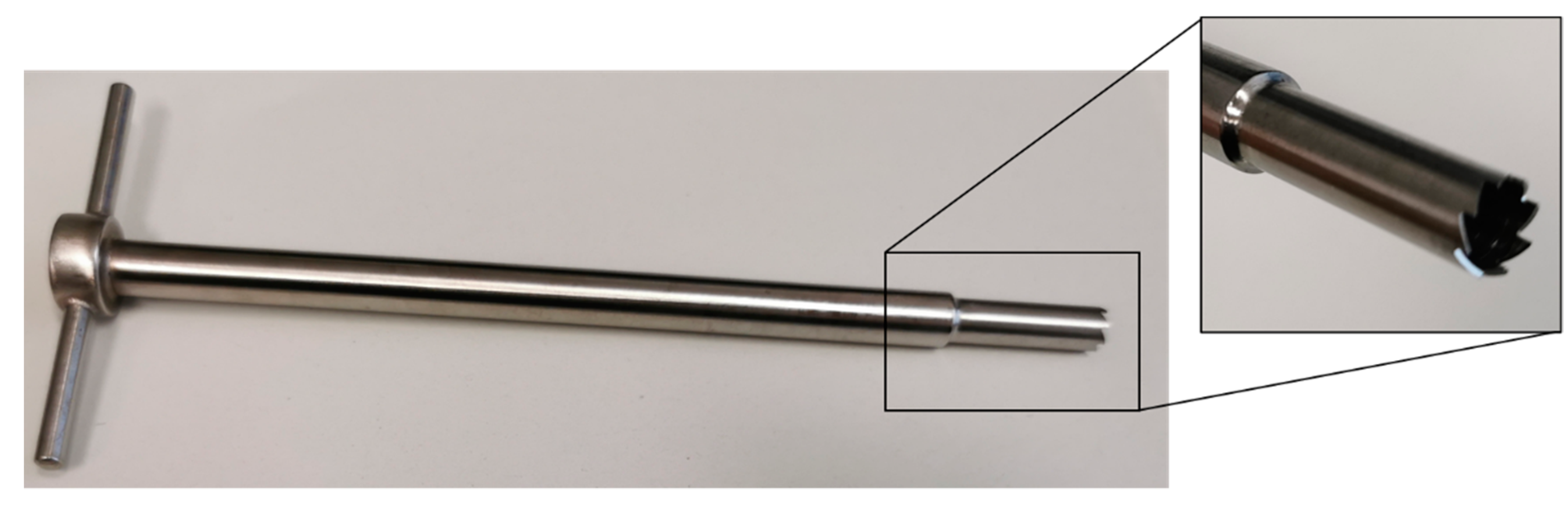
| Criteria | Shepard Chisel (Figure 1) | Trephine Hand Drill (Figure 2) |
|---|---|---|
| Material separation process | stamping | machining–core drill |
| Feed movement | linear | helical (linear feed + rotary cutting movement) |
| Type of feed | impact (manual) | quasi-continuous (manual) |
| Auxiliary tool | hammer | - |
| Hole type | blind hole | blind or through hole |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Schröder, T.A.; Maiwald, M.; Reinicke, A.; Teicher, U.; Seidel, A.; Schmidt, T.; Ihlenfeldt, S.; Kozak, K.; Pradel, W.; Lauer, G.; et al. A Holistic Approach for the Identification of Success Factors in Secondary Cleft Osteoplasty. J. Pers. Med. 2022, 12, 506. https://doi.org/10.3390/jpm12030506
Schröder TA, Maiwald M, Reinicke A, Teicher U, Seidel A, Schmidt T, Ihlenfeldt S, Kozak K, Pradel W, Lauer G, et al. A Holistic Approach for the Identification of Success Factors in Secondary Cleft Osteoplasty. Journal of Personalized Medicine. 2022; 12(3):506. https://doi.org/10.3390/jpm12030506
Chicago/Turabian StyleSchröder, Tom A., Martin Maiwald, Axel Reinicke, Uwe Teicher, André Seidel, Thorsten Schmidt, Steffen Ihlenfeldt, Karol Kozak, Winnie Pradel, Günter Lauer, and et al. 2022. "A Holistic Approach for the Identification of Success Factors in Secondary Cleft Osteoplasty" Journal of Personalized Medicine 12, no. 3: 506. https://doi.org/10.3390/jpm12030506
APA StyleSchröder, T. A., Maiwald, M., Reinicke, A., Teicher, U., Seidel, A., Schmidt, T., Ihlenfeldt, S., Kozak, K., Pradel, W., Lauer, G., & Ben Achour, A. (2022). A Holistic Approach for the Identification of Success Factors in Secondary Cleft Osteoplasty. Journal of Personalized Medicine, 12(3), 506. https://doi.org/10.3390/jpm12030506






