Abstract
Non-sustained ventricular tachycardia (nsVT) creates the electrical basis for sudden cardiac death (SCD) in hypertrophic cardiomyopathy (HCM). We aimed to evaluate the relationship between interstitial fibrosis on cardiac magnetic resonance (CMR) and nsVT in HCM. A total of 50 HCM patients underwent CMR with a 3 T scanner to determine the presence of replacement fibrosis expressed by late gadolinium enhancement (LGE), and interstitial fibrosis expressed by native T₁, post-contrast T₁, and extracellular volume (ECV). The incidence of nsVT was assessed by Holter monitoring. We detected nsVT in 14 (28%) out of 50 HCM patients. Replacement fibrosis expressed by LGE was present in 37 (74%) patients and only showed a trend towards a differentiation between the groups with and without nsVT (p = 0.07). However, the extent of LGE was clearly higher in the nsVT group (3.8 ± 4.9% vs. 7.94 ± 4.5%, p = 0.002) and was an independent predictor of nsVT in a multivariable regression analysis (OR 1.2; 95%CI 1.02–1.4; p = 0.02). No relationship was observed between interstitial fibrosis and nsVT. To conclude, it was found that it is not the mere presence but the actual extent of LGE that determines the occurrence of nsVT in HCM patients; the role of interstitial fibrosis remains unclear.
1. Introduction
Hypertrophic cardiomyopathy (HCM) is a common genetic myocardial disease with a prevalence of approximately 1:500, caused by mutations in sarcomeric genes [1,2,3]. Macroscopically, HCM is characterized by a non-dilated left ventricle (LV), various degrees of LV hypertrophy (LVH), and normal systolic function. At the cellular level, the typical features of HCM include areas of hypertrophied and disorganized (disarray) cardiac myocytes and widespread areas of fibrosis [4]. Most patients with HCM are minimally symptomatic [4,5]. However, approximately one-fifth of patients develop moderate-to-severe symptoms of chest pain, early fatigue, palpitations, syncope, etc., that result in five major pathologies: diastolic dysfunction (DD), LV outflow tract obstruction (LVOTO), an imbalance between the myocardial oxygen supply and demand, end-stage heart failure (HF), and arrhythmias, including atrial fibrillation and non-sustained ventricular tachycardia (nsVT) that may lead to sudden cardiac death (SCD) [6,7,8].
Cardiac fibrosis is common in HCM and is particularly responsible for DD, arrhythmias, and end-stage HF. Two types of cardiac fibrosis of differing pathologies and biological roles exist: namely local (replacement, scarring) and diffuse (interstitial, reactive) fibrosis [5]. Replacement fibrosis develops as a consequence of the death of local myocytes (necrosis, apoptosis), whereas interstitial fibrosis is caused by systemic processes, such as hypertension, inflammation, or genetic mutations. Both local and diffuse fibrosis coexist in HCM, as well as in many other cardiomyopathies.
Cardiac fibrosis can be diagnosed either invasively, by means of an endomyocardial biopsy, or by imaging methods. Among non-invasive methods, cardiac magnetic resonance (CMR) is considered the most optimal and is a validated tool for fibrosis assessment. After the administration of a gadolinium-based contrast agent, late gadolinium enhancement (LGE) imaging makes the identification of areas of local fibrosis possible. Currently, it is widely accepted that the quantification of the LGE area is the most preferred method as it allows for longitudinal measurements rather than a mere binary classification (e.g., LGE present or absent). Since the introduction of T1 parametric mapping, interstitial fibrosis can be evaluated [9]. Among all the T1-parametric indices, extracellular volume (ECV) is the one best suited to measure and quantify interstitial collagen expansion (fibrosis). In brief, ECV is measured by combining native and contrast-enhanced T1 maps of blood and myocardium and is typically expressed as a percentage (%).
To date, numerous studies have shown that the presence and size of LGE (i.e., replacement fibrosis) may be related to ventricular arrhythmia and SCD [10,11,12]. On the other hand, an association between ventricular arrhythmia (i.e., nsVT) with interstitial fibrosis (i.e., as assessed with T1 mapping) is far less studied. Given the fact that interstitial fibrosis is a common and potentially clinically relevant finding, its eventual role in arrhythmic risk stratification should be thoroughly investigated. Thus, the principal aim of the study was to evaluate the relationship between interstitial fibrosis, expressed as ECV, and nsVT in HCM patients.
2. Materials and Methods
2.1. Study Population
In this prospective, single-center, observational study, a total of 50 patients with a diagnosis of HCM was included. HCM was diagnosed on the basis of the current guidelines of the European Society of Cardiology (ESC) [13], defined as: ≥15 mm thickness of one or more of the LV wall segments which cannot be accounted for by the common causes of increased afterload (hypertension or aortic stenosis) or, in the case of first-degree relatives of HCM patients, as a thickness of LV ≥ 13 mm. We did not include patients with previously implanted cardiac devices, severely reduced kidney function (GFR < 30 mL/min), or infiltrative disease. Patients underwent diagnostic procedures, including laboratory tests, echocardiography, a six-minute walk test, electrocardiographic (ECG) Holter monitoring, and CMR. Echocardiographic examinations were performed on commercially available devices in accordance with the current European and American guidelines [14]. All of the patients gave their informed consent. The study was conducted in accordance with the Declaration of Helsinki, and prior to the study, the protocol was approved by the Jagiellonian University Ethical Committee.
2.2. Cardiac Magnetic Resonance
CMR exams were performed on a 3.0-T scanner (Magnetom Skyra, Siemens, Erlangen, Germany) at the time of inclusion. The analysis of the CMR studies was based on the guidelines of the Society of Cardiovascular Magnetic Resonance [15] and the Syngo. VIA software version VB 40 (Siemens, Erlangen, Germany) was used to conduct this analysis. Three long-axis (2-, 3-, and 4-chamber) slices and short-axis slices covering the LV were used to obtain steady-state free precession cine images. The CMR protocol consisted of cine CMR, native and post-contrast T1 mapping, and LGE imaging.
2.2.1. Assessment of Replacement Fibrosis
Approximately 15 min after the intravenous administration of 0.1 mmol/kg of body weight of gadolinium-based contrast agent, the short-axis LGE images were acquired sequentially. The presence of LGE in both the short axis and adequate perpendicular images indicated the presence of fibrosis. A threshold of 5 standard deviations in subsequent short-axis slices was used to assess the quantitative extent of LGE, and its value was stated as a percentage of the total LV mass [15].
2.2.2. Assessment of Interstitial Fibrosis
T1 mapping was performed using (Siemens Skyra VE11 with MyoMaps) a Modified Look Locker Inversion (MOLLI) Recovery sequence before, and 15 min after, a gadolinium-based contrast agent injection. The following parameters of this sequence were used: breath-hold TR/TE of 281/1.1 ms, slice thickness of 8 mm, matrix of 144 × 256 pixels, FOV from 320 × 260 mm2, and a flip angle of 35°. Drawing regions of interest (ROI) in the mid-wall regions of each myocardial segment according to the AHA 16-segment model determined the native and post-contrast T1 values. To measure T1 blood pools, drawings from the center of the LV cavity were used. ROIs were copied between the pre- and post-contrast T1 maps. Artifact segments were not included. The means of all segments native and post-contrast T1 times was the global value. The ECV was computed by the following formula [15]: ECV = ((1/(post-contrast T1) − 1/(native T1))/(1/(blood post-contrast T1)) − 1/(blood native T1))*(1 − Hct).
2.3. Electrocardiographic Examinations
During the index visit, patients also underwent 48 h ECG Holter monitoring (Spacelabs Healthcare, Reynolds Medical, Lifecard CF, Snoqualmie, DC, USA). The analysis was conducted by two experienced technicians and supervised by a cardiologist. Ventricular tachycardia (VT) was defined as three or more consecutive ventricular beats at a rate greater than 100 beats/min [16]. All recorded VTs were non-sustained, which was defined as having a duration of less than 30 s.
2.4. Statistical Analysis
Results are presented as percentages (counts) or mean ± standard deviations. The normal distribution of quantitative variables was assessed using the Shapiro–Wilk test. Qualitative variables were compared with the chi-squared test, and quantitative ones with the t-Student or U-Mann–Whitney test according to the analysis of the normal distribution. All parameters differentiating patients with and without nsVT with p-values < 0.05 (Table 1 and Table 2) were included in the regression analyses. For two closely related variables, one was used in the regression model. Uni- and multivariable logistic regression models analyzed the associations between the analyzed parameters and the presence of nsVT. When the p-value was <0.05, the results were considered statistically significant. The statistical analysis was conducted with the Statistica package, version 13.0 (StatSoft, TIBCO Software Inc., Palo Alto, CA, USA).

Table 1.
Baseline characteristics. Comparison of HCM patients with and without nsVT.

Table 2.
Comparison of CMR findings between HCM patients with and without nsVT.
3. Results
3.1. Baseline Characteristics
Based on 48 h Holter data, patients were classified into those with (n = 14; 28%) and without nsVT (n = 36; 72%). Patients with nsVT had a significantly higher value of body mass index, experienced dyslipidemia more often, and had a higher estimated 5-year risk of SCD, a larger left atrium (LA) diameter and LA volume index, and a higher E/e’ ratio. We did not observe differences in the levels of NT-proBNP and high-sensitive troponin T. Moreover, the patients did not differ from each other in terms of the applied pharmacotherapy (Table 1).
3.2. nsVT and CMR Data
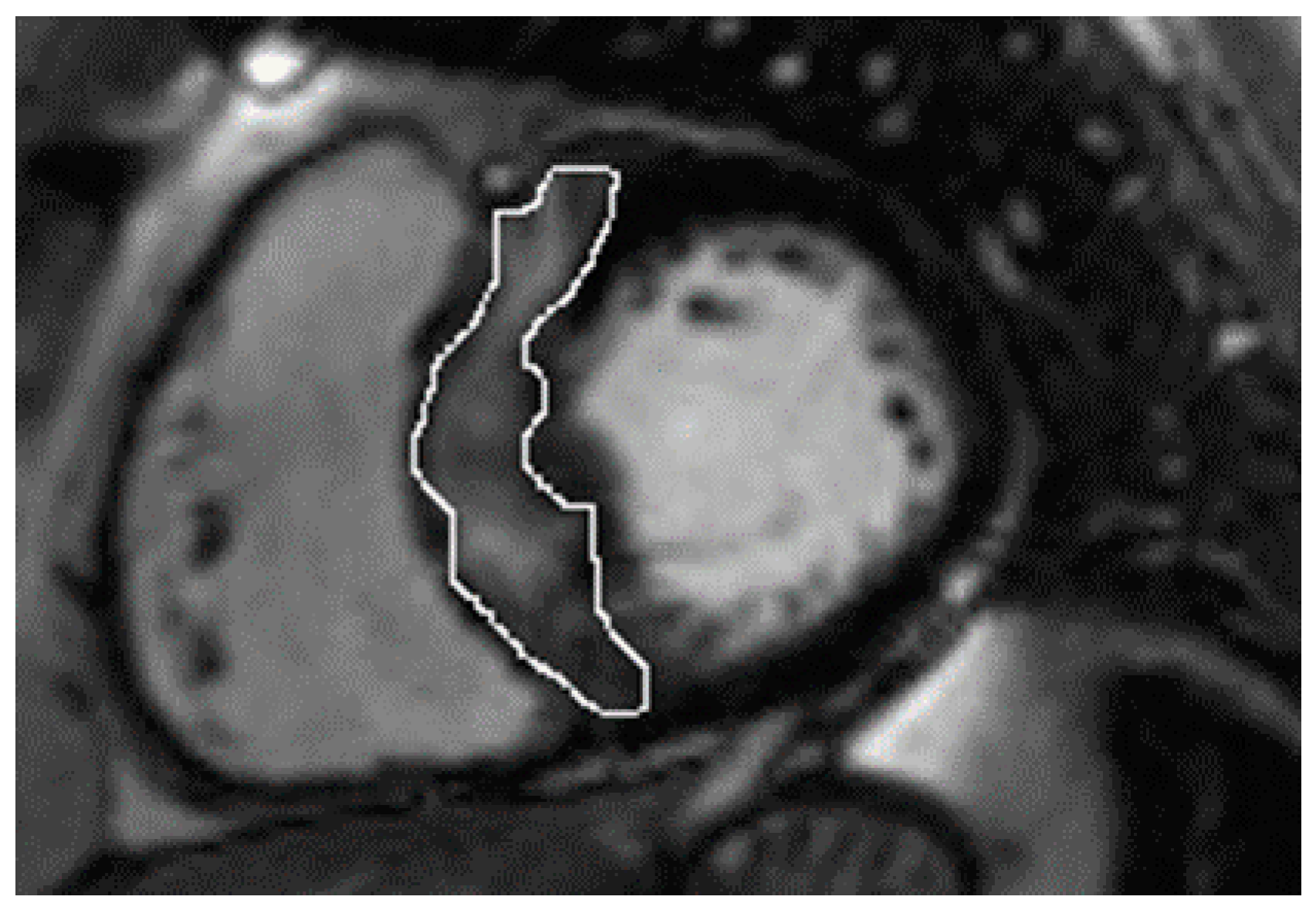
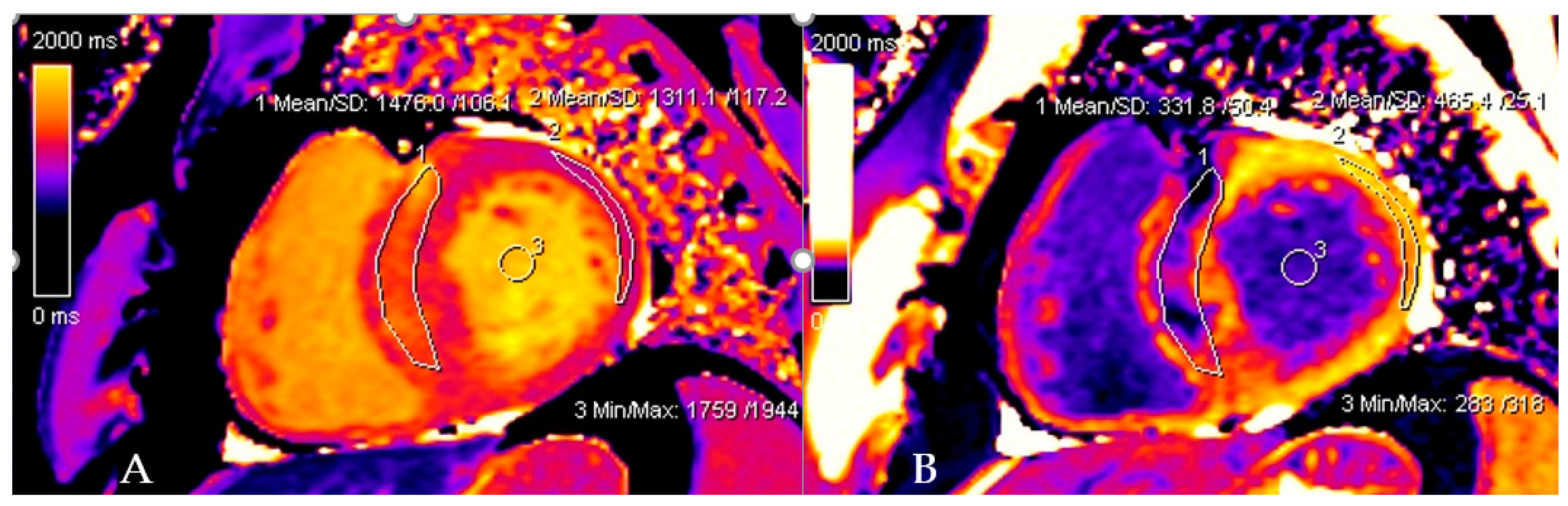
In the whole group, LGE was present in 37 (74%) patients. Patients with nsVT had a larger extent with respect to LGE (Table 2). However, the patients did not differ in native and post-contrast T1 times and ECV values, and the mere presence of LGE only showed a trend towards significance. Figure 1 and Figure 2 present examples of images obtained in the CMR studies.
Figure 1.
Late gadolinium enhancement (LGE) images show the quantification of the septal burden of replacement fibrosis (circled) via the technique which uses a 5-standard-deviations threshold on consecutive short-axis slices.
Figure 2.
Native and post-contrast contours in the mid-myocardial area. The left ventricular cavity is shown (orange in native T1 mapping and dark blue in post-contrast T1 mapping) to enable the derivation of blood and myocardial T1 values. Standardized ROIs are placed in the septum to measure native (A) and post-contrast T1 times (B).
3.3. Predictor Factors for nsVT
Among all the parameters differentiating patients with and without nsVT, univariable regression analysis presented a significant association between nsVT and LA diameter, and E/e’ and LGE extent (Table 3). However, in the multivariable regression model, only LA diameter and LGE extent were independently associated with nsVT (Table 3).

Table 3.
Uni- and multivariable regression models for nsVT presence.
4. Discussion
The study findings can be summarized as follows: an independent association was found between replacement fibrosis (expressed as LGE extent and LA diameter) with nsVT. On the other hand, parameters that quantify interstitial fibrosis, such as native and post-contrast T1 times and ECV, were not found to be related to ventricular arrhythmias.
4.1. nsVT Predictors
4.1.1. Replacement Fibrosis
Previous CMR studies have revealed the presence of LGE in approximately 70% of HCM patients [17,18], including those who are oligo- and asymptomatic [19]. In our group, LGE was present in 74% of patients, which is in line with previous observations. However, in some reports, the presence of LGE has ranged from 41% [20] to 90% [21]. Demonstrating the presence of LGE in the majority of patients with HCM, including the asymptomatic ones, sparked numerous studies investigating its relationship with prognoses and risk stratification. For the same reason, the quantitative analysis of LGE extent and its predictive value has also been investigated. While the evaluation of the presence of LGE is relatively simple, quantitative assessment is more complex, requires appropriate software, and is not standardized [22]. Although the bulk of studies have demonstrated a relationship between LGE and SCD risk, there are also reports that question these associations. Chan et al. in a study involving 1293 patients, demonstrated a significant relationship between LGE extent and the risk of SCD events [23], which was also confirmed in the meta-analysis by Weng et al., which included seven studies and 2993 patients [24]. Moreover, Weissler-Snir et al. showed a relationship between LGE extent and nsVT in HCM patients [25]. By way of contrast, Briasoulis et al., in his meta-analysis of six studies, showed that while there is a significant relationship between the mere presence of LGE and an increased risk of SCD in non-high-risk patients, the LGE extent was not significantly related to the risk of SCD [26]. Beyond this, Maron et al. showed no relationship at all between LGE and adverse cardiovascular events (SCD, appropriate implantable cardioverter-defibrillator discharge, and progressive HF symptoms) [27]; and Green et al., in his meta-analysis, only showed a trend towards significance in predicting SCD [28]. Although there are studies that have shown a significant relationship between the LGE extent and the arrhythmic endpoint in univariable analysis, this relationship was not confirmed in their multivariable analysis [29,30].
Importantly, we demonstrated an association between LGE extent and nsVT, evaluated at the same time (as CMR and Holter were performed almost simultaneously—within 1–2 days), which is dissimilar to most studies that have analyzed CMR and Holter at various time points, including several months apart or at unknown time intervals [31,32,33]. This may have some important implications. Given that the patients were in the same condition and being treated with stable therapies, it is probable that, as the clinical status changes (e.g., there is an exacerbation of the disease or medication is not taken), the arrhythmic risk is also probably changing. Despite the fact that this subject is poorly investigated, there is a likelihood that the amount of replacement fibrosis (i.e., LGE extent) is not a static pathology but varies over time. According to our observations, it was not merely the presence of LGE but its extent that was found to have diagnostic value for nsVT risk stratification. This is a finding that is consistent with a number of other studies [31,32].
Regarding the use of the LGE value as a factor in SCD risk stratification, there is a discrepancy between the American and European approaches [13,22]. The older European HCM risk score model takes into account the following parameters: age, maximum LV wall thickness, LA dimension, maximum LVOT gradient, the presence of nsVT, a family history of SCD, and unexplained syncope. Crucially, it fails to take into account the presence or extent of LGE. On the other hand, on the basis of several papers from Chan et al., Weng et, al., and Mentias et al. [23,24,34], the American College of Cardiology and American Heart Association Joint Committee issued a recommendation that extensive LGE be taken into consideration as a risk factor for potentially life-threatening ventricular arrhythmias [22]. Chan et al., as well as proving that the risk of SCD increased substantially with LGE levels at ≥15% of the LV mass, emphasized the linear relation between the %LGE and SCD event risk. Moreover, Chan et al. did not observe a significant increase in SCD in HCM patients with minimal LGE (1–5%) compared with those with no LGE [23]. In the work of Mentias et al., the study risk of primary events, consisting of SCD and appropriate implantable cardioverter-defibrillator (ICD) discharge, increased when %LGE was ≥15% [34]. In our study, we report lower values of LGE extent, as it was almost 8% in the nsVT-positive group in comparison to 3.8% in the nsVT-negative group; the difference is statistically sound and clearly indicates that more fibrotic LV is more prone to ventricular arrhythmias. A lack of consensus on the optimal quantitative method may be a source of variance in the results, as cited in the American guidelines [22].
4.1.2. Left Atrium and nsVT
In many HCM patients, an enlarged left atrium is observed, which may be due to, among other causes, mitral regurgitation or DD [13]. Its size provides a lot of prognostic information [35,36] and is an independent risk factor for SCD included in the HCM risk score model [13,35]. In our observations, the enlarged size of the LA was an independent predictor of nsVT, a finding which is consistent with a previous study [25].
4.1.3. Interstitial Fibrosis
Until recently, it was impossible to visualize and diagnose interstitial fibrosis, as conventional CMR only allows for the assessment of large areas of replacement fibrosis. Thanks to T1 parametric mapping, interstitial fibrosis can now be accurately assessed. As these two types of fibrosis have different pathologies, they most likely also have different clinical meanings, but this is an issue that is the subject of ongoing research.
As T1 mapping is a relatively new technology, only five studies analyzing the role of T1 times and ECV in the context of ventricular arrhythmia in HCM have been published so far. At present, the general picture emerging from these studies is unclear. Among these five studies, three reported some degree of association with ventricular arrhythmia. Levine et al. observed a significant two-fold increased prevalence of nsVT in patients with mean ECV above the study population mean of 27% compared with those with mean ECV < 27% [33]. The HCM group with nsVT or syncope in the study of Avanesov et al. had significantly higher global ECV than patients without nsVT or syncope, and the authors found that a cut-off value of ≥34% for global ECV resulted in a sensitivity of 88% and a specificity of 77% in the prediction of an increased SCD risk in HCM [32]. McLellan et al. showed that post-contrast ventricular T1 relaxation time was significantly reduced in patients with nsVT and patients with aborted SCD, and the quantity rather than the presence of LGE was associated with nsVT and aborted SCD [31].
Adding to the lack of clarity on the matter, the comparison of the ECV values between patients with and without nsVT by Chung et al. showed no statistically significant differences [37]. Furthermore, Mirelis et al. showed that ECV was not increased in ICD-implanted HCM patients with malignant ventricular arrhythmias vs. those without arrhythmias; however, in this study, the ECV was assessed by computed tomography [38]. In our group, the average ECV was approximately 28%, which is a figure that is slightly lower than that reported by Levine and Avanessov; nevertheless, septal ECV values were higher, reaching 30.5% in patients with documented nsVT. We observed no difference between native and post-contrast T1 times between patients with and without nsVT. As for ECV, which is a complex measure, involving myocardial and blood T1 times as well as hematocrit, there was no difference in terms of global ECV between patients with and without nsVT; still, it is worth noting that there was a numerical trend towards higher septal ECV values in nsVT patients compared to those without nsVT (30.5 ± 7.2 vs. 27.7 ± 5.6; p = 0.099). As fibrosis in HCM is most commonly present in the mid-septum, it may be that increased septal ECV is related to some level of arrhythmic risk.
The question of the relationship between ECV and nsVT remains unanswered, and our observations have not proved the value of ECV as a potential prognostic factor. In our opinion, the assessment of the relationship between ECV and ventricular arrhythmias and SCD requires multicenter studies with diverse populations and a standardized methodology.
An interpretation of the study results is offered here: LGE areas are large, disrupting myocyte organization, and exacerbating disarray. Large areas of scar tissue slow down the conduction-forming electro-micro circle loops. In contrast to replacement fibrosis, interstitial fibrosis is not induced by cell death and is a gradual process that can be reversed if the cause is treated promptly [39]. We can hypothesize that the gap junctions in diffuse fibrosis are not so far apart from each other, and therefore do not affect electrical impulse conduction to the same extent as is the case in irreversible replacement fibrosis.
4.2. Study Limitations
Our group was relatively small, especially after the division used. Therefore, the results should be interpreted with caution. Due to the small size of the subgroups, no analyses were performed, with the exception of drugs modifying the course of the fibrosis process. We only analyzed the effect of fibrosis on the Holter index and did not conduct a follow-up with extended duration. Larger multicenter studies with a long follow-up could provide valuable data.
5. Conclusions
In a contemporary cohort of HCM patients, an independent association was observed between a quantitative measure of replacement fibrosis—both LGE extent and nsVT. Conversely, T1 mapping derived measures of interstitial fibrosis; native and post-contrast T1 times and ECV were not related to nsVT. This study provides one further argument for the incorporation of LGE extent into a comprehensive SCD prognostic model. Moreover, further studies are needed to verify the role of interstitial fibrosis indices in SCD risk stratification in HCM, which currently remains undefined.
Author Contributions
Conceptualization P.R. and A.K.-M.; Methodology P.R., A.K.-M., P.B. and M.U.-Z.; Formal Analysis A.K.-M. and E.D.; Investigation A.K.-M., P.R., E.D., S.W.-Ś. and P.P.; Resources P.B., M.U.-Z., M.M., M.K. (Maciej Krupiński) and J.Ł.; Data Curation A.B., Ł.Ż. and M.K. (Magdalena Kostkiewicz); Writing—Original Draft Preparation A.K.-M.; Writing—Review and Editing P.R.; Supervision P.R.; Project Administration A.K.-M., E.D., S.W.-Ś., K.H. and P.P.; Funding Acquisition P.R. and A.K.-M. All authors have read and agreed to the published version of the manuscript.
Funding
This work was funded through the Department of Scientific Research and Structural Funds of Medical College, Jagiellonian University (grant number N41/DBS/000308; grant number N41/DBS/000595). The authors report no involvement in the research by the sponsor that could have influenced the outcome of this work.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki, and the protocol was approved by the Jagiellonian University Ethical Committee—the protocol number is 1072.6120.237.2019; date of approval: 24 October 2019.
Informed Consent Statement
All subjects gave their informed consent for inclusion before they participated in the study.
Data Availability Statement
The data presented in this study are available on request from the corresponding author. The data are not publicly available due to their clinical nature.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Semsarian, C.; Ingles, J.; Maron, M.S.; Maron, B.J. New Perspectives on the Prevalence of Hypertrophic Cardiomyopathy. J. Am. Coll. Cardiol. 2015, 65, 1249–1254. [Google Scholar] [CrossRef] [Green Version]
- Dorobantu, L.; Ticulescu, R.; Greavu, M.; Dermengiu, A.; Alexandrescu, M.; Trofin, M. Current Management and Surgical Advances in Patients with Hypertrophic Obstructive Cardiomyopathy. Kardiol. Pol. 2019, 77, 829–836. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zschirnt, M.; Thul, J.; Akintürk, H.; Valeske, K.; Schranz, D.; Skrzypek, S.; Müller, M.; Jux, C.; Hahn, A.; Rupp, S. Aetiology and 30-Year Long-Term Outcome of Children with Cardiomyopathy Necessitating Heart Transplantation. J. Pers. Med. 2020, 10, 251. [Google Scholar] [CrossRef] [PubMed]
- Marian, A.J.; Braunwald, E. Hypertrophic Cardiomyopathy: Genetics, Pathogenesis, Clinical Manifestations, Diagnosis, and Therapy. Circ. Res. 2017, 121, 749–770. [Google Scholar] [CrossRef] [PubMed]
- Maron, B.J. Clinical Course and Management of Hypertrophic Cardiomyopathy. N. Engl. J. Med. 2018, 379, 655–668. [Google Scholar] [CrossRef]
- Maron, B.J.; Rowin, E.J.; Casey, S.A.; Maron, M.S. How Hypertrophic Cardiomyopathy Became a Contemporary Treatable Genetic Disease with Low Mortality: Shaped by 50 Years of Clinical Research and Practice. JAMA Cardiol. 2016, 1, 98–105. [Google Scholar] [CrossRef] [Green Version]
- Maron, B.J.; Maron, M.S. Hypertrophic Cardiomyopathy. Lancet 2013, 381, 242–255. [Google Scholar] [CrossRef]
- Geske, J.B.; Ommen, S.R.; Gersh, B.J. Hypertrophic Cardiomyopathy: Clinical Update. JACC Heart Fail. 2018, 6, 364–375. [Google Scholar] [CrossRef]
- Taylor, A.J.; Salerno, M.; Dharmakumar, R.; Jerosch-Herold, M. T1 Mapping Basic Techniques and Clinical Applications. JACC Cardiovasc. Imaging 2016, 9, 67–81. [Google Scholar] [CrossRef] [Green Version]
- Bacmeister, L.; Schwarzl, M.; Warnke, S.; Stoffers, B.; Blankenberg, S.; Westermann, D.; Lindner, D. Inflammation and Fibrosis in Murine Models of Heart Failure; Springer: Berlin/Heidelberg, Germany, 2019; Volume 114. [Google Scholar] [CrossRef]
- Rai, V.; Sharma, P.; Agrawal, S.; Agrawal, D.K. Relevance of Mouse Models of Cardiac Fibrosis and Hypertrophy in Cardiac Research. Mol. Cell. Biochem. 2017, 424, 123–145. [Google Scholar] [CrossRef]
- Cooper, L.T.; Baughman, K.L.; Feldman, A.M.; Frustaci, A.; Jessup, M.; Kuhl, U.; Levine, G.N.; Narula, J.; Starling, R.C.; Towbin, J.; et al. The Role of Endomyocardial Biopsy in the Management of Cardiovascular Disease: A Scientific Statement from the American Heart Association, the American College of Cardiology, and the European Society of Cardiology Endorsed by the Heart Failure Society of America and the Heart Failure Association of the European Society of Cardiology. Eur. Heart J. 2007, 28, 3076–3093. [Google Scholar] [CrossRef] [PubMed]
- Elliott, P.M.; Anastasakis, A.; Borger, M.A.; Borggrefe, M.; Cecchi, F.; Charron, P.; Hagege, A.A.; Lafont, A.; Limongelli, G.; Mahrholdt, H.; et al. European Society of Cardiology Guidelines on Diagnosis and Management of Hypertrophic Cardiomyopathy. Eur. Heart J. 2014, 35, 2733–2779. [Google Scholar] [PubMed]
- Lang, R.M.; Badano, L.P.; Victor, M.A.; Afilalo, J.; Armstrong, A.; Ernande, L.; Flachskampf, F.A.; Foster, E.; Goldstein, S.A.; Kuznetsova, T.; et al. Recommendations for Cardiac Chamber Quantification by Echocardiography in Adults: An Update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. J. Am. Soc. Echocardiogr. 2015, 16, 233–271. [Google Scholar] [CrossRef]
- Messroghli, D.R.; Moon, J.C.; Ferreira, V.M.; Grosse-Wortmann, L.; He, T.; Kellman, P.; Mascherbauer, J.; Nezafat, R.; Salerno, M.; Schelbert, E.B.; et al. Clinical Recommendations for Cardiovascular Magnetic Resonance Mapping of T1, T2, T2 and Extracellular Volume: A Consensus Statement by the Society for Cardiovascular Magnetic Resonance (SCMR) Endorsed by the European Association for Cardiovascular Imagin. J. Cardiovasc. Magn. Reson. 2017, 19, 75. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Boas, R.; Thune, J.J.; Pehrson, S.; Køber, L.; Nielsen, J.C.; Videbæk, L.; Haarbo, J.; Korup, E.; Bruun, N.E.; Brandes, A.; et al. Prevalence and Prognostic Association of Ventricular Arrhythmia in Non-Ischaemic Heart Failure Patients: Results from the DANISH Trial. Europace 2021, 23, 587–595. [Google Scholar] [CrossRef]
- Rudolph, A.; Abdel-Aty, H.; Bohl, S.; Boyé, P.; Zagrosek, A.; Dietz, R.; Schulz-Menger, J. Noninvasive Detection of Fibrosis Applying Contrast-Enhanced Cardiac Magnetic Resonance in Different Forms of Left Ventricular Hypertrophy. Relation to Remodeling. J. Am. Coll. Cardiol. 2009, 53, 284–291. [Google Scholar] [CrossRef] [Green Version]
- Moon, J.C.C.; Reed, E.; Sheppard, M.N.; Elkington, A.G.; Ho, S.Y.; Burke, M.; Petrou, M.; Pennell, D.J. The Histologic Basis of Late Gadolinium Enhancement Cardiovascular Magnetic Resonance in Hypertrophic Cardiomyopathy. J. Am. Coll. Cardiol. 2004, 43, 2260–2264. [Google Scholar] [CrossRef]
- Choudhury, L.; Mahrholdt, H.; Wagner, A.; Choi, K.M.; Elliott, M.D.; Klocke, F.J.; Bonow, R.O.; Judd, R.M.; Kim, R.J. Myocardial Scarring in Asymptomatic or Mildly Symptomatic Patients with Hypertrophic Cardiomyopathy. J. Am. Coll. Cardiol. 2002, 40, 2156–2164. [Google Scholar] [CrossRef] [Green Version]
- Adabag, A.S.; Maron, B.J.; Appelbaum, E.; Harrigan, C.J.; Buros, J.L.; Gibson, C.M.; Lesser, J.R.; Hanna, C.A.; Udelson, J.E.; Manning, W.J.; et al. Occurrence and Frequency of Arrhythmias in Hypertrophic Cardiomyopathy in Relation to Delayed Enhancement on Cardiovascular Magnetic Resonance. J. Am. Coll. Cardiol. 2008, 51, 1369–1374. [Google Scholar] [CrossRef] [Green Version]
- Prinz, C.; Schwarz, M.; Ilic, I.; Laser, K.T.; Lehmann, R.; Prinz, E.M.; Bitter, T.; Vogt, J.; Van Buuren, F.; Bogunovic, N.; et al. Myocardial Fibrosis Severity on Cardiac Magnetic Resonance Imaging Predicts Sustained Arrhythmic Events in Hypertrophic Cardiomyopathy. Can. J. Cardiol. 2013, 29, 358–363. [Google Scholar] [CrossRef]
- Ommen, S.R.; Mital, S.; Burke, M.A.; Day, S.M.; Deswal, A.; Elliott, P.; Evanovich, L.L.; Hung, J.; Joglar, J.A.; Kantor, P.; et al. 2020 AHA/ACC Guideline for the Diagnosis and Treatment of Patients with Hypertrophic Cardiomyopathy: Executive Summary: A Report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. J. Am. Coll. Cardiol. 2020, 76, 3022–3055. [Google Scholar] [CrossRef] [PubMed]
- Chan, R.H.; Maron, B.J.; Olivotto, I.; Pencina, M.J.; Assenza, G.E.; Haas, T.; Lesser, J.R.; Gruner, C.; Crean, A.M.; Rakowski, H.; et al. Prognostic Value of Quantitative Contrast-Enhanced Cardiovascular Magnetic Resonance for the Evaluation of Sudden Death Risk in Patients with Hypertrophic Cardiomyopathy. Circulation 2014, 130, 484–495. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Weng, Z.; Yao, J.; Chan, R.H.; He, J.; Yang, X.; Zhou, Y.; He, Y. Prognostic Value of LGE-CMR in HCM: A Meta-Analysis. JACC Cardiovasc. Imaging 2016, 9, 1392–1402. [Google Scholar] [CrossRef]
- Weissler-Snir, A.; Hindieh, W.; Spears, D.A.; Adler, A.; Rakowski, H.; Chan, R.H. The Relationship between the Quantitative Extent of Late Gadolinium Enhancement and Burden of Nonsustained Ventricular Tachycardia in Hypertrophic Cardiomyopathy: A Delayed Contrast-Enhanced Magnetic Resonance Study. J. Cardiovasc. Electrophysiol. 2019, 30, 651–657. [Google Scholar] [CrossRef]
- Briasoulis, A.; Mallikethi-Reddy, S.; Palla, M.; Alesh, I.; Afonso, L. Myocardial Fibrosis on Cardiac Magnetic Resonance and Cardiac Outcomes in Hypertrophic Cardiomyopathy: A Meta-Analysis. Heart 2015, 101, 1406–1411. [Google Scholar] [CrossRef] [PubMed]
- Maron, M.S.; Appelbaum, E.; Harrigan, C.J.; Buros, J.; Gibson, C.M.; Hanna, C.; Lesser, J.R.; Udelson, J.E.; Manning, W.J.; Maron, B.J. Clinical Profile and Significance of Delayed Enhancement in Hypertrophic Cardiomyopathy. Circ. Heart Fail. 2008, 1, 184–191. [Google Scholar] [CrossRef] [Green Version]
- Green, J.J.; Berger, J.S.; Kramer, C.M.; Salerno, M. Prognostic Value of Late Gadolinium Enhancement in Clinical Outcomes for Hypertrophic Cardiomyopathy. JACC Cardiovasc. Imaging 2012, 5, 370–377. [Google Scholar] [CrossRef] [Green Version]
- Ismail, T.F.; Jabbour, A.; Gulati, A.; Mallorie, A.; Raza, S.; Cowling, T.E.; Das, B.; Khwaja, J.; Alpendurada, F.D.; Wage, R.; et al. Role of Late Gadolinium Enhancement Cardiovascular Magnetic Resonance in the Risk Stratification of Hypertrophic Cardiomyopathy. Heart 2014, 100, 1851–1858. [Google Scholar] [CrossRef]
- O’Hanlon, R.; Grasso, A.; Roughton, M.; Moon, J.C.; Clark, S.; Wage, R.; Webb, J.; Kulkarni, M.; Dawson, D.; Sulaibeekh, L.; et al. Prognostic Significance of Myocardial Fibrosis in Hypertrophic Cardiomyopathy. J. Am. Coll. Cardiol. 2010, 56, 867–874. [Google Scholar] [CrossRef] [Green Version]
- McLellan, A.J.A.; Ellims, A.H.; Prabhu, S.; Voskoboinik, A.; Iles, L.M.; Hare, J.L.; Kaye, D.M.; MacCiocca, I.; Mariani, J.A.; Kalman, J.M.; et al. Diffuse Ventricular Fibrosis on Cardiac Magnetic Resonance Imaging Associates with Ventricular Tachycardia in Patients with Hypertrophic Cardiomyopathy. J. Cardiovasc. Electrophysiol. 2016, 27, 571–580. [Google Scholar] [CrossRef]
- Avanesov, M.; Münch, J.; Weinrich, J.; Well, L.; Säring, D.; Stehning, C.; Tahir, E.; Bohnen, S.; Radunski, U.K.; Muellerleile, K.; et al. Prediction of the Estimated 5-Year Risk of Sudden Cardiac Death and Syncope or Non-Sustained Ventricular Tachycardia in Patients with Hypertrophic Cardiomyopathy Using Late Gadolinium Enhancement and Extracellular Volume CMR. Eur. Radiol. 2017, 27, 5136–5145. [Google Scholar] [CrossRef] [PubMed]
- Levine, J.; Collins, J.D.; Ogele, E.; Murtagh, G.; Carr, J.C.; Bonow, R.O.; Choudhury, L. Relation of Late Gadolinium Enhancement and Extracellular Volume Fraction to Ventricular Arrhythmias in Hypertrophic Cardiomyopathy. Am. J. Cardiol. 2020, 131, 104–108. [Google Scholar] [CrossRef] [PubMed]
- Mentias, A.; Raeisi-Giglou, P.; Smedira, N.G.; Feng, K.; Sato, K.; Wazni, O.; Kanj, M.; Flamm, S.D.; Thamilarasan, M.; Popovic, Z.B.; et al. Late Gadolinium Enhancement in Patients With Hypertrophic Cardiomyopathy and Preserved Systolic Function. J. Am. Coll. Cardiol. 2018, 72, 857–870. [Google Scholar] [CrossRef] [PubMed]
- O’Mahony, C.; Jichi, F.; Pavlou, M.; Monserrat, L.; Anastasakis, A.; Rapezzi, C.; Biagini, E.; Gimeno, J.R.; Limongelli, G.; McKenna, W.J.; et al. A Novel Clinical Risk Prediction Model for Sudden Cardiac Death in Hypertrophic Cardiomyopathy (HCM Risk-SCD). Eur. Heart J. 2014, 35, 2010–2020. [Google Scholar] [CrossRef]
- Spirito, P.; Autore, C.; Rapezzi, C.; Bernabò, P.; Badagliacca, R.; Maron, M.S.; Bongioanni, S.; Coccolo, F.; Estes, N.A.M.; Barillà, C.S.; et al. Syncope and Risk of Sudden Death in Hypertrophic Cardiomyopathy. Circulation 2009, 119, 1703–1710. [Google Scholar] [CrossRef] [Green Version]
- Chung, H.; Park, C.H.; Kim, Y.; Kim, J.Y.; Min, P.K.; Yoon, Y.W.; Lee, K.A.; Lee, B.K.; Hong, B.K.; Kim, T.H.; et al. Burden of Premature Ventricular Contractions beyond Nonsustained Ventricular Tachycardia Is Related to the Myocardial Extracellular Space Expansion in Patients with Hypertrophic-Cardiomyopathy. Clin. Cardiol. 2020, 43, 1317–1325. [Google Scholar] [CrossRef]
- Mirelis, J.G.; Sánchez-González, J.; Zorio, E.; Ripoll-Vera, T.; Salguero-Bodes, R.; Filgueiras-Rama, D.; González-López, E.; Gallego-Delgado, M.; Fernández-Jiménez, R.; Soleto, M.J.; et al. Myocardial Extracellular Volume Is Not Associated With Malignant Ventricular Arrhythmias in High-Risk Hypertrophic Cardiomyopathy. Rev. Española Cardiol. (Engl. Ed.) 2017, 70, 933–940. [Google Scholar] [CrossRef]
- Karamitsos, T.D.; Arvanitaki, A.; Karvounis, H.; Neubauer, S.; Ferreira, V.M. Myocardial Tissue Characterization and Fibrosis by Imaging. JACC Cardiovasc. Imaging 2020, 13, 1221–1234. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).