Traditional versus Minimally Invasive Spinopelvic Fixation for Sacral Fracture Treatment in Vertically Unstable Pelvic Fractures
Abstract
1. Introduction
2. Materials and Methods
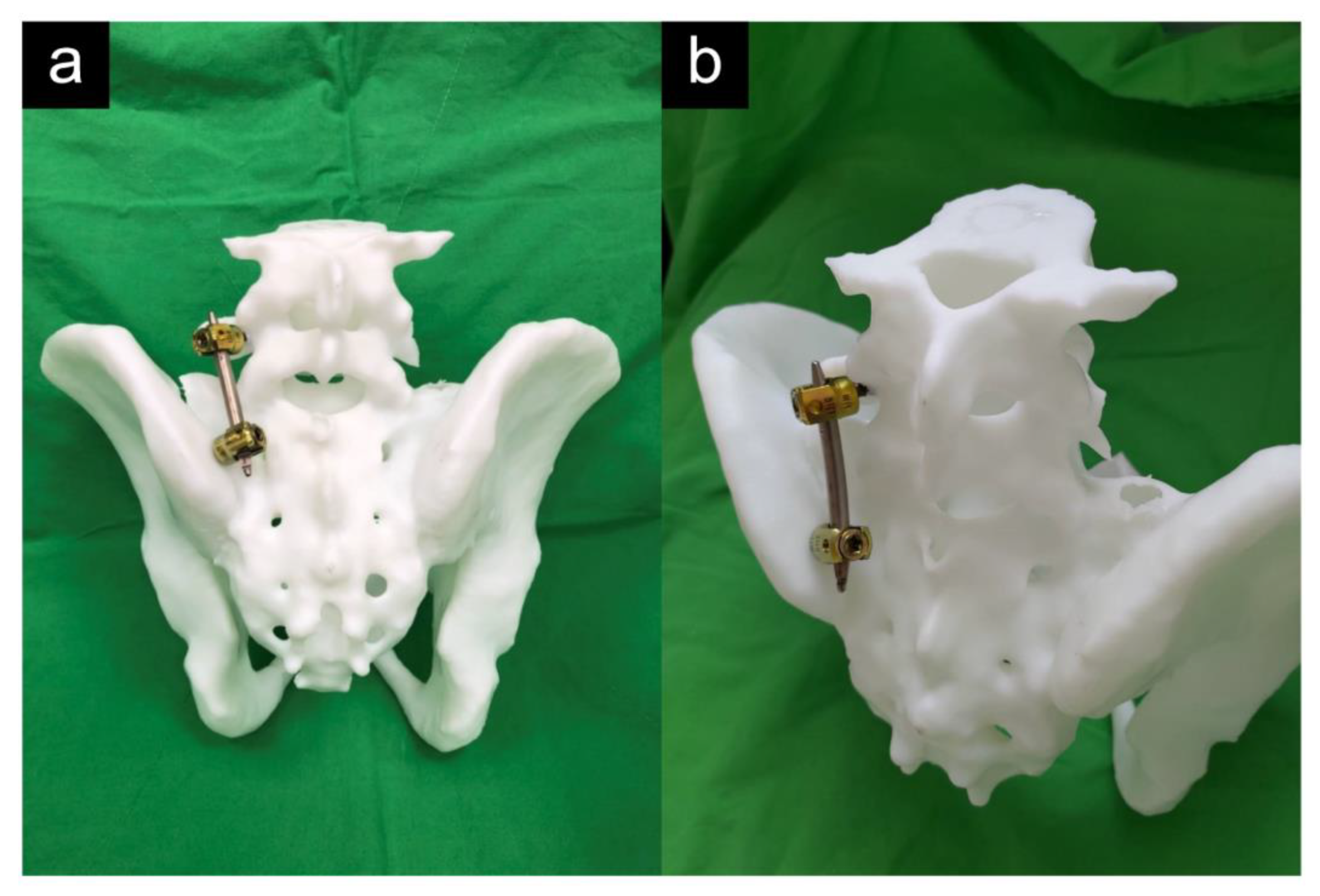
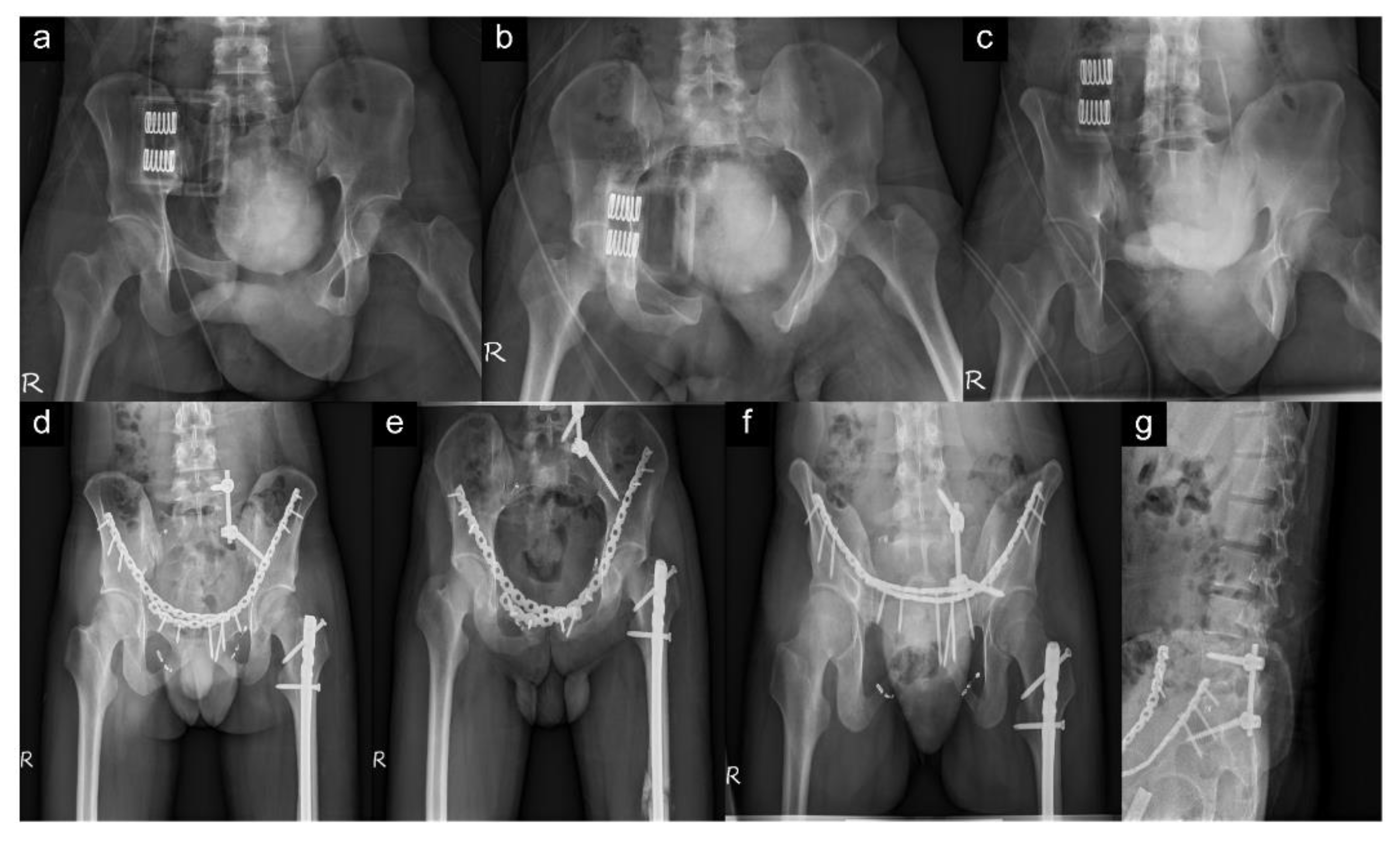
2.1. Surgical Technique
2.2. Outcome Measurement
3. Results
3.1. Perioperative Clinical Parameters
3.2. Postoperative Radiographic Results and Functional Outcome
3.3. Postoperative Complications
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Rodrigues-Pinto, R.; Kurd, M.F.; Schroeder, G.D.; Kepler, C.K.; Krieg, J.C.; Holstein, J.H.; Bellabarba, C.; Firoozabadi, R.; Oner, F.C.; Kandziora, F.; et al. Sacral Fractures and Associated Injuries. Glob. Spine J. 2017, 7, 609–616. [Google Scholar] [CrossRef] [PubMed]
- Bydon, M.; De la Garza-Ramos, R.; Macki, M.; Desai, A.; Gokaslan, A.K.; Bydon, A. Incidence of Sacral Fractures and In-Hospital Postoperative Complications in the United States: An analysis of 2002–2011 data. Spine 2014, 39, E1103–E1109. [Google Scholar] [CrossRef] [PubMed]
- Denis, F.; Davis, S.; Comfort, T. Sacral fractures: An important problem. Retrospective analysis of 236 cases. Clin. Orthop. Relat. Res. 1988, 227, 67–81. [Google Scholar] [CrossRef] [PubMed]
- Jazini, E.; Weir, T.; Nwodim, E.; Tannous, O.; Saifi, C.; Caffes, N.; Costales, T.; Koh, E.; Banagan, K.; Gelb, D.; et al. Outcomes of lumbopelvic fixation in the treatment of complex sacral fractures using minimally invasive surgical techniques. Spine J. 2017, 17, 1238–1246. [Google Scholar] [CrossRef] [PubMed]
- Berber, O.; Amis, A.A.; Day, A.C. Biomechanical testing of a concept of posterior pelvic reconstruction in rotationally and vertically unstable fractures. J. Bone Jt. Surgery. Br. Vol. 2011, 93-B, 237–244. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Schildhauer, T.A.; Ledoux, W.; Chapman, J.R.; Henley, M.B.; Tencer, A.F.; Routt, M.L.C. Triangular Osteosynthesis and Iliosacral Screw Fixation for Unstable Sacral Fractures: A Cadaveric and Biomechanical Evaluation under Cyclic Loads. J. Orthop. Trauma 2003, 17, 22–31. [Google Scholar] [CrossRef] [PubMed]
- Chou, D.T.S.; El-Daly, I.; Ranganathan, A.; Montgomery, A.; Culpan, P.; Bates, P. Spinopelvic Dissociation: A retrospective case study and review of treatment controversies. J. Am. Acad. Orthop. Surg. 2018, 26, e302–e312. [Google Scholar] [CrossRef] [PubMed]
- Bellabarba, C.; Schildhauer, T.A.; Vaccaro, A.R.; Chapman, J.R. Complications Associated with Surgical Stabilization of High-Grade Sacral Fracture Dislocations with Spino-Pelvic Instability. Spine 2006, 31 (Suppl. 11), S80–S88. [Google Scholar] [CrossRef] [PubMed]
- Koshimune, K.; Ito, Y.; Sugimoto, Y.; Kikuchi, T.; Morita, T.; Mizuno, S.; Ozaki, T. Minimally Invasive Spinopelvic Fixation for Unstable Bilateral Sacral Fractures. Clin. Spine Surg. 2016, 29, 124–127. [Google Scholar] [CrossRef] [PubMed]
- Okuda, A.; Maegawa, N.; Matsumori, H.; Kura, T.; Mizutani, Y.; Shigematsu, H.; Iwata, E.; Tanaka, M.; Masuda, K.; Yamamoto, Y.; et al. Minimally invasive spinopelvic “crab-shaped fixation” for unstable pelvic ring fractures: Technical note and 16 case series. J. Orthop. Surg. Res. 2019, 14, 1–7. [Google Scholar] [CrossRef]
- Nepola, J.V.; Trenhaile, S.W.; Miranda, M.A.; Butterfield, S.L.; Fredericks, D.C.; Riemer, B.L. Vertical Shear Injuries: Is there a relationship between residual displacement and functional outcome? J. Trauma Acute Care Surg. 1999, 46, 1024–1030. [Google Scholar] [CrossRef] [PubMed]
- Williams, S.K.; Quinnan, S.M. Percutaneous Lumbopelvic Fixation for Reduction and Stabilization of Sacral Fractures with Spinopelvic Dissociation Patterns. J. Orthop. Trauma 2016, 30, e318–e324. [Google Scholar] [CrossRef] [PubMed]
- König, M.A.; Jehan, S.; Boszczyk, A.A.; Boszczyk, B.M. Surgical management of U-shaped sacral fractures: A systematic review of current treatment strategies. Eur. Spine J. 2012, 21, 829–836. [Google Scholar] [CrossRef] [PubMed]
- Schildhauer, T.; Bellabarba, C.; Nork, S.E.; Barei, D.P.; Routt, M.L.C.; Chapman, J.R. Decompression and Lumbopelvic Fixation for Sacral Fracture-Dislocations with Spino-pelvic Dissociation. J. Orthop. Trauma 2006, 20, 447–457. [Google Scholar] [CrossRef] [PubMed]
- Gray, R.; Molnar, R.; Suthersan, M. A minimally invasive surgical technique for the management of U-shape sacral fractures. Spinal Cord Ser. Cases 2017, 3, 17045. [Google Scholar] [CrossRef] [PubMed]
- Sohn, S.; Chung, C.K.; Kim, Y.J.; Kim, C.H.; Park, S.B.; Kim, H. Modified iliac screw fixation: Technique and clinical application. Acta Neurochir. 2016, 158, 975–980. [Google Scholar] [CrossRef] [PubMed]
- Lonstein, J.E.; Denis, F.; Perra, J.H.; Pinto, M.R.; Smith, M.D.; Winter, R.B. Complications Associated with Pedicle Screws*. J. Bone Jt. Surg. 1999, 81, 1519–1528. [Google Scholar] [CrossRef] [PubMed]
- Sagi, H.C. Technical Aspects and Recommended Treatment Algorithms in Triangular Osteosynthesis and Spinopelvic Fixation for Vertical Shear Transforaminal Sacral Fractures. J. Orthop. Trauma 2009, 23, 354–360. [Google Scholar] [CrossRef] [PubMed]
- Kaye, I.D.; Yoon, R.S.; Stickney, W.; Snavely, J.; Vaccaro, A.R.; Liporace, F.A. Treatment of Spinopelvic Dissociation: A critical analysis review. JBJS Rev. 2018, 6, e7. [Google Scholar] [CrossRef] [PubMed]


| Variables | Group 1 (n = 21) | Group 2 (n = 17) | p Value |
|---|---|---|---|
| Age, M ± SD | 38.24 ± 12.91 | 44.71 ± 19.07 | 0.222 a |
| Day to surgery, M ± SD | 9.38 ± 7.36 | 7.71 ± 5.99 | 0.454 a |
| Sex | 1.000 a | ||
| Female | 9 (42.9%) | 7 (41.2%) | |
| Male | 12 (57.1%) | 10 (58.8%) | |
| Denis classification | 0.101 b | ||
| Zone I | 8 (38.1%) | 12 (70.6%) | |
| Zone II | 12 (57.1%) | 5 (29.4%) | |
| Zone III | 1 (4.8%) | 0 (0%) | |
| Implant | 0.638 a | ||
| Unilateral | 15 (71.4%) | 10 (58.8%) | |
| Bilateral | 6 (28.6%) | 7 (41.2%) | |
| Sacroiliac screw | 1.000 b | ||
| No | 5 (23.8%) | 4 (23.5%) | |
| Yes | 16 (76.2%) | 13 (76.5%) |
| Group 1 (n = 21) | Group 2 (n = 17) | p Value | |
|---|---|---|---|
| Operation time | 193.19 ± 89.88 | 141.47 ± 34.88 | 0.022 a |
| Blood loss | 330.48 ± 137.20 | 42.65 ± 25.50 | <0.001 a |
| Radiographic grading | 0.489 b | ||
| Excellent | 15 (71.4%) | 9 (52.9%) | |
| Good | 5 (23.8%) | 7 (41.2%) | |
| Fair | 1 (4.8%) | 1 (5.9%) | |
| Complications | 1.000 b | ||
| No | 19 (90.5%) | 16 (94.1%) | |
| Yes | 2 (9.5%) | 1 (5.9%) |
| Group 1 (n = 21) | Group 2 (n = 17) | ||
|---|---|---|---|
| No. (%) | No. (%) | ap-Value | |
| Iowa score, M ± SD | 83.3 ± 8.1 | 87.6 ± 5.7 | 0.072 |
| With associated injury | (n = 17) | (n = 14) | |
| Iowa score, M ± SD | 82.8 ± 7.8 | 87.6 ± 5.9 | 0.067 |
| Without associated injury | (n = 4) | (n = 3) | |
| Iowa score, M ± SD | 85.3 ± 10.2 | 87.3 ± 5.1 | 0.763 |
| Associated injury | 1.000 | ||
| Yes | 17 (81.0) | 14 (82.4) | |
| No | 4 (19.0) | 3 (17.6) | |
| Cosmetic appearance | 0.007 | ||
| Significant | 14 (66.7) | 3 (17.6) | |
| Not significant | 7 (33.3) | 14 (82.4) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tsai, Y.-T.; Chou, Y.-C.; Wu, C.-C.; Yeh, T.-T. Traditional versus Minimally Invasive Spinopelvic Fixation for Sacral Fracture Treatment in Vertically Unstable Pelvic Fractures. J. Pers. Med. 2022, 12, 262. https://doi.org/10.3390/jpm12020262
Tsai Y-T, Chou Y-C, Wu C-C, Yeh T-T. Traditional versus Minimally Invasive Spinopelvic Fixation for Sacral Fracture Treatment in Vertically Unstable Pelvic Fractures. Journal of Personalized Medicine. 2022; 12(2):262. https://doi.org/10.3390/jpm12020262
Chicago/Turabian StyleTsai, Yao-Tung, Yu-Ching Chou, Chia-Chun Wu, and Tsu-Te Yeh. 2022. "Traditional versus Minimally Invasive Spinopelvic Fixation for Sacral Fracture Treatment in Vertically Unstable Pelvic Fractures" Journal of Personalized Medicine 12, no. 2: 262. https://doi.org/10.3390/jpm12020262
APA StyleTsai, Y.-T., Chou, Y.-C., Wu, C.-C., & Yeh, T.-T. (2022). Traditional versus Minimally Invasive Spinopelvic Fixation for Sacral Fracture Treatment in Vertically Unstable Pelvic Fractures. Journal of Personalized Medicine, 12(2), 262. https://doi.org/10.3390/jpm12020262







