Effect of Pillbox Organizers with Alarms on Adherence to Pharmacotherapy in Parkinson Disease Patients Taking Three and More Daily Doses of Dopaminergic Medications
Abstract
:1. Introduction
2. Material and Methods
2.1. Participants
- idiopathic PD diagnosed according to the Movement Disorder Society (MDS) Clinical Diagnostic Criteria for PD [16],
- on standard dopaminergic medication with levodopa (plus dopa-decarboxylase inhibitor) and/or dopamine agonists in a minimum of three daily doses (therapeutic regimen had to be stable for a minimum of four weeks prior enrollment),
- without cognitive impairment (>26/30 points on the Mini-Mental State Examination, MMSE), and
- non-adherent patients who scored <6/8 points on the Morisky 8-Item Medication Adherence Scale (MMAS-8) [17].
2.2. Methods
- the Morisky 8-Item Medication Adherence Scale (MMAS-8), to detect medication adherence [17],
- the 8-Item Parkinson’s Disease Questionnaire (PDQ-8) [18], to detect QoL,
- the Non-Motor Symptom Assessment Scale for Parkinson’s Disease (NMSS) [21], to detect frequency and severity of NMS,
- the Movement Disorder Society—Unified Parkinson’s Disease Rating Scale (MDS-UPDRS)—part III: Motor examination (MDS-UPDRS III), to detect motor score,
- MDS-UPDRS—part IV: Motor complications (MDS-UPDRS IV) [22], to detect motor complications, and
- the Nine-Item Wearing-off Questionnaire (WOQ-9) [23], to detect wearing-off phenomenon (defined as motor and NMS fluctuations).
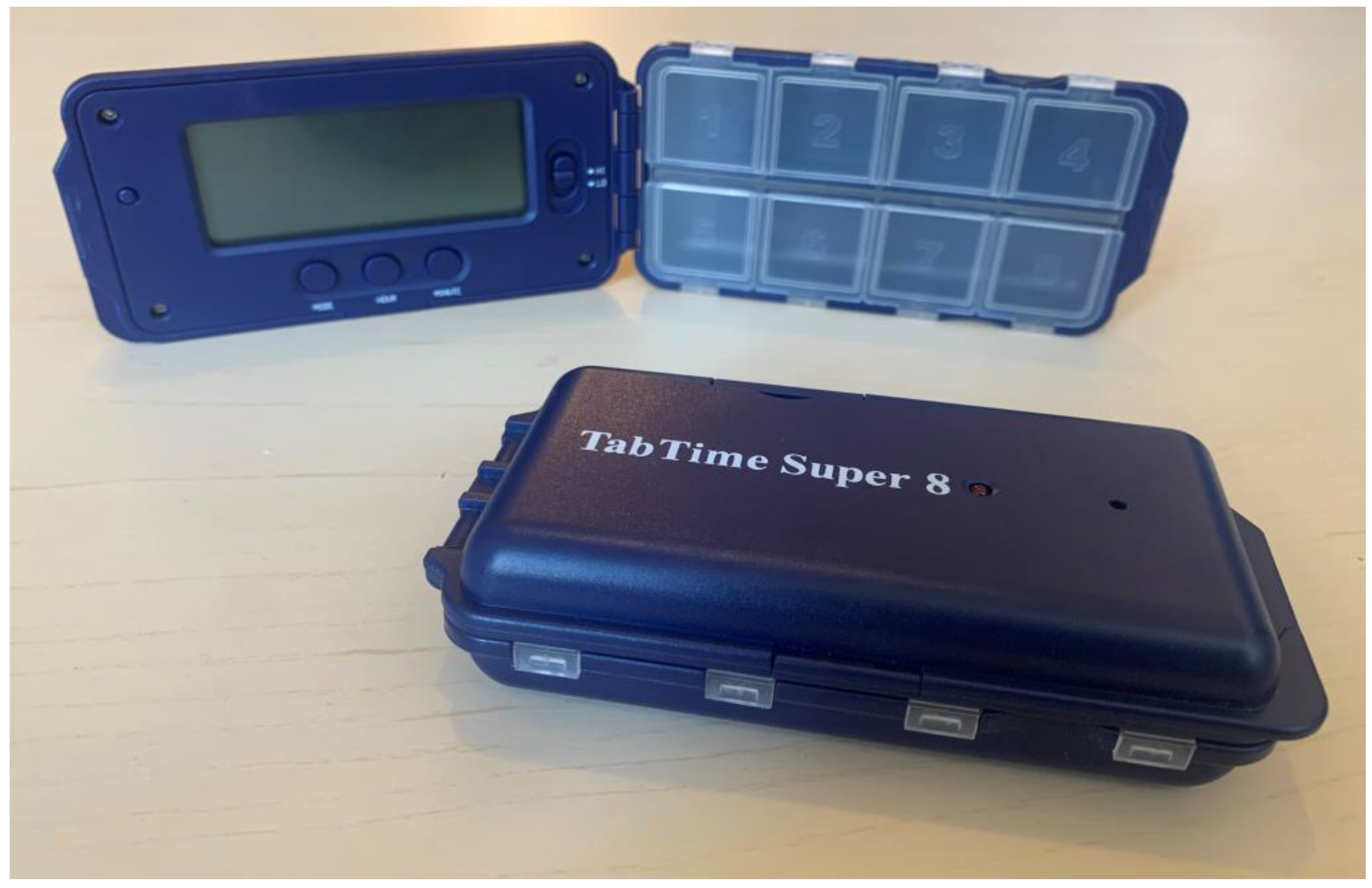
2.3. Pillbox Organizer with Alarm
2.4. Study Protocol
2.5. Statistical Analysis
3. Results
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Chaudhuri, K.R.; Poewe, W.; Brooks, D. Motor and Nonmotor Complications of Levodopa: Phenomenology, Risk Factors, and Imaging Features. Mov. Disord. 2018, 33, 909–919. [Google Scholar] [CrossRef] [PubMed]
- Sabaté, E.; World Health Organization (Eds.) Adherence to Long-Term Therapies: Evidence for Action; World Health Organization: Geneva, Switzerland, 2003. [Google Scholar]
- Brown, M.T.; Bussell, J.K. Medication adherence: WHO cares? Mayo Clin. Proc. 2011, 86, 304–314. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Giardini, A.; Maffoni, M.; Kardas, P.; Costa, E. A Cornerstone of Healthy Aging: Do We Need to Rethink the Concept of Adherence in the Elderly? Patient Prefer. Adherence 2018, 12, 1003–1005. [Google Scholar] [CrossRef] [Green Version]
- Prell, T.; Grosskreutz, J.; Mendorf, S.; Franke, G.H.; Witte, O.W.; Kunze, A. Clusters of Non-Adherence to Medication in Neurological Patients. Res. Soc. Adm. Pharm. 2019, 15, 1419–1424. [Google Scholar] [CrossRef] [PubMed]
- Richy, F.F.; Pietri, G.; Moran, K.A.; Senior, E.; Makaroff, L.E. Compliance with Pharmacotherapy and Direct Healthcare Costs in Patients with Parkinson’s Disease: A Retrospective Claims Database Analysis. Appl. Health Econ. Health Policy 2013, 11, 395–406. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Malek, N.; Grosset, D.G. Medication Adherence in Patients with Parkinson’s Disease. CNS Drugs 2015, 29, 47–53. [Google Scholar] [CrossRef] [PubMed]
- Foppa, A.A.; Chemello, C.; Vargas-Peláez, C.M.; Farias, M.R. Medication Therapy Management Service for Patients with Parkinson’s Disease: A Before-and-After Study. Neurol. Ther. 2016, 5, 85–99. [Google Scholar] [CrossRef] [Green Version]
- Johnsrud, M.; Richards, K.; Arcona, S.; Sasané, R.; Leoni, M. An Assessment of Parkinson’s Disease Medication Treatment Patterns in the Medicaid Population. Clin. Park. Relat. Disord. 2021, 5, 100109. [Google Scholar] [CrossRef]
- Straka, I.; Minár, M.; Škorvánek, M.; Grofik, M.; Danterová, K.; Benetin, J.; Kurča, E.; Gažová, A.; Boleková, V.; Wyman-Chick, K.A.; et al. Adherence to Pharmacotherapy in Patients with Parkinson’s Disease Taking Three and More Daily Doses of Medication. Front. Neurol. 2019, 10, 799. [Google Scholar] [CrossRef] [Green Version]
- Valldeoriola, F.; Coronell, C.; Pont, C.; Buongiorno, M.T.; Cámara, A.; Gaig, C.; Compta, Y.; on behalf of the members of the ADHESON Study Group. Socio-Demographic and Clinical Factors Influencing the Adherence to Treatment in Parkinson’s Disease: The ADHESON Study: Socio-Demographic and Clinical Factors in Treatment of Parkinson’s Disease. Eur. J. Neurol. 2011, 18, 980–987. [Google Scholar] [CrossRef]
- Costa, E.; Pecorelli, S.; Giardini, A.; Savin, M.; Menditto, E.; Lehane, E.; Laosa, O.; Monaco, A.; Marengoni, A. Interventional Tools to Improve Medication Adherence: Review of Literature. Patient Prefer. Adherence 2015, 9, 1303–1314. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kini, V.; Ho, P.M. Interventions to Improve Medication Adherence: A Review. JAMA 2018, 320, 2461. [Google Scholar] [CrossRef] [PubMed]
- Vieira, L.B.; Reis, A.M.M.; de Ramos, C.Á.; dos Reis, T.M.; de Cassiani, S.H.B. The Use of an Electronic Medication Organizer Device with Alarm to Improve Medication Adherence of Older Adults with Hypertension. Einstein São Paulo 2021, 19, eAO6011. [Google Scholar] [CrossRef] [PubMed]
- Straka, I.; Minár, M.; Gažová, A.; Valkovič, P.; Kyselovič, J. Clinical Aspects of Adherence to Pharmacotherapy in Parkinson Disease: A PRISMA-Compliant Systematic Review. Medicine 2018, 97, e10962. [Google Scholar] [CrossRef]
- Postuma, R.B.; Berg, D.; Stern, M.; Poewe, W.; Olanow, C.W.; Oertel, W.; Obeso, J.; Marek, K.; Litvan, I.; Lang, A.E.; et al. MDS Clinical Diagnostic Criteria for Parkinson’s Disease: MDS-PD Clinical Diagnostic Criteria. Mov. Disord. 2015, 30, 1591–1601. [Google Scholar] [CrossRef]
- Morisky, D.E.; Ang, A.; Krousel-Wood, M.; Ward, H.J. Predictive Validity of a Medication Adherence Measure in an Outpatient Setting. J. Clin. Hypertens. 2008, 10, 348–354. [Google Scholar] [CrossRef] [Green Version]
- Jenkinson, C.; Fitzpatrick, R.; Peto, V.; Greenhall, R.; Hyman, N. The PDQ-8: Development and Validation of a Short-Form Parkinson’s Disease Questionnaire. Psychol. Health 1997, 12, 805–814. [Google Scholar] [CrossRef]
- Ertan, F.S. Reliability and Validity of the Geriatric Depression Scale in Depression in Parkinson’s Disease. J. Neurol. Neurosurg. Psychiatry 2005, 76, 1445–1447. [Google Scholar] [CrossRef] [Green Version]
- Yesavage, J.A.; Brink, T.L.; Rose, T.L.; Lum, O.; Huang, V.; Adey, M.; Leirer, V.O. Development and Validation of a Geriatric Depression Screening Scale: A Preliminary Report. J. Psychiatr. Res. 1982, 17, 37–49. [Google Scholar] [CrossRef]
- Chaudhuri, K.R.; Martinez-Martin, P.; Brown, R.G.; Sethi, K.; Stocchi, F.; Odin, P.; Ondo, W.; Abe, K.; MacPhee, G.; MacMahon, D.; et al. The Metric Properties of a Novel Non-Motor Symptoms Scale for Parkinson’s Disease: Results from an International Pilot Study. Mov. Disord. 2007, 22, 1901–1911. [Google Scholar] [CrossRef]
- Goetz, C.G.; Tilley, B.C.; Shaftman, S.R.; Stebbins, G.T.; Fahn, S.; Martinez-Martin, P.; Poewe, W.; Sampaio, C.; Stern, M.B.; Dodel, R.; et al. Movement Disorder Society-Sponsored Revision of the Unified Parkinson’s Disease Rating Scale (MDS-UPDRS): Scale Presentation and Clinimetric Testing Results. Mov. Disord. 2008, 23, 2129–2170. [Google Scholar] [CrossRef] [PubMed]
- Stacy, M.; Hauser, R.; Oertel, W.; Schapira, A.; Sethi, K.; Stocchi, F.; Tolosa, E. End-of-Dose Wearing Off in Parkinson Disease: A 9-Question Survey Assessment. Clin. Neuropharmacol. 2006, 29, 312–321. [Google Scholar] [CrossRef] [PubMed]
- Jankovic, J.; McDermott, M.; Carter, J.; Gauthier, S.; Goetz, C.; Golbe, L.; Huber, S.; Koller, W.; Olanow, C.; Shoulson, I. Variable Expression of Parkinson’s Disease: A Base-Line Analysis of the DATATOP Cohort. The Parkinson Study Group. Neurology 1990, 40, 1529–1534. [Google Scholar] [CrossRef] [PubMed]
- Abegaz, T.M.; Shehab, A.; Gebreyohannes, E.A.; Bhagavathula, A.S.; Elnour, A.A. Nonadherence to Antihypertensive Drugs: A Systematic Review and Meta-Analysis. Medicine 2017, 96, e5641. [Google Scholar] [CrossRef]
- Morello, C.M.; Chynoweth, M.; Kim, H.; Singh, R.F.; Hirsch, J.D. Strategies to Improve Medication Adherence Reported by Diabetes Patients and Caregivers: Results of a Taking Control of Your Diabetes Survey. Ann. Pharmacother. 2011, 45, 145–153. [Google Scholar] [CrossRef]
- Porter, A.K.; Taylor, S.R.; Yabut, A.H.; Al-Achi, A. Impact of a Pill Box Clinic to Improve Systolic Blood Pressure in Veterans with Uncontrolled Hypertension Taking 3 or More Antihypertensive Medications. J. Manag. Care Pharm. 2014, 20, 905–911. [Google Scholar] [CrossRef] [Green Version]
- Castro, G.S.; Aguilar-Alvarado, C.M.; Zúñiga-Ramírez, C.; Sáenz-Farret, M.; Otero-Cerdeira, E.; Serrano-Dueñas, M.; González-Usigli, H.A.; Bernal, O.; Leal-Ortega, R.; Estrada-Bellmann, I.; et al. Adherence to Treatment in Parkinson’s Disease: A Multicenter Exploratory Study with Patients from Six Latin American Countries. Parkinsonism Relat. Disord. 2021, 93, 1–7. [Google Scholar] [CrossRef]
- Grosset, D.; Antonini, A.; Canesi, M.; Pezzoli, G.; Lees, A.; Shaw, K.; Cubo, E.; Martinez-Martin, P.; Rascol, O.; Negre-Pages, L.; et al. Adherence to Antiparkinson Medication in a Multicenter European Study. Mov. Disord. 2009, 24, 826–832. [Google Scholar] [CrossRef]
- Grosset, K.A.; Bone, I.; Grosset, D.G. Suboptimal Medication Adherence in Parkinson’s Disease. Mov. Disord. 2005, 20, 1502–1507. [Google Scholar] [CrossRef]
- Kulkarni, A.S.; Balkrishnan, R.; Anderson, R.T.; Edin, H.M.; Kirsch, J.; Stacy, M.A. Medication Adherence and Associated Outcomes in Medicare Health Maintenance Organization-Enrolled Older Adults with Parkinson’s Disease. Mov. Disord. 2008, 23, 359–365. [Google Scholar] [CrossRef]
- Mendorf, S.; Witte, O.W.; Grosskreutz, J.; Zipprich, H.M.; Prell, T. What Predicts Different Kinds of Nonadherent Behavior in Elderly People with Parkinson’s Disease? Front. Med. 2020, 7, 103. [Google Scholar] [CrossRef] [PubMed]
- Mendorf, S.; Witte, O.W.; Zipprich, H.; Prell, T. Association Between Nonmotor Symptoms and Nonadherence to Medication in Parkinson’s Disease. Front. Neurol. 2020, 11, 551696. [Google Scholar] [CrossRef] [PubMed]
- Ahlskog, J.E.; Muenter, M.D. Frequency of Levodopa-Related Dyskinesias and Motor Fluctuations as Estimated from the Cumulative Literature. Mov. Disord. Off. J. Mov. Disord. Soc. 2001, 16, 448–458. [Google Scholar] [CrossRef] [PubMed]
- Rascol, O.; Brooks, D.J.; Korczyn, A.D.; De Deyn, P.P.; Clarke, C.E.; Lang, A.E.; Abdalla, M. Development of Dyskinesias in a 5-Year Trial of Ropinirole and L-Dopa. Mov. Disord. 2006, 21, 1844–1850. [Google Scholar] [CrossRef]
- Van Wamelen, D.J.; Grigoriou, S.; Chaudhuri, K.R.; Odin, P. Continuous Drug Delivery Aiming Continuous Dopaminergic Stimulation in Parkinson’s Disease. J. Park. Dis. 2018, 8, S65–S72. [Google Scholar] [CrossRef] [Green Version]
- Kim, S.R.; Kim, J.Y.; Kim, H.Y.; So, H.Y.; Chung, S.J. Factors Associated with Medication Beliefs in Patients with Parkinson’s Disease: A Cross-Sectional Study. J. Mov. Disord. 2021, 14, 133–143. [Google Scholar] [CrossRef]
- Zipprich, H.M.; Mendorf, S.; Lehmann, T.; Prell, T. Self-Reported Nonadherence to Medication Is Not Associated with Health-Related Quality of Life in Parkinson’s Disease. Brain Sci. 2021, 11, 273. [Google Scholar] [CrossRef]
- Titova, N.; Chaudhuri, K.R. Non-Motor Parkinson Disease: New Concepts and Personalised Management. Med. J. Aust. 2018, 208, 404–409. [Google Scholar] [CrossRef] [Green Version]
- Zipprich, H.M.; Mendorf, S.; Schönenberg, A.; Prell, T. The Impact of Poor Medication Knowledge on Health-Related Quality of Life in People with Parkinson’s Disease: A Mediation Analysis. Qual. Life Res. 2021, 1–10. [Google Scholar] [CrossRef]
- Bainbridge, J.L.; Ruscin, J.M. Challenges of Treatment Adherence in Older Patients with Parkinson’s Disease. Drugs Aging 2009, 26, 145–155. [Google Scholar] [CrossRef]

| Demographic and Clinical Data | Together | Group A (n = 20) | Group B (n = 20) | p |
|---|---|---|---|---|
| Men | 26 (65.00%) | 12 (60.00%) | 14 (70.00%) | 0.507 |
| Women | 14 (35.00%) | 8 (40.00%) | 6 (30.00%) | |
| Age (year) | 68.50 (13.50) | 68.00 (8.75) | 69.50 (16.50) | 0.659 |
| Duration of PD (year) | 7.00 (4.00) | 7.50 (3.75) | 7.00 (3.75) | 0.096 |
| H&Y | 2.5 (1.00) | 2.5 (0.88) | 2.5 (1.00) | 0.371 |
| LEDD | 1314.00 (611.00) | 1185.00 (638.50) | 1367.50 (628.13) | 0.799 |
| Number of PD drug/day | 7.00 (4.75) | 9.00 (6.00) | 7.00 (2.75) | 0.253 |
| Number of PD doses/day | 5.00 (1.75) | 5.00 (2.00) | 5.00 (1.00) | 0.841 |
| Fluctuating patients (according to MDS-UPDRS IV) | 27 (67.50%) | 15 (75.00%) | 16 (80.00%) | 0.705 |
| Scales and Questionnaires | V0 | V1 | V2 | Wilcoxon Test | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Median (IQR) | Median (IQR) | Median (IQR) | V0–V1 | V1–V2 | V0–V2 | ||||||||
| Z | p | r | Z | p | r | Z | p | r | |||||
| MMAS-8 | A | 4.00 (2.00) | 7.00 (1.00) | 6.00 (1.00) | −3.985 | <0.001 | 0.891 | 3.333 | 0.999 | 0.745 | −3.967 | <0.001 | 0.887 |
| B | 4.50 (1.00) | 4.00 (1.00) | 7.00 (0.75) | −1.342 | 0.540 | 0.300 | −3.975 | <0.001 | 0.889 | −3.975 | <0.001 | 0.889 | |
| PDQ-8 | A | 8.50 (10.00) | 7.00 (7.50) | 7.50 (6.75) | −3.639 | <0.001 | 0.814 | −0.162 | 0.999 | 0.036 | −3.401 | 0.003 | 0.760 |
| B | 9.50 (9.00) | 10.00 (9.50) | 7.00 (7.50) | −1.732 | 0.249 | 0.387 | −3.535 | <0.001 | 0.790 | −3.531 | <0.001 | 0.790 | |
| GDS | A | 9.00 (9.50) | 9.50 (7.50) | 9.00 (7.00) | −1.103 | 0.810 | 0.247 | −1.107 | 0.804 | 0.248 | −0.082 | 0.999 | 0.018 |
| B | 10.00 (10.50) | 10.00 (9.75) | 11.00 (12.25) | −0.500 | 0.999 | 0.112 | −1.637 | 0.306 | 0.366 | −1.457 | 0.435 | 0.326 | |
| NMSS | A | 64.50 (49.00) | 65.50 (44.25) | 64.00 (45.75) | −1.645 | 0.300 | 0.368 | −0.044 | 0.999 | 0.010 | −1.572 | 0.348 | 0.352 |
| B | 76.50 (50.75) | 76.00 (51.00) | 75.50 (49.50) | −0.526 | 0.999 | 0.118 | −1.164 | 0.735 | 0.260 | −1.727 | 0.252 | 0.386 | |
| MDS-UPDRS III | A | 33.00 (10.75) | 31.00 (10.75) | 31.00 (11.50) | −2.999 | 0.009 | 0.671 | −1.811 | 0.210 | 0.405 | −2.389 | 0.051 | 0.534 |
| B | 35.00 (13.50) | 35.00 (13.75) | 32.00 (12.50) | −0.957 | 0.999 | 0.214 | −3.275 | 0.003 | 0.732 | −2.441 | 0.045 | 0.546 | |
| MDS-UPDRS IV | A | 7.00 (9.25) | 5.00 (7.00) | 5.00 (6.75) | −3.209 | 0.003 | 0.718 | −0.557 | 0.999 | 0.125 | −3.238 | 0.003 | 0.724 |
| B | 7.00 (6.50) | 7.00 (6.00) | 4.50 (4.00) | −1.633 | 0.306 | 0.365 | −3.438 | 0.003 | 0.769 | −3.184 | 0.003 | 0.712 | |
| WOQ-9 | A | 4.00 (3.00) | 2.00 (3.00) | 2.00 (2.00) | −3.442 | 0.003 | 0.770 | −1.265 | 0.618 | 0.283 | −3.602 | <0.001 | 0.805 |
| B | 4.00 (2.75) | 3.50 (3.00) | 2.00 (1.00) | −1.414 | 0.471 | 0.316 | −2.986 | 0.009 | 0.668 | −3.114 | 0.006 | 0.696 | |
| Scales and Questionnaires | Visit | Mann-Whitney U | Z | p | r |
|---|---|---|---|---|---|
| MMAS-8 | V0 | 154.50 | −1.311 | 0.663 | 0.207 |
| V1 | 16.00 | −5.127 | <0.001 | 0.811 | |
| V2 | 123.50 | −2.315 | 0.114 | 0.366 | |
| PDQ-8 | V0 | 199.00 | −0.027 | 0.999 | 0.004 |
| V1 | 137.00 | −1.710 | 0.273 | 0.270 | |
| V2 | 191.00 | −0.245 | 0.999 | 0.039 | |
| GDS | V0 | 166.50 | −0.909 | 0.999 | 0.144 |
| V1 | 175.50 | −0.664 | 0.999 | 0.105 | |
| V2 | 184.00 | −0.434 | 0.999 | 0.069 | |
| NMSS | V0 | 190.00 | −0.271 | 0.999 | 0.043 |
| V1 | 189.00 | −0.298 | 0.999 | 0.047 | |
| V2 | 185.00 | −0.406 | 0.999 | 0.064 | |
| MDS-UPDRS III | V0 | 164.00 | −0.975 | 0.999 | 0.154 |
| V1 | 134.50 | −1.774 | 0.228 | 0.280 | |
| V2 | 173.00 | −0.731 | 0.999 | 0.116 | |
| MDS-UPDRS IV | V0 | 197.00 | −0.082 | 0.999 | 0.013 |
| V1 | 137.50 | −1.707 | 0.273 | 0.270 | |
| V2 | 193.00 | −0.191 | 0.999 | 0.030 | |
| WOQ-9 | V0 | 191.00 | −0.247 | 0.999 | 0.039 |
| V1 | 136.00 | −1.754 | 0.258 | 0.277 | |
| V2 | 173.00 | −0.748 | 0.999 | 0.118 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Straka, I.; Minar, M.; Grofik, M.; Skorvanek, M.; Bolekova, V.; Gazova, A.; Kyselovic, J.; Valkovic, P. Effect of Pillbox Organizers with Alarms on Adherence to Pharmacotherapy in Parkinson Disease Patients Taking Three and More Daily Doses of Dopaminergic Medications. J. Pers. Med. 2022, 12, 179. https://doi.org/10.3390/jpm12020179
Straka I, Minar M, Grofik M, Skorvanek M, Bolekova V, Gazova A, Kyselovic J, Valkovic P. Effect of Pillbox Organizers with Alarms on Adherence to Pharmacotherapy in Parkinson Disease Patients Taking Three and More Daily Doses of Dopaminergic Medications. Journal of Personalized Medicine. 2022; 12(2):179. https://doi.org/10.3390/jpm12020179
Chicago/Turabian StyleStraka, Igor, Michal Minar, Milan Grofik, Matej Skorvanek, Veronika Bolekova, Andrea Gazova, Jan Kyselovic, and Peter Valkovic. 2022. "Effect of Pillbox Organizers with Alarms on Adherence to Pharmacotherapy in Parkinson Disease Patients Taking Three and More Daily Doses of Dopaminergic Medications" Journal of Personalized Medicine 12, no. 2: 179. https://doi.org/10.3390/jpm12020179
APA StyleStraka, I., Minar, M., Grofik, M., Skorvanek, M., Bolekova, V., Gazova, A., Kyselovic, J., & Valkovic, P. (2022). Effect of Pillbox Organizers with Alarms on Adherence to Pharmacotherapy in Parkinson Disease Patients Taking Three and More Daily Doses of Dopaminergic Medications. Journal of Personalized Medicine, 12(2), 179. https://doi.org/10.3390/jpm12020179







