Antidepressants Drug Use during COVID-19 Waves in the Tuscan General Population: An Interrupted Time-Series Analysis
Abstract
:1. Introduction
2. Materials and Methods
2.1. Data Source and Ethical Approval
2.2. Study Cohorts
2.3. Exposure Definition
2.4. Outcomes and Definitions
2.5. Statistical Analysis
2.6. Patient and Public Involvement
3. Results
3.1. Prevalence of Drug Use
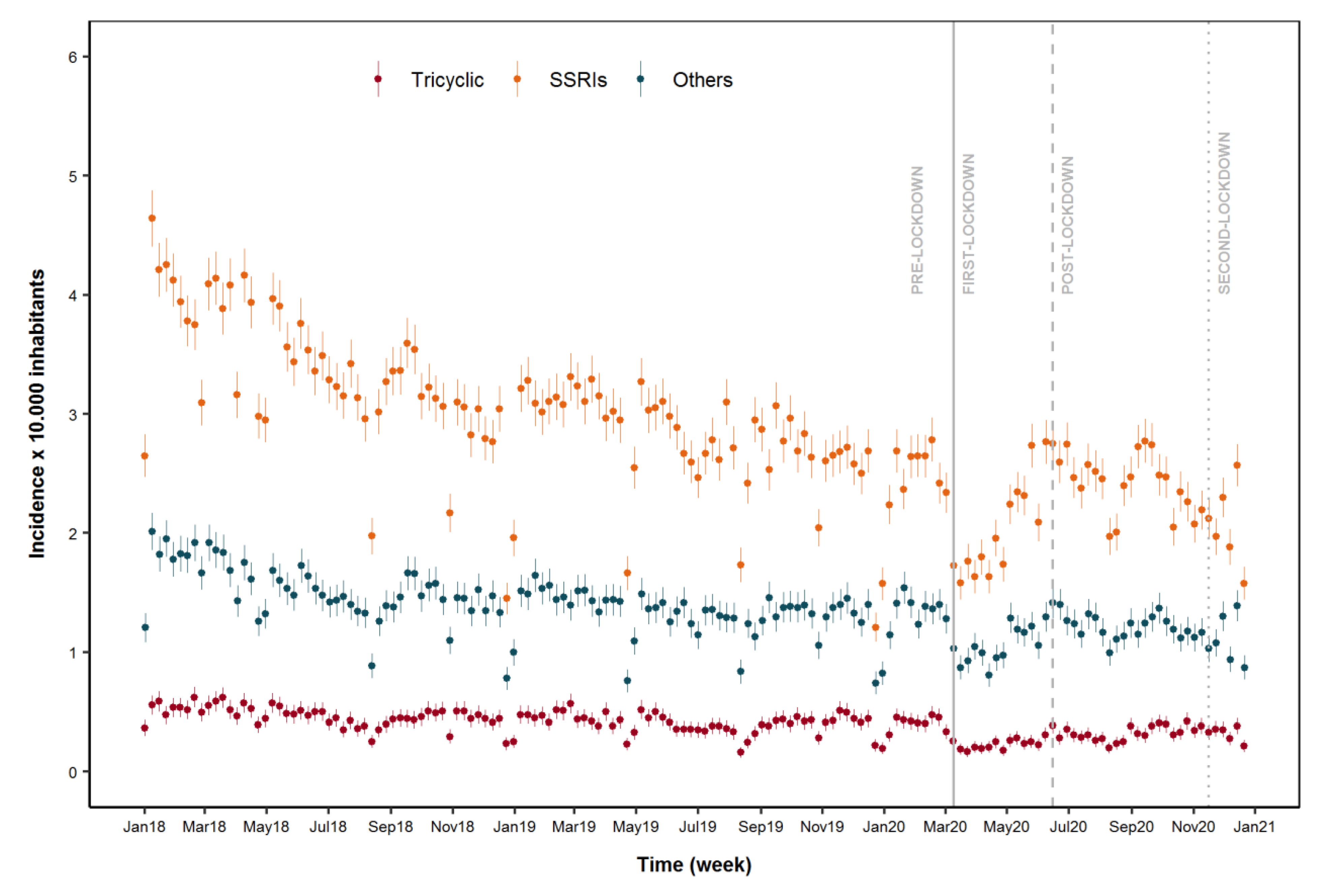
3.2. Incidence of Drug Use
4. Discussion
Strengths and Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A
References
- World Health Organization (WHO). WH Coronavirus (COVID-19) Dashboard. Available online: https://covid19.who.int/ (accessed on 10 October 2021).
- Helmy, Y.A.; Fawzy, M.; Elaswad, A.; Sobieh, A.; Kenney, S.P.; Shehata, A.A. The COVID-19 Pandemic: A Comprehensive Review of Taxonomy, Genetics, Epidemiology, Diagnosis, Treatment, and Control. J. Clin. Med. 2020, 9, 1225. [Google Scholar] [CrossRef] [PubMed]
- Sharma, R.; Agarwal, M.; Gupta, M.; Somendra, S.; Saxena, S.K. Clinical characteristics and differential clinical diagnosis of novel coronavirus disease 2019 (COVID-19). Coronavirus Dis. 2020; 9, 55–70. [Google Scholar] [CrossRef]
- Conti, S.; Ferrara, P.; Mazzaglia, G.; D’Orso, M.I.; Ciampichini, R.; Fornari, C.; Madotto, F.; Magoni, M.; Sampietro, G.; Silenzi, A.; et al. Magnitude and time-course of excess mortality during COVID-19 outbreak: Population-based empirical evidence from highly impacted provinces in northern Italy. ERJ Open Res. 2020, 6, 00458–2020. [Google Scholar] [CrossRef] [PubMed]
- Official Gazette of the Italian Republic. DPCM 22 marzo 2020. Ulteriori Disposizioni Attuative del Decreto-Legge 23 Febbraio 2020, n. 6, Recante Misure Urgenti in Materia di Contenimento e Gestione Dell’emergenza Epidemiologica da COVID-19, Applicabili Sull’intero Territorio Nazionale. n. 76 del 22 Marzo 2020. 2020. Available online: http://www.governo.it/it/articolo/coronavirus-firmato-il-dpcm-22-marzo-2020/14363 (accessed on 20 December 2020).
- Brooks, S.K.; Webster, R.K.; Smith, L.E.; Woodland, L.; Wessely, S.; Greenberg, N.; Rubin, G.J. The psychological impact of quarantine and how to reduce it: Rapid review of the evidence. Lancet 2020, 395, 912–920. [Google Scholar] [CrossRef] [Green Version]
- COVID-19 Mental Disorders Collaborators. Global prevalence and burden of depressive and anxiety disorders in 204 countries and territories in 2020 due to the COVID-19 pandemic. Lancet 2021, 398, 1700–1712. [Google Scholar] [CrossRef]
- Jacob, L.; Smith, L.; Koyanagi, A.; Oh, H.; Tanislav, C.; Shin, J.I.; Konrad, M.; Kostev, K. Impact of the coronavirus 2019 (COVID-19) pandemic on anxiety diagnosis in general practices in Germany. J. Psychiatr. Res. 2020, 143, 528–533. [Google Scholar] [CrossRef] [PubMed]
- Bäuerle, A.; Teufel, M.; Musche, V.; Weismüller, B.; Kohler, H.; Hetkamp, M.; Dörrie, N.; Schweda, A.; Skoda, E.-M. Increased generalized anxiety, depression and distress during the COVID-19 pandemic: A cross-sectional study in Germany. J. Public Health 2020, 42, 672–678. [Google Scholar] [CrossRef] [PubMed]
- Kamal, N.M.; Othman, N. Depression, Anxiety, and Stress in the time of COVID-19 Pandemic in Kurdistan Region, Iraq. Kurd. J. Appl. Res. 2020, 37–44. [Google Scholar] [CrossRef]
- Mazza, C.; Ricci, E.; Biondi, S.; Colasanti, M.; Ferracuti, S.; Napoli, C.; Roma, P. A Nationwide Survey of Psychological Distress among Italian People during the COVID-19 Pandemic: Immediate Psychological Responses and Associated Factors. Int. J. Environ. Res. Public Health 2020, 17, 3165. [Google Scholar] [CrossRef]
- Moghanibashi-Mansourieh, A. Assessing the anxiety level of Iranian general population during COVID-19 outbreak. Asian J. Psychiatry 2020, 51, 102076. [Google Scholar] [CrossRef]
- Odriozola-González, P.; Planchuelo-Gómez, A.; Irurtia, M.J.; de Luis-García, R. Psychological effects of the COVID-19 outbreak and lockdown among students and workers of a Spanish university. Psychiatry Res. 2020, 290, 113108. [Google Scholar] [CrossRef]
- Stanton, R.; To, Q.G.; Khalesi, S.; Williams, S.L.; Alley, S.J.; Thwaite, T.L.; Fenning, A.S.; Vandelanotte, C. Depression, Anxiety and stress during COVID-19: Associations with changes in physical activity, sleep, tobacco and alcohol use in australian adults. Int. J. Environ. Res. Public Health 2020, 17, 4065. [Google Scholar] [CrossRef] [PubMed]
- Jones, C.M.; Guy, G.P.; Board, A. Comparing actual and forecasted numbers of unique patients dispensed select medications for opioid use disorder, opioid overdose reversal, and mental health, during the COVID-19 pandemic, United States, January 2019 to May 2020. Drug Alcohol Depend. 2021, 219, 108486. [Google Scholar] [CrossRef] [PubMed]
- Uthayakumar, S.; Tadrous, M.; Vigod, S.N.; Kitchen, S.A.; Gomes, T. The effects of COVID-19 on the dispensing rates of antidepressants and benzodiazepines in Canada. Depress. Anxiety 2021. [Google Scholar] [CrossRef] [PubMed]
- Armitage, R. Antidepressants, primary care, and adult mental health services in England during COVID-19. Lancet Psychiatry 2021, 8, e3. [Google Scholar] [CrossRef]
- Milani, S.A.; Raji, M.A.; Chen, L.; Kuo, Y.-F. Trends in the Use of Benzodiazepines, Z-Hypnotics, and Serotonergic Drugs among US Women and Men Before and During the COVID-19 Pandemic. JAMA Netw. Open 2021, 4, e2131012. [Google Scholar] [CrossRef]
- Stall, N.M.; Zipursky, J.S.; Rangrej, J.; Jones, A.; Costa, A.P.; Hillmer, M.P.; Brown, K. Assessment of Psychotropic Drug Prescribing Among Nursing Home Residents in Ontario, Canada, During the COVID-19 Pandemic. JAMA Intern. Med. 2021, 181, 861. [Google Scholar] [CrossRef]
- De Oliveira Costa, J.; Gillies, M.B.; Schaffer, A.L.; Peiris, D.; Zoega, H.; Pearson, S. Changes in antidepressant use in Australia: A nationwide analysis prior to and during the COVID-19 pandemic. MedRxiv 2021. [Google Scholar] [CrossRef]
- Carr, M.J.; Steeg, S.; Webb, R.T.; Kapur, N.; Chew-Graham, A.C.; Abel, K.M.; Hope, H.; Pierce, M.; Ashcroft, D.M. Effects of the COVID-19 pandemic on primary care-recorded mental illness and self-harm episodes in the UK: A population-based cohort study. Lancet Public Health 2021, 6, e124–e135. [Google Scholar] [CrossRef]
- Wolfschlag, M.; Grudet, C.; Håkansson, A. Impact of the COVID-19 Pandemic on the General Mental Health in Sweden: No Observed Changes in the Dispensed Amount of Common Psychotropic Medications in the Region of Scania. Front. Psychiatry 2021, 12, 731297. [Google Scholar] [CrossRef]
- Antonazzo, I.C.; Fornari, C.; Paoletti, O.; Bartolini, C.; Conti, S.; Cortesi, P.A.; Mantovani, L.G.; Gini, R.; Mazzaglia, G. COVID-19 Outbreak Impact on Anticoagulants Utilization: An Interrupted Time-Series Analysis Using Health Care Administrative Databases. Thromb. Haemost. 2021, 121, 1115–1118. [Google Scholar] [CrossRef]
- Antonazzo, I.C.; Fornari, C.; Maumus-Robert, S.; Cei, E.; Paoletti, O.; Conti, S.; Cortesi, P.A.; Mantovani, L.G.; Gini, R.; Mazzaglia, G. Impact of COVID-19 Lockdown, during the Two Waves, on Drug Use and Emergency Department Access in People with Epilepsy: An Interrupted Time-Series Analysis. Int. J. Environ. Res. Public Health 2021, 24, 13253. [Google Scholar] [CrossRef] [PubMed]
- Trifirò, G.; Gini, R.; Barone-Adesi, F.; Beghi, E.; Cantarutti, A.; Capuano, A.; Carnovale, C.; Clavenna, A.; Dellagiovanna, M.; Ferrajolo, C.; et al. The Role of European Healthcare Databases for Post-Marketing Drug Effectiveness, Safety and Value Evaluation: Where Does Italy Stand? Drug Saf. 2019, 42, 347–363. [Google Scholar] [CrossRef] [PubMed]
- Merlo, J.; Wessling, A.; Melander, A. Comparison of dose standard units for drug utilisation studies. Eur. J. Clin. Pharmacol. 1996, 50, 27–30. [Google Scholar] [CrossRef]
- Pazzagli, L.; Brandt, L.; Linder, M.; Myers, D.; Mavros, P.; Andersen, M.; Bahmanyar, S. Methods for constructing treatment episodes and impact on exposure-outcome associations. Eur. J. Clin. Pharmacol. 2019, 76, 267–275. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Italian Office of National Statistics—Istituto Nazionale di Statistica (ISTAT). Available online: https://www.istat.it/ (accessed on 6 June 2021).
- Penfold, R.B.; Zhang, F. Use of Interrupted Time Series Analysis in Evaluating Health Care Quality Improvements. Acad. Pediatr. 2013, 13 (Suppl. S6), S38–S44. [Google Scholar] [CrossRef] [PubMed]
- Kontopantelis, E.; Doran, T.; Springate, D.A.; Buchan, I.; Reeves, D. Regression based quasi-experimental approach when randomisation is not an option: Interrupted time series analysis. BMJ 2015, 350, h2750. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wagner, A.K.; Soumerai, S.B.; Zhang, F.; Ross-Degnan, D. Segmented regression analysis of interrupted time series studies in medication use research. J. Clin. Pharm. Ther. 2002, 27, 299–309. [Google Scholar] [CrossRef]
- Derrick, T.R.; Thomas, J.M. Time Series Analysis: The Cross-Correlation Function. Kinesiology Publications 2004 at Iowa State University Digital Repository. Available online: https://lib.dr.iastate.edu/kin_pubs/46 (accessed on 10 December 2021).
- Rømer, T.B.; Christensen, R.H.B.; Blomberg, S.N.; Folke, F.; Christensen, H.C.; Benros, M.E. Psychiatric Admissions, Referrals, and Suicidal Behavior Before and During the COVID-19 Pandemic in Denmark: A Time-Trend Study. Acta Psychiatr. Scand. 2021, 144, 553–562. [Google Scholar] [CrossRef]
- Abbas, M.J.; Kronenberg, G.; McBride, M.; Chari, D.; Alam, F.; Mukaetova-Ladinska, E.; Al-Uzri, M.; Brugha, T. The Early Impact of the COVID-19 Pandemic on Acute Care Mental Health Services. Psychiatr. Serv. 2021, 72, 242–246. [Google Scholar] [CrossRef]
- Clerici, M.; Durbano, F.; Spinogatti, F.; Vita, A.; De Girolamo, G.; Micciolo, R. Psychiatric hospitalization rates in Italy before and during COVID-19: Did they change? An analysis of register data. Ir. J. Psychol. Med. 2020, 37, 283–290. [Google Scholar] [CrossRef]
- Hansen, J.P.; van Sas, T.Q.B.; Fløjstrup, M.; Brabrand, M.; Hvolby, A. The effect of the March 2020 COVID-19 lockdown on national psychiatric contacts in Denmark: An interrupted time series analysis. Brain Behav. 2021, 11, e2264. [Google Scholar] [CrossRef] [PubMed]
- Balestrieri, M.; Rucci, P.; Amendola, D.; Bonizzoni, M.; Cerveri, G.; Colli, C.; Dragogna, F.; Ducci, G.; Elmo, M.G.; Ghio, L.; et al. Emergency Psychiatric Consultations During and After the COVID-19 Lockdown in Italy. A Multicentre Study. Front. Psychiatry 2021, 12, 697058. [Google Scholar] [CrossRef] [PubMed]
- Golinelli, D.; Boetto, E.; Carullo, G.; Nuzzolese, A.G.; Landini, M.P.; Fantini, M.P. Adoption of Digital Technologies in Health Care During the COVID-19 Pandemic: Systematic Review of Early Scientific Literature. J. Med. Internet Res. 2020, 22, e22280. [Google Scholar] [CrossRef] [PubMed]
- Lima, C.K.T.; Carvalho, P.M.D.M.; Lima, I.D.A.A.S.; Nunes, J.V.A.D.O.; Saraiva, J.S.; de Souza, R.I.; da Silva, C.G.L.; Neto, M.L.R. The emotional impact of Coronavirus 2019-nCoV (new Coronavirus disease). Psychiatry Res. 2020, 287, 112915. [Google Scholar] [CrossRef]
- Yao, H.; Chen, J.-H.; Xu, Y.-F. Patients with mental health disorders in the COVID-19 epidemic. Lancet Psychiatry 2020, 7, e21. [Google Scholar] [CrossRef]
- Pacchiarotti, I.; Anmella, G.; Fico, G.; Verdolini, N.; Vieta, E. A psychiatrist’s perspective from a COVID-19 epicentre: A personal account. BJPsych Open 2020, 6, e108. [Google Scholar] [CrossRef]
- Sim, K.; Chua, H.C.; Vieta, E.; Fernandez, G. The anatomy of panic buying related to the current COVID-19 pandemic. Psychiatry Res. 2020, 288, 113015. [Google Scholar] [CrossRef]
- Fullana, M.A.; Hidalgo-Mazzei, D.; Vieta, E.; Radua, J. Coping behaviors associated with decreased anxiety and depressive symptoms during the COVID-19 pandemic and lockdown. J. Affect. Disord. 2020, 275, 80–81. [Google Scholar] [CrossRef]
- Kozloff, N.; Mulsant, B.H.; Stergiopoulos, V.; Voineskos, A.N. The COVID-19 Global Pandemic: Implications for People with Schizophrenia and Related Disorders. Schizophr. Bull. 2020, 46, 752–757. [Google Scholar] [CrossRef]
- Claassen, C.A.; Carmody, T.; Stewart, S.M.; Bossarte, R.M.; Larkin, G.L.; Woodward, W.A.; Trivedi, M.H. Effect of 11 September 2001 terrorist attacks in the USA on suicide in areas surrounding the crash sites. Br. J. Psychiatry 2010, 196, 359–364. [Google Scholar] [CrossRef] [Green Version]
- Osman, M.; Parnell, A.C. Effect of the First World War on suicide rates in Ireland: An investigation of the 1864–1921 suicide trends. BJPsych Open 2015, 1, 164–165. [Google Scholar] [CrossRef] [Green Version]
- Batty, G.; Kivimäki, M.; Bell, S.; Gale, C.R.; Shipley, M.; Whitley, E.; Gunnell, D. Psychosocial characteristics as potential predictors of suicide in adults: An overview of the evidence with new results from prospective cohort studies. Transl. Psychiatry 2018, 8, 22. [Google Scholar] [CrossRef] [Green Version]
- Cobo, A.; Porras-Segovia, A.; Pérez-Rodríguez, M.M.; Artés-Rodríguez, A.; Barrigón, M.L.; Courtet, P.; Baca-García, E. Patients at high risk of suicide before and during a COVID-19 lockdown: Ecological momentary assessment study. BJPsych Open 2021, 7, e82. [Google Scholar] [CrossRef]
- Boldrini, T.; Girardi, P.; Clerici, M.; Conca, A.; Creati, C.; Di Cicilia, G.; Ducci, G.; Durbano, F.; Maci, C.; Maone, A.; et al. Consequences of the COVID-19 pandemic on admissions to general hospital psychiatric wards in Italy: Reduced psychiatric hospitalizations and increased suicidality. Prog. Neuro-Psychopharmacol. Biol. Psychiatry 2021, 110, 110304. [Google Scholar] [CrossRef]
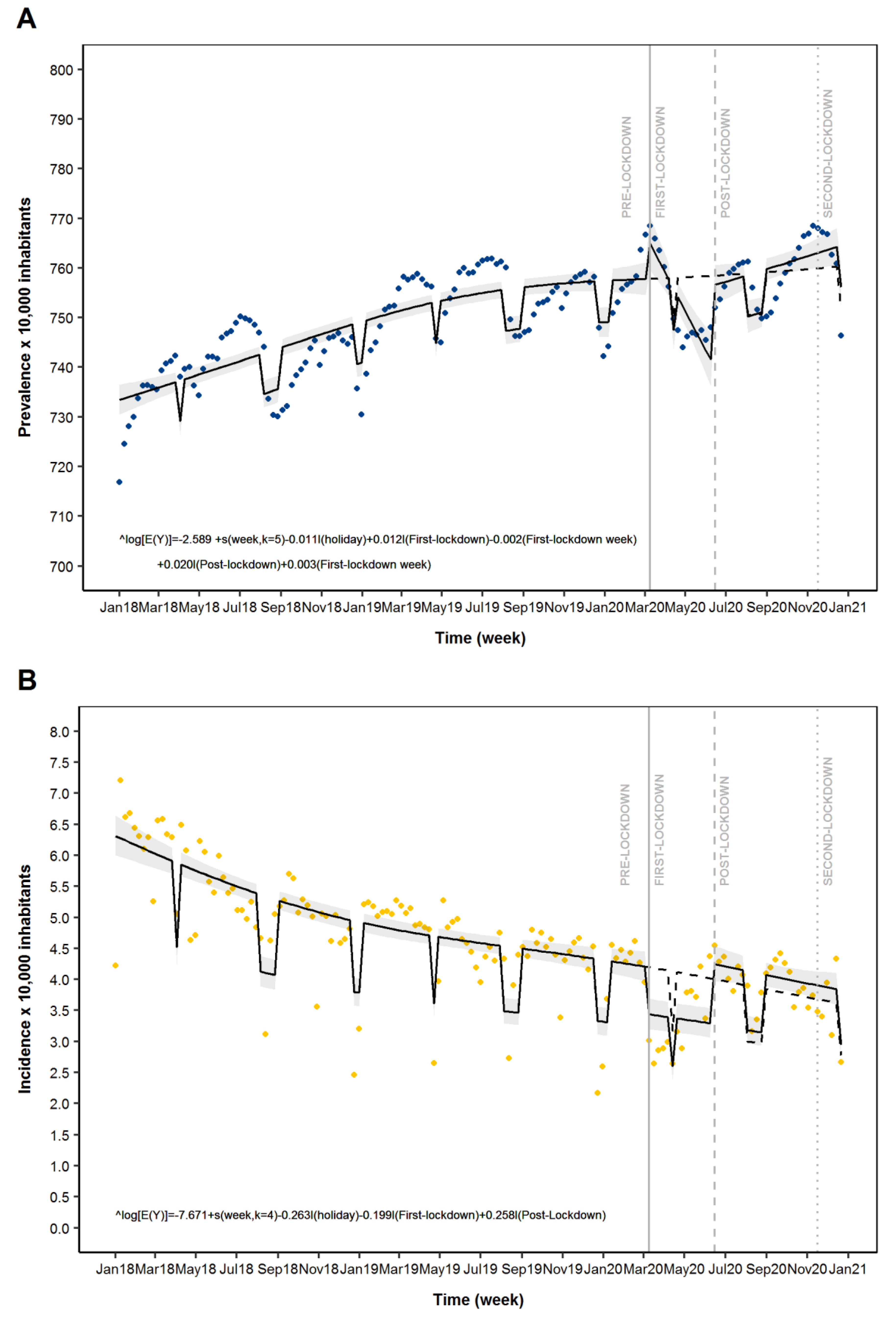
| Prevalence of AD Drug Use | ||||
|---|---|---|---|---|
| Model Parameter 1 | β | Prevalence Ratio | 95% CI | p-Value |
| First Lockdown (1st week) 3 | 0.012 | 1.012 | 1.003–1.021 | <0.05 |
| First Lockdown (1st week) 4 | −0.002 | 0.998 | 0.997–0.999 | <0.001 |
| Post-First Lockdown (1st week) 3 | 0.020 | 1.020 | 1.011–1.029 | <0.001 |
| Post-First Lockdown (1st week) 4 | 0.003 | 1.003 | 1.002–1.004 | <0.001 |
| Incidence of AD Drug Use | ||||
| Model Parameter 2 | β | Incidence Ratio | 95% CI | p-Value |
| First Lockdown (1st week) 3 | −0.199 | 0.819 | 0.742–0.905 | <0.001 |
| Post-First Lockdown (1th week) 3 | 0.258 | 1.295 | 1.160–1.445 | <0.001 |
| Pre-Lockdown | First-Lockdown | Post-First Lockdown | Second-Lockdown | |
|---|---|---|---|---|
| Number of weeks | 114 | 14 | 22 | 6 |
| Number of patients | 175,563 | 14,684 | 27,695 | 6631 |
| Sex, N (%) | ||||
| Female | 112,024 (63.8) | 8770 (59.7) | 17,445 (63.0) | 4109 (62.0) |
| Male | 63,539 (36.2) | 5914 (40.3) | 10,250 (37.0) | 2522 (38.0) |
| Age, N (%) | ||||
| 18–29 | 10,315 (5.9) | 898 (6.1) | 1708 (6.2) | 483 (7.3) |
| 30–39 | 13,121 (7.5) | 998 (6.8) | 1825 (6.6) | 490 (7.4) |
| 40–49 | 23,245 (13.2) | 1807 (12.3) | 3285 (11.9) | 840 (12.7) |
| 50–59 | 28,598 (16.3) | 2374 (16.2) | 4184 (15.1) | 1072 (16.2) |
| 60–69 | 25,413 (14.5) | 2169 (14.8) | 4039 (14.6) | 988 (14.9) |
| 70–79 | 33,020 (18.8) | 2689 (18.3) | 5361 (19.4) | 1168 (17.6) |
| 80+ | 41,851 (23.8) | 3749 (25.5) | 7293 (26.3) | 1590 (24) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Antonazzo, I.C.; Fornari, C.; Maumus-Robert, S.; Cei, E.; Paoletti, O.; Ferrara, P.; Conti, S.; Cortesi, P.A.; Mantovani, L.G.; Gini, R.; et al. Antidepressants Drug Use during COVID-19 Waves in the Tuscan General Population: An Interrupted Time-Series Analysis. J. Pers. Med. 2022, 12, 178. https://doi.org/10.3390/jpm12020178
Antonazzo IC, Fornari C, Maumus-Robert S, Cei E, Paoletti O, Ferrara P, Conti S, Cortesi PA, Mantovani LG, Gini R, et al. Antidepressants Drug Use during COVID-19 Waves in the Tuscan General Population: An Interrupted Time-Series Analysis. Journal of Personalized Medicine. 2022; 12(2):178. https://doi.org/10.3390/jpm12020178
Chicago/Turabian StyleAntonazzo, Ippazio Cosimo, Carla Fornari, Sandy Maumus-Robert, Eleonora Cei, Olga Paoletti, Pietro Ferrara, Sara Conti, Paolo Angelo Cortesi, Lorenzo Giovanni Mantovani, Rosa Gini, and et al. 2022. "Antidepressants Drug Use during COVID-19 Waves in the Tuscan General Population: An Interrupted Time-Series Analysis" Journal of Personalized Medicine 12, no. 2: 178. https://doi.org/10.3390/jpm12020178
APA StyleAntonazzo, I. C., Fornari, C., Maumus-Robert, S., Cei, E., Paoletti, O., Ferrara, P., Conti, S., Cortesi, P. A., Mantovani, L. G., Gini, R., & Mazzaglia, G. (2022). Antidepressants Drug Use during COVID-19 Waves in the Tuscan General Population: An Interrupted Time-Series Analysis. Journal of Personalized Medicine, 12(2), 178. https://doi.org/10.3390/jpm12020178










