Chronic Kidney Disease and Its Relationship with Mental Health: Allostatic Load Perspective for Integrated Care
Abstract
1. Introduction
2. Materials and Methods
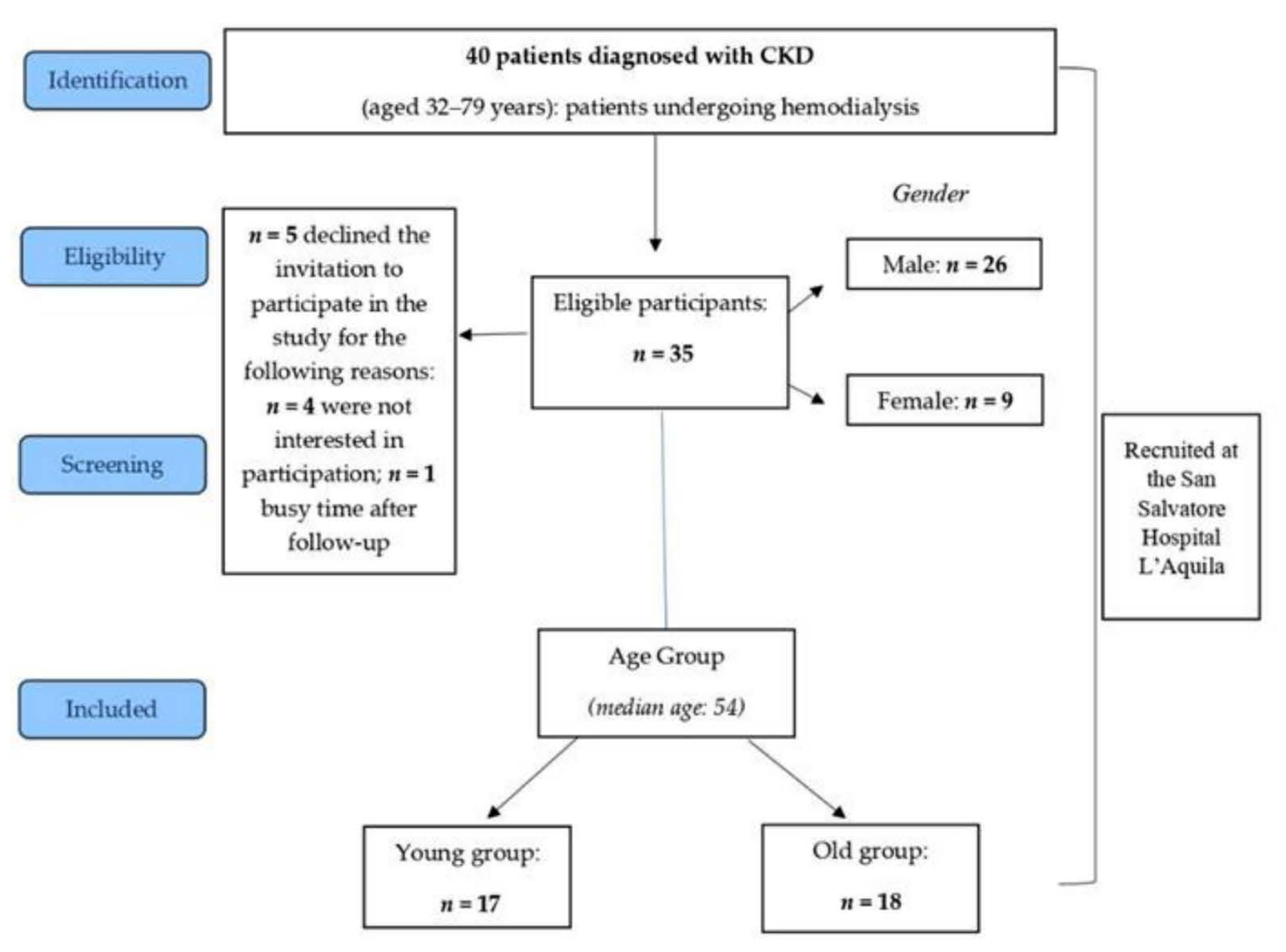
2.1. Participants
2.2. Procedure
2.3. Measures
2.3.1. Sociodemographic Variables
2.3.2. Psychological Measurement
2.4. Study Design
2.5. Statistical Analysis
3. Results
3.1. Correlation among the Study Variables
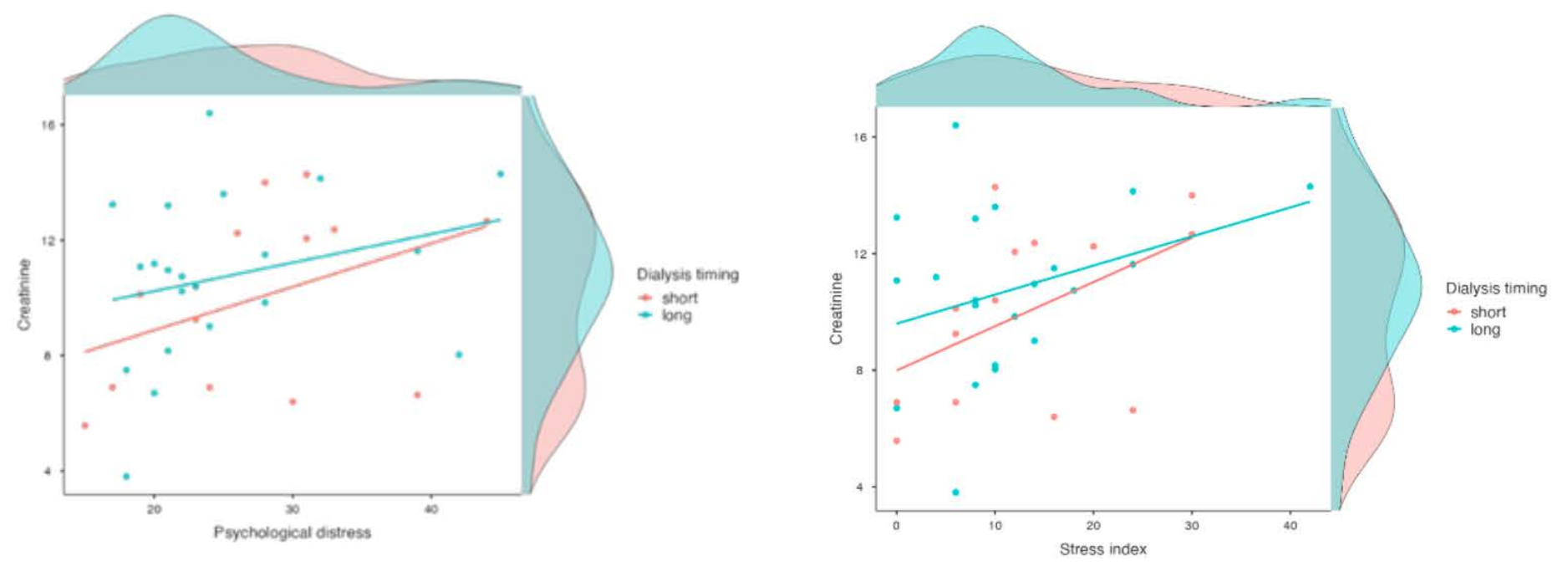
3.2. Testing Direct Effects and Moderating Effects
4. Discussion and Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Saran, R.; Robinson, B.; Abbott, K.C.; Bragg-Gresham, J.; Chen, X.; Gipson, D.; Gu, H.; Hirth, R.A.; Hutton, D.; Jin, Y.; et al. US Renal Data System 2019 Annual Data Report: Epidemiology of Kidney Disease in the United States. Am. J. Kidney Dis. 2020, 75, A6–A7. [Google Scholar] [CrossRef] [PubMed]
- Dziubek, W.; Kowalska, J.; Kusztal, M.; Rogowski, Ł.; Gołębiowski, T.; Nikifur, M.; Szczepańska-Gieracha, J.; Zembroń-Łacny, A.; Klinger, M.; Woźniewski, M. The Level of Anxiety and Depression in Dialysis Patients Undertaking Regular Physical Exercise Training—A Preliminary Study. Kidney Blood Press. Res. 2016, 41, 86–98. [Google Scholar] [CrossRef] [PubMed]
- Mollahadi, M.; Tayyebi, A.; Ebadi, A.; Daneshmandi, M. Comparison of anxiety, depression and stress among hemodialysis and kidney transplantation patients. Iran. J. Crit. Care Nurs. Winter 2010, 2, 153–156. [Google Scholar]
- Navidian, A.; Arbabisarjou, A.; Kikhai, A. Frequency of mental disturbances in hemodialysis patients referred to hemodialysis ward of Khatam-Al-Anbia hospital in Zahedan. J. Guilan Univ. Med. Sci. 2006, 15, 61. [Google Scholar]
- Heidarigorji, A.; Davanloo, A.A. The efficacy of relaxation training on stress, anxiety, and pain perception in hemodialysis patients. Indian J. Nephrol. 2014, 24, 356–361. [Google Scholar] [CrossRef] [PubMed]
- van Sandwijk, M.S.; Al Arashi, D.; van de Hare, F.M.; van der Torren, J.M.R.; Kersten, M.-J.; A Bijlsma, J.; Berge, I.J.M.T.; Bemelman, F.J. Fatigue, anxiety, depression and quality of life in kidney transplant recipients, haemodialysis patients, patients with a haematological malignancy and healthy controls. Nephrol. Dial. Transplant. 2018, 34, 833–838. [Google Scholar] [CrossRef] [PubMed]
- Silva, A.; Moratelli, L.; Costa, A.; Carminatti, M.; Bastos, M.; Colugnati, F.; Grincenkov, F.; Sanders-Pinheiro, H. Waiting for a Kidney Transplant: Association with Anxiety and Stress. Transplant. Proc. 2014, 46, 1695–1697. [Google Scholar] [CrossRef] [PubMed]
- Dąbrowska-Bender, M.; Dykowska, G.; Żuk, W.; Milewska, M.; Staniszewska, A. The impact on quality of life of dialysis patients with renal insufficiency. Patient Prefer. Adherence 2018, 12, 577–583. [Google Scholar] [CrossRef] [PubMed]
- Thomas, C.V.; de Castro, E.K.; Antonello, I.C.F. Personality traits and clinical/biochemical course in the first year after kidney transplant. Ren. Fail. 2016, 38, 1383–1390. [Google Scholar] [CrossRef][Green Version]
- Guerra, F.; Ranieri, J.; Passafiume, D.; Lupi, D.; Maccarone, D.; Pisani, F.; Ferri, C.; Di Giacomo, D. Psychosomatic interactions in kidney transplantation: Role of personality dimensions in mental health-related quality of life. Ther. Adv. Chronic Dis. 2021, 12, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Dobbels, F.; Vanhaecke, J.; Dupont, L.; Nevens, F.; Verleden, G.; Pirenne, J.; De Geest, J. Pretransplant predictors of posttransplant adherence and clinical outcome: An evidence base for pretransplant psychosocial screening. Transplantation 2009, 87, 1497–1504. [Google Scholar] [CrossRef] [PubMed]
- Bogg, T.; Roberts, B.W. Conscientiousness and health-related behaviours: A meta-analysis of the leading behavioural contributors to mortality. Psychol. Bull. 2004, 130, 887–919. [Google Scholar] [CrossRef] [PubMed]
- Kidachi, R.; Kikuchi, A.; Nishizawa, Y.; Hiruma, T.; Kaneko, S. Personality types and coping style in hemodialysis patients. Psychiatry Clin. Neurosci. 2007, 61, 339–347. [Google Scholar] [CrossRef] [PubMed]
- McEwen, B.S.; Stellar, E. Stress and the individual. Mechanisms leading to disease. Arch. Intern. Med. 1993, 153, 2093–2101. [Google Scholar] [CrossRef] [PubMed]
- Guidi, J.; Lucente, M.; Sonino, N.; Fava, G.A. Allostatic Load and Its Impact on Health: A Systematic Review. Psychother. Psychosom. 2020, 90, 11–27. [Google Scholar] [CrossRef] [PubMed]
- Bottesi, G.; Ghisi, M.; Alto, G.; Conforti, E.; Melli, G.; Sica, C. The Italian version of the depression anxiety stress scales-21: Factor structure and psychometric properties on community and clinical samples. Compr. Psychiatry 2015, 60, 170–181. [Google Scholar] [CrossRef] [PubMed]
- Morasso, G.; Costantini, M.; Baracco, G.; Borreani, C.; Capelli, M. Assessing Psychological Distress in Cancer Patients: Validation of a Self-Administered Questionnaire. Oncology 1996, 53, 295–302. [Google Scholar] [CrossRef] [PubMed]
- Guido, G.; Peluso, A.M.; Capestro, M.; Miglietta, M. An Italian version of the 10-item Big Five Inventory: An application to hedonic and utilitarian shopping values. Pers. Individ. Differ. 2015, 76, 135–140. [Google Scholar] [CrossRef]
| DT (n = 35) | |
|---|---|
| Age (years) | X55.4 SD ± 11.32 |
| Age groups: n (%) | |
| ≤54 years | 17 (48.57) |
| >54 years | 18 (51.43) |
| Gender: n (%) | |
| Male | 26 (74.3) |
| Female | 9 (25.7) |
| Marital status: n (%) | |
| Single | 9 (25.7) |
| Married | 26 (74.3) |
| Educational level: n (%) | |
| High school graduate | 18 (51.43) |
| No graduate | 17 (48.57) |
| Occupational status: n (%) | |
| Unemployed | 21 (60.00) |
| Employed | 14 (40.00) |
| DT | Total | |
|---|---|---|
| x SD | x SD | |
| PDI | 26.1 ± 7.9 | 25.7 ± 9.4 |
| DASS-21 | ||
| Depression | 9.03 ± 9.4 | 8.43 ± 10.2 |
| Anxiety | 8.46 ± 6.3 | 9.31 ± 8.3 |
| Stress | 12.2 ± 9.6 | 12.0 ± 9.6 |
| BFI-10 | ||
| Ag | 6.51 ± 1.99 | 6.26 ± 1.9 |
| Co | 7.66 ± 2.1 | 7.41 ± 2.1 |
| Es | 5.69 ± 1.4 | 5.73 ± 1.6 |
| Ex | 6.49 ± 2.1 | 6.44 ± 2.0 |
| Op | 6.83 ± 2.2 | 6.71 ± 2.1 |
| Statistic | df | p | Mean Difference | Effect Size | |||
|---|---|---|---|---|---|---|---|
| PDI index | Student’s t | 19.30 | 34.00 | <0.0001 | 26.06 | Cohen’s d | 3.26 |
| Depression | Student’s t | 5.63 | 34.00 | <0.0001 | 9.03 | Cohen’s d | 0.95 |
| Anxiety | Student’s t | 7.84 | 34.00 | <0.0001 | 8.46 | Cohen’s d | 1.33 |
| Stress | Student’s t | 7.46 | 34.00 | <0.0001 | 12.17 | Cohen’s d | 1.26 |
| Creatinine | Distress | Depression | Anxiety | Stress | Time of Dialysis | Age | Time from Diagnosis | ||
|---|---|---|---|---|---|---|---|---|---|
| Creatinine | Spearman’s rho | ||||||||
| p-value | |||||||||
| Distress | Spearman’s rho | 0.39 | |||||||
| p-value | 0.0199 | ||||||||
| Depression | Spearman’s rho | 0.20 | 0.78 | ||||||
| p-value | 0.2441 | <0.0001 | |||||||
| Anxiety | Spearman’s rho | 0.01 | 0.55 | 0.78 | |||||
| p-value | 0.9619 | 0.0006 | <0.0001 | ||||||
| Stress | Spearman’s rho | 0.36 | 0.80 | 0.75 | 0.63 | ||||
| p-value | 0.0352 | <0.0001 | <0.0001 | <0.0001 | |||||
| Time of Dialysis | Spearman’s rho | −0.05 | −0.19 | −0.02 | −0.07 | −0.15 | |||
| p-value | 0.7965 | 0.2761 | 0.8937 | 0.6756 | 0.4005 | ||||
| Age | Spearman’s rho | −0.14 | −0.05 | 0.05 | 0.09 | 0.13 | 0.25 | ||
| p-value | 0.4209 | 0.7569 | 0.7712 | 0.6250 | 0.4637 | 0.1472 | |||
| Time from diagnosis | Spearman’s rho | 0.09 | 0.09 | 0.17 | −0.01 | 0.05 | 0.38 | −0.11 | |
| p-value | 0.5957 | 0.5876 | 0.3162 | 0.9735 | 0.7912 | 0.0253 | 0.5187 |
| Overall Model Test | ||||||
|---|---|---|---|---|---|---|
| Model | R2 | Adjusted R2 | F | df1 | df2 | p |
| 1 | 0.14 | 0.12 | 5.59 | 1 | 33 | 0.0241 |
| 2 | 0.16 | 0.11 | 3.11 | 2 | 33 | 0.0584 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Guerra, F.; Di Giacomo, D.; Ranieri, J.; Tunno, M.; Piscitani, L.; Ferri, C. Chronic Kidney Disease and Its Relationship with Mental Health: Allostatic Load Perspective for Integrated Care. J. Pers. Med. 2021, 11, 1367. https://doi.org/10.3390/jpm11121367
Guerra F, Di Giacomo D, Ranieri J, Tunno M, Piscitani L, Ferri C. Chronic Kidney Disease and Its Relationship with Mental Health: Allostatic Load Perspective for Integrated Care. Journal of Personalized Medicine. 2021; 11(12):1367. https://doi.org/10.3390/jpm11121367
Chicago/Turabian StyleGuerra, Federica, Dina Di Giacomo, Jessica Ranieri, Marilena Tunno, Luca Piscitani, and Claudio Ferri. 2021. "Chronic Kidney Disease and Its Relationship with Mental Health: Allostatic Load Perspective for Integrated Care" Journal of Personalized Medicine 11, no. 12: 1367. https://doi.org/10.3390/jpm11121367
APA StyleGuerra, F., Di Giacomo, D., Ranieri, J., Tunno, M., Piscitani, L., & Ferri, C. (2021). Chronic Kidney Disease and Its Relationship with Mental Health: Allostatic Load Perspective for Integrated Care. Journal of Personalized Medicine, 11(12), 1367. https://doi.org/10.3390/jpm11121367







