Functional Profile of Older Adults Hospitalized in Convalescence Units of the National Network of Integrated Continuous Care of Portugal: A Longitudinal Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Type and Sample
2.2. Instrument
2.3. Data Collection
2.4. Statistical Analysis
2.5. Ethical Procedures
3. Results
3.1. Sociodemographic and Clinical Characteristics
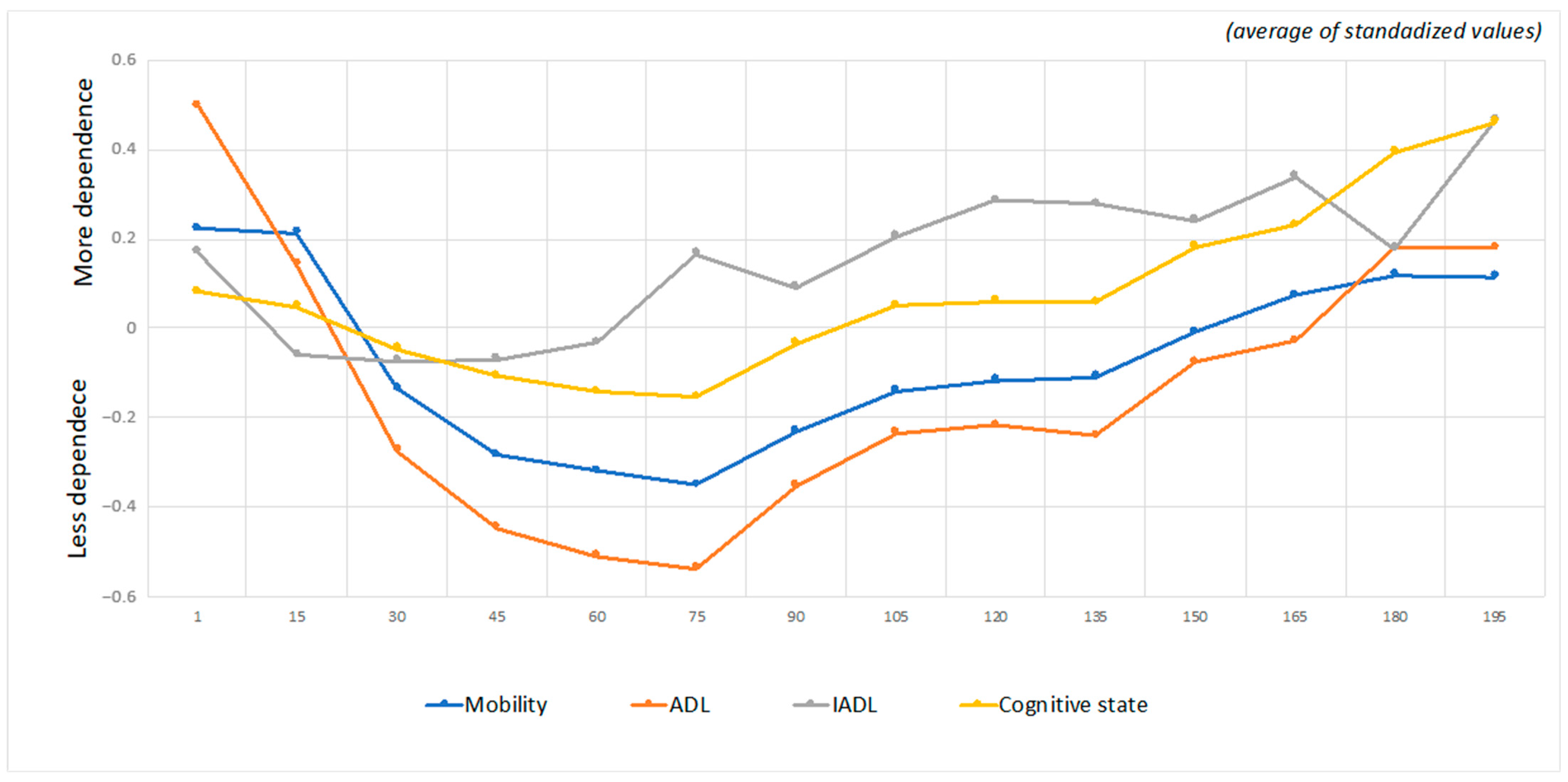
3.2. Evolution of the Functional Profile during Hospitalization
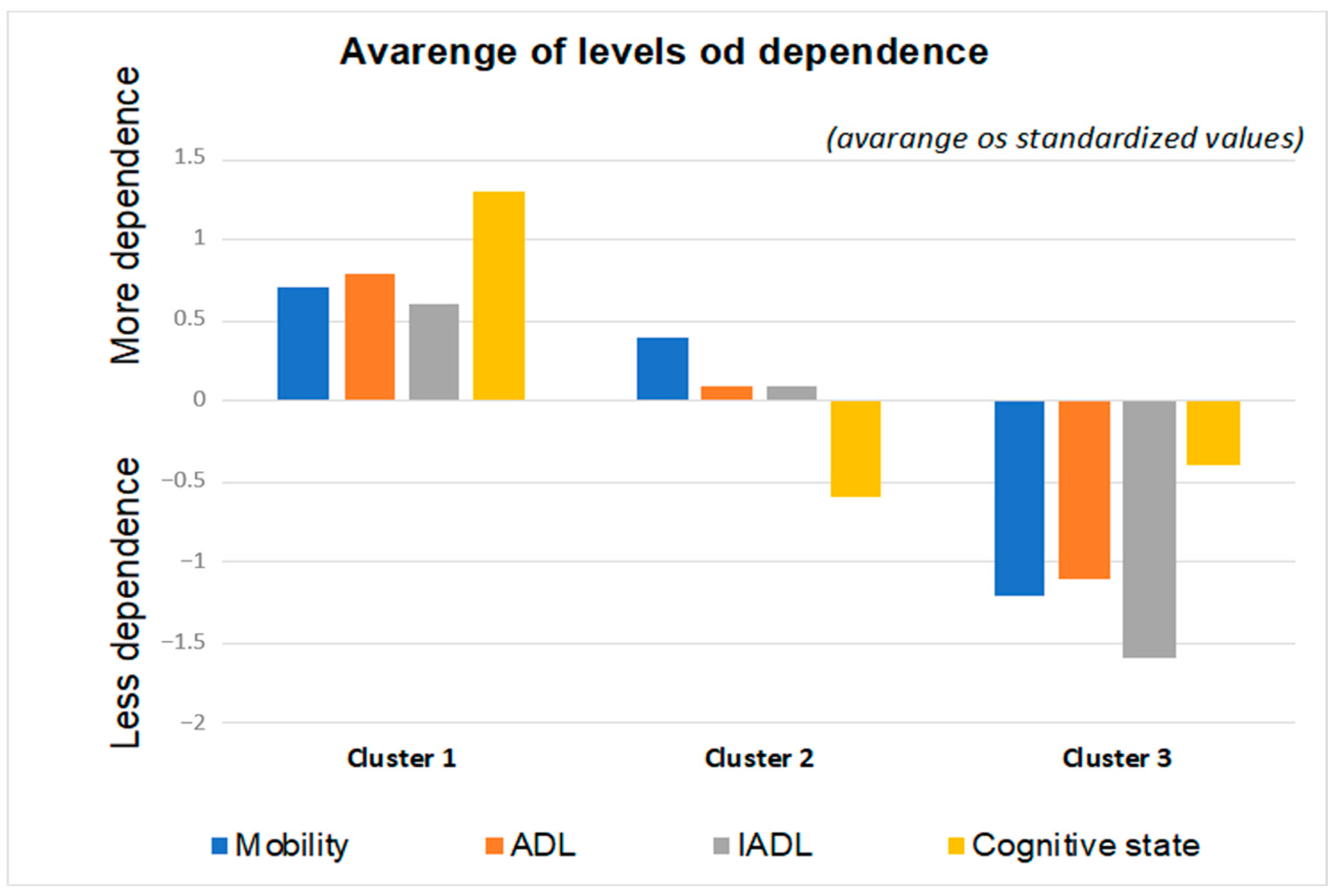
3.3. Dependence Clusters
- (1)
- Cluster 1: Older adults with a higher degree of dependence (severe/complete self-care deficit);
- (2)
- Cluster 2: Older adults with an intermediate degree of dependence (moderate self-care deficit);
- (3)
- Cluster 3: Older adults with a lower degree of dependence (mild self-care deficit).
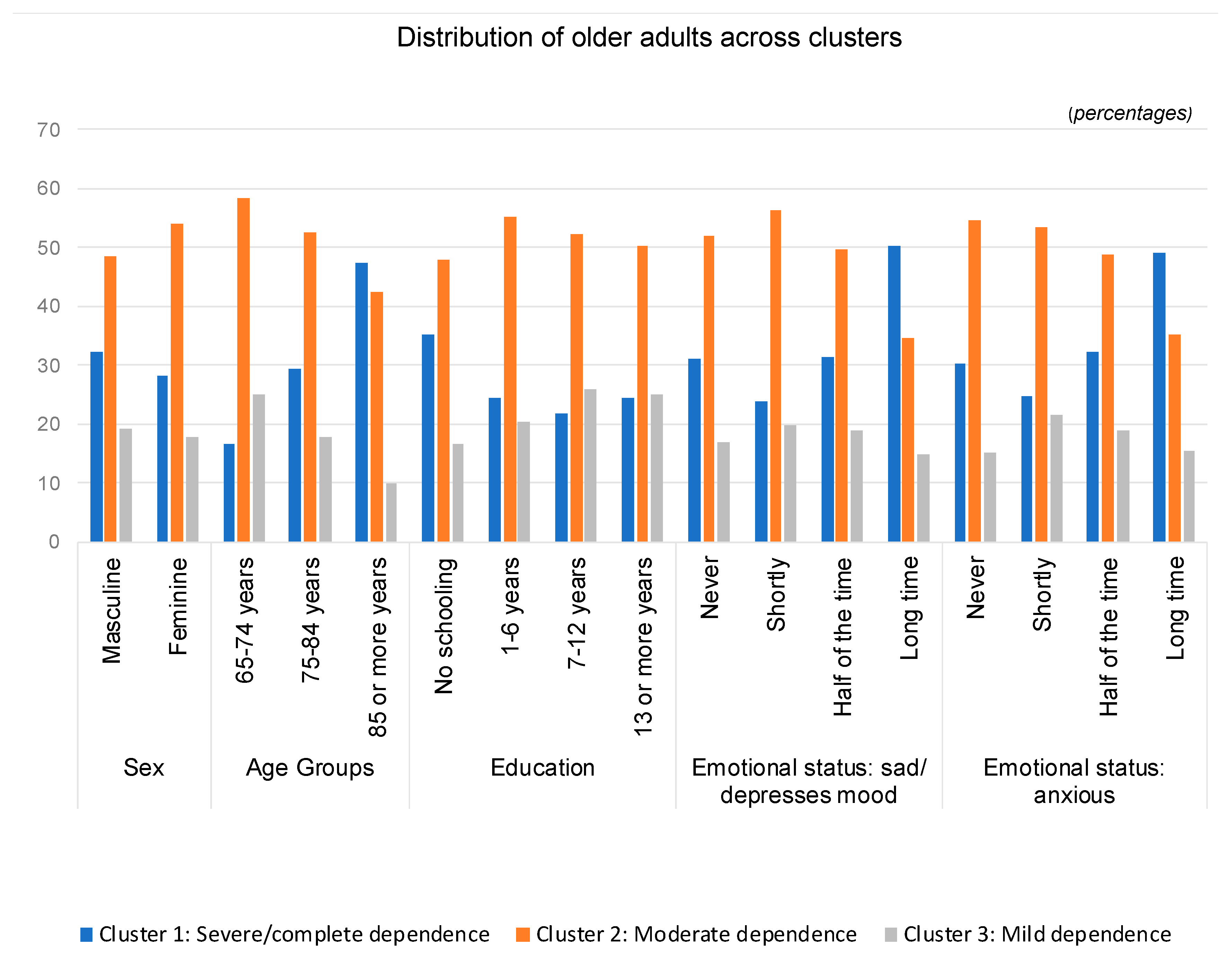
- (1)
- Cluster 1 (severe/complete dependence) is composed of a higher percentage of males, aged 85 years or older, older adults who did not attend school and who have been feeling depressed and anxious for a long time;
- (2)
- Cluster 2 (moderate dependence) encompasses a greater percentage of females, aged between 65 and 84 years, with 1 to 6 years of education and who have felt sad or anxious for a short time;
- (3)
- Cluster 3 (mild dependence) is predominantly composed of males aged 65 to 74 years, with more years of schooling (7 or more) and who feel depressed or anxious for a short time.
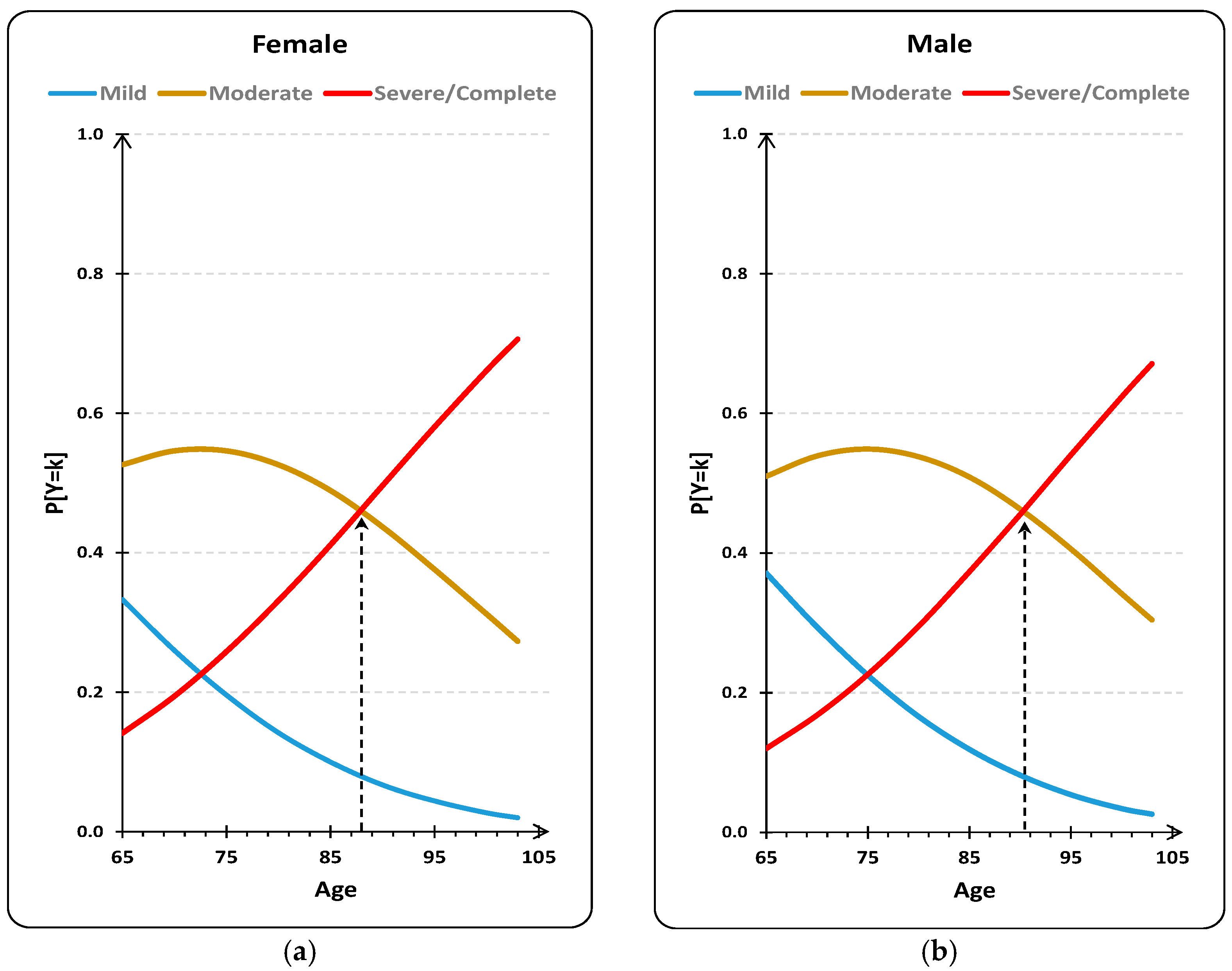
3.4. Degree of Dependence as a Function of Age and Sex
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- European Pathway Association. Care Pathways. 2019. Available online: http://e-p-a.org/care-pathways/ (accessed on 31 July 2021).
- Lopes, M.J. Desafios de Inovação em Saúde: Repensar os Modelos de Cuidados; Universidade de Évora: Évora, Portugal, 2021. [Google Scholar]
- World Health Organization. Integrated Care Models: An Overview: WHO Regional Office for Europe; World Health Organization, Ed.; World Health Organization: Geneva, Switzerland, 2016; Available online: https://www.euro.who.int/en/health-topics/Health-systems/health-services-delivery/publications/2016/integrated-care-models-an-overview-2016 (accessed on 31 July 2021).
- Goddard, M.; Mason, A.R. Integrated Care: A Pill for All Ills? Int. J. Health Policy Manag. 2016, 6, 1–3. [Google Scholar] [CrossRef]
- Hopman, P.; de Bruin, S.R.; Forjaz, M.J.; Rodriguez-Blazquez, C.; Tonnara, G.; Lemmens, L.C.; Onder, G.; Baan, C.A.; Rijken, M. Effectiveness of comprehensive care programs for patients with multiple chronic conditions or frailty: A systematic literature review. Health Policy 2016, 120, 818–832. [Google Scholar] [CrossRef]
- Agerholm, J.; de Leon, A.P.; Schön, P.; Burström, B. Impact of Integrated Care on the Rate of Hospitalization for Ambulatory Care Sensitive Conditions among Older Adults in Stockholm County: An Interrupted Time Series Analysis. Int. J. Integr. Care 2021, 21, 22. [Google Scholar] [CrossRef]
- Fanciullo, G.J.; Washington, T. Best practices to reduce the risk of drug-drug interactions: Opportunities for managed care. Am. J. Manag. Care 2011, 17 (Suppl. 1), S299–S304. [Google Scholar]
- Baxter, S.; Johnson, M.; Chambers, D.; Sutton, A.; Goyder, E.; Booth, A. The effects of integrated care: A systematic review of UK and international evidence. BMC Health Serv. Res. 2018, 18, 350. [Google Scholar] [CrossRef]
- Pereira, C.; Fonseca, C.; Pinho, L. A Rede Nacional de Cuidados Continuados Integrados em Portugal. In Os Cuidados de Saúde Face Aos Desafios do Nosso Tempo: Contributos para a Gestão da Mudança; Lopes, M., Sakellaridesm, C., Eds.; Universidade de Évora: Évora, Portugal, 2021; pp. 36–47. [Google Scholar]
- World Health Organization. The International Classification of Functioning, Disability and Health (ICF); World Health Organization, Ed.; World Health Organization: Geneva, Switzerland, 2001. [Google Scholar]
- Morgado, B.; Fonseca, C.; Lopes, M.; Pinho, L. Components of Care Models that Influence Functionality in People Over 65 in the Context of Long-Term Care: Integrative Literature Review BT Gerontechnology III; García-Alonso, J., Fonseca, C., Eds.; Springer International Publishing: Cham, Switzerland, 2021; pp. 324–335. [Google Scholar]
- Lesende, I.M.; Crespo, L.I.M.; Manzanares, S.C.; Otter, A.-S.D.; Bilbao, I.G.; Rodríguez, J.P.; Pérez, I.N.; Azcoaga, I.S.; Fernández, M.J.D.L.R. Functional decline and associated factors in patients with multimorbidity at 8 months of follow-up in primary care: The functionality in pluripathological patients (FUNCIPLUR) longitudinal descriptive study. BMJ Open 2018, 8, e022377. [Google Scholar] [CrossRef] [PubMed]
- Narasimhan, M.; Kapila, M. Implications of self- care for health service provision. Bull. World Health Organ 2019, 97, 76A. [Google Scholar] [CrossRef] [PubMed]
- Romeyke, T.; Stummer, H. Clinical pathways as instruments for risk and cost management in hospitals—A discussion paper. Glob. J. Health Sci. 2012, 4, 50–59. [Google Scholar] [CrossRef][Green Version]
- Narasimhan, M.; Allotey, P.; Hardon, A. Self care interventions to advance health and wellbeing: A conceptual framework to inform normative guidance. BMJ 2019, 365, l688. [Google Scholar] [CrossRef]
- Romeyke, T.; Noehammer, E.; Stummer, H. Ensuring Quality in Interdisciplinary Inpatient Chronic Care. SAGE Open 2020, 10, 1–10. [Google Scholar] [CrossRef]
- Ramos, A.; Lopes, M.; Fonseca, C.; Henriques, A. Sociodemographic Profile of People Aged 65 or Over in Long-Term Care in Portugal: Analysis of a Big Data. In Gerontechnology III. IWoG 2020. Lecture Notes in Bioengineering; García-Alonso, J., Fonseca, C., Eds.; Springer: Cham, Switzerland, 2021; pp. 438–446. Available online: https://doi.org/10.1007/978-3-030-72567-9_40 (accessed on 31 July 2021). [CrossRef]
- Ramos, A.; Fonseca, C.; Henriques, A. Developing and Managing Health Systems and Organizations for an Aging Society. In Handbook of Research on Health Systems and Organizations for an Aging Society; Fonseca, C., Mendes, D., Mendes, F., García-Alonso, J., Eds.; IGI Global: Hershey, PA, USA, 2020; pp. 62–68. [Google Scholar] [CrossRef]
- World Health Organization. Decade of Healthy Ageing: Baseline Report; World Health Organization: Geneva, Switzerland, 2020; Available online: https://www.who.int/publications/i/item/9789240017900 (accessed on 31 July 2021).
- Brites, R. Análise de Dados com IBM SPSS®: Mix Essencial para Relatórios Profissionais e Teses Académicas, Módulo I—Básico; ISEG, Ed.; ISEG: Lisboa, Portugal, 2015. [Google Scholar]
- Marôco, J. Análise Estatística com o SPSS Statistics v18–v27, 8th ed.; Pêro Pinheiro: Lisboa, Portugal, 2021. [Google Scholar]
- Lafont, C.; Gérard, S.; Voisin, T.; Pahor, M.; Vellas, B. Reducing “iatrogenic disability” in the hospitalized frail elderly. J. Nutr. Health Aging 2011, 15, 645–660. [Google Scholar] [CrossRef] [PubMed]
- Cuevas-Lara, C.; Izquierdo, M.; de Asteasu, M.L.S.; Ramírez-Vélez, R.; Zambom-Ferraresi, F.; Zambom-Ferraresi, F.; Martínez-Velilla, N. Impact of Game-Based Interventions on Health-Related Outcomes in Hospitalized Older Patients: A Systematic Review. J. Am. Med Dir. Assoc. 2021, 22, 364–371. [Google Scholar] [CrossRef] [PubMed]
- Gill, T.M.; Allore, H.G.; Gahbauer, E.A.; Murphy, T.E. Change in disability after hospitalization or restricted activity in older persons. JAMA 2010, 304, 1919–1928. [Google Scholar] [CrossRef]
- Luchetti, M.; Cutti, A.G.; Verni, G.; Sacchetti, R.; Rossi, N. Impact of Michelangelo prosthetic hand: Findings from a crossover longitudinal study. J. Rehabil Res. Dev. 2015, 52, 605–618. [Google Scholar] [CrossRef]
- Fonseca, C.; de Pinho, L.G.; Lopes, M.J.; Marques, M.D.C.; Garcia-Alonso, J. The Elderly Nursing Core Set and the cognition of Portuguese older adults: A cross-sectional study. BMC Nurs 2021, 20, 108. [Google Scholar] [CrossRef]
- Rodrigues, M.A.P.; Facchini, L.A.; Thumé, E.; Maia, F. Gender and incidence of functional disability in the elderly: A systematic review. Cad. Saude Publica 2009, 25 (Suppl. 3), S464–S476. [Google Scholar] [CrossRef]
- Lopes, M.J.; Pinho, L.G.; de Fonseca, C.; Goes, M.; Oliveira, H.; Garcia-Alonso, J.; Afonso, A. Functioning and Cognition of Portuguese Older Adults Attending in Residential Homes and Day Centers: A Comparative Study. Int. J. Environ. Res. Public Health 2021, 18, 7030. [Google Scholar] [CrossRef]
- Serrano-Alarcón, M.; Perelman, J. Ageing under unequal circumstances: A cross-sectional analysis of the gender and socioeconomic patterning of functional limitations among the Southern European elderly. Int. J. Equity Health 2017, 16, 175. [Google Scholar] [CrossRef]
- Lee, J.; Meijer, E.; Phillips, D.; Hu, P. Disability Incidence Rates for Men and Women in 23 Countries: Evidence on Health Effects of Gender Inequality. J. Gerontol. A Biol. Sci. Med. Sci. 2021, 76, 328–338. [Google Scholar] [CrossRef] [PubMed]
- Schmitz, A.; Lazarevič, P. The gender health gap in Europe’s ageing societies: Universal findings across countries and age groups? Eur. J. Ageing 2020, 17, 509–520. [Google Scholar] [CrossRef] [PubMed]
- Coutinho, A.T.D.Q.; Vilela, M.B.R.; Lima, M.L.L.T.D.; Silva, V.D.L. Social communication and functional independence of the elderly in a community assisted by the family health strategy. Rev. CEFAC 2018, 20, 363–373. [Google Scholar] [CrossRef]
- Abalo, E.M.; Mensah, C.M.; Agyemang-Duah, W.; Peprah, P.; Budu, H.I.; Gyasi, R.M.; Donkor, P.; Amoako, J. Geographical Differences in Perceived Health Status Among Older Adults in Ghana: Do Gender and Educational Status Matter? Gerontol. Geriatr. Med. 2018, 4, 2333721418796663. [Google Scholar] [CrossRef]
- Cui, S.; Wang, R.; Lu, L.; Wang, H.; Zhang, Y. Influence of Education Level on Mental Health and Medical Coping Modes: A Correlation Analysis in the Elderlies. Am. J. Nurs. Sci. 2019, 8, 324. [Google Scholar] [CrossRef]
- Quach, A.; Levine, M.E.; Tanaka, T.; Lu, A.T.; Chen, B.H.; Ferrucci, L.; Ritz, B.; Bandinelli, S.; Neuhouser, M.L.; Beasley, J.; et al. Epigenetic clock analysis of diet, exercise, education, and lifestyle factors. Aging 2017, 9, 419–446. [Google Scholar] [CrossRef]
- Chen, Y.H.; Karimi, M.; Rutten-van Mölken, M.P.M.H. The disease burden of multimorbidity and its interaction with educational level. PLoS ONE 2020, 15, e0243275. [Google Scholar] [CrossRef]
- McClellan, S.P.; Haque, K.; García-Peña, C. Diabetes multimorbidity combinations and disability in the Mexican Health and Aging Study, 2012–2015. Arch. Gerontol. Geriatr. 2021, 93, 104292. [Google Scholar] [CrossRef] [PubMed]
- Quiñones, A.R.; Markwardt, S.; Thielke, S.; Rostant, O.; Vásquez, E.; Botoseneanu, A. Prospective Disability in Different Combinations of Somatic and Mental Multimorbidity. J. Gerontol. A Biol. Sci. Med. Sci. 2018, 73, 204–210. [Google Scholar] [CrossRef] [PubMed]
| Sociodemographic Variables | n (%) |
|---|---|
| Age (years) | |
| 65–74 | 15,320 (29.0) |
| 75–84 | 24,987 (47.2) |
| ≥85 | 12,578 (23.8) |
| Sex | |
| Female | 32,535 (61.5) |
| Male | 20,350 (38.5) |
| Marital status | |
| Single | 6193 (13.2) |
| Married | 20,763 (44.4) |
| Domestic partnership | 454 (0.3) |
| Divorced | 2018 (4.3) |
| Widowed | 17,578 (37.6) |
| Unknown | 109 (0.2) |
| Education (years) | |
| No education | 8244 (31.5) |
| 1 to 6 | 15,802 (60.4) |
| 7 to 12 | 1087 (4.2) |
| ≥13 | 1047 (4.0) |
| Professional Level | |
| Unskilled | 18,379 (70.3) |
| Skilled | 6191 (23.7) |
| Intermediate | 1139 (4.4) |
| Specialist | 453 (1.7) |
| Cohabitation | |
| Lives alone | 7192 (27.5) |
| Lives with other (s) | 18,988 (72.5) |
| Region of Portugal | |
| Alentejo | 4913 (9.7) |
| Algarve | 3659 (7.2) |
| Center | 11,937 (22.6) |
| Lisbon and Vale do Tejo | 11,362 (22.4) |
| North | 18,805 (37.1) |
| Parameters | Estimate | Standard Error | df | p Value | 95% Confidence Interval | ||
|---|---|---|---|---|---|---|---|
| Thresholds | Mild | αMild = 2.439 | 0.065 | 1421.020 | 1 | <0.001 | [2.312; 2.566] |
| Moderate | αModerate = 3.946 | 0.066 | 3559.323 | 1 | <0.001 | [3.816; 4.075] | |
| Localization | Age | bAge = 0.043 | 0.001 | 2684.676 | 1 | <0.001 | [0.041; 0.044] |
| Sex (Female) | bSex(Female) = 0.101 | 0.012 | 69.659 | 1 | <0.001 | [0.078; 0.125] | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ramos, A.; Fonseca, C.; Pinho, L.; Lopes, M.; Oliveira, H.; Henriques, A. Functional Profile of Older Adults Hospitalized in Convalescence Units of the National Network of Integrated Continuous Care of Portugal: A Longitudinal Study. J. Pers. Med. 2021, 11, 1350. https://doi.org/10.3390/jpm11121350
Ramos A, Fonseca C, Pinho L, Lopes M, Oliveira H, Henriques A. Functional Profile of Older Adults Hospitalized in Convalescence Units of the National Network of Integrated Continuous Care of Portugal: A Longitudinal Study. Journal of Personalized Medicine. 2021; 11(12):1350. https://doi.org/10.3390/jpm11121350
Chicago/Turabian StyleRamos, Ana, César Fonseca, Lara Pinho, Manuel Lopes, Henrique Oliveira, and Adriana Henriques. 2021. "Functional Profile of Older Adults Hospitalized in Convalescence Units of the National Network of Integrated Continuous Care of Portugal: A Longitudinal Study" Journal of Personalized Medicine 11, no. 12: 1350. https://doi.org/10.3390/jpm11121350
APA StyleRamos, A., Fonseca, C., Pinho, L., Lopes, M., Oliveira, H., & Henriques, A. (2021). Functional Profile of Older Adults Hospitalized in Convalescence Units of the National Network of Integrated Continuous Care of Portugal: A Longitudinal Study. Journal of Personalized Medicine, 11(12), 1350. https://doi.org/10.3390/jpm11121350








