Previous, Current, and Future Pharmacotherapy and Diagnosis of Prostate Cancer—A Comprehensive Review
Abstract
1. Introduction
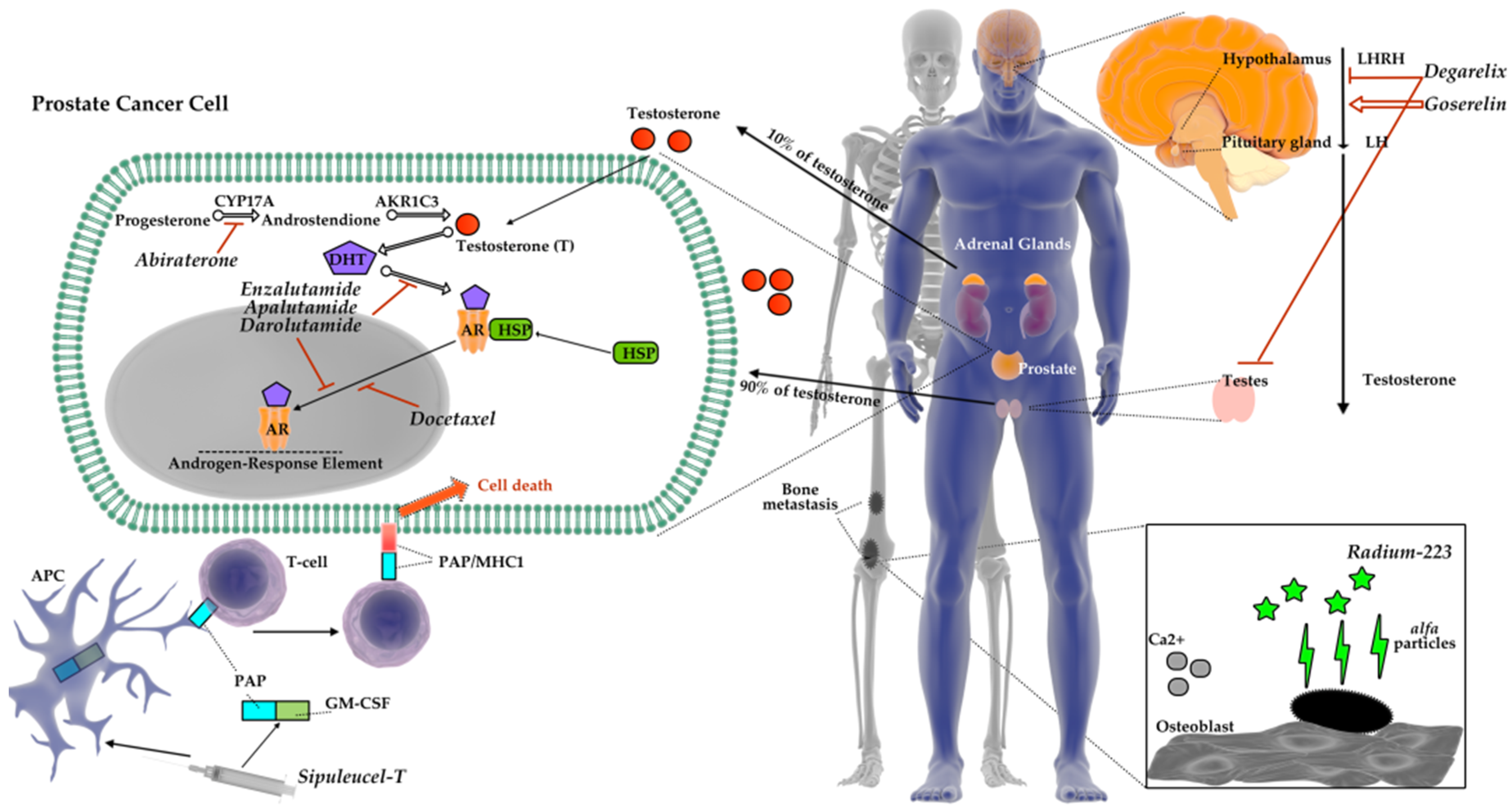
2. The Role of Androgens and Androgenic Receptors in Prostate Gland
3. Histology of Prostate Cancer
4. Diagnosis of Prostate Cancer
5. Prostate Cancer Therapy
5.1. Abiraterone
5.2. Enzalutamide
5.2.1. Safety and Efficacy Study of Enzalutamide (MDV3100) in Patients with Castration-Resistant Prostate Cancer Who Have Been Previously Treated with Docetaxel-Based Chemotherapy (AFFIRM)
5.2.2. Safety and Efficacy Study of Enzalutamide in Patients with Nonmetastatic Castration-Resistant Prostate Cancer nmCRPC (PROSPER)
5.3. Apalutamide
A Study of Apalutamide (ARN-509) in Men with Non-Metastatic Castration-Resistant Prostate Cancer (SPARTAN)
5.4. Darolutamide
Efficacy and Safety Study of Darolutamide (ODM-201) in Men with High-Risk Non-Metastatic Castration-Resistant Prostate Cancer (ARAMIS) Trial
5.5. Radium-223
5.6. Chemotherapy
5.7. Immunotherapy
5.7.1. Sipuleucel-T (Provenge)
5.7.2. PROSTVAC
5.7.3. Listeria Monocytogenes Vaccine
5.7.4. Immune Checkpoint Inhibitors (Ipilimumab, Pembrolizumab)
5.7.5. CAR-T Cells in Prostate Cancer Therapy
6. New Potential Therapeutic Targets in Prostate Cancer
7. Conclusions
Conflicts of Interest
Abbreviations
| ADT | androgen deprivation therapy |
| AR | androgen receptor |
| ARE | androgen receptor element |
| BPH | benign prostatic hyperplasia |
| CRPC | castration-resistant prostate cancer |
| CYP17 | cytochrome P450-17 |
| DHEA | dehydroepiandrosterone |
| DHT | dihydrotestosterone |
| GABAA | gamma-aminobutyric acid type A |
| LBD | ligand binding domain |
| LHRH | luteinizing hormone-releasing hormone |
| m-CRPC | metastatic castration-resistant prostate cancer |
| nm-CRPC | non-metastatic castration-resistant prostate cancer |
| NSAA | non-steroidal antiandrogen |
| PCa | prostate cancer |
| PSA | Prostate specific antigen |
| PSAD | prostate-specific antigen density |
| PSAV | prostate-specific antigen velocity |
| SAA | steroid antiandrogen |
References
- Pishgar, F.; Ebrahimi, H.; Saeedi Moghaddam, S.; Fitzmaurice, C.; Amini, E. Global, Regional and National Burden of Prostate Cancer, 1990 to 2015: Results from the Global Burden of Disease Study 2015. J. Urol. 2018, 199, 1224–1232. [Google Scholar] [CrossRef] [PubMed]
- Bray, F.; Ferlay, J.; Soerjomataram, I.; Siegel, R.L.; Torre, L.A.; Jemal, A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries: Global Cancer Statistics 2018. CA Cancer J. Clin. 2018, 68, 394–424. [Google Scholar] [CrossRef] [PubMed]
- Sobin, L.H.; Gospodarowicz, M.K.; Wittekind, C. Urological Tumors, Prostate. In TNM Classification of Malignant Tumours, 7th ed.; Sobin, L.H., Gospodarowicz, M.K., Wittekind, C., Eds.; Wiley-Blackwell: Hoboken, NJ, USA, 2009; pp. 243–248. [Google Scholar]
- Greiman, A.K.; Rosoff, J.S.; Prasad, S.M. Association of Human Development Index with global bladder, kidney, prostate and testis cancer incidence and mortality. BJU Int. 2017, 120, 799–807. [Google Scholar] [CrossRef] [PubMed]
- Mustafa, M.; Salih, A.F.; Illzam, E.M.; Sharifa, A.M.; Suleiman, M.; Hussain, S.S. Prostate Cancer: Pathophysiology, Diagnosis, and Prognosis. J. Dent. Med. Sci. 2016, 15, 4–11. [Google Scholar]
- Heidenreich, A.; Bastian, P.J.; Bellmunt, J.; Bolla, M.; Joniau, S.; van der Kwast, T.; Mason, M.; Matveev, V.; Wiegel, T.; Zattoni, F.; et al. EAU Guidelines on Prostate Cancer. Part II: Treatment of Advanced, Relapsing, and Castration-Resistant Prostate Cancer. Eur. Urol. 2014, 65, 467–479. [Google Scholar] [CrossRef] [PubMed]
- Mateo, J.; Fizazi, K.; Gillessen, S.; Heidenreich, A.; Perez-Lopez, R.; Oyen, W.J.G.; Shore, N.; Smith, M.; Sweeney, C.; Tombal, B.; et al. Managing Nonmetastatic Castration-resistant Prostate Cancer. Eur. Urol. 2018, 75, 285–293. [Google Scholar] [CrossRef] [PubMed]
- Holka-Pokorska, J.; Jarema, M.; Wichniak, A. Androgeny–wspólny marker biologiczny zaburzeń snu oraz wybranych dysfunkcji seksualnych? Psychiatr. Pol. 2014, 48, 701–714. [Google Scholar]
- Li, H.; Pham, T.; McWhinney, B.C.; Ungerer, J.P.; Pretorius, C.J.; Richard, D.J.; Mortimer, R.H.; d’Emden, M.C.; Richard, K. Sex Hormone Binding Globulin Modifies Testosterone Action and Metabolism in Prostate Cancer Cells. Int. J. Endocrinol. 2016, 2016, 1–10. [Google Scholar] [CrossRef]
- Zitzmann, M.; Nieschlag, E. The CAG repeat polymorphism within the androgen receptor gene and malaness. Int. J. Androl. 2003, 26, 76–83. [Google Scholar] [CrossRef]
- Wilson, C.M.; McPhaul, M.J. A and B form of the androgen receptor are present in human skin fibroblasts. Proc. Natl. Acad. Sci. USA 1994, 91, 1234–1238. [Google Scholar] [CrossRef]
- Zeng, R.; Liu, Z.; Sun, Y.; Xu, C. Differential expression and function of AR isoforms in prostate cancer. Oncol. Rep. 2012, 27, 492–498. [Google Scholar] [PubMed]
- Ruizeveld de Winter, J.A.; Trapman, J.; Vermey, M.; Mulder, E.; Zegers, N.D.; van der Kwast, T.H. Androgen receptor expression in human tissues: An immunohistochemical study. J. Histochem. Cytochem. 1991, 39, 927–936. [Google Scholar] [CrossRef] [PubMed]
- Davey, R.A.; Grossmann, M. Androgen Receptor Structure, Function and Biology: From Bench to Bedside. Clin. Biochem. Rev. 2016, 37, 3–15. [Google Scholar] [PubMed]
- Velcheti, V.; Karnik, S.; Bardot, S.F.; Prakash, O. Pathogenesis of Prostate Cancer: Lessons from Basic Research. Ochs. J. 2008, 8, 213–218. [Google Scholar]
- Kosaka, T.; Miyajima, A.; Oya, M. Is DHT Production by 5α-Reductase Friend or Foe in Prostate Cancer? Front. Oncol. 2014, 4, 1–4. [Google Scholar] [CrossRef]
- Benedettini, E.; Nguyen, P.; Loda, M. The pathogenesis of prostate cancer: From molecular to metabolic alterations. Diagn. Histopathol. 2008, 14, 195–201. [Google Scholar] [CrossRef]
- De Marzo, A.M.; Platz, E.A.; Sutcliffe, S.; Xu, J.; Grönberg, H.; Drake, C.G.; Nakai, Y.; Isaacs, W.B.; Nelson, W.G. Inflammation in prostate carcinogenesis. Nat. Rev. Cancer. 2007, 7, 256–269. [Google Scholar] [CrossRef]
- Humphrey, P.A. Histological variants of prostatic carcinoma and their significance: Prostatic carcinoma variants. Histopathology 2012, 60, 59–74. [Google Scholar] [CrossRef]
- Li, J.; Wang, Z. The pathology of unusual subtypes of prostate cancer. Chin. J. Caner Res. 2016, 28, 130–143. [Google Scholar]
- Kaleem, Z.; Swanson, P.E.; Vollmer, R.T.; Humphrey, P.A. Prostatic Adenocarcinoma with Atrophic Features: A Study of 202 Consecutive Completely Embedded Radical Prostatectomy Specimens. Am. J. Clin. Pathol. 1998, 109, 695–703. [Google Scholar] [CrossRef]
- Arista-Nasr, J.; Martínez-Benítez, B.; Aguilar-Ayala, E.L.; Aleman-Sanchez, C.N.; Bornstein-Quevedo, L.; Albores-Saavedra, J. Pseudohyperplastic prostate carcinoma: Histologic patterns and differential diagnosis. Ann. Diagn. Pathol. 2015, 19, 253–260. [Google Scholar] [CrossRef] [PubMed]
- Warner, J.N.; Nakamura, L.Y.; Pacelli, A.; Humphreys, M.R.; Castle, E.P. Primary Signet Ring Cell Carcinoma of the Prostate. MayoClin. Proc. 2010, 85, 1130–1136. [Google Scholar] [CrossRef] [PubMed]
- Venyo Kodzo-Grey, A. Primary Lymphoepithelioma-Like Carcinoma of the Prostate Gland: A Review of the Literature. scientifica 2016, 2016, 1–7. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Mottet, N.; Bellmunt, J.; Bolla, M.; Briers, E.; Cumberbatch, M.G.; De Santis, M.; Fossati, N.; Gross, T.; Henry, A.M.; Joniau, S.; et al. EAU-ESTRO-SIOG Guidelines on Prostate Cancer. Part 1: Screening, Diagnosis, and Local Treatment with Curative Intent. Eur. Urol. 2017, 71, 618–629. [Google Scholar] [CrossRef] [PubMed]
- Velonas, V.; Woo, H.; Remedios, C.; Assinder, S. Current Status of Biomarkers for Prostate Cancer. Int. J. Mol. Sci. 2013, 14, 11034–11060. [Google Scholar] [CrossRef] [PubMed]
- Kotb, A.F.; Tanguay, S.; Luz, M.A.; Kassouf, W.; Aprikian, A.G. Relationship between initial PSA density with future PSA kinetics and repeat biopsies in men with prostate cancer on active surveillance. Prost. Caner Prost. Dis. 2011, 14, 53–57. [Google Scholar] [CrossRef][Green Version]
- Naya, Y.; Okihara, K. Role of Complexed PSA in the Early Detection of Prostate Cancer. J. Natl. Compr. Cancer Netw. 2004, 2, 209–212. [Google Scholar] [CrossRef][Green Version]
- Karnes, R.J.; MacKintosh, F.R.; Morrell, C.H.; Rawson, L.; Sprenkle, P.C.; Kattan, M.W.; Colicchia, M.; Neville, T.B. Prostate-Specific Antigen Trends Predict the Probability of Prostate Cancer in a Very Large, U.S. Veterans Affairs Cohort. Front. Oncol. 2018, 8, 1–11. [Google Scholar] [CrossRef]
- Oesterling, J.E.; Jacobsen, S.J.; Klee, G.G.; Pettersson, K.; Piironen, T.; Abrahamsson, P.A.; Stenman, U.H.; Dowell, B.; Lövgren, T.; Lilja, H. Free, complexed and total serum prostate specific antigen: The establishment of appropriate reference ranges for their concentrations and ratios. J. Urol. 1995, 54, 1090–1095. [Google Scholar] [CrossRef]
- Catalona, W.J.; Smith, D.S.; Wolfert, R.L.; Wang, T.J.; Rittenhouse, H.G.; Ratliff, T.L.; Nadler, R.B. Evaluation of percentage of free serum prostate-specific antigen to improve specificity of prostate cancer screening. JAMA 1995, 274, 1214–1220. [Google Scholar] [CrossRef]
- Grummet, J. How to Biopsy: Transperineal Versus Transrectal, Saturation Versus Targeted, What’s the Evidence? Urol. Clin. N. Am. 2017, 44, 525–534. [Google Scholar] [CrossRef] [PubMed]
- Grummet, J.; Pepdjonovic, L.; Huang, S.; Anderson, E.; Hadaschik, B. Transperineal vs. transrectal biopsy in MRI targeting. Transl. Androl. Urol. 2017, 6, 368–375. [Google Scholar] [CrossRef] [PubMed]
- McGrath, S.; Christidis, D.; Clarebrough, E.; Ingle, R.; Perera, M.; Bolton, D.; Lawrentschuk, N. Transperineal prostate biopsy - tips for analgesia. BJU Int. 2017, 120, 164–167. [Google Scholar] [CrossRef] [PubMed]
- Sivaraman, A.; Sanchez-Salas, R.; Barret, E.; Ahallal, Y.; Rozet, F.; Galiano, M.; Prapotnich, D.; Cathelineau, X. Transperineal template-guided mapping biopsy of the prostate. Int. J. Urol. 2015, 22, 146–151. [Google Scholar] [CrossRef]
- Nakai, Y.; Tanaka, N.; Anai, S.; Miyake, M.; Hori, S.; Tatsumi, Y.; Morizawa, Y.; Fujii, T.; Konishi, N.; Fujimoto, K. Transperineal template-guided saturation biopsy aimed at sampling one core for each milliliter of prostate volume: 103 cases requiring repeat prostate biopsy. BMC Urol. 2017, 17, 28. [Google Scholar] [CrossRef]
- Xiang, J.; Yan, H.; Li, J.; Wang, X.; Chen, H.; Zheng, X. Transperineal versus transrectal prostate biopsy in the diagnosis of prostate cancer: A systematic review and meta-analysis. World. J. Surg. Oncol. 2019, 17, 1–11. [Google Scholar] [CrossRef]
- Sarkar, S.; Das, S. A Review of Imaging Methods for Prostate Cancer Detection: Supplementary Issue: Image and Video Acquisition and Processing for Clinical Applications. Biomed. Eng. Comput. Biol. 2016, 7, 1–15. [Google Scholar] [CrossRef]
- Turkbey, B.; Choyke, P.L. Future Perspectives and Challenges of Prostate MR Imaging. Radiol. Clin. N. Am. 2018, 56, 327–337. [Google Scholar] [CrossRef]
- Humphrey, P.A. Gleason grading and prognostic factors in carcinoma of the prostate. Mod. Pathol. 2004, 17, 292–306. [Google Scholar] [CrossRef]
- Herden, J.; Weissbach, L. Utilization of Active Surveillance and Watchful Waiting for localized prostate cancer in the daily practice. World. J. Urol. 2018, 36, 383–391. [Google Scholar] [CrossRef]
- Miller, K.D.; Siegel, R.L.; Lin, C.C.; Mariotto, A.B.; Kramer, J.L.; Rowland, J.H.; Stein, K.D.; Alteri, R.; Jemal, A. Cancer treatment and survivorship statistics, 2016. CA Cancer. J. Clin. 2016, 66, 271–289. [Google Scholar] [CrossRef] [PubMed]
- Kawahara, T.; Miyamoto, H. Androgen Receptor Antagonists in the Treatment of Prostate Cancer. Clin. Immunol. Endocr. Metab. Drugs 2014, 1, 11–19. [Google Scholar] [CrossRef]
- Chen, Y.; Clegg, N.J.; Scher, H.I. Anti-androgens and androgen-depleting therapies in prostate cancer: New agents for an established target. Lan. Oncol. 2009, 10, 981–991. [Google Scholar] [CrossRef]
- Del Moral, P.F.; Dijkman, G.A.; Debruyne, F.M.J.; Witjes, W.P.J.; Kolvenbag, G.J. Three-month Depot of Goserelin Acetate: Clinical Efficacy and Endocrine Profile. Urology 1996, 48, 894–900. [Google Scholar] [CrossRef]
- Merseburger, A.S.; Hupe, M.C. An Update on Triptorelin: Current Thinking on Androgen Deprivation Therapy for Prostate Cancer. Adv. Ther. 2016, 33, 1072–1093. [Google Scholar] [CrossRef] [PubMed]
- Klotz, L.; Boccon-Gibod, L.; Shore, N.D.; Andreou, C.; Persson, B.-E.; Cantor, P.; Jensen, J.-K.; Olesen, T.K.; Schröder, F.H. The efficacy and safety of degarelix: A 12-month, comparative, randomized, open-label, parallel-group phase III study in patients with prostate cancer. BJIUI 2008, 102, 1531–1538. [Google Scholar] [CrossRef]
- Ryan, C.J.; Smith, M.R.; de Bono, J.S.; Molina, A.; Logothetis, C.J.; de Souza, P.; Fizazi, K.; Mainwaring, P.; Piulats, J.M.; Ng, S.; et al. COU-AA-302 Investigators. Abiraterone in metastatic prostate cancer without previous chemotherapy. N. Engl. J. Med. 2013, 368, 138–148. [Google Scholar] [CrossRef]
- Heidenreich, A.; Bellmunt, J.; Bolla, M.; Joniau, S.; Mason, M.; Matveev, V.; Mottet, N.; Schmid, H.P.; van der Kwast, T.; Wiegel, T.; et al. EAU Guidelines on Prostate Cancer. Part I: Screening, diagnosis, and treatment of clinically localised disease. Eur. Urol. 2011, 59, 61–71. [Google Scholar] [CrossRef]
- El-Rayes, B.F.; Hussain, M.H. Hormonal therapy for prostate cancer: Past, present and future. Exp. Rev. Antican. Ther. 2002, 2, 37–47. [Google Scholar] [CrossRef]
- Moul, J.W. Utility of LHRH antagonists for advanced prostate cancer. Can. J. Urol. 2014, 21, 22–27. [Google Scholar]
- Peto, R.; Dalesio, O. Breast and prostate cancer: 10-year survival gains in the hormonal adjuvant treatment trials. In Proceedings of the 12th European Conference on Clinical Oncology, Copenhagen, Denmark, 21–25 September 2003; p. S101. [Google Scholar]
- Nguyen, P.L.; Alibhai, S.M.; Basaria, S.; D’Amico, A.V.; Kantoff, P.W.; Keating, N.L.; Penson, D.F.; Rosario, D.J.; Tombal, B.; Smith, M.R. Adverse effects of androgen deprivation therapy and strategies to mitigate them. Eur. Urol. 2015, 67, 825–836. [Google Scholar] [CrossRef] [PubMed]
- Skolarus, T.A.; Caram, M.V.; Shahinian, V.B. Androgen-deprivation-associated bone disease. Curr. Opin. Urol. 2014, 24, 601–607. [Google Scholar] [CrossRef] [PubMed]
- Nead, K.T.; Gaskin, G.; Chester, C.; Swisher-McClure, S.; Leeper, N.J.; Shah, N.H. Association between androgen deprivation therapy and risk of dementia. JAMA Oncol. 2017, 3, 49–55. [Google Scholar] [CrossRef] [PubMed]
- Auchus, R.J. The backdoor pathway to dihydrotestosterone. Trends Endocrinol. Metab. 2014, 15, 432–438. [Google Scholar] [CrossRef]
- Attard, G.; Reid, A.H.; Yap, T.A.; Raynaud, F.; Dowsett, M.; Settatree, S.; Barrett, M.; Parker, C.; Martins, V.; Folkerd, E.; et al. Phase I clinical trial of a selective inhibitor of CYP17, abiraterone acetate, confirms that castration-resistant prostate cancer commonly remains hormone driven. J. Clin. Oncol. 2008, 26, 4563–4571. [Google Scholar] [CrossRef]
- Fizazi, K.; Scher, H.I.; Molina, A.; Logothetis, C.J.; Chi, K.N.; Jones, R.J.; Staffurth, J.N.; North, S.; Vogelzang, N.J.; Saad, F.; et al. COU-AA-301 Investigators. Abiraterone acetate for treatment of metastatic castration-resistant prostate cancer: Final overall survival analysis of the COU-AA-301 randomised, double-blind, placebo-controlled phase 3 study. Lancet Oncol. 2012, 13, 983–992. [Google Scholar] [CrossRef]
- Denis, L.J.; Carneiro De Moura, J.L.; Bono, A.; Sylvester, R.; Whelan, P.; Newling, D.; Depauw, M. Members of the eortc gu group and eortc data center. Goserelin acetate and flutamide versus bilateral orchiectomy: A phase III eortc trial. Urology 1993, 42, 119–130. [Google Scholar] [CrossRef]
- Dijkman, G.A.; Janknegt, R.A.; De Reijke, T.M.; Debruyne, F.M. Long-term efficacy and safety of nilutamide plus castration in advanced prostate cancer, and the significance of early prostate specific antigen normalization. International Anandron Study Group. J. Urol. 1997, 158, 160–163. [Google Scholar] [CrossRef]
- Kolvenbag, G.J.; Blackledge, G.R.; Gotting-Smith, K. Bicalutamide (Casodex) in the treatment of prostate cancer: History of clinical development. Prostate 1998, 34, 61–72. [Google Scholar] [CrossRef]
- Scher, H.I.; Fizazi, K.; Saad, F.; Taplin, M.E.; Sternberg, C.N.; Miller, K.; de Wit, R.; Mulders, P.; Chi, K.N.; Shore, N.D.; et al. AFFIRM Investigators. Increased survival with enzalutamide in prostate cancer after chemotherapy. N. Engl. J. Med. 2012, 367, 1187–1197. [Google Scholar] [CrossRef]
- Smith, M.R.; Saad, F.; Chowdhury, S.; Oudard, S.; Hadaschik, B.A.; Graff, J.N.; Olmos, D.; Mainwaring, P.N.; Youl Lee, J.; Uemura, H.; et al. Apalutamide Treatment and Metastasis-free Survival in Prostate Cancer. N. Engl. J. Med. 2018, 378, 1408–1418. [Google Scholar] [CrossRef] [PubMed]
- Fizazi, K.; Shore, N.; Tammela, T.L.; Ulys, A.; Vjaters, E.; Polyakov, S.; Jievaltas, M.; Luz, M.; Alekseev, B.; Kuss, I.; et al. ARAMIS Investigators. Darolutamide in Nonmetastatic, Castration-Resistant Prostate Cancer. N. Engl. J. Med. 2019, 380, 1235–1246. [Google Scholar] [CrossRef] [PubMed]
- Schröder, F.H.; Whelan, P.; de Reijke, T.M.; Kurth, K.H.; Pavone-Macaluso, M.; Mattelaer, J.; van Velthoven, R.F.; Debois, M.; Collette, L. Members of the EORTC Genito-Urinary Group. Metastatic prostate cancer treated by flutamide versus cyproterone acetate. Final analysis of the “European Organization for Research and Treatment of Cancer” (EORTC) Protocol 30892. Eur. Urol. 2004, 45, 457–464. [Google Scholar] [CrossRef] [PubMed]
- McLeod, D.G. Tolerability of Nonsteroidal Antiandrogens in the Treatment of Advanced Prostate Cancer. Oncology 1997, 2, 18–27. [Google Scholar]
- Crawford, E.D.; Eisenberger, M.A.; McLeod, D.G.; Spaulding, J.T.; Benson, R.; Dorr, F.A.; Blumenstein, B.A.; Davis, M.A.; Goodman, P.J. A controlled trial of leuprolide with and without flutamide in prostatic carcinoma. N. Engl. J. Med. 1989, 321, 419–424. [Google Scholar] [CrossRef]
- Jung, M.E.; Ouk, S.; Yoo, D.; Sawyers, C.L.; Chen, C.; Tran, C.; Wongvipat, J. Structure-activity relationship for thiohydantoin androgen receptor antagonists for castration-resistant prostate cancer (CRPC). J. Med. Chem. 2010, 53, 2779–2796. [Google Scholar] [CrossRef]
- Guerrero, J.; Alfaro, I.E.; Gómez, F.; Protter, A.A.; Bernales, S. Enzalutamide, an androgen receptor signaling inhibitor, in- duces tumor regression in a mouse model of castration-resistant prostate cancer. Prostate 2013, 73, 1291–1305. [Google Scholar] [CrossRef]
- Korpal, M.; Korn, J.M.; Gao, X.; Rakiec, D.P.; Ruddy, D.A.; Doshi, S.; Yuan, J.; Kovats, S.G.; Kim, S.; Cooke, V.G.; et al. An F876L mutation in androgen receptor confers genetic and phenotypic resistance to MDV3100 (enzalutamide). Cancer Discov. 2013, 3, 1030–1043. [Google Scholar] [CrossRef]
- Lin, T.H.; Lee, S.O.; Niu, Y.; Xu, D.; Liang, L.; Li, L.; Yeh, S.D.; Fujimoto, N.; Yeh, S.; Chang, C. Differential androgen deprivation therapies with anti-androgens casodex/bicalutamide or MDV3100/Enzalutamide versus anti-androgen receptor ASC-J9(R) Lead to promotion versus suppression of prostate cancer metastasis. J. Biol. Chem. 2013, 288, 9359–19369. [Google Scholar] [CrossRef]
- Asangani, I.A.; Dommeti, V.L.; Wang, X.; Malik, R.; Cieslik, M.; Yang, R.; Escara-Wilke, J.; Wilder-Romans, K.; Dhanireddy, S.; Engelke, C.; et al. Therapeutic Targeting of BET Bromodomain Proteins in Castration-Resistant Prostate Cancer. Nature 2014, 510, 278–282. [Google Scholar] [CrossRef]
- Scher, H.I.; Beer, T.M.; Higano, C.S.; Anand, A.; Taplin, M.E.; Efstathiou, E.; Rathkopf, D.; Shelkey, J.; Yu, E.Y.; Alumkal, J.; et al. Prostate Cancer Foundation/Department of Defense Prostate Cancer Clinical Trials Consortium. Antitumour activity of MDV3100 in castration-resistant prostate cancer: A phase 1-2 study. Lancet 2010, 375, 1437–1446. [Google Scholar] [CrossRef]
- Hussain, M.; Fizazi, K.; Saad, F.; Rathenborg, P.; Shore, N.; Ferreira, U.; Ivashchenko, P.; Demirhan, E.; Modelska, K.; de Phung, B.S.; et al. Enzalutamide in Men with Nonmetastatic, Castration-Resistant Prostate Cancer. N. Engl. J. Med. 2018, 378, 2465–2474. [Google Scholar] [CrossRef] [PubMed]
- Chong, J.; Oh, W.; Liaw, B. Profile of apalutamide in the treatment of metastatic castration-resistant prostate cancer: Evidence to date. OncoTarg. Ther. 2018, 11, 2141–2147. [Google Scholar] [CrossRef] [PubMed]
- Clegg, N.J.; Wongvipat, J.; Joseph, J.D.; Tran, C.; Ouk, S.; Dilhas, A.; Chen, Y.; Grillot, K.; Bischoff, E.D.; Cail, L.; et al. ARN-509: A Novel Antiandrogen for Prostate Cancer Treatment. Cancer Res. 2012, 72, 1494–1503. [Google Scholar] [CrossRef] [PubMed]
- Rathkopf, D.E.; Scher, H.I. Apalutamide for the treatment of prostate cancer. Exp. Rev. Antican. Ther. 2018, 18, 823–836. [Google Scholar] [CrossRef]
- Al-Salama, Z.T. Apalutamide: First Global Approval. Drugs 2018, 78, 699–705. [Google Scholar] [CrossRef]
- Ranjan, R.K.; Chandra, A. Apalutamide: A better option for the treatment of non-metastatic castration resistant prostatic carcinoma. Int. J. Basic. Clin. Pharmacol. 2018, 7, 1853–1856. [Google Scholar] [CrossRef]
- Joseph, J.D.; Lu, N.; Qian, J.; Sensintaffar, J.; Shao, G.; Brigham, D.; Moon, M.; Chow Maneval, E.; Chen, I.; Darimont, B.; et al. Clinically Relevant Androgen Receptor Mutation Confers Resistance to Second-Generation Antiandrogens Enzalutamide and ARN-509. Cancer Discov. 2013, 3, 1020–1029. [Google Scholar] [CrossRef]
- Borgmann, H.; Lallous, N.; Ozistanbullu, D.; Beraldi, E.; Paul, N.; Dalal, K.; Fazli, L.; Haferkamp, A.; Lejeune, P.; Cherkasov, A.; et al. Head-to-head comparison of efficacy of darolutamide (ODM-201) vs. enzalutamide on mutated forms of the androgen receptor. Eur. Urol. Suppl. 2018, 17, e505. [Google Scholar] [CrossRef]
- Hotte, S.J.; Saad, F. Current management of castrate-resistant prostate cancer. Curr. Oncol. 2010, 17, 72–79. [Google Scholar] [CrossRef]
- Saad, F.; Cella, D.; Basch, E.; Hadaschik, B.A.; Mainwaring, P.N.; Oudard, S.; Graff, J.N.; McQuarrie, K.; Li, S.; Hudgens, S.; et al. Effect of apalutamide on health-related quality of life in patients with non-metastatic castration-resistant prostate cancer: An analysis of the SPARTAN randomised, placebo-controlled, phase 3 trial. Lancet Oncol. 2018, 19, 1404–1416. [Google Scholar] [CrossRef]
- Moilanen, A.M.; Riikonen, R.; Oksala, R.; Ravanti, L.; Aho, E.; Wohlfahrt, G.; Nykänen, P.S.; Törmäkangas, O.P.; Palvimo, J.J.; Kallioa, P.J. Discovery of ODM-201, a new-generation androgen receptor inhibitor targeting resistance mechanisms to androgen signaling-directed prostate cancer therapies. Sci. Rep. 2015, 5, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Zurth, C.; Sandman, S.; Trummel, D.; Seidel, D.; Nubbemeyer, R.; Gieschen, H. Higher blood–brain barrier penetration of [14C]apalutamide and [14C]enzalutamide compared to [14C]darolutamide in rats using whole-body autoradiography. J. Clin. Oncol. 2019, 37, 156. [Google Scholar] [CrossRef]
- Zurth, C.; Graudenz, K.; Denner, K.; Korjamo, T.; Fricke, R.; Wilkinson, G.; Seitz, F.; Prien, O. Drug-drug interaction (DDI) of darolutamide with cytochrome P450 (CYP) and P-glycoprotein (P-gp) substrates: Results from clinical and in vitro studies. J. Clin. Oncol. 2019, 37, 297. [Google Scholar] [CrossRef]
- Kim, H.J.; Kim, J.H.; Bae, S.C.; Choi, J.Y.; Kim, H.J.; Ryoo, H.M. The protein kinase C pathway plays a central role in the fibroblast growth factor-stimulated expression and transactivation activity of Runx2. J. Biol. Chem. 2003, 278, 319–326. [Google Scholar] [CrossRef]
- Abou, D.S.; Pickett, J.; Mattson, J.E.; Thorek, D.L.J. A Radium-223 microgenerator from cyclotron-produced trace Actinium-227. Appl. Radiat. Isot. 2017, 119, 36–42. [Google Scholar] [CrossRef]
- Heinrich, D.; Bektic, J.; Bergman, A.M.; Caffo, O.; Cathomas, R.; Chi, K.N.; Daugaard, G.; Keizman, D.; Kindblom, J.; Kramer, G.; et al. The Contemporary Use of Radium-223 in Metastatic Castration-resistant Prostate Cancer. Clin. Genit. Cancer. 2018, 16, 223–231. [Google Scholar] [CrossRef]
- Deshayes, E.; Roumiguie, M.; Thibault, C.; Beuzeboc, P.; Cachin, F.; Hennequin, C.; Huglo, D.; Rozet, F.; Kassab-Chahmi, D.; Rebillard, X.; et al. Radium 223 dichloride for prostate cancer treatment. Drug Des. Dev. Ther. 2017, 11, 2643–2651. [Google Scholar] [CrossRef]
- Spratt, D.E. Combination therapies in prostate cancer: Proceed with caution. Lancet Oncol. 2019, 20, 321–323. [Google Scholar] [CrossRef]
- Tannock, I.F.; de Wit, R.; Berry, W.R.; Horti, J.; Pluzanska, A.; Chi, K.N.; Oudard, S.; Théodore, C.; James, N.D.; Turesson, I.; et al. TAX 327 Investigators. Docetaxel plus prednisone or mitoxantrone plus prednisone for advanced prostate cancer. N. Engl. J. Med. 2004, 351, 1502–1512. [Google Scholar] [CrossRef]
- Sartor, O.; Michels, R.M.; Massard, C.; de Bono, J.S. Novel therapeutic strategies for metastatic prostate cancer in the post-docetaxel setting. Oncologist 2011, 16, 1487–1497. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Zhu, M.L.; Horbinski, C.M.; Garzotto, M.; Qian, D.Z.; Beer, T.M.; Kyprianou, N. Tubulin-targeting chemotherapy impairs androgen receptor activity in prostate cancer. Cancer Res. 2010, 70, 7992–8002. [Google Scholar] [CrossRef] [PubMed]
- Fitzpatrick, J.M.; de Wit, R. Taxane mechanisms of action: Potential implications for treatment sequencing in metastatic castration-resistant prostate cancer. Eur. Urol. 2014, 65, 1198–1204. [Google Scholar] [CrossRef] [PubMed]
- Galsky, M.D.; Vogelzang, N.J. Docetaxel-based combination therapy for castration-resistant prostate cancer. Ann. Oncol. 2010, 21, 2135–2144. [Google Scholar] [CrossRef] [PubMed]
- Handy, C.E.; Antonarakis, E.S. Sipuleucel-T for the treatment of prostate cancer: Novel insights and future directions. Future Oncol. 2018, 14, 907–917. [Google Scholar] [CrossRef]
- Higano, C.S.; Schellhammer, P.F.; Small, E.J.; Burch, P.A.; Neumunaitis, J.; Yuh, L.; Provost, N.; Frohlich, M.W. Integrated data from 2 randomized, double-blind, placebo-controlled, phase 3 trials of active cellular immunotherapy with sipuleucel-T in advanced prostate cancer. Cancer 2009, 115, 3670–3679. [Google Scholar] [CrossRef]
- Sheikh, N.; Cham, J.; Zhang, L.; DeVries, T.; Letarte, S.; Pufnock, J.; Hamm, D.; Trager, J.; Fong, L. Clonotypic Diversification of Intratumoral T Cells Following Sipuleucel-T Treatment in Prostate Cancer Subjects. Cancer Res. 2016, 76, 3711–3718. [Google Scholar] [CrossRef]
- Gulley, J.L.; Borre, M.; Vogelzang, N.J.; Ng, S.; Agarwal, N.; Parker, C.C.; Pook, D.W.; Rathenborg, P.; Flaig, T.W.; Carles, J.; et al. Phase III Trial of PROSTVAC in Asymptomatic or Minimally Symptomatic Metastatic Castration-Resistant Prostate Cancer. J. Clin. Oncol. 2019, 37, 1051–1061. [Google Scholar] [CrossRef]
- Shahabi, V.; Reyes-Reyes, M.; Wallecha, A.; Rivera, S.; Paterson, Y.; Maciag, P. Development of a Listeria monocytogenes based vaccine against prostate cancer. Cancer Immunol. Immunother. 2008, 57, 1301–1313. [Google Scholar] [CrossRef]
- Gunn, G.R.; Zubair, A.; Peters, C.; Pan, Z.K.; Wu, T.C.; Paterson, Y. Two Listeria monocytogenes vaccine vectors that express different molecular forms of human papilloma virus-16 (HPV-16) E7 induce qualitatively different T cell immunity that correlates with their ability to induce regression of established tumors immortalized by HPV-16. J. Immunol. 2001, 167, 6471–6479. [Google Scholar]
- Haas, N.B.; Stein, M.N.; Tutrone, R.; Perini, R.; Denker, A.; Mauro, D.; Fong, L. Phase I-II study of ADXS31-142 alone and in combination with pembrolizumab in patients with previously treated metastatic castration-resistant prostate cancer (mCRPC): The KEYNOTE-046 trial. J. Immunother. Cancer 2015, 3, 153. [Google Scholar] [CrossRef]
- Le, D.T.; Dubenksy, T.W.; Brockstedt, D.G. Clinical development of Listeria monocytogenes-based immunotherapies. Semin. Oncol. 2012, 39, 311–322. [Google Scholar] [CrossRef] [PubMed]
- Kwon, E.D.; Drake, C.G.; Scher, H.I.; Fizazi, K.; Bossi, A.; van den Eertwegh, A.J.M.; Krainer, M.; Houede, N.; Santos, R.; Mahammedi, H.; et al. Ipilimumab versus placebo after radiotherapy in patients with metastatic castration-resistant prostate cancer that had progressed after docetaxel chemotherapy (CA184-043): A multicentre, randomised, double-blind, phase 3 trial. Lancet Oncol. 2014, 15, 700–712. [Google Scholar] [CrossRef]
- Yu, E.Y.; Massard, C.; Retz, M.; Tafreshi, A.; Carles Galceran, J.; Hammerer, P.; Fong, P.C.C.; Shore, N.D.; Joshua, A.; Linch, M.D.; et al. Keynote-365 cohort a: Pembrolizumab (pembro) plus olaparib in docetaxel-pretreated patients (pts) with metastatic castrate-resistant prostate cancer (mCRPC). J. Clin. Oncol. 2019, 37, 145. [Google Scholar] [CrossRef]
- Majzner, R.G.; Mackall, C.L. Clinical lessons learned from the first leg of the CAR T cell journey. Nat. Med. 2019, 25, 1341–1355. [Google Scholar] [CrossRef]
- Junghans, R.P.; Ma, Q.; Rathore, R.; Gomes, E.M.; Bais, A.J.; Lo, A.S.; Abedi, M.; Davies, R.A.; Cabral, H.J.; Al-Homsi, A.S.; et al. Phase I Trial of Anti-PSMA Designer CAR-T Cells in Prostate Cancer: Possible Role for Interacting Interleukin 2-T Cell Pharmacodynamics as a Determinant of Clinical Response. Prostate 2016, 76, 1257–1270. [Google Scholar] [CrossRef]
- Hirano, T.; Ishihara, K.; Hibi, M. Roles of STAT3 in mediating the cell growth, differentiation and survival signals relayed through the IL-6 family of cytokine receptors. Oncogene 2000, 19, 2548–2556. [Google Scholar] [CrossRef]
- Kang, T.S.; Wang, W.; Zhong, H.J.; Dong, Z.Z.; Huang, Q.; Mok, S.W.; Leung, C.H.; Wong, V.K.; Ma, D.L. An anti-prostate cancer benzofuran-conjugated iridium(III) complex as a dual inhibitor of STAT3 and NF-κB. Cancer Lett. 2017, 396, 76–84. [Google Scholar] [CrossRef]
- Wu, K.J.; Zhong, H.J.; Yang, G.; Wu, C.; Huang, J.M.; Li, G.; Ma, D.L.; Leung, C.H. Small Molecule Pin1 Inhibitor Blocking NF-κB signaling in prostate cancer cells. Chem. Asian. J. 2018, 13, 275–279. [Google Scholar] [CrossRef]
- Yang, C.; Wang, W.; Liang, J.X.; Li, G.; Vellaisamy, K.; Wong, C.Y.; Ma, D.L.; Leung, C.H. A rhodium(III)-based inhibitor of lysine-specific histone demethylase 1 as an epigenetic modulator in prostate cancer cells. J. Med. Chem. 2017, 60, 2597–2603. [Google Scholar] [CrossRef]
- Welsh, J.B.; Sapinoso, L.M.; Su, A.I.; Kern, S.G.; Wang-Rodriguez, J.; Moskaluk, C.A.; Frierson, H.F., Jr.; Hampton, G.M. Analysis of gene expression identifies candidate markers and pharmacological targets in prostate cancer. Cancer Res. 2001, 61, 5974–5978. [Google Scholar] [PubMed]
- Ding, M.; Van der Kwast, T.H.; Vellanki, R.N.; Foltz, W.D.; McKee, T.D.; Sonenberg, N.; Pandolfi, P.P.; Koritzinsky, M.; Wouters, B.G. The mTOR Targets 4E-BP1/2 restrain tumor growth and promote hypoxia tolerance in PTEN-driven prostate cancer. Mol. Cancer Res. 2018, 16, 682–695. [Google Scholar] [CrossRef] [PubMed]
| Drug Classification | Example of Drug | Mechanism of Action | Clinical End Point |
|---|---|---|---|
| LHRH agonists | Goserelin Triptorelin | Induces testosterone suppression by binding to LHRH receptors in pituitary gland; thus, acting as an agonist that stimulates the production of LH and FSH. As a result, it promotes the production of testosterone in a non-physiological way. Finally, TTE levels decrease due to the regulation of the hormonal feedback systems. | Clinical trials have shown a reduction in serum testosterone levels below the castration level [45,46]. |
| LHRH antagonists | Degarelix | Induces testosterone suppression by binding to LHRH receptors in pituitary gland; thus, blocking their interaction with LHRH and then reducing the level of LH and FSH. | Treatment resulted in suppression of testosterone levels to ≤0.5 ng/mL between 28 and 364 days [47]. |
| CYP17 inhibitor | Abiraterone acetate | Lowers androgens (DHEA, TTE, DHT) levels by irreversible inhibition of CYP17A1 activity. Furthermore, it has partial affinity to AR. | Treatment resulted in 57% prolonged radiographic progression-free survival (rPFS) and 25% decrease in the risk of death [48]. |
| Drug Classification | Example of Drug | Mechanism of Action | Clinical End Point |
|---|---|---|---|
| First-generation NSAAs | Flutamide | The mechanism is based on the selective binding of the drug to the AR, which blocks the effects of androgens (TTE, DHT) on prostate cells. | Flutamide with LHRH-A prolong the survival and time to progression [59]. |
| Nilutamide | Nilutamide with orchiectomy improve survival and prolong time to progression [60]. | ||
| Bicalutamide | Bicalutamide with LHRH-A lower TTE levels and prolong the median survival compared with the flutamide with LHRH-A combination [61]. | ||
| Second-generation NSAAs | Enzalutamide | Prolongs the survival of patients with m-CRPC after chemotherapy [62]. | |
| Apalutamide | Prolongs metastasis-free survival and time to progression of patients with nm-CRPC [63]. | ||
| Darolutamide | Prolongs metastasis-free survival of patients with nm-CRPC [64]. | ||
| SAAs | Cyproterone acetate | SAAs act similarly to NSAAs, but in addition to blocking the effects of androgens, they also suppress their gonadal production. | SAAs exhibit poor effectiveness in prostate cancer therapy (lower than NSAAs) and have more side effects [65]. |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Malinowski, B.; Wiciński, M.; Musiała, N.; Osowska, I.; Szostak, M. Previous, Current, and Future Pharmacotherapy and Diagnosis of Prostate Cancer—A Comprehensive Review. Diagnostics 2019, 9, 161. https://doi.org/10.3390/diagnostics9040161
Malinowski B, Wiciński M, Musiała N, Osowska I, Szostak M. Previous, Current, and Future Pharmacotherapy and Diagnosis of Prostate Cancer—A Comprehensive Review. Diagnostics. 2019; 9(4):161. https://doi.org/10.3390/diagnostics9040161
Chicago/Turabian StyleMalinowski, Bartosz, Michał Wiciński, Nikola Musiała, Ilona Osowska, and Mateusz Szostak. 2019. "Previous, Current, and Future Pharmacotherapy and Diagnosis of Prostate Cancer—A Comprehensive Review" Diagnostics 9, no. 4: 161. https://doi.org/10.3390/diagnostics9040161
APA StyleMalinowski, B., Wiciński, M., Musiała, N., Osowska, I., & Szostak, M. (2019). Previous, Current, and Future Pharmacotherapy and Diagnosis of Prostate Cancer—A Comprehensive Review. Diagnostics, 9(4), 161. https://doi.org/10.3390/diagnostics9040161





