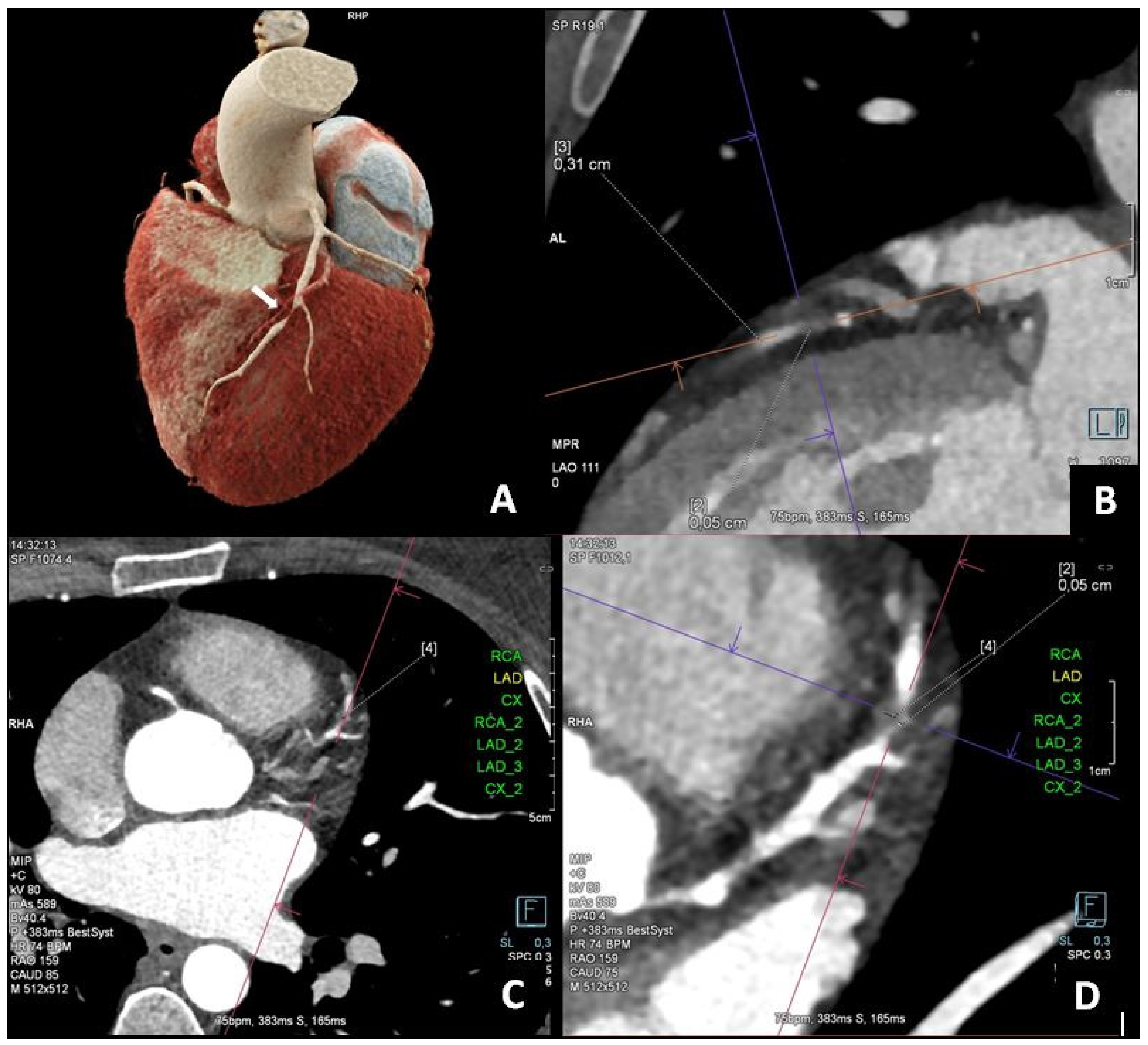
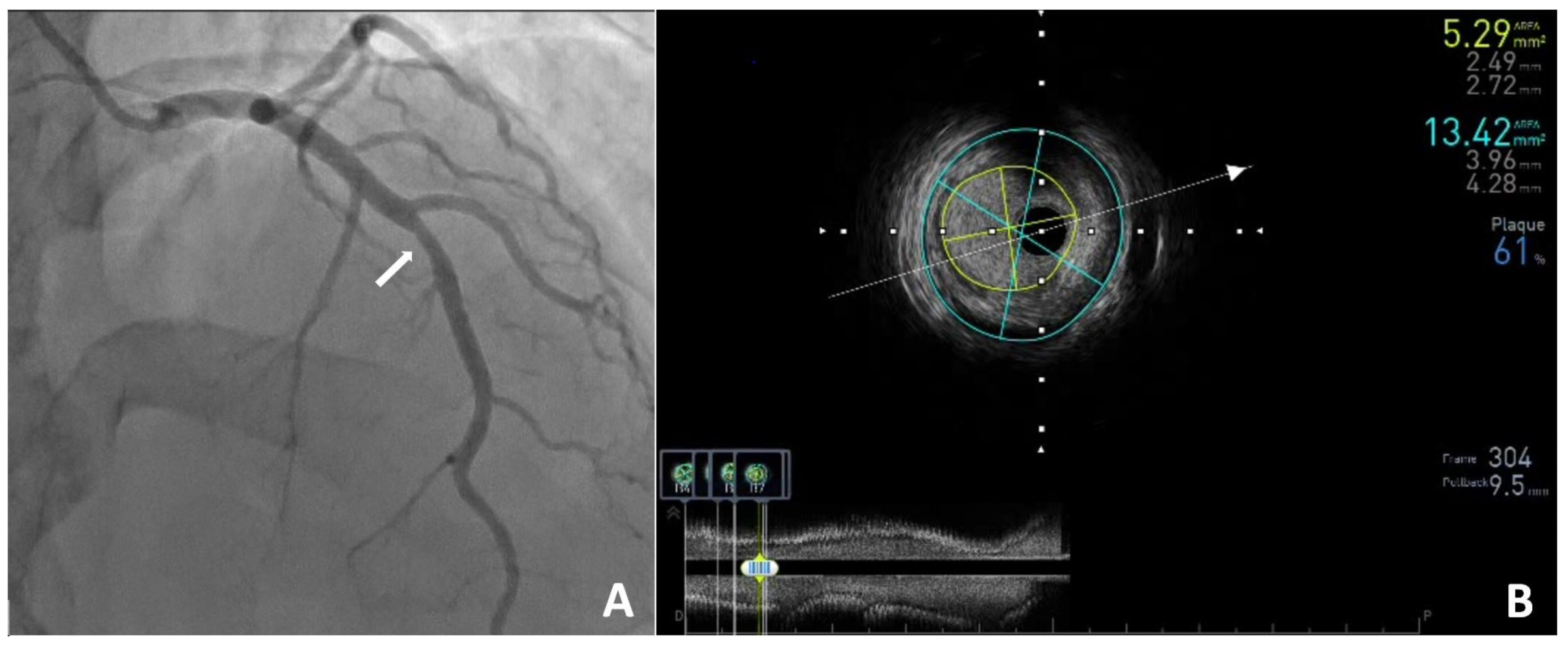
Computed Tomography, Coronary Angiography, and Intravascular Ultrasound in the Diagnosis of Left Anterior Descending Stenosis in a 38-Year-Old Woman with a Calcium Score of Zero
Abstract
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Vrints, C.; Andreotti, F.; Koskinas, K.C.; Rossello, X.; Adamo, M.; Ainslie, J.; Banning, A.P.; Budaj, A.; Buechel, R.R.; Chiariello, G.A.; et al. 2024 ESC Guidelines for the management of chronic coronary syndromes. Eur. Heart J. 2024, 45, 3415–3537. [Google Scholar] [CrossRef] [PubMed]
- Morrone, D.; Gentile, F.; Aimo, A.; Cameli, M.; Barison, A.; Picoi, M.E.; Guglielmo, M.; Villano, A.; DeVita, A.; Mandoli, G.E.; et al. Coronary Physiopathology and Microcirculation Working Group and Cluster Imaging of the Italian Society of Cardiology (SIC). Perspectives in noninvasive imaging for chronic coronary syndromes. Int. J. Cardiol. 2022, 365, 19–29. [Google Scholar] [CrossRef] [PubMed]
- Pawłowski, T.; Legutko, J.; Kochman, J.; Roleder, T.; Pręgowski, J.; Chmielak, Z.; Kubica, J.; Ochała, A.; Parma, R.; Grygier, M.; et al. Clinical use of intracoronary imaging modalities in Poland. Expert opinion of the Association of Cardiovascular Interventions of the Polish Cardiac Society. Pol. Heart J. 2022, 80, 509–519. [Google Scholar] [CrossRef] [PubMed]
- Wojciechowski, A.; Zarotyńska, M.; Chyrchel, B.; Terlecki, M.; Wojciechowska, W.; Rajzer, M. Zero calcium score: A potential pitfall in the diagnosis of coronary artery disease. Pol. Arch. Intern. Med. 2025, 135, 16936. [Google Scholar] [CrossRef] [PubMed]
- Gać, P.; Jaworski, A.; Parfianowicz, A.; Karwacki, J.; Wysocki, A.; Poręba, R. Discrepancies between Coronary Artery Calcium Score and Coronary Artery Disease Severity in Computed Tomography Angiography Studies. Diagnostics 2024, 14, 1928. [Google Scholar] [CrossRef] [PubMed]
- Mortensen, M.B.; Gaur, S.; Frimmer, A.; Bøtker, H.E.; Sørensen, H.T.; Kragholm, K.H.; Niels Peter, S.R.; Steffensen, F.H.; Jensen, R.V.; Mæng, M.; et al. Association of Age with the Diagnostic Value of Coronary Artery Calcium Score for Ruling Out Coronary Stenosis in Symptomatic Patients. JAMA Cardiol. 2022, 7, 36–44. [Google Scholar] [CrossRef] [PubMed]
- Bergström, G.; Persson, M.; Adiels, M.; Björnson, E.; Bonander, C.; Ahlström, H.; Alfredsson, J.; Angerås, O.; Berglund, G.; Blomberg, A.; et al. Prevalence of Subclinical Coronary Artery Atherosclerosis in the General Population. Circulation 2021, 144, 916–929. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zalewska-Adamiec, M.; Dobrzycki, S. Computed Tomography, Coronary Angiography, and Intravascular Ultrasound in the Diagnosis of Left Anterior Descending Stenosis in a 38-Year-Old Woman with a Calcium Score of Zero. Diagnostics 2025, 15, 1169. https://doi.org/10.3390/diagnostics15091169
Zalewska-Adamiec M, Dobrzycki S. Computed Tomography, Coronary Angiography, and Intravascular Ultrasound in the Diagnosis of Left Anterior Descending Stenosis in a 38-Year-Old Woman with a Calcium Score of Zero. Diagnostics. 2025; 15(9):1169. https://doi.org/10.3390/diagnostics15091169
Chicago/Turabian StyleZalewska-Adamiec, Malgorzata, and Slawomir Dobrzycki. 2025. "Computed Tomography, Coronary Angiography, and Intravascular Ultrasound in the Diagnosis of Left Anterior Descending Stenosis in a 38-Year-Old Woman with a Calcium Score of Zero" Diagnostics 15, no. 9: 1169. https://doi.org/10.3390/diagnostics15091169
APA StyleZalewska-Adamiec, M., & Dobrzycki, S. (2025). Computed Tomography, Coronary Angiography, and Intravascular Ultrasound in the Diagnosis of Left Anterior Descending Stenosis in a 38-Year-Old Woman with a Calcium Score of Zero. Diagnostics, 15(9), 1169. https://doi.org/10.3390/diagnostics15091169





