The Metabolic Score for Insulin Resistance (METS-IR), a Predictor of Cardiovascular Events, Relates to Disease Activity in Patients with Rheumatoid Arthritis
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Participants
2.2. Data Collection
2.3. Laboratory Assessments
2.4. Carotid Ultrasound Assessment
2.5. Statistical Analysis
3. Results
3.1. Demographics and Disease-Related Data
3.2. Univariable Analysis of the Relationship Between METS-IR and Cardiovascular Traditional Risk Factors, Lipid Pattern, Insulin Resistance, and Carotid Subclinical Atherosclerosis
3.3. Multivariable Analysis of the Association of Disease-Related Data with METS-IR
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| METS-IR | Metabolic Score for Insulin Resistance |
| CV | Cardiovascular |
| RA | Rheumatoid arthritis |
| DAS28 | Disease Activity Score |
| CDAI | Clinical Disease Activity Index |
| SDAI | Simple Disease Activity Index |
| CI | Confidence interval |
| SCORE2 | Systematic Coronary Risk Evaluation-2 |
| HDL | High-density lipoprotein |
| LDL | Low-density lipoprotein |
| CRP | C-reactive protein |
| HOMA | Homeostatic model assessment |
| cIMT | Carotid intima–media wall |
| IQR | Interquartile range |
| BMI | Body mass index |
| ESR | Erythrocyte sedimentation rate |
| ACPAs | Anti-citrullinated protein antibodies |
| NSAIDs | Nonsteroidal anti-inflammatory drugs |
| DMARDs | Disease-modifying antirheumatic drug |
| TNF | Tumor necrosis factor |
References
- Conforti, A.; Di Cola, I.; Pavlych, V.; Ruscitti, P.; Berardicurti, O.; Ursini, F.; Giacomelli, R.; Cipriani, P. Beyond the Joints, the Extra-Articular Manifestations in Rheumatoid Arthritis. Autoimmun. Rev. 2021, 20, 102735. [Google Scholar] [CrossRef] [PubMed]
- Wolfe, F.; Michaud, K. The Risk of Myocardial Infarction and Pharmacologic and Nonpharmacologic Myocardial Infarction Predictors in Rheumatoid Arthritis: A Cohort and Nested Case-Control Analysis. Arthritis Rheum. 2008, 58, 2612–2621. [Google Scholar] [CrossRef]
- Aviña-Zubieta, J.A.; Choi, H.K.; Sadatsafavi, M.; Etminan, M.; Esdaile, J.M.; Lacaille, D. Risk of Cardiovascular Mortality in Patients with Rheumatoid Arthritis: A Meta-Analysis of Observational Studies. Arthritis Rheum. 2008, 59, 1690–1697. [Google Scholar] [CrossRef]
- Quevedo-Abeledo, J.C.; Sánchez-Pérez, H.; Tejera-Segura, B.; de Armas-Rillo, L.; Ojeda, S.; Erausquin, C.; González-Gay, M.; Ferraz-Amaro, I. Higher Prevalence and Degree of Insulin Resistance in Patients with Rheumatoid Arthritis than in Patients with Systemic Lupus Erythematosus. J. Rheumatol. 2021, 48, 339–347. [Google Scholar] [CrossRef] [PubMed]
- Tejera-Segura, B.; López-Mejías, R.; De Vera-González, A.M.; Jiménez-Sosa, A.; Olmos, J.M.; Hernández, J.L.; Llorca, J.; González-Gay, M.A.; Ferraz-Amaro, I. Relationship between Insulin Sensitivity and β-Cell Secretion in Nondiabetic Subjects with Rheumatoid Arthritis. J. Rheumatol. 2019, 46, 229–236. [Google Scholar] [CrossRef]
- Ferraz-Amaro, I.; González-Juanatey, C.; López-Mejias, R.; Riancho-Zarrabeitia, L.; González-Gay, M.A. Metabolic Syndrome in Rheumatoid Arthritis. Mediat. Inflamm. 2013, 2013, 710928. [Google Scholar] [CrossRef]
- Cai, W.; Tang, X.; Pang, M. Prevalence of Metabolic Syndrome in Patients with Rheumatoid Arthritis: An Updated Systematic Review and Meta-Analysis. Front. Med. 2022, 9, 855141. [Google Scholar] [CrossRef]
- Santos-Moreno, P.; Rodríguez-Vargas, G.-S.; Martínez, S.; Ibatá, L.; Rojas-Villarraga, A. Metabolic Abnormalities, Cardiovascular Disease, and Metabolic Syndrome in Adult Rheumatoid Arthritis Patients: Current Perspectives and Clinical Implications. Open Access Rheumatol. 2022, 14, 255–267. [Google Scholar] [CrossRef]
- Castañeda, S.; Nurmohamed, M.T.; González-Gay, M.A. Cardiovascular Disease in Inflammatory Rheumatic Diseases. Best Pr. Res. Clin. Rheumatol. 2016, 30, 851–869. [Google Scholar] [CrossRef]
- Bello-Chavolla, O.Y.; Almeda-Valdes, P.; Gomez-Velasco, D.; Viveros-Ruiz, T.; Cruz-Bautista, I.; Romo-Romo, A.; Sánchez-Lázaro, D.; Meza-Oviedo, D.; Vargas-Vázquez, A.; Campos, O.A.; et al. METS-IR, a Novel Score to Evaluate Insulin Sensitivity, Is Predictive of Visceral Adiposity and Incident Type 2 Diabetes. Eur. J. Endocrinol. 2018, 178, 533–544. [Google Scholar] [CrossRef]
- Hou, Y.; Li, R.; Xu, Z.; Chen, W.; Li, Z.; Jiang, W.; Meng, Y.; Han, J. Association of METS-IR Index with Type 2 Diabetes: A Cross-Sectional Analysis of National Health and Nutrition Examination Survey Data from 2009 to 2018. PLoS ONE 2024, 19, e0308597. [Google Scholar] [CrossRef]
- Qian, T.; Sheng, X.; Shen, P.; Fang, Y.; Deng, Y.; Zou, G. Mets-IR as a Predictor of Cardiovascular Events in the Middle-Aged and Elderly Population and Mediator Role of Blood Lipids. Front. Endocrinol. 2023, 14, 1224967. [Google Scholar]
- Aletaha, D.; Neogi, T.; Silman, A.J.; Funovits, J.; Felson, D.T.; Bingham, C.O.; Birnbaum, N.S.; Burmester, G.R.; Bykerk, V.P.; Cohen, M.D.; et al. 2010 Rheumatoid Arthritis Classification Criteria: An American College of Rheumatology/European League Against Rheumatism Collaborative Initiative. Ann. Rheum. Dis. 2010, 69, 1580–1588. [Google Scholar] [CrossRef]
- Prevoo, M.L.L.; Van’T Hof, M.A.; Kuper, H.H.; Van Leeuwen, M.A.; Van De Putte, L.B.A.; Van Riel, P.L.C.M. Modified Disease Activity Scores That Include Twenty-eight-joint Counts Development and Validation in a Prospective Longitudinal Study of Patients with Rheumatoid Arthritis. Arthritis Rheum. 1995, 38, 44–48. [Google Scholar] [CrossRef] [PubMed]
- Smolen, J.S.; Breedveld, F.C.; Schiff, M.H.; Kalden, J.R.; Emery, P.; Eberl, G.; van Riel, P.L.; Tugwell, P. A Simplified Disease Activity Index for Rheumatoid Arthritis for Use in Clinical Practice. Rheumatology 2003, 42, 244–257. [Google Scholar] [CrossRef]
- Aletaha, D.; Smolen, J. The Simplified Disease Activity Index (SDAI) and the Clinical Disease Activity Index (CDAI): A Review of Their Usefulness and Validity in Rheumatoid Arthritis. Clin. Exp. Rheumatol. 2005, 23, S100–S108. [Google Scholar]
- Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults. Executive Summary of the Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III). JAMA 2001, 285, 2486–2497. [CrossRef]
- SCORE2 Working Group and ESC Cardiovascular Risk Collaboration. SCORE2 Risk Prediction Algorithms: New Models to Estimate 10-Year Risk of Cardiovascular Disease in Europe. Eur. Heart J. 2021, 42, 2439–2454. [Google Scholar] [CrossRef]
- Wallace, T.M.; Levy, J.C.; Matthews, D.R. Use and Abuse of HOMA Modeling. Diabetes Care 2004, 27, 1487–1495. [Google Scholar]
- Touboul, P.J.; Hennerici, M.G.; Meairs, S.; Adams, H.; Amarenco, P.; Bornstein, N.; Csiba, L.; Desvarieux, M.; Ebrahim, S.; Hernandez Hernandez, R.; et al. Mannheim Carotid Intima-Media Thickness and Plaque Consensus (2004-2006-2011). An Update on Behalf of the Advisory Board of the 3rd, 4th and 5th Watching the Risk Symposia, at the 13th, 15th and 20th European Stroke Conferences, Mannheim, Germany, 2004, Brussels, Belgium, 2006, and Hamburg, Germany, 2011. Cerebrovasc. Dis. 2012, 34, 290–296. [Google Scholar] [CrossRef]
- Cheng, H.; Jia, Z.; Li, Y.T.; Yu, X.; Wang, J.J.; Xie, Y.J.; Hernandez, J.; Wang, H.H.X. Metabolic Score for Insulin Resistance and New-Onset Type 2 Diabetes in a Middle-Aged and Older Adult Population: Nationwide Prospective Cohort Study and Implications for Primary Care. JMIR Public Health Surveill. 2024, 10, e49617. [Google Scholar] [CrossRef]
- Rao, K.; Yang, J.; Wu, M.; Zhang, H.; Zhao, X.; Dong, Y. Association Between the Metabolic Score for Insulin Resistance and Hypertension in Adults: A Meta-Analysis. Horm. Metab. Res. 2023, 55, 256–265. [Google Scholar] [CrossRef] [PubMed]
- Ezhova, N.E.; Shavarova, E.K.; Kobalava, Z.D.; Bazdyreva, E.I.; Shavarov, A.A. Metabolic Score for Insulin Resistance (METS-IR) Associations with Subclinical Left Ventricular and Left Atrial Remodelling in Young Subjects with Hypertension. Ann. Clin. Cardiol. 2024, 6, 82–87. [Google Scholar] [CrossRef]
- Ferraz-Amaro, I.; García-Dopico, J.A.; Medina-Vega, L.; González-Gay, M.A.; Díaz-González, F. Impaired Beta Cell Function Is Present in Nondiabetic Rheumatoid Arthritis Patients. Arthritis Res. Ther. 2013, 15, R17. [Google Scholar] [CrossRef]
- Tejera-Segura, B.; Macía-Díaz, M.; Machado, J.D.; de Vera-González, A.; García-Dopico, J.A.; Olmos, J.M.; Hernández, J.L.; Díaz-González, F.; González-Gay, M.A.; Ferraz-Amaro, I. HDL Cholesterol Efflux Capacity in Rheumatoid Arthritis Patients: Contributing Factors and Relationship with Subclinical Atherosclerosis. Arthritis Res. Ther. 2017, 19, 113. [Google Scholar] [CrossRef]
- Zhou, Y.; Gao, J. Association between Metabolic Score for Insulin Resistance and Cardiovascular Disease Mortality in Patients with Rheumatoid Arthritis: Evidence from the NHANES 1999–2018. Front. Endocrinol. 2024, 15, 1444800. [Google Scholar] [CrossRef]
- Ke, W.; Xu, L.; Luo, N. Predictive Value of Insulin Resistance Metabolic Score for Cardiovascular Disease in Chinese Arthritis Patients: A Prospective Cohort Study. Rheumatology 2025, keaf048. [Google Scholar] [CrossRef]
| Rheumatoid Arthritis | |
|---|---|
| (n = 515) | |
| METS-IR | 42 ± 10 |
| Age, years | 56 ± 10 |
| Female, n (%) | 417 (81) |
| BMI, kg/m2 | 28 ± 5 |
| Abdominal circumference, cm | 96 ± 13 |
| Hip circumference, cm | 105 ± 11 |
| Abdominal-to-hip ratio | 1.14 ± 4.93 |
| Cardiovascular data | |
| CV risk factors, n (%) | |
| Current smoker | 112 (22) |
| Obesity | 160 (34) |
| Hypertension | 177 (34) |
| Diabetes Mellitus | 70 (14) |
| Metabolic syndrome, n (%) | 272 (56) |
| Statins, n (%) | 166 (32) |
| Aspirin, n (%) | 38 (11) |
| SCORE2, % | 3.9 (1.9–6.2) |
| Low to moderate | 292 (57) |
| High | 144 (28) |
| Very high | 79 (15) |
| Carotid ultrasound | |
| cIMT, microns | 703 ± 141 |
| Carotid plaque, n (%) | 222 (46) |
| Analytical | |
| Total cholesterol, mg/dL | 202 ± 39 |
| Triglycerides, mg/dL | 145 ± 83 |
| HDL-cholesterol, mg/dL | 56 ± 15 |
| LDL-cholesterol, mg/dL | 117 ± 34 |
| LDL:HDL cholesterol ratio | 2.22 ± 0.92 |
| Non-HDL cholesterol, mg/dL | 146 ± 39 |
| Lipoprotein (a), mg/dL | 33 (11–96) |
| Apolipoprotein A1, mg/dL | 172 ± 32 |
| Apolipoprotein B, mg/dL | 106 ± 43 |
| Apo B:Apo A ratio | 0.63 ± 0.26 |
| Insulin resistance indices | |
| Glucose, mg/dL | 94 ± 23 |
| Insulin, µU/mL | 16 ± 26 |
| C-peptide, ng/mL | 3.42 ± 2.70 |
| HOMA2-IR | 1.17 (0.76–2.00) |
| HOMA2-S% | 100 ± 71 |
| HOMA2-B%-C-peptide | 163 ± 76 |
| Disease-related data | |
| Disease duration, years | 8 (4–15) |
| CRP at time of study, mg/L | 2.3 (1.0–5.4) |
| ESR at time of study, mm/1st hour | 17 (7–32) |
| Rheumatoid factor, n (%) | 377 (75) |
| ACPAs, n (%) | 326 (69) |
| DAS28-ESR | 3.27 ± 1.38 |
| Remission | 180 (36) |
| Low disease activity | 89 (18) |
| Moderate disease activity | 182 (36) |
| High disease activity | 55 (11) |
| DAS28-CRP | 2.85 ± 1.14 |
| Remission | 246 (49) |
| Low disease activity | 86 (17) |
| Moderate disease activity | 151 (30) |
| High disease activity | 24 (5) |
| SDAI | 12 (6–19) |
| Remission | 53 (11) |
| Low disease activity | 166 (35) |
| Moderate disease activity | 197 (41) |
| High disease activity | 63 (13) |
| CDAI | 7 (3–14) |
| Remission | 122 (24) |
| Low disease activity | 212 (42) |
| Moderate disease activity | 137 (27) |
| High disease activity | 38 (7) |
| History of extraarticular manifestations, n (%) | 65 (14) |
| Erosions, n (%) | 195 (41) |
| Current drugs, n (%) | |
| Prednisone | 193 (37) |
| Prednisone doses, mg/day | 5.34 ± 3.67 |
| NSAIDs | 210 (41) |
| DMARDs | 452 (88) |
| Methotrexate | 378 (73) |
| Leflunomide | 109 (21) |
| Hydroxychloroquine | 54 (10) |
| Salazopyrin | 31 (6) |
| Anti-TNF therapy | 101 (20) |
| Tocilizumab | 25 (5) |
| Rituximab | 11 (2) |
| Abatacept | 17 (3) |
| Baricitinib | 8 (2) |
| Tofacitinib | 5 (1) |
| METS-IR | ||
|---|---|---|
| Beta Coefficient (95% CI), p | ||
| Age, years | 0.1 (0.03–0.2) | 0.007 |
| Female, n (%) | −4 (−1–6) | 0.002 |
| BMI, kg/m2 | 2 (2–2) | <0.001 |
| Abdominal circumference, cm | 1 (1–1) | <0.001 |
| Hip circumference, cm | 1 (1–1) | <0.001 |
| Abdominal-to-hip ratio | 0.2 (−0.1–0.5) | 0.31 |
| Cardiovascular data | ||
| CV risk factors, n (%) | ||
| Current smoker | −4 (−6–(−1)) | 0.002 |
| Obesity | 15 (14–17) | <0.001 |
| Hypertension | 5 (3–7) | <0.001 |
| Diabetes Mellitus | 5 (2–7) | 0.001 |
| Metabolic syndrome | 9 (7–11) | <0.001 |
| Statins, n (%) | 3 (1–5) | 0.001 |
| Aspirin, n (%) | 4 (0–8) | 0.040 |
| SCORE2, % | 0.5 (0.2–0.7) | <0.001 |
| Low to moderate | ref. | |
| High | 3 (0.5–5) | 0.015 |
| Very high | 3 (0.02–6) | 0.048 |
| Analytical | ||
| Total cholesterol, mg/dL | −0.01 (−0.03–0.01) | 0.44 |
| Triglycerides, mg/dL | 0.06 (0.05–0.07) | <0.001 |
| HDL-cholesterol, mg/dL | −0.3 (−0.4–−0.3) | <0.001 |
| LDL-cholesterol, mg/dL | −0.01 (−0.04–0.02) | 0.38 |
| LDL:HDL cholesterol ratio | 4 (3–5) | <0.001 |
| Non-HDL cholesterol, mg/dL | 0.05 (0.02–0.07) | <0.001 |
| Lipoprotein (a), mg/dL | 0.01 (−0.01–0.02) | 0.29 |
| Apolipoprotein A1, mg/dL | −0.1 (−0.2–−0.1) | <0.001 |
| Apolipoprotein B, mg/dL | 0.01 (−0.01–0.03) | 0.32 |
| Apo B:Apo A1 ratio | 14 (11–17) | <0.001 |
| Insulin resistance indices | ||
| Glucose, mg/dL | 0.1 (0.06–0.14) | <0.001 |
| Insulin, µU/mL | 0.11 (0.08–0.15) | <0.001 |
| C-peptide, ng/mL | 1 (1–2) | <0.001 |
| HOMA2-IR | 2 (2–3) | <0.001 |
| HOMA2-S% | −0.06 (−0.07–−0.05) | <0.001 |
| HOMA2-B%-C-peptide | 0.04 (0.02–0.05) | <0.001 |
| Carotid ultrasound | ||
| cIMT, microns | 0.01 (0.002–0.02) | 0.01 |
| Carotid plaque, n (%) | 0.6 (−1.3–2.5) | 0.54 |
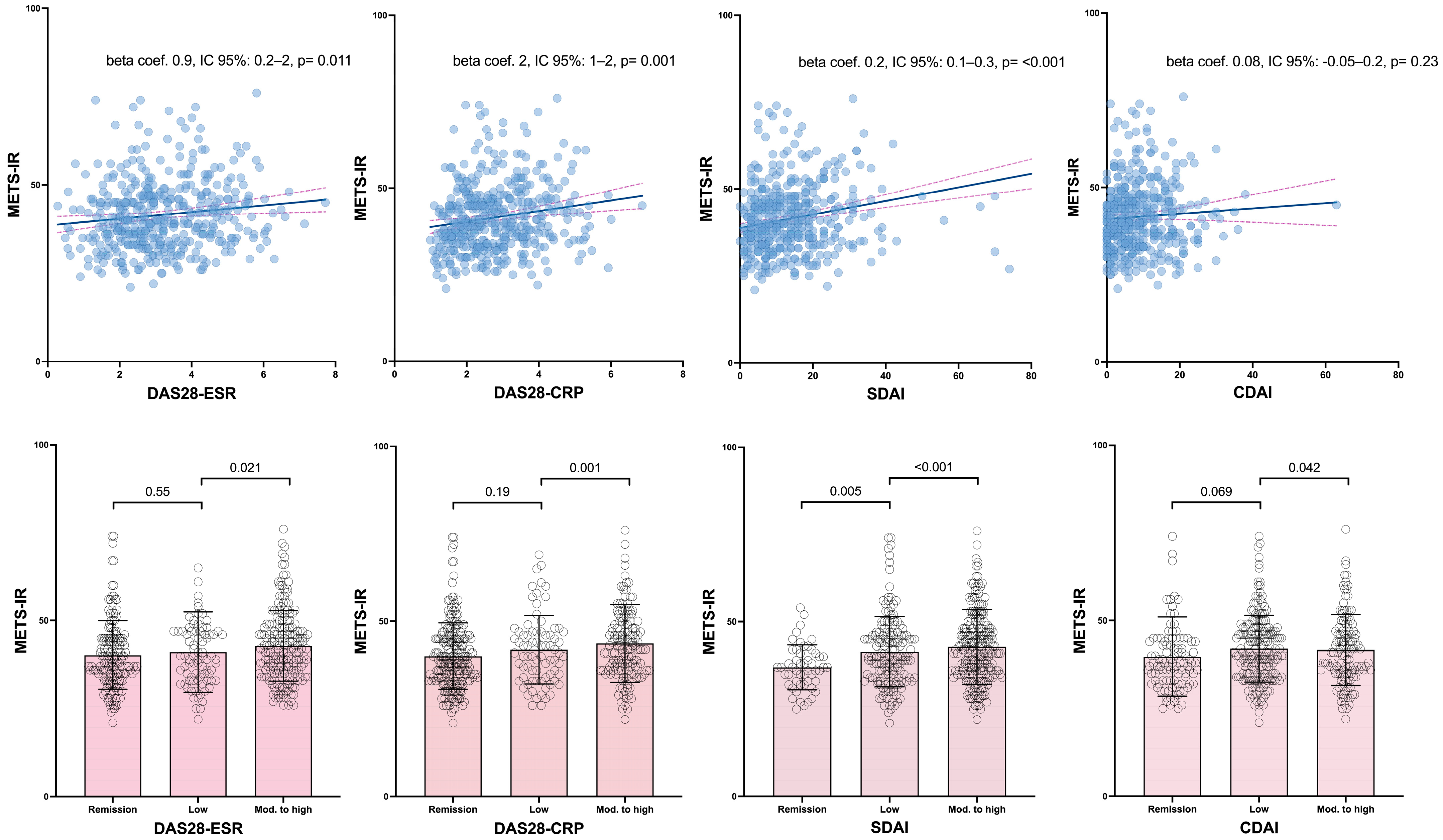
| METS-IR | ||||
|---|---|---|---|---|
| Univariable | Multivariable | |||
| Beta Coefficient (95% Confidence Interval), p | ||||
| Disease duration, years | −0.008 (−0.1–0.1) | 0.88 | ||
| CRP at time of study, mg/L | 0.2 (0.2–0.3) | <0.001 | 0.2 (0.1–0.3) | <0.001 |
| ESR at time of study, mm/1° hour | 0.04 (−0.01–0.09) | 0.15 | 0.03 (−0.02–0.08) | 0.29 |
| Rheumatoid factor, n (%) | −1 (−4–0.8) | 0.23 | ||
| ACPAs, n (%) | −2 (−4–0.3) | 0.090 | −0.8 (−3–1) | 0.43 |
| DAS28-ESR | 0.9 (0.2–2) | 0.011 | 0.8 (0.09–2) | 0.028 |
| Remission | ref. | ref. | ||
| Low disease activity | 1 (−2–4) | 0.55 | 0.9 (−2–4) | 0.50 |
| Moderate and high disease activity | 3 (0.4–5) | 0.021 | 2 (0.09–4) | 0.041 |
| DAS28-PCR | 2 (1–2) | 0.001 | 1 (0.5–2) | 0.002 |
| Remission | ref. | ref. | ||
| Low disease activity | 2 (−1–4) | 0.19 | 2 (−1–4) | 0.24 |
| Moderate and high disease activity | 4 (1–6) | 0.001 | 3 (1–5) | 0.002 |
| SDAI | 0.2 (0.1–0.3) | <0.001 | 0.2 (0.1–0.2) | <0.001 |
| Remission | ref. | ref. | ||
| Low disease activity | 5 (1–8) | 0.005 | 3 (0.3–6) | 0.030 |
| Moderate and high disease activity | 6 (3–9) | <0.001 | 5 (2–8) | 0.002 |
| CDAI | 0.08 (−0.05–0.2) | 0.23 | 0.07 (−0.06–0.2) | 0.28 |
| Remission | ref. | ref. | ||
| Low disease activity | 2 (−0.2–5) | 0.069 | 1 (−1–4) | 0.32 |
| Moderate and high disease activity | 3 (0.09–5) | 0.042 | 2 (−0.6–4) | 0.14 |
| History of extraarticular manifestations, n (%) | −0.3 (−3–3) | 0.86 | ||
| Erosions, n (%) | −2 (−4–0.3) | 0.089 | −2 (−4–0.2) | 0.074 |
| Current drugs, n (%) | ||||
| Prednisone | −2 (−4–0.004) | 0.050 | −2 (−4–(−0.07)) | 0.043 |
| Prednisone doses, mg/day | −0.1 (−0.4–0.3) | 0.72 | ||
| NSAIDs | 0.4 (−1.5–2.3) | 0.69 | ||
| DMARDs | −1 (−3–2) | 0.73 | ||
| Methotrexate | −0.2 (−2.3–1.9) | 0.84 | ||
| Leflunomide | −0.6 (−2.9–1.6) | 0.58 | ||
| Hydroxychloroquine | −0.4 (−3.4–2.6) | 0.80 | ||
| Salazopyrin | −2 (−6–2) | 0.38 | ||
| Anti-TNF therapy | −0.1 (−2.5–2.3) | 0.92 | ||
| Tocilizumab | 0.1 (−4.2–4.4) | 0.98 | ||
| Rituximab | −0.1 (−6.2–6) | 0.98 | ||
| Abatacept | 0.2 (−4.9–5.3) | 0.94 | ||
| Baricitinib | 1 (−6–9) | 0.72 | ||
| Tofacitinib | −1 (−8–6) | 0.73 | ||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Aznar-Esquivel, A.; Gómez-Bernal, F.; García-González, M.; Hernández-Diaz, M.; Heras-Recuero, E.; de Vera-González, A.; González-Delgado, A.; Quevedo-Rodríguez, A.; Quevedo-Abeledo, J.C.; Castañeda, S.; et al. The Metabolic Score for Insulin Resistance (METS-IR), a Predictor of Cardiovascular Events, Relates to Disease Activity in Patients with Rheumatoid Arthritis. Diagnostics 2025, 15, 861. https://doi.org/10.3390/diagnostics15070861
Aznar-Esquivel A, Gómez-Bernal F, García-González M, Hernández-Diaz M, Heras-Recuero E, de Vera-González A, González-Delgado A, Quevedo-Rodríguez A, Quevedo-Abeledo JC, Castañeda S, et al. The Metabolic Score for Insulin Resistance (METS-IR), a Predictor of Cardiovascular Events, Relates to Disease Activity in Patients with Rheumatoid Arthritis. Diagnostics. 2025; 15(7):861. https://doi.org/10.3390/diagnostics15070861
Chicago/Turabian StyleAznar-Esquivel, Antonio, Fuensanta Gómez-Bernal, María García-González, Marta Hernández-Diaz, Elena Heras-Recuero, Antonia de Vera-González, Alejandra González-Delgado, Adrián Quevedo-Rodríguez, Juan C. Quevedo-Abeledo, Santos Castañeda, and et al. 2025. "The Metabolic Score for Insulin Resistance (METS-IR), a Predictor of Cardiovascular Events, Relates to Disease Activity in Patients with Rheumatoid Arthritis" Diagnostics 15, no. 7: 861. https://doi.org/10.3390/diagnostics15070861
APA StyleAznar-Esquivel, A., Gómez-Bernal, F., García-González, M., Hernández-Diaz, M., Heras-Recuero, E., de Vera-González, A., González-Delgado, A., Quevedo-Rodríguez, A., Quevedo-Abeledo, J. C., Castañeda, S., González-Gay, M. Á., & Ferraz-Amaro, I. (2025). The Metabolic Score for Insulin Resistance (METS-IR), a Predictor of Cardiovascular Events, Relates to Disease Activity in Patients with Rheumatoid Arthritis. Diagnostics, 15(7), 861. https://doi.org/10.3390/diagnostics15070861








