Efficacy of Percutaneous Vertebroplasty Versus Placebo and Conservative Treatment in Osteoporotic Vertebral Fractures: An Updated Systematic Review and Meta-Analysis of Randomized Clinical Trials
Abstract
1. Introduction
2. Methods
2.1. Study Design and Eligibility Criteria
2.2. Database Search Strategy
2.3. Risk of Bias Assessment
2.4. Variables of Interest and Data Extraction
2.5. Management of Missing Data
- When data were reported as the difference in means from baseline, SDs were calculated using the formula:
- 3.
- When only the 95%CI of the mean value of the variable of interest at follow-up was provided, the corresponding SD was estimated from the standard error using the following formulas:
- 4.
- 5.
2.6. Statistical Analysis
- Control group: CT vs. placebo.
- Number of institutions involved: single-center vs. multi-center.
- Geographic region: Western vs. Eastern countries.
- Risk of bias: high risk vs. low/uncertain risk (according to RoB2).
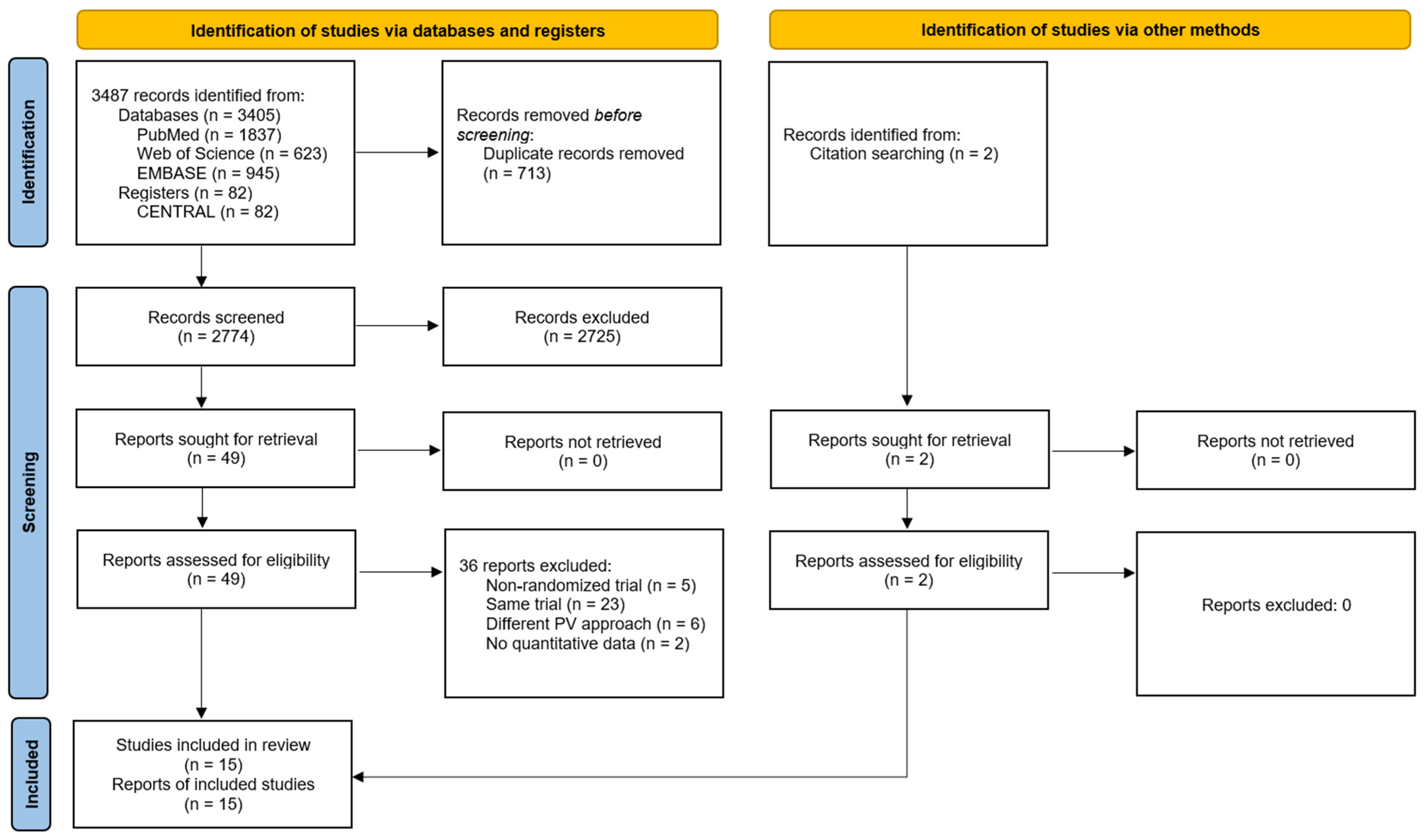
3. Results
3.1. Characteristics of the Included Studies
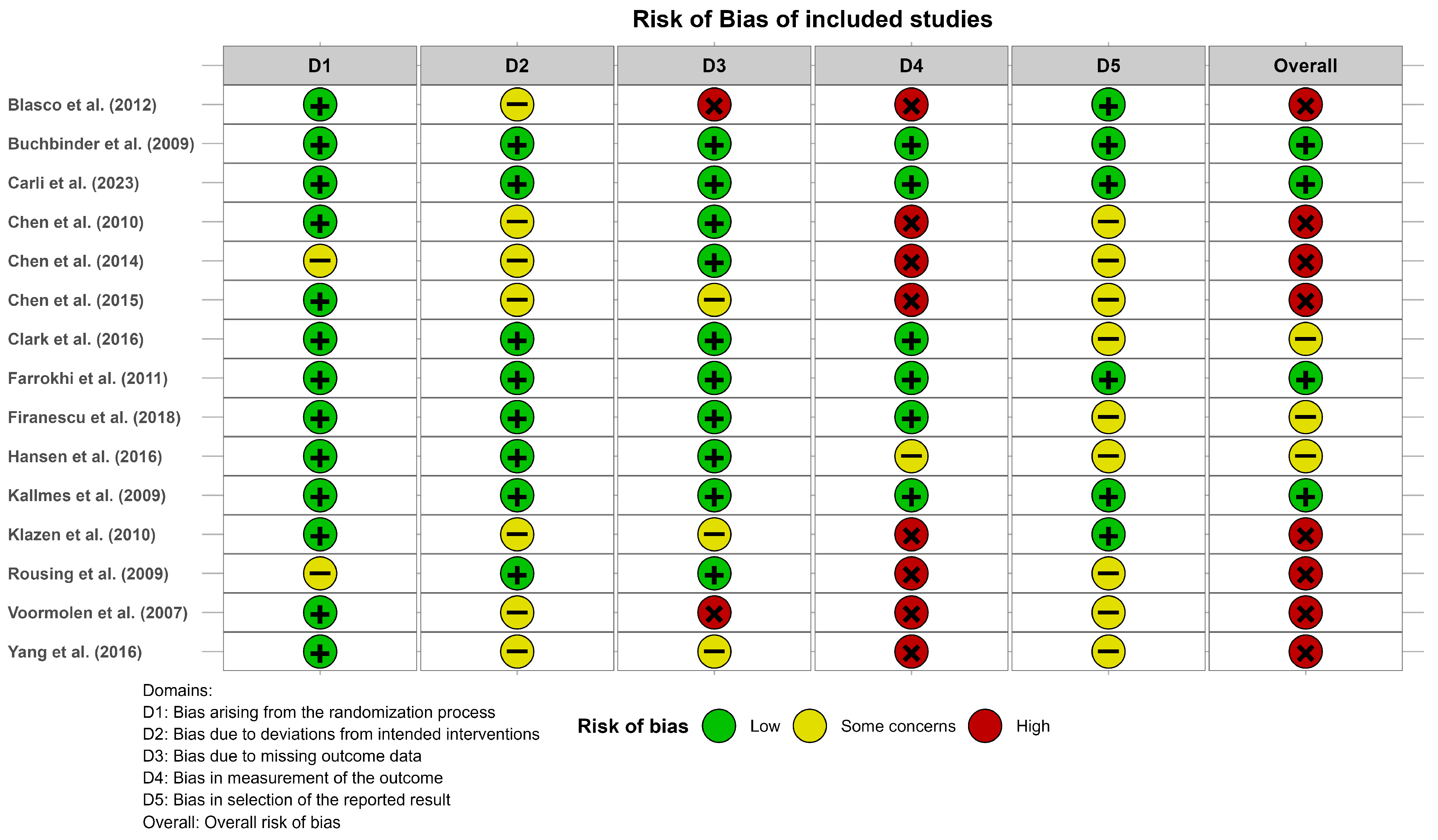
3.2. Results of Risk of Bias Assessment
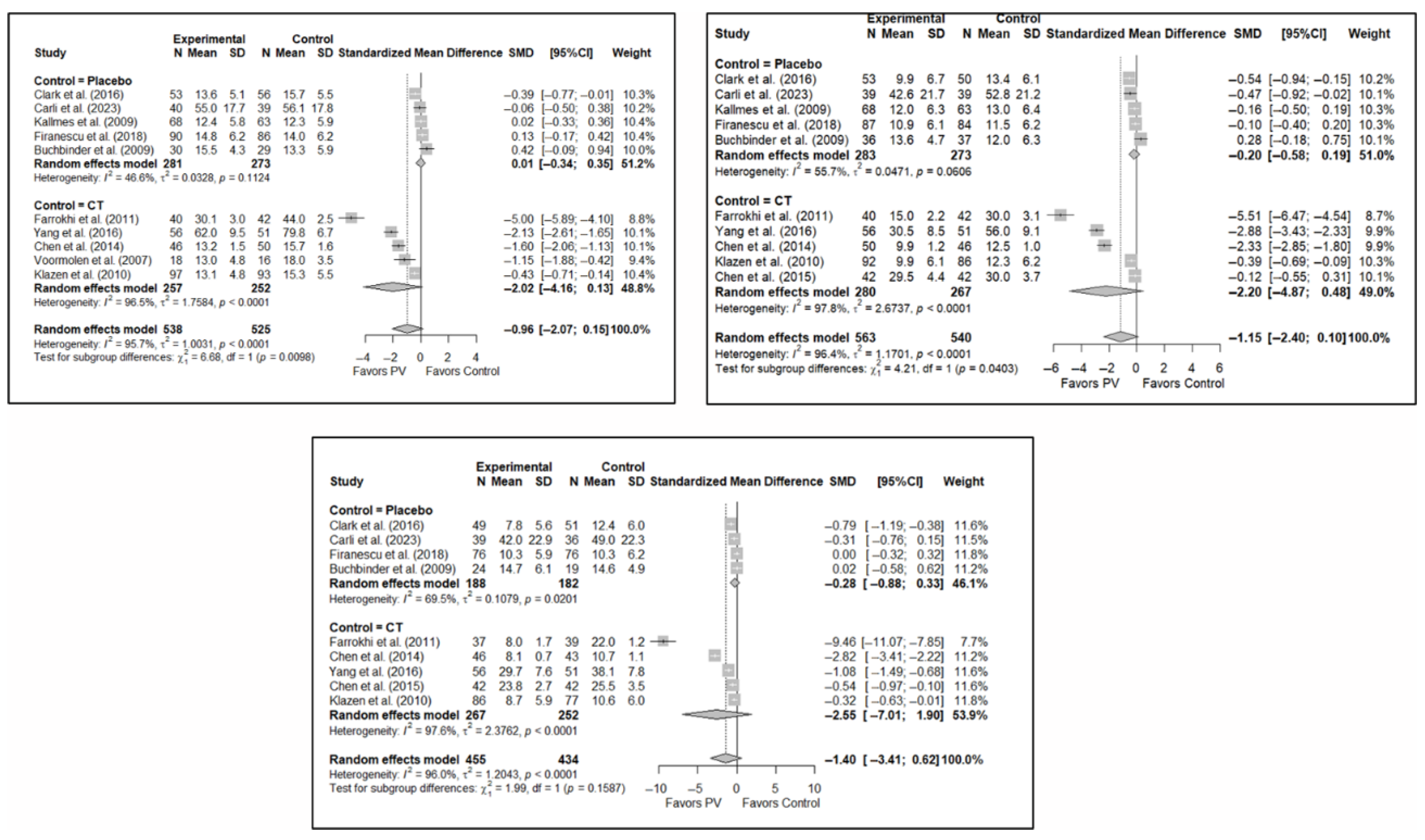
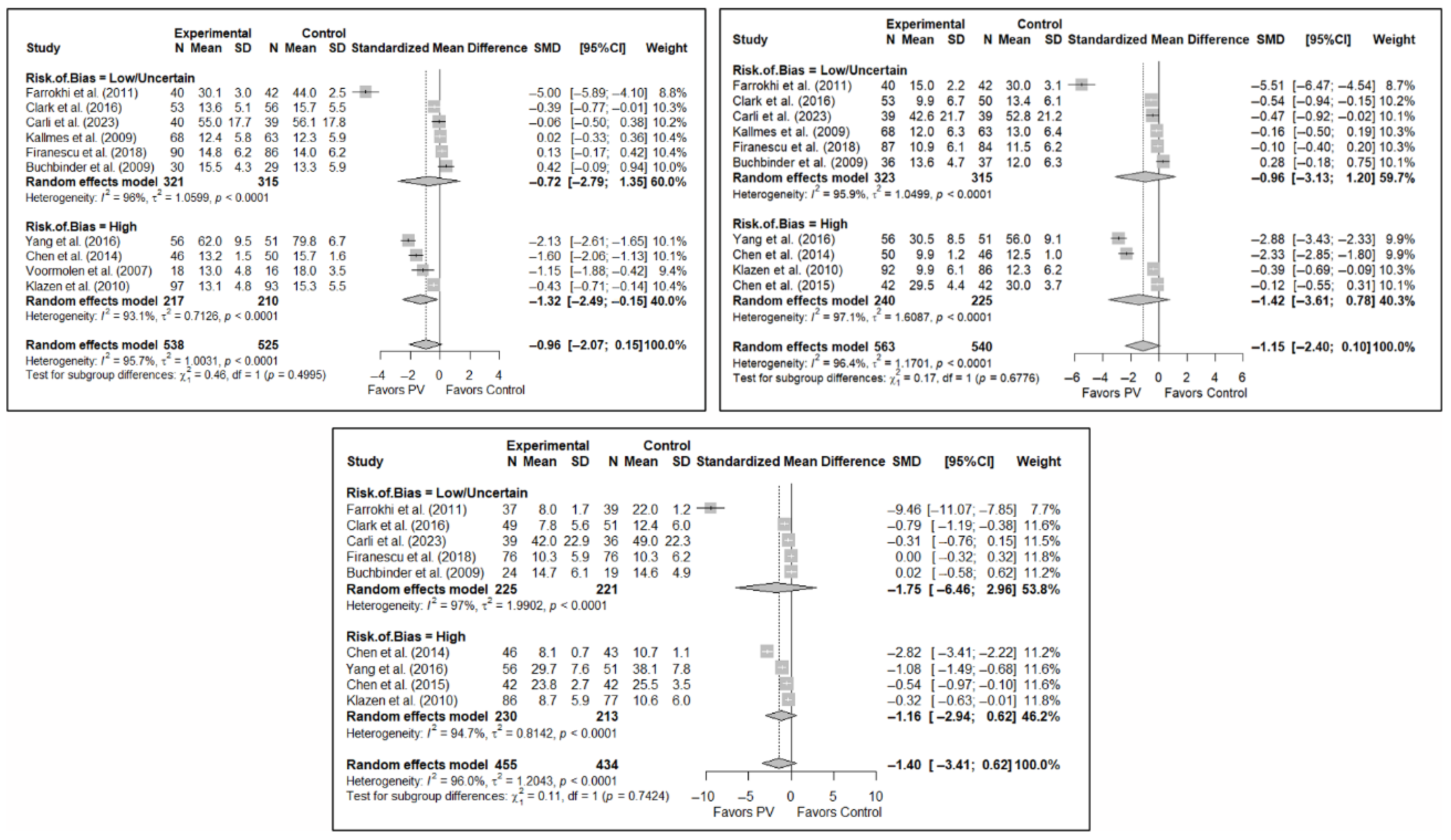
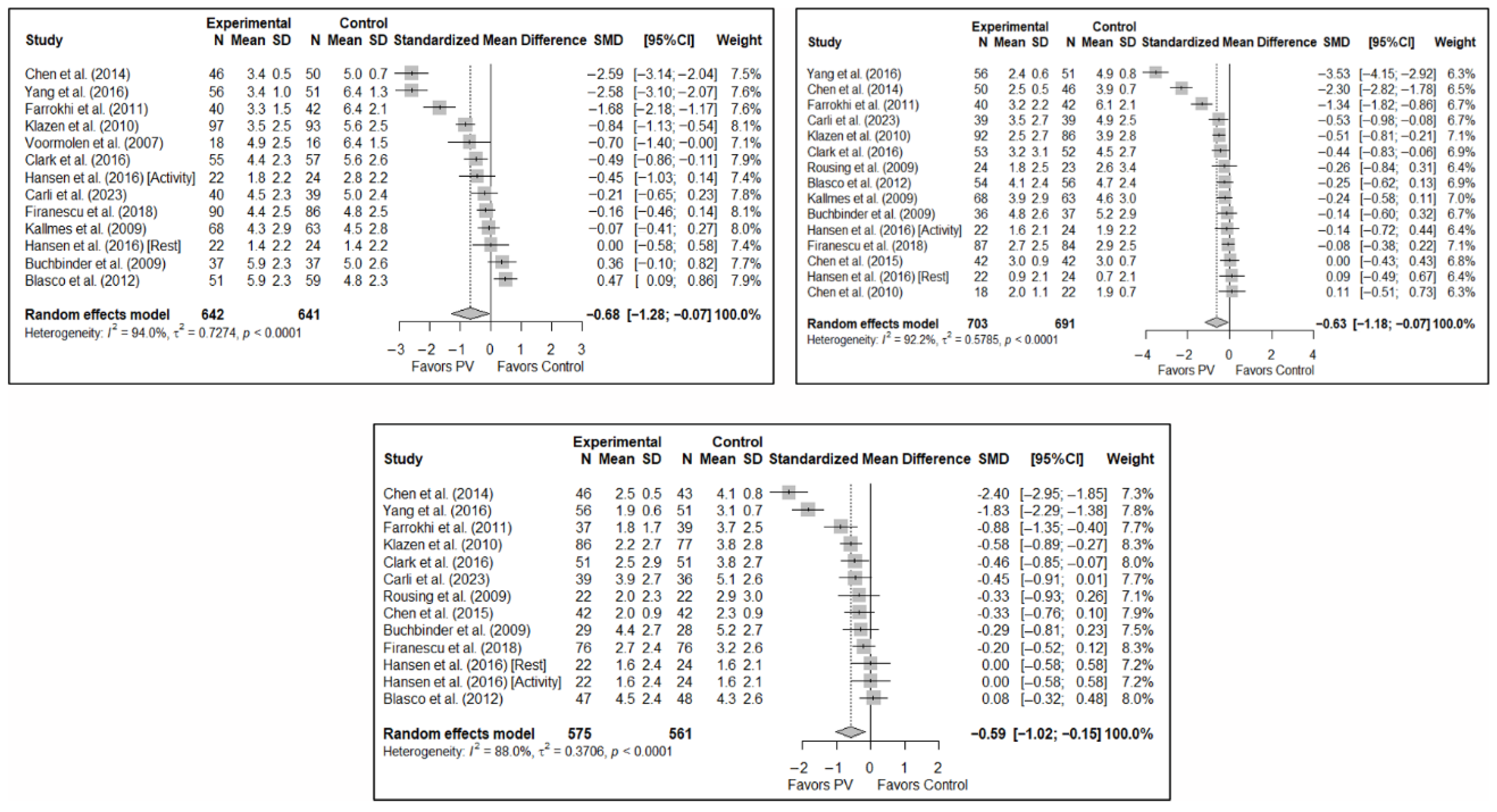
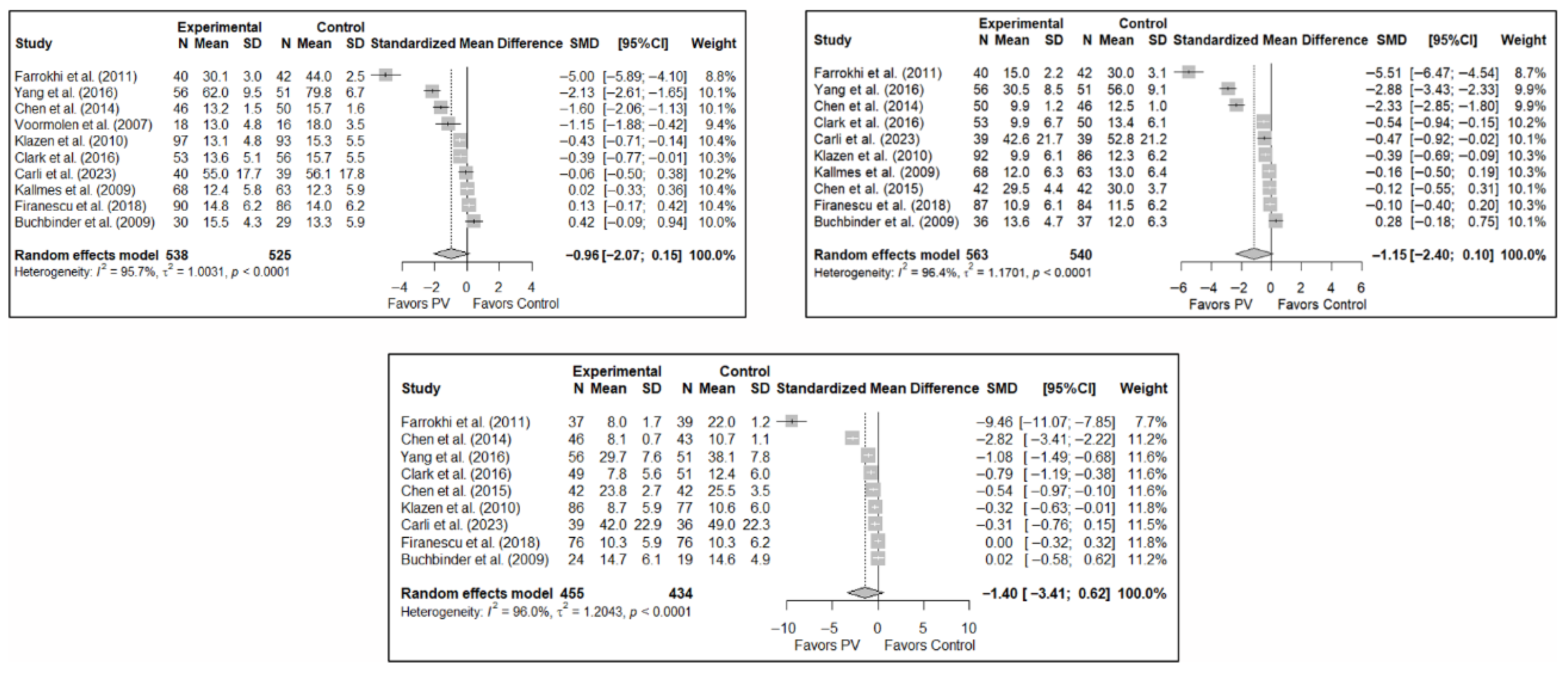
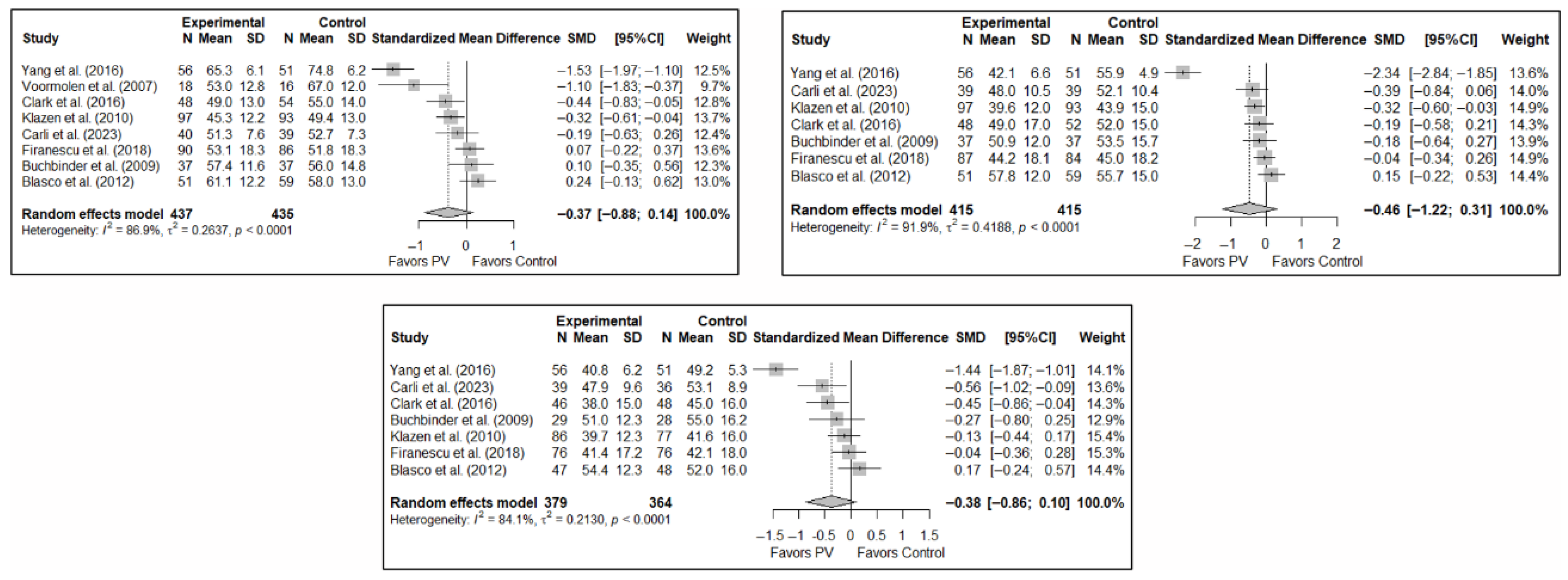
3.3. Efficacy of Vertebroplasty in Pain Relief
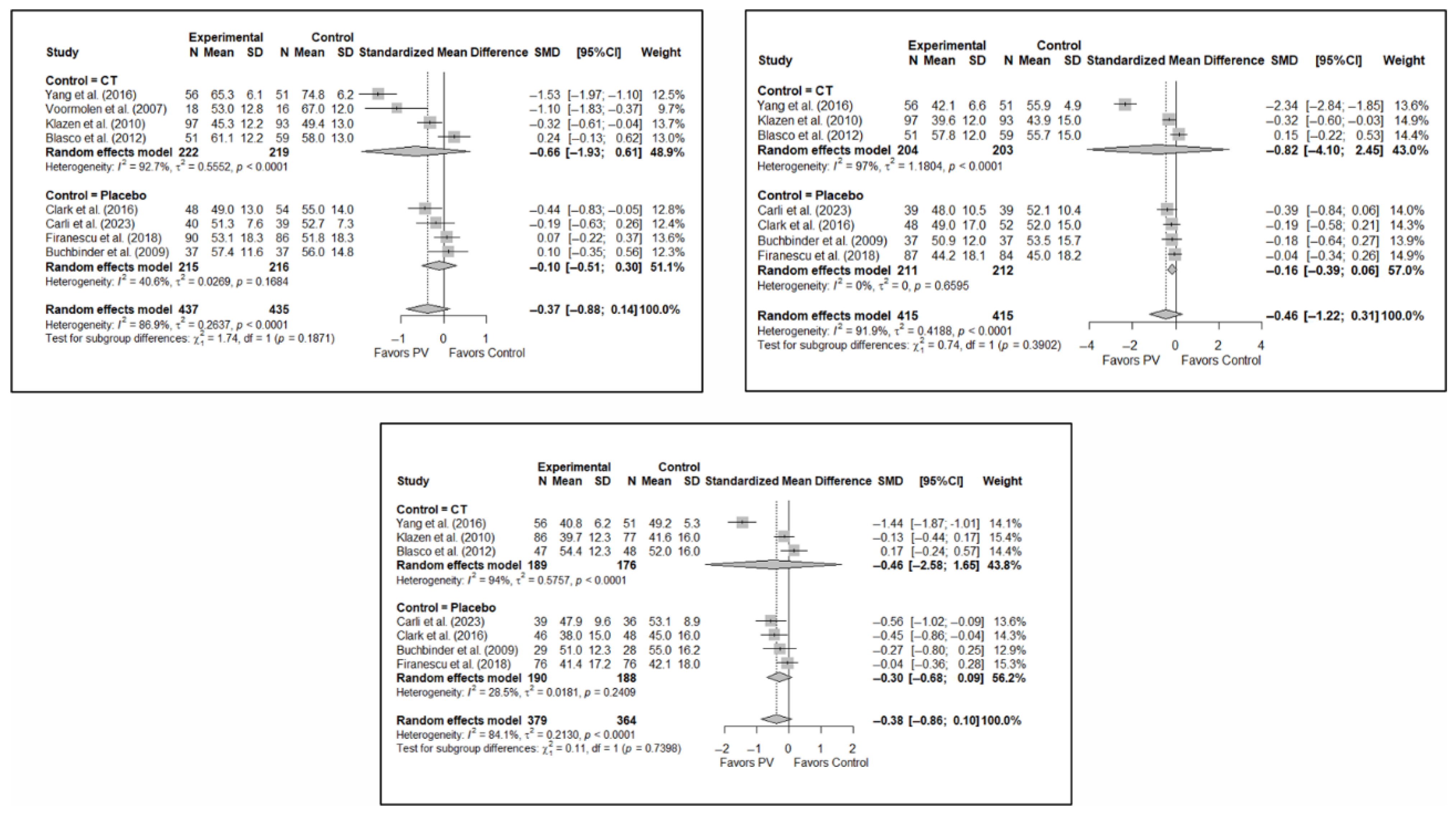
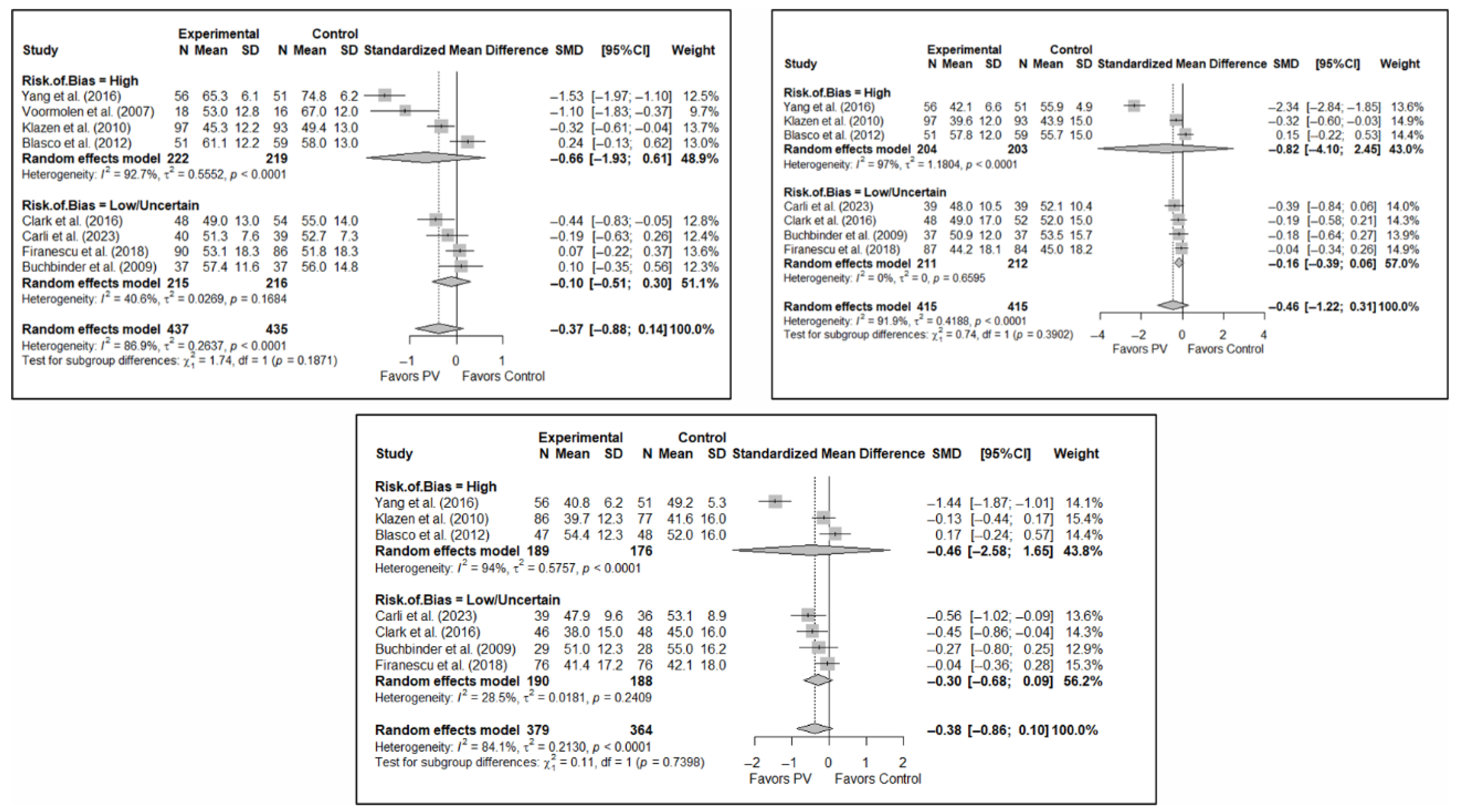
3.4. Efficacy of Percutaneous Vertebroplasty in Functionality Improvement
3.5. Efficacy of Percutaneous Vertebroplasty in Quality of Life Improvement
3.6. Subgroup Analyses
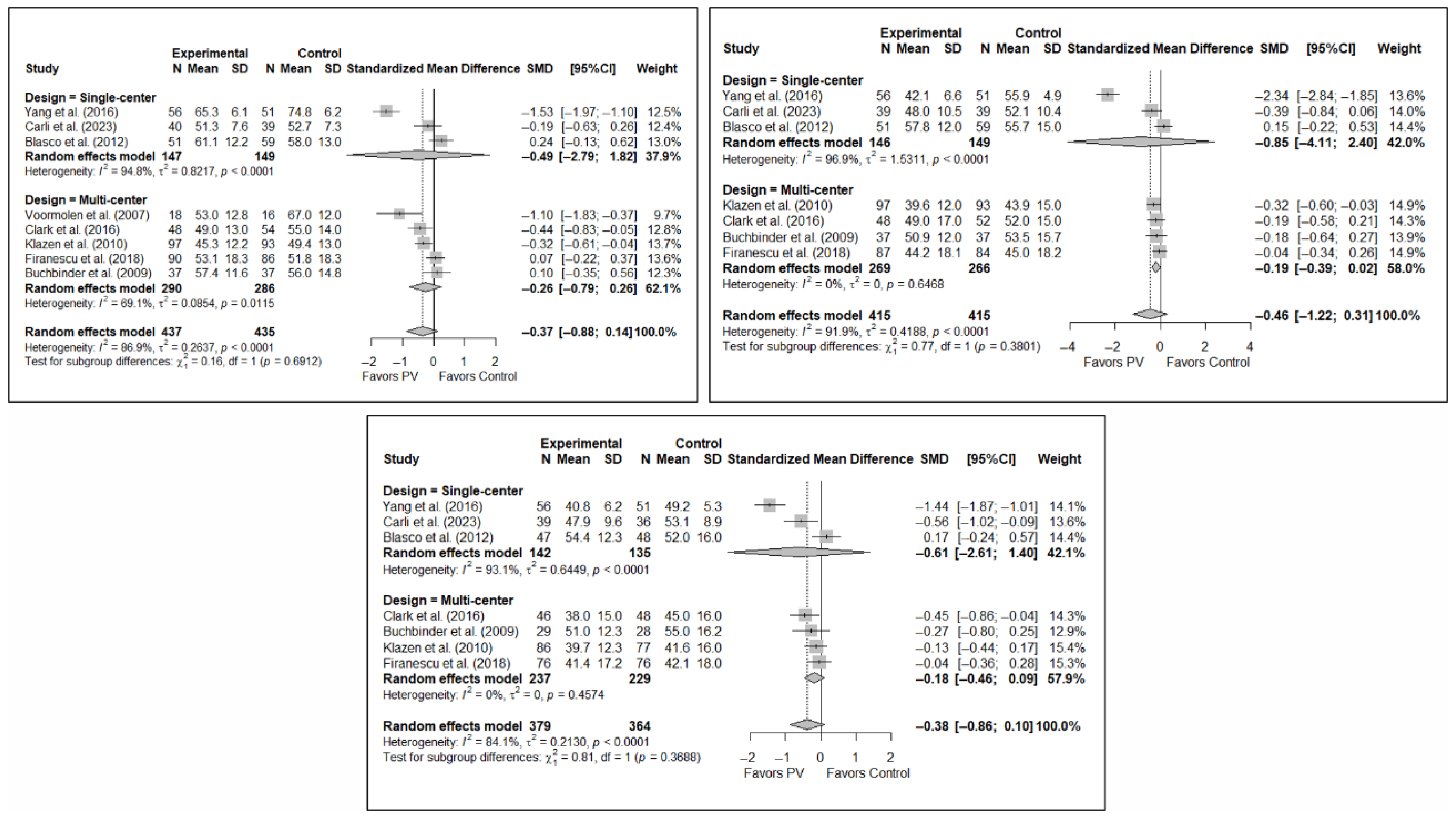
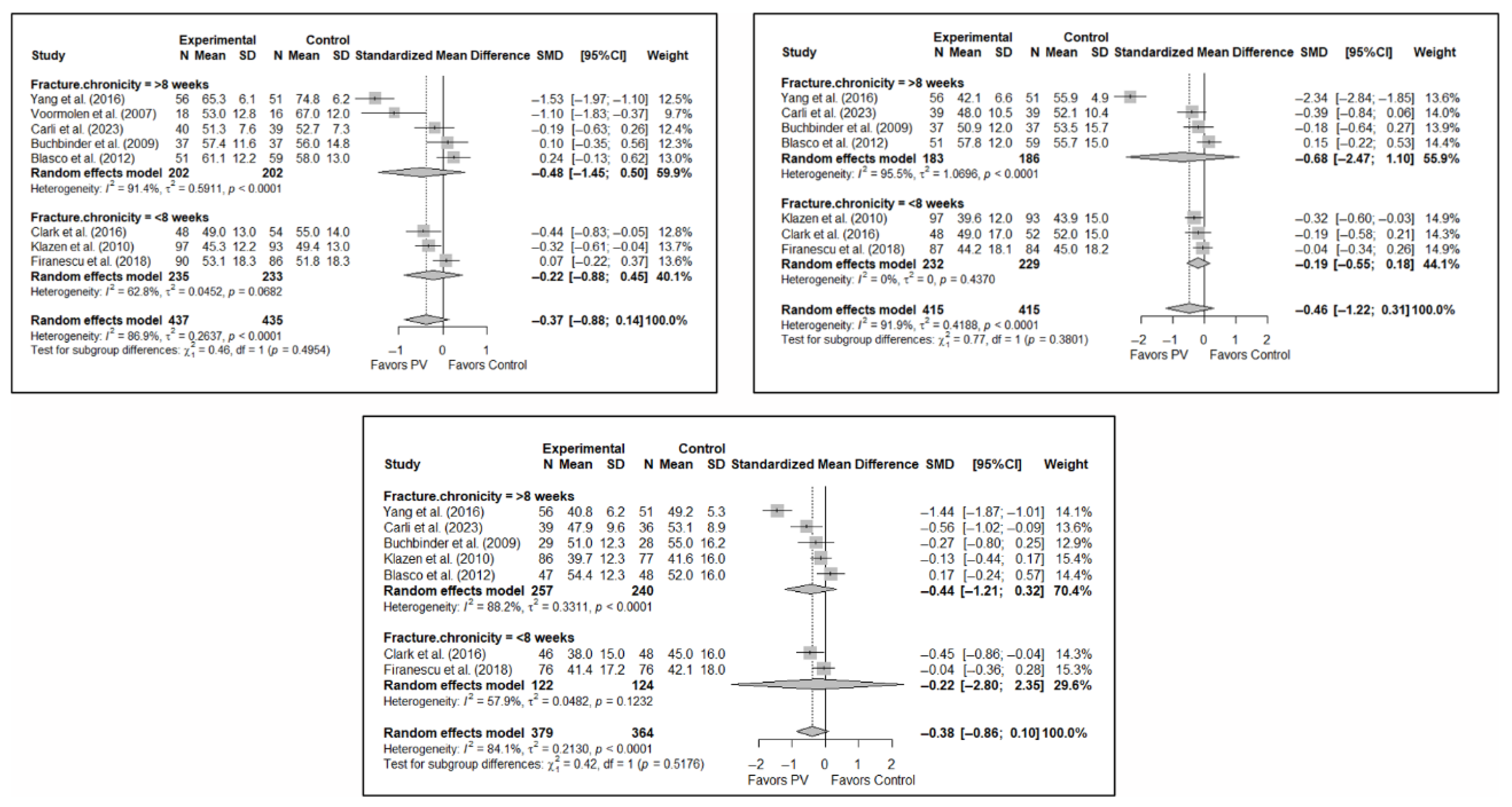
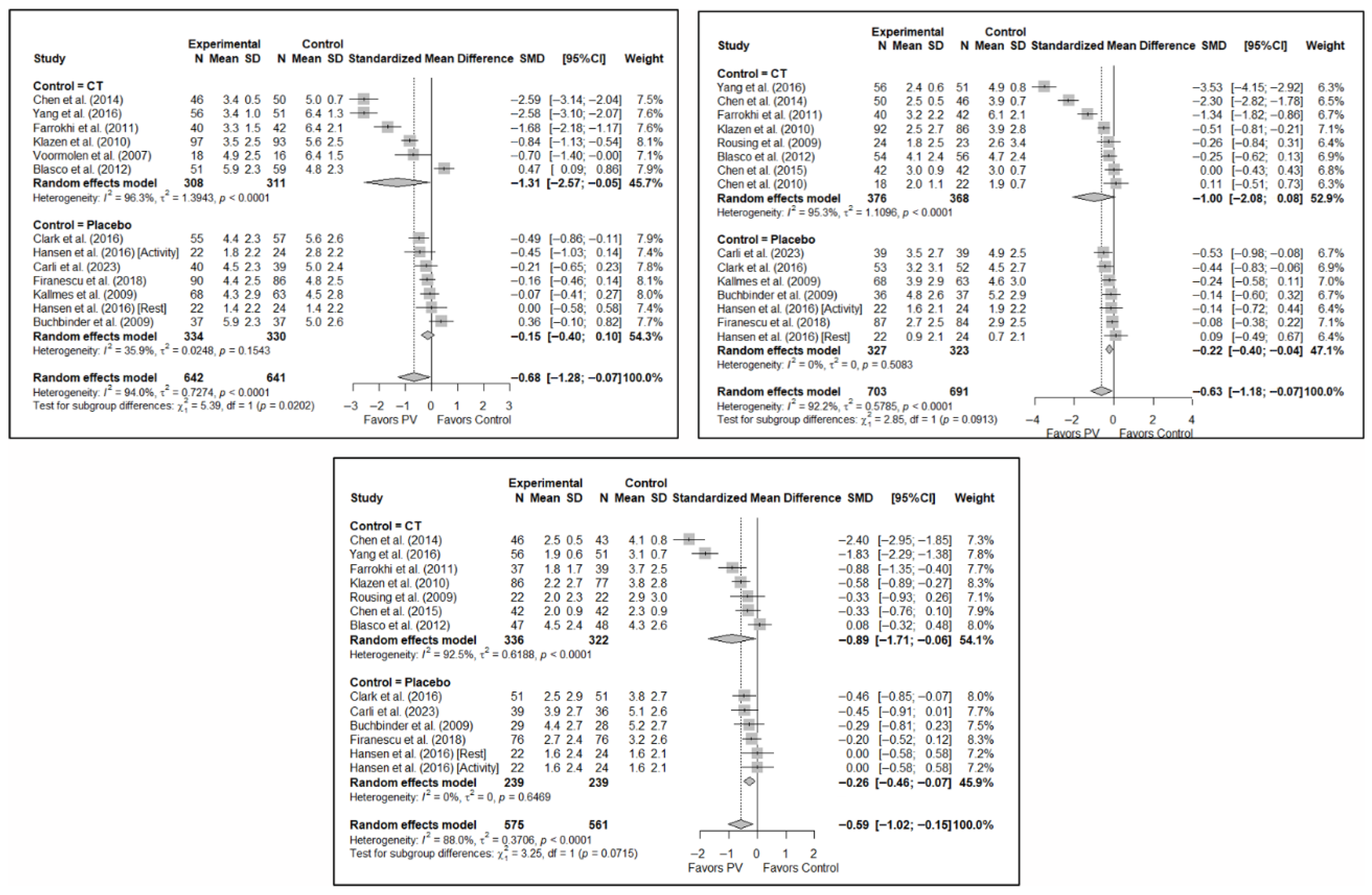
3.6.1. Analysis Based on the Type of Control Group
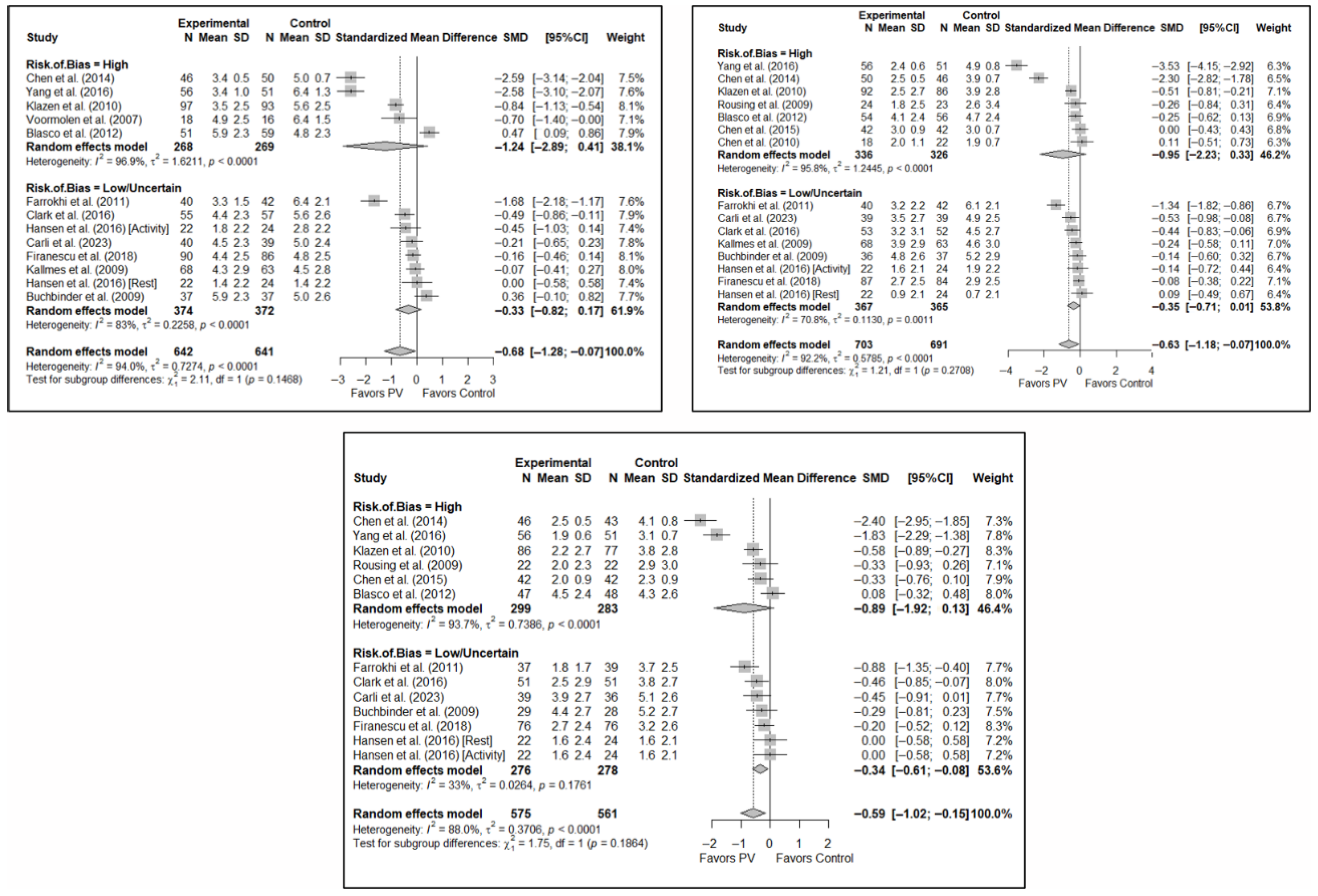
3.6.2. Analysis Based on the Assessment of Risk of Bias in Each Study
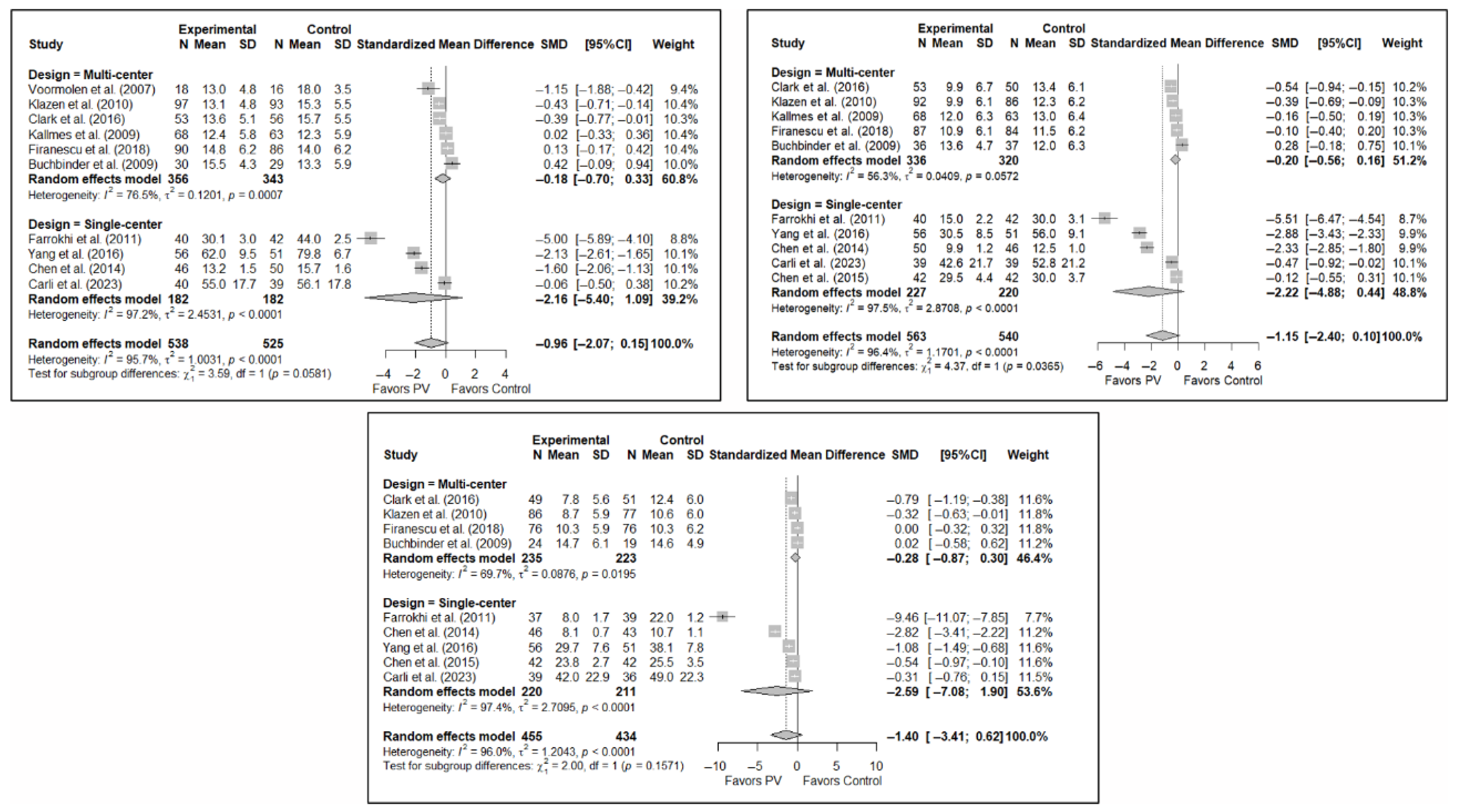
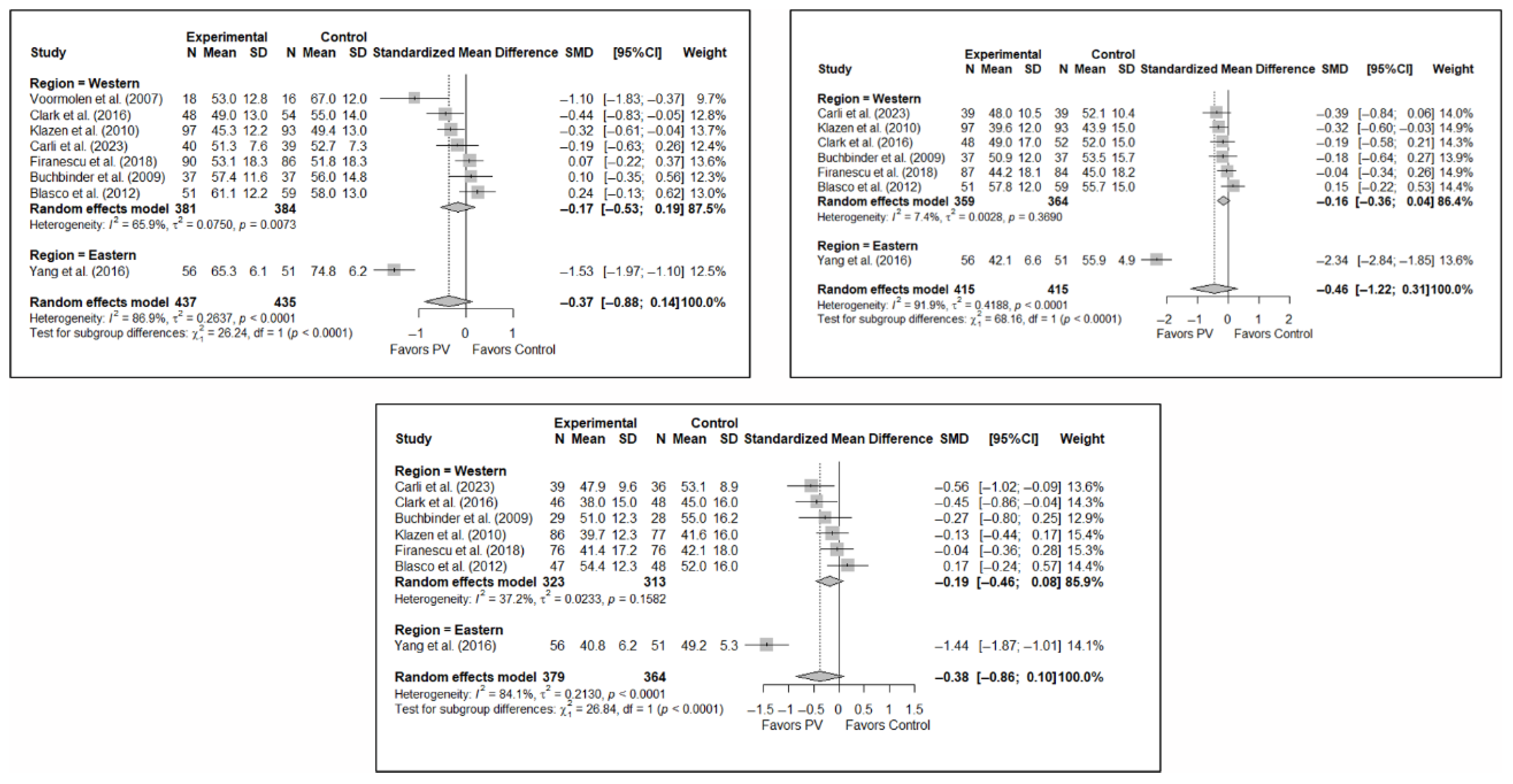
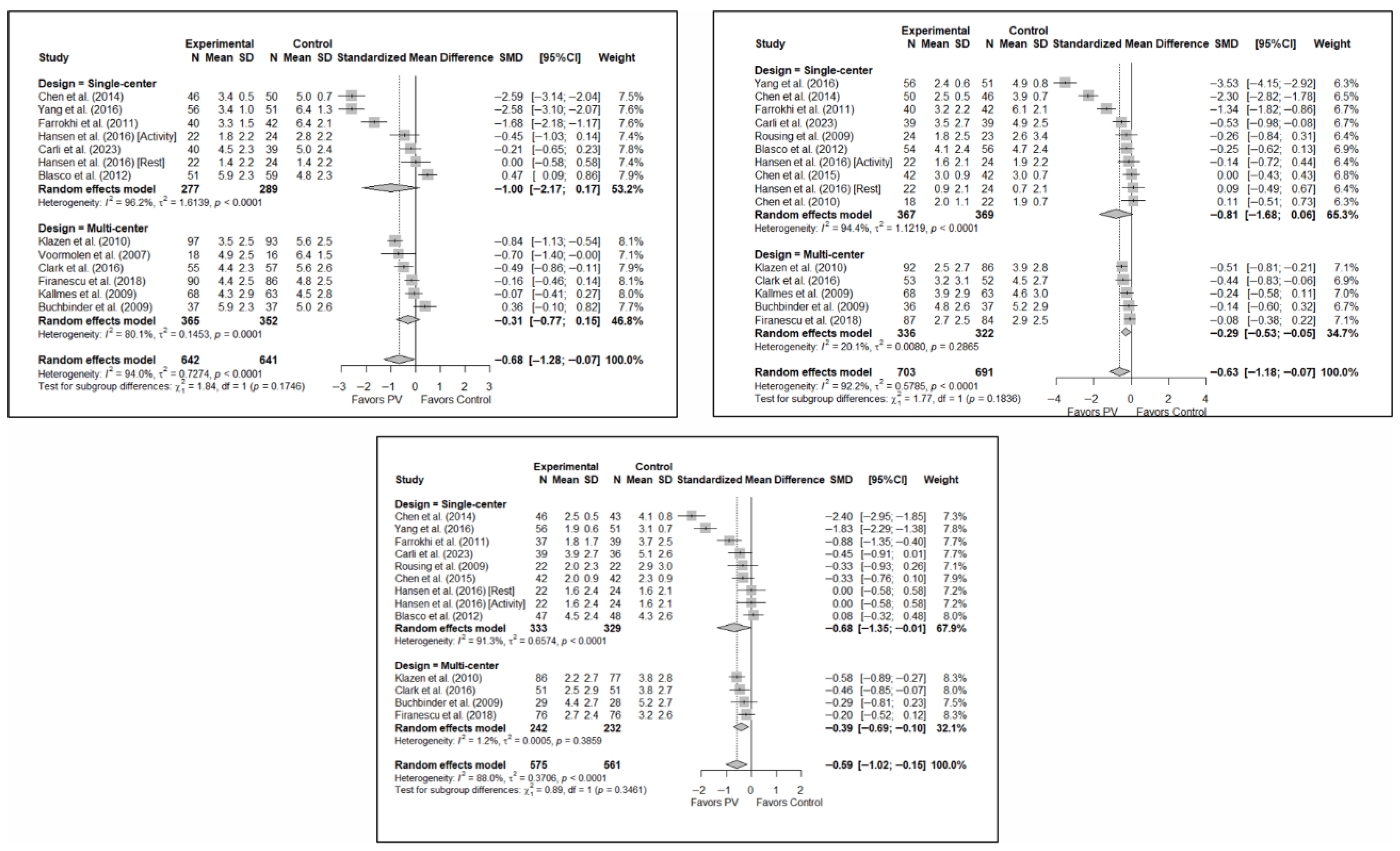
3.6.3. Analysis Based on the Number of Institutions Involved (Single- vs. Multi-Center)
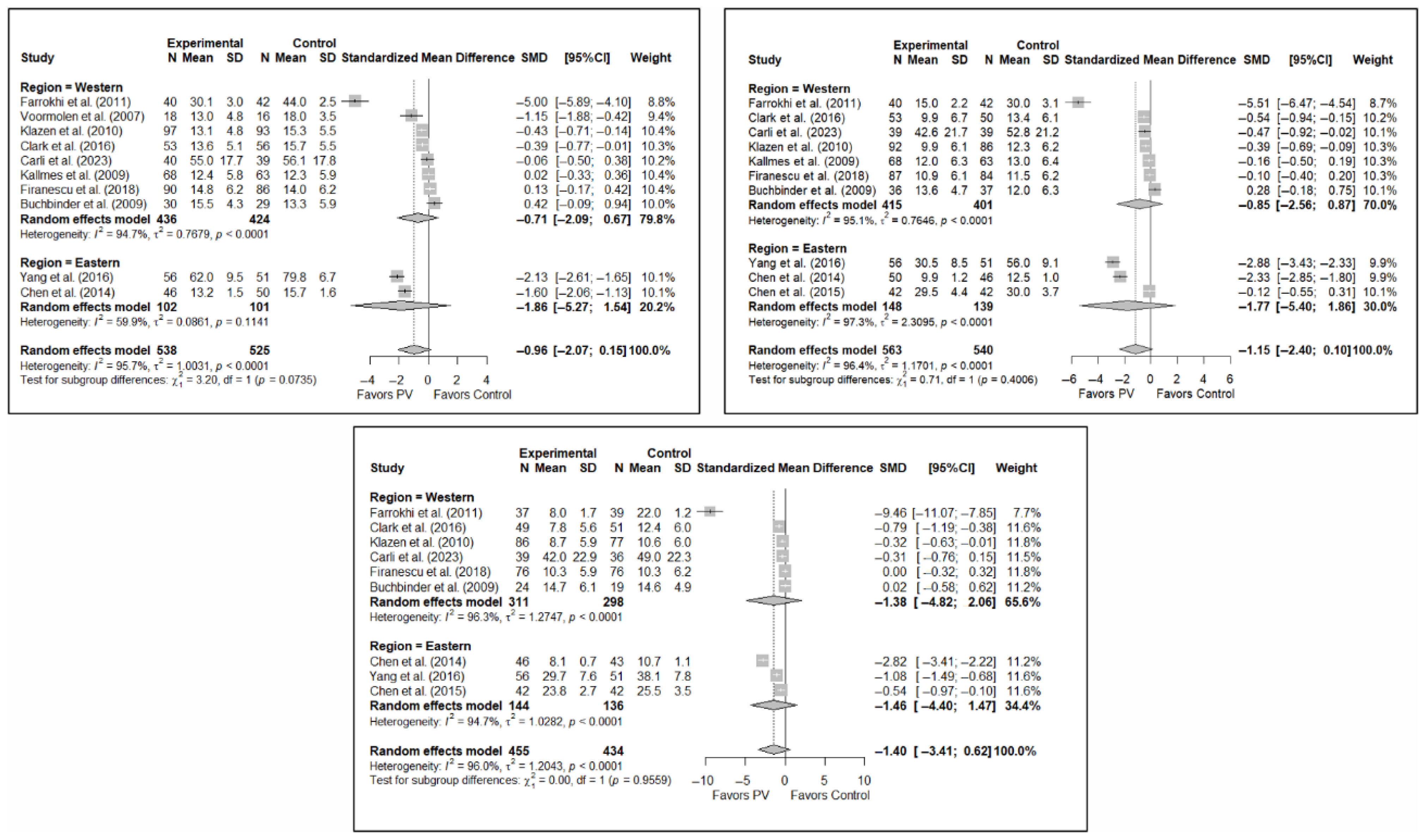
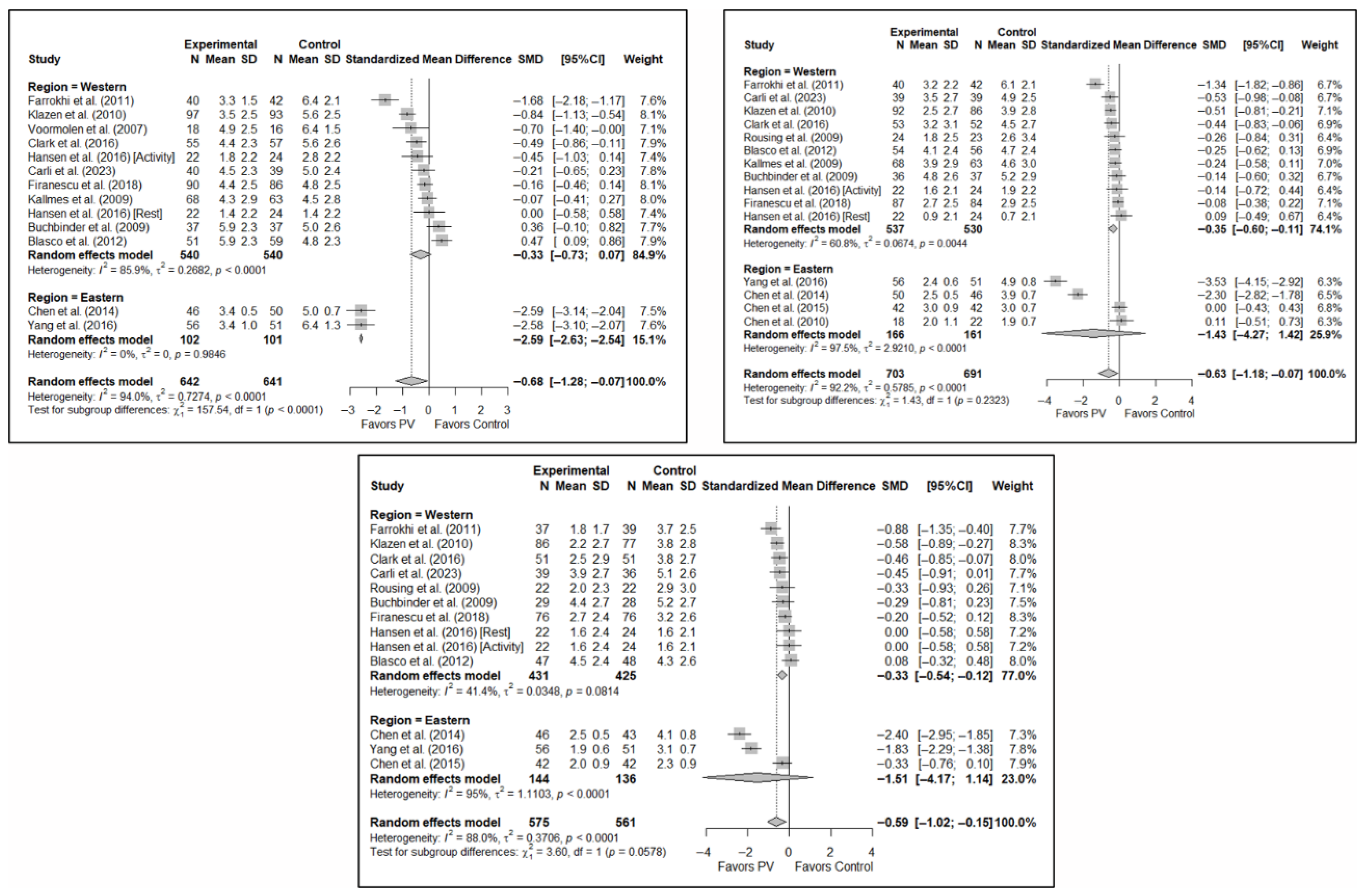
3.6.4. Analysis Based on Geographic Region
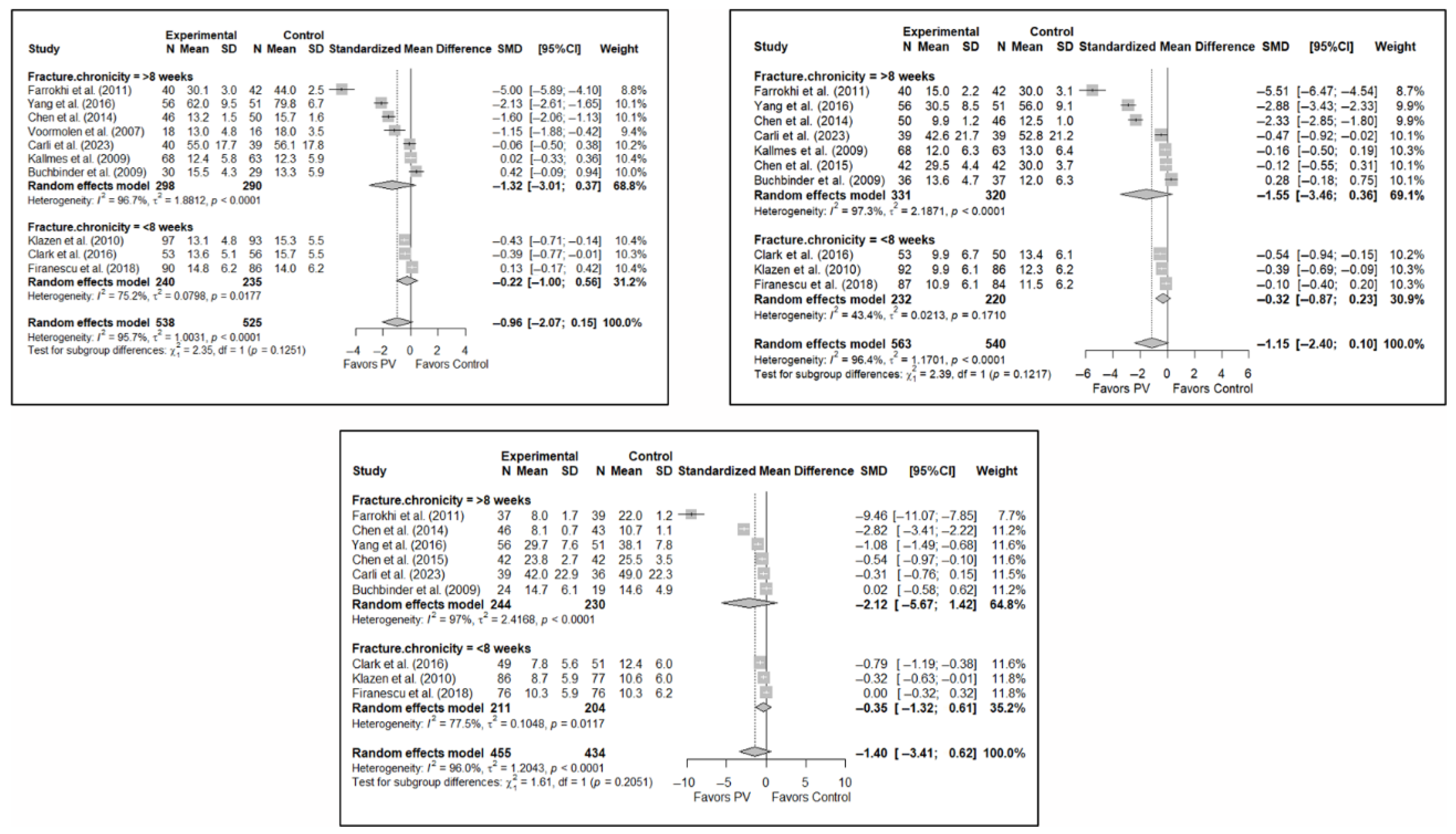
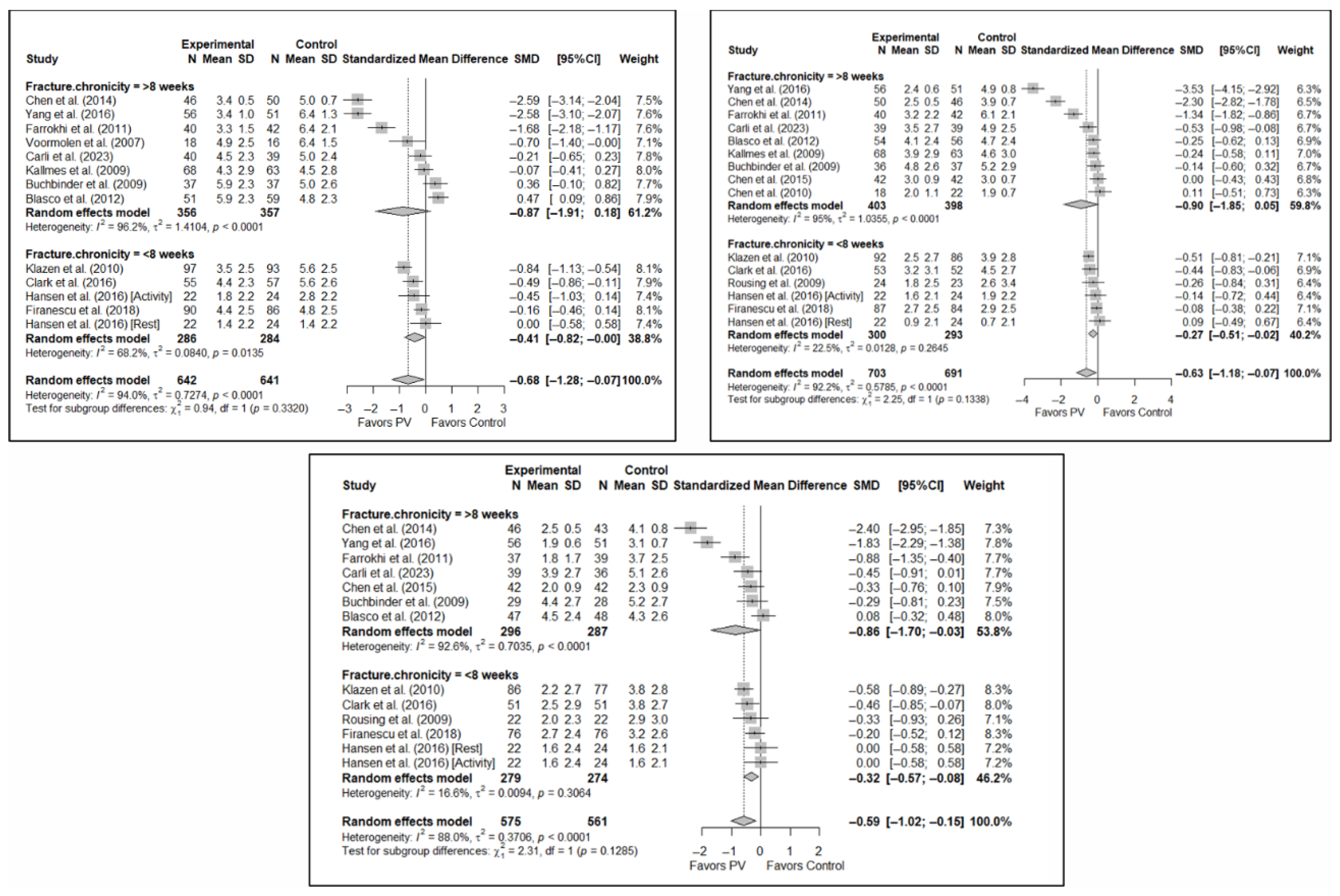
3.6.5. Analysis Based on Fracture Chronicity
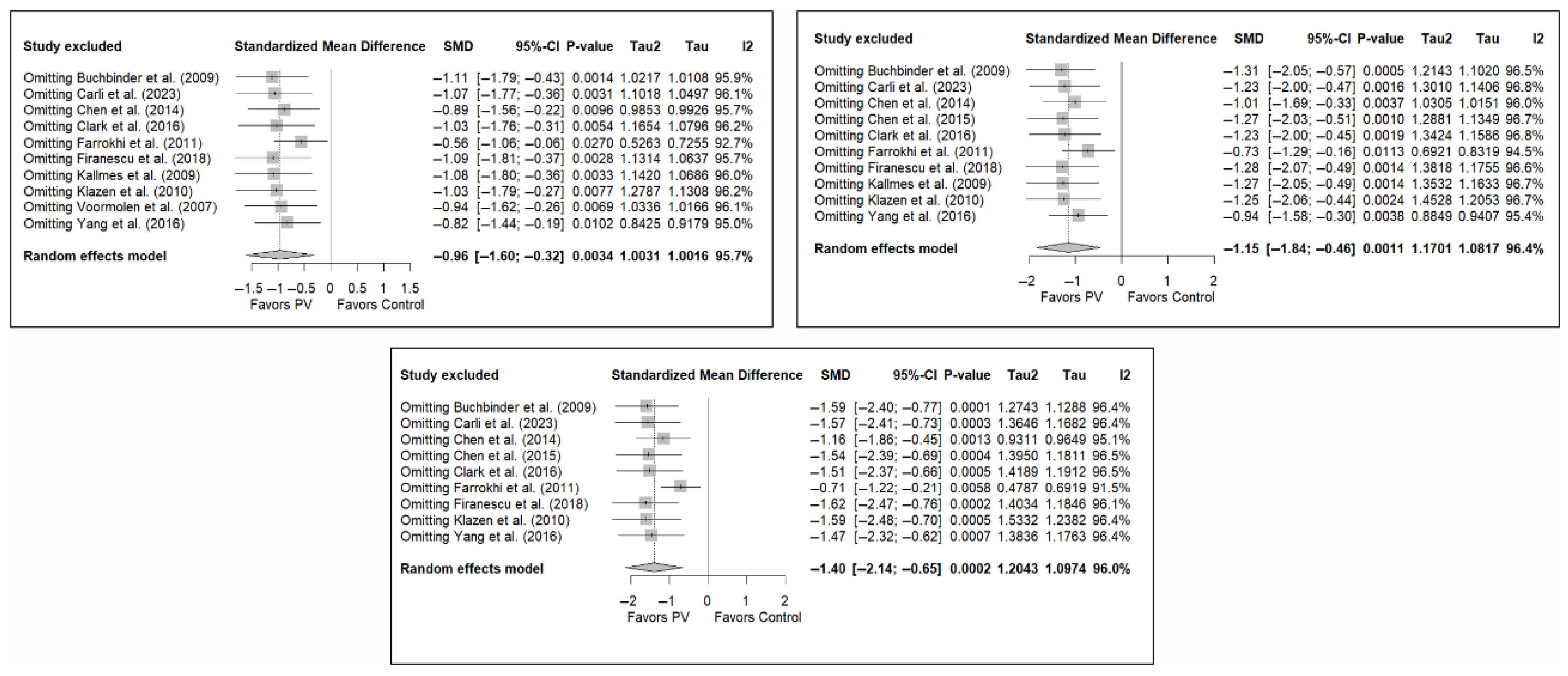
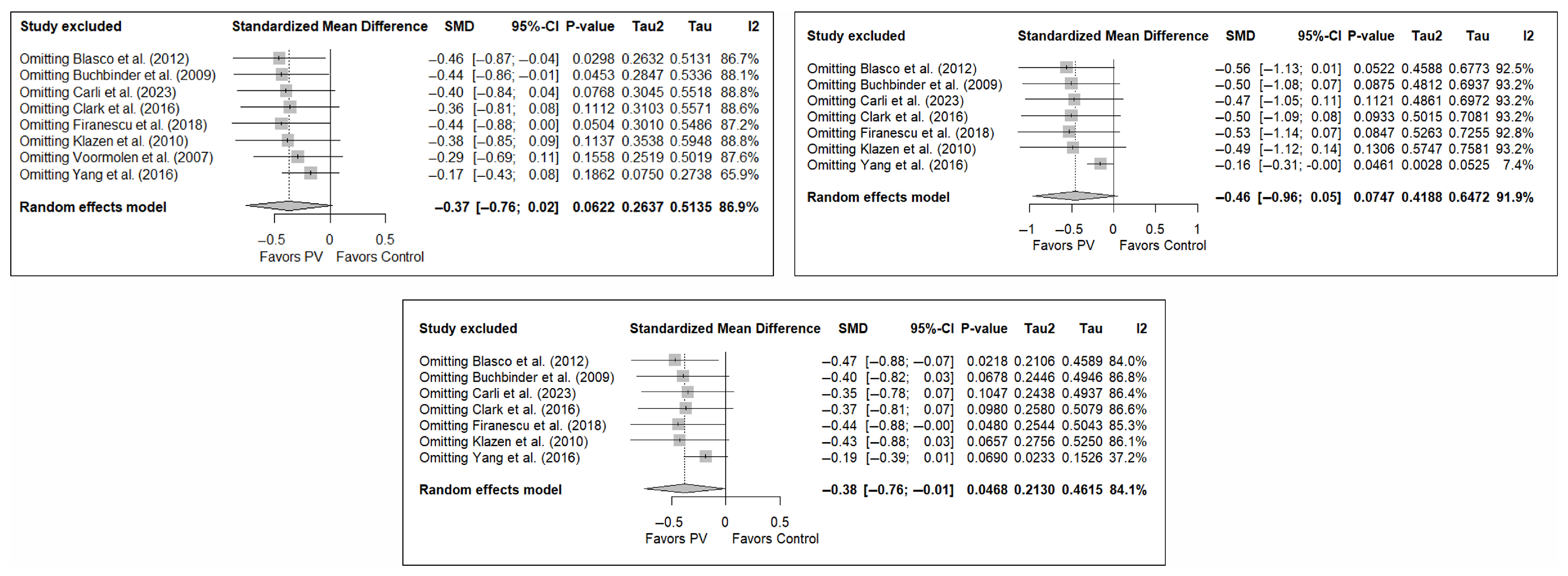
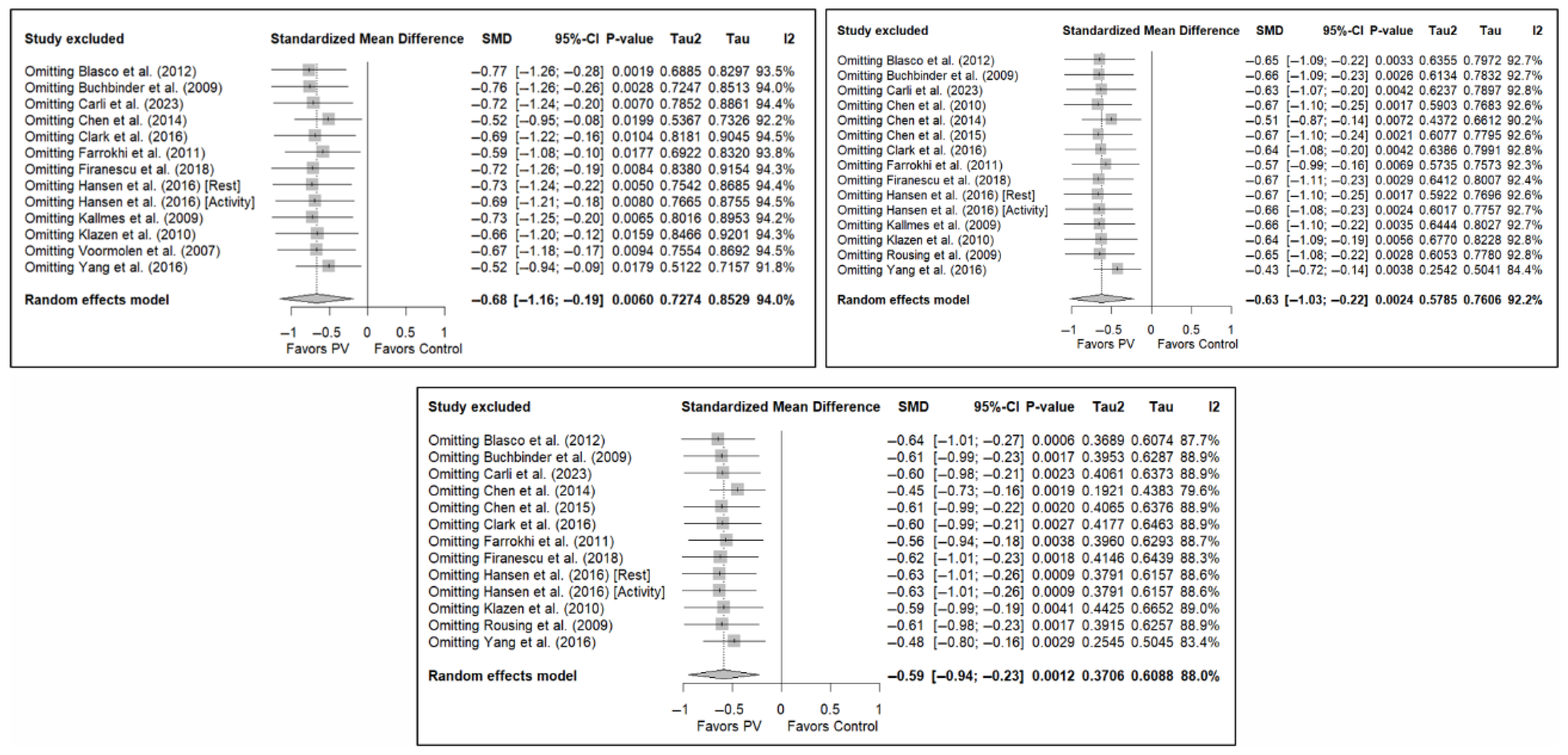
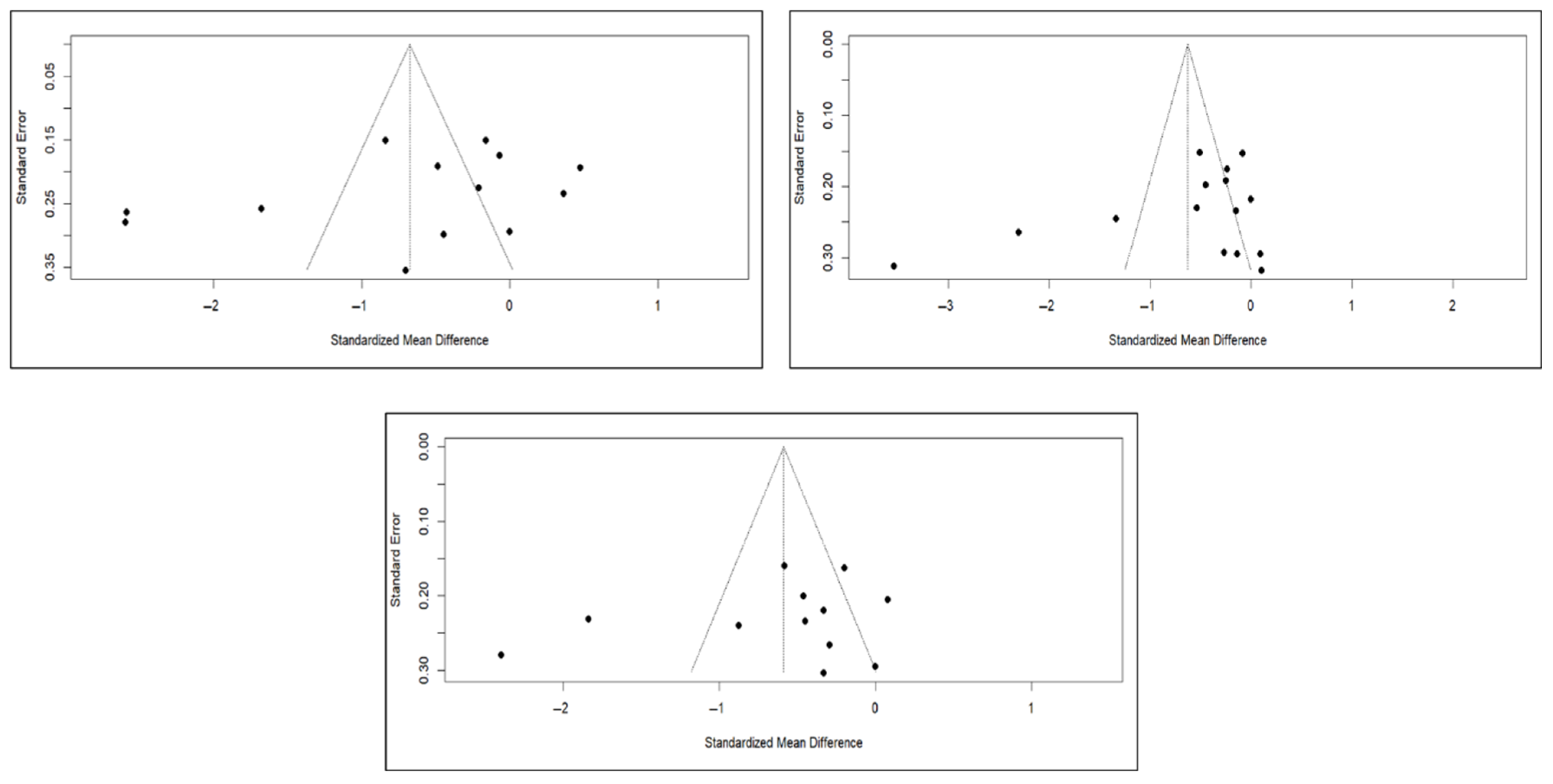
3.7. Sensitivity and Publication Bias Analysis
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A. Search Strategies
Appendix A.1. Search Strategy in the PubMed Database
Appendix A.2. Search Strategy in the EMBASE Database
Appendix A.3. Search Strategy in the Web of Science Database
Appendix A.4. Search Strategy in the CENTRAL Database
Appendix B. Subgroup Analyses
Appendix C. Funnel Plots and Egger’s Test Results
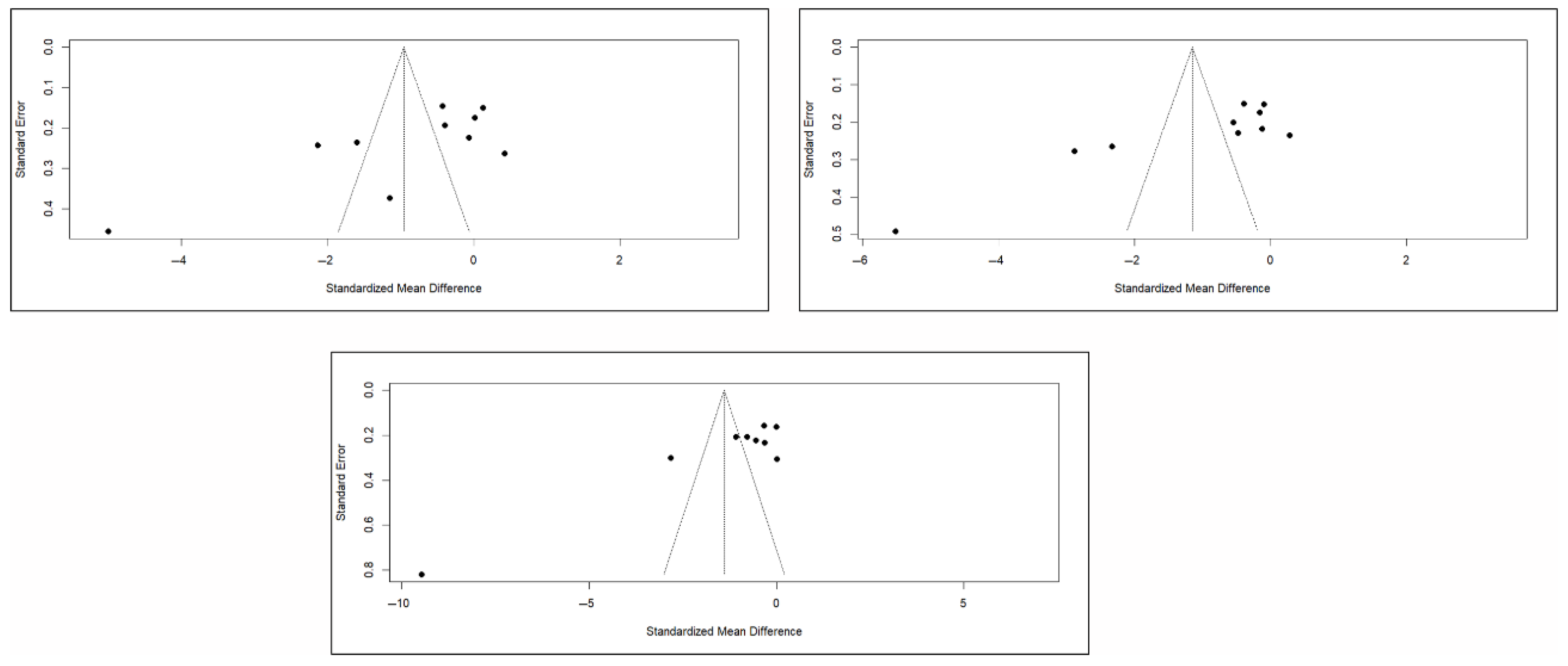
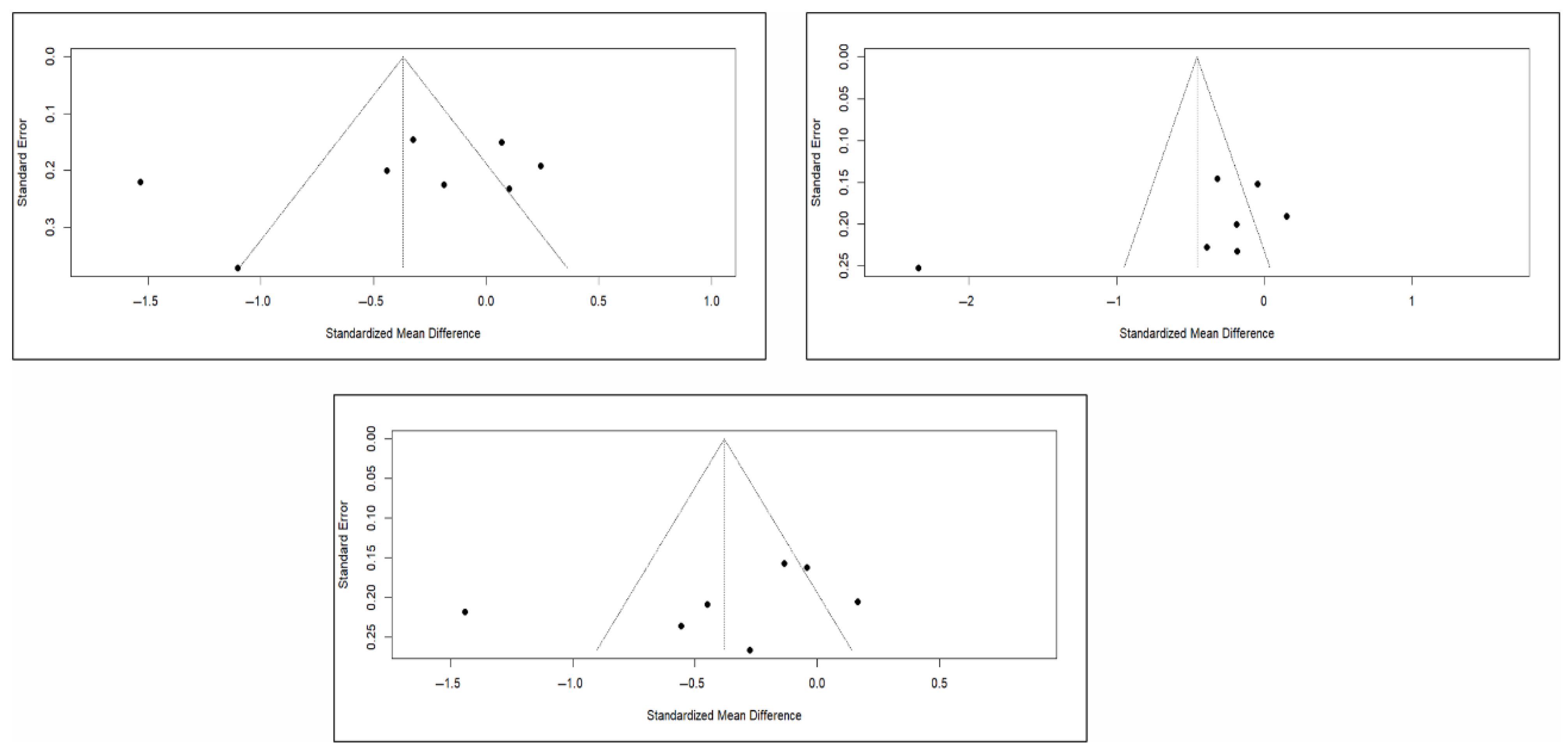
| Pain (short-term) Test result: t = −1.23, df = 11, p-value = 0.2447 Bias estimate: −5.3138 (SE = 4.3239) Pain (medium-term) Test result: t = −1.37, df = 13, p-value = 0.1944 Bias estimate: −5.0604 (SE = 3.6982) Pain (long-term) Test result: t = −0.64, df = 11, p-value = 0.5362 Bias estimate: −2.4923 (SE = 3.9034) Functionality (short-term) Test result: t = −2.50, df = 8, p-value = 0.0367 Bias estimate: −10.0162 (SE = 4.0003) Functionality (medium-term) Test result: t = −3.67, df = 8, p-value = 0.0063 Bias estimate: −14.2904 (SE = 3.8903) Functionality (long-term) Test result: t = −3.65, df = 7, p-value = 0.0082 Bias estimate: −11.6978 (SE = 3.2039) Quality of Life (short-term) Test result: t = −1.08, df = 6, p-value = 0.3224 Bias estimate: −4.2649 (SE = 3.9560) Quality of Life (medium-term) Test result: t = −1.36, df = 5, p-value = 0.2331 Bias estimate: −8.5357 (SE = 6.2939) Quality of Life (long-term) Test result: t = −1.05, df = 5, p-value = 0.3414 Bias estimate: −5.5917 (SE = 5.3204) |
References
- Kanis, J.A.; Norton, N.; Harvey, N.C.; Jacobson, T.; Johansson, H.; Lorentzon, M.; McCloskey, E.V.; Willers, C.; Borgström, F. SCOPE 2021: A New Scorecard for Osteoporosis in Europe. Arch. Osteoporos. 2021, 16, 82. [Google Scholar] [CrossRef]
- Xiao, P.-L.; Cui, A.-Y.; Hsu, C.-J.; Peng, R.; Jiang, N.; Xu, X.-H.; Ma, Y.-G.; Liu, D.; Lu, H.-D. Global, Regional Prevalence, and Risk Factors of Osteoporosis According to the World Health Organization Diagnostic Criteria: A Systematic Review and Meta-Analysis. Osteoporos. Int. 2022, 33, 2137–2153. [Google Scholar] [CrossRef]
- Walker, M.D.; Shane, E. Postmenopausal Osteoporosis. N. Engl. J. Med. 2023, 389, 1979–1991. [Google Scholar] [CrossRef] [PubMed]
- Zeng, Q.; Li, N.; Wang, Q.; Feng, J.; Sun, D.; Zhang, Q.; Huang, J.; Wen, Q.; Hu, R.; Wang, L.; et al. The Prevalence of Osteoporosis in China, a Nationwide, Multicenter DXA Survey. J. Bone Miner. Res. 2019, 34, 1789–1797. [Google Scholar] [CrossRef]
- Rachner, T.D.; Khosla, S.; Hofbauer, L.C. Osteoporosis: Now and the Future. Lancet 2011, 377, 1276–1287. [Google Scholar] [CrossRef]
- Reginster, J.-Y.; Burlet, N. Osteoporosis: A Still Increasing Prevalence. Bone 2006, 38, S4–S9. [Google Scholar] [CrossRef]
- Camacho, P.M.; Petak, S.M.; Binkley, N.; Diab, D.L.; Eldeiry, L.S.; Farooki, A.; Harris, S.T.; Hurley, D.L.; Kelly, J.; Lewiecki, E.M.; et al. American Association of Clinical Endocrinologists/American College of Endocrinology Clinical Practice Guidelines for the Diagnosis and Treatment of Postmenopausal Osteoporosis-2020 Update. Endocr. Pract. 2020, 26, 379–380. [Google Scholar] [CrossRef]
- Ruiz Santiago, F.; Láinez Ramos-Bossini, A.J.; Wáng, Y.X.J.; López Zúñiga, D. The Role of Radiography in the Study of Spinal Disorders. Quant. Imaging Med. Surg. 2020, 10, 2322–2355. [Google Scholar] [CrossRef]
- Ruiz Santiago, F.; Láinez Ramos-Bossini, A.; Wáng, Y.X.J.; Martínez Barbero, J.; García Espinosa, J.; Martínez Martínez, A. The Value of Magnetic Resonance Imaging and Computed Tomography in the Study of Spinal Disorders. Quant. Imaging Med. Surg. 2022, 12, 3947–3986. [Google Scholar] [CrossRef] [PubMed]
- Láinez Ramos-Bossini, A.J.; Ruiz Santiago, F.; Moraleda Cabrera, B.; López Zúñiga, D.; Ariza Sánchez, A. Imaging of Low-Energy Vertebral Fractures. Radiologia 2023, 65, 239–250. [Google Scholar] [CrossRef] [PubMed]
- Chau, L.T.C.; Hu, Z.; Ko, K.S.Y.; Man, G.C.W.; Yeung, K.H.; Law, Y.Y.; Lau, L.C.M.; Wong, R.M.Y.; Chu, W.C.W.; Cheng, J.C.Y.; et al. Global Sagittal Alignment of the Spine, Pelvis, Lower Limb after Vertebral Compression Fracture and Its Effect on Quality of Life. BMC Musculoskelet. Disord. 2021, 22, 476. [Google Scholar] [CrossRef]
- Son, H.J.; Park, S.-J.; Kim, J.-K.; Park, J.-S. Mortality Risk after the First Occurrence of Osteoporotic Vertebral Compression Fractures in the General Population: A Nationwide Cohort Study. PLoS ONE 2023, 18, e0291561. [Google Scholar] [CrossRef]
- Alsoof, D.; Anderson, G.; McDonald, C.L.; Basques, B.; Kuris, E.; Daniels, A.H. Diagnosis and Management of Vertebral Compression Fracture. Am. J. Med. 2022, 135, 815–821. [Google Scholar] [CrossRef]
- Teixeira Taborda, A.; De Miguel Benadiva, C.; Sánchez Tarifa, P. Rehabilitation and Orthopedic Management of Osteoporotic Vertebral Compression Fractures. Rev. Esp. Cir. Ortop. Traumatol. 2024, 68, 624–628. [Google Scholar] [CrossRef] [PubMed]
- Bornemann, R.; Koch, E.M.W.; Wollny, M.; Pflugmacher, R. Treatment Options for Vertebral Fractures an Overview of Different Philosophies and Techniques for Vertebral Augmentation. Eur. J. Orthop. Surg. Traumatol. 2014, 24, S131–S143. [Google Scholar] [CrossRef] [PubMed]
- Galibert, P.; Deramond, H.; Rosat, P.; Le Gars, D. Preliminary note on the treatment of vertebral angioma by percutaneous acrylic vertebroplasty. Neurochirurgie 1987, 33, 166–168. [Google Scholar] [PubMed]
- Beall, D.P.; Phillips, T.R. Vertebral Augmentation: An Overview. Skelet. Radiol. 2023, 52, 1911–1920. [Google Scholar] [CrossRef]
- Mehbod, A.; Aunoble, S.; Le Huec, J.C. Vertebroplasty for Osteoporotic Spine Fracture: Prevention and Treatment. Eur. Spine J. 2003, 12, S155–S162. [Google Scholar] [CrossRef]
- Láinez Ramos-Bossini, A.J.; Jiménez Gutiérrez, P.M.; Ruiz Santiago, F. Efficacy of Radiofrequency in Lumbar Facet Joint Pain: A Systematic Review and Meta-Analysis of Placebo-Controlled Randomized Controlled Trials. Radiol. Med. 2024, 129, 794–806. [Google Scholar] [CrossRef]
- Ruiz Santiago, F.; Pérez Abela, A.L.; Almagro Ratia, M.M. The end of vertebroplasties. Radiologia 2012, 54, 532–538. [Google Scholar] [CrossRef]
- Buchbinder, R.; Osborne, R.H.; Ebeling, P.R.; Wark, J.D.; Mitchell, P.; Wriedt, C.; Graves, S.; Staples, M.P.; Murphy, B. A Randomized Trial of Vertebroplasty for Painful Osteoporotic Vertebral Fractures. N. Engl. J. Med. 2009, 361, 557–568. [Google Scholar] [CrossRef]
- Kallmes, D.F.; Comstock, B.A.; Heagerty, P.J.; Turner, J.A.; Wilson, D.J.; Diamond, T.H.; Edwards, R.; Gray, L.A.; Stout, L.; Owen, S.; et al. A Randomized Trial of Vertebroplasty for Osteoporotic Spinal Fractures. N. Engl. J. Med. 2009, 361, 569–579. [Google Scholar] [CrossRef]
- Carli, D.; Venmans, A.; Lodder, P.; Donga, E.; van Oudheusden, T.; Boukrab, I.; Schoemaker, K.; Smeets, A.; Schonenberg, C.; Hirsch, J.; et al. Vertebroplasty versus Active Control Intervention for Chronic Osteoporotic Vertebral Compression Fractures: The VERTOS V Randomized Controlled Trial. Radiology 2023, 308, e222535. [Google Scholar] [CrossRef] [PubMed]
- Lainez Ramos-Bossini, A.J.; Lopez Zuniga, D.; Ruiz Santiago, F. Percutaneous Vertebroplasty versus Conservative Treatment and Placebo in Osteoporotic Vertebral Fractures: Meta-Analysis and Critical Review of the Literature. Eur. Radiol. 2021, 31, 8542–8553. [Google Scholar] [CrossRef]
- Láinez Ramos-Bossini, A.; Jiménez Gutiérerz, P.; Moraleda Cabrera, B.; Bueno Caravacal, L.; González Díez, M.; Ruiz Santiago, F. Risk of New Vertebral Compression Fractures and Serious Adverse Effects after Vertebroplasty. A Systematic, Critical Review and Meta-Analysis of Randomized Controlled Trials. Quant. Imaging Med. Surg. 2024, 14, 7848–7861. [Google Scholar] [CrossRef]
- Lou, S.; Shi, X.; Zhang, X.; Lyu, H.; Li, Z.; Wang, Y. Percutaneous Vertebroplasty versus Non-Operative Treatment for Osteoporotic Vertebral Compression Fractures: A Meta-Analysis of Randomized Controlled Trials. Osteoporos. Int. 2019, 30, 2369–2380. [Google Scholar] [CrossRef]
- Buchbinder, R.; Johnston, R.V.; Rischin, K.J.; Homik, J.; Jones, C.A.; Golmohammadi, K.; Kallmes, D.F. Percutaneous Vertebroplasty for Osteoporotic Vertebral Compression Fracture. Cochrane Database Syst. Rev. 2018, 11, CD006349. [Google Scholar] [CrossRef] [PubMed]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 Statement: An Updated Guideline for Reporting Systematic Reviews. BMJ 2021, 372, 71. [Google Scholar] [CrossRef] [PubMed]
- DeepL Translator (DeepL SE, Cologne, Germany). DeepL Pro (Web Version). Available online: https://www.deepl.com/es/translator (accessed on 21 August 2025).
- Sterne, J.A.C.; Savović, J.; Page, M.J.; Elbers, R.G.; Blencowe, N.S.; Boutron, I.; Cates, C.J.; Cheng, H.-Y.; Corbett, M.S.; Eldridge, S.M.; et al. RoB 2: A Revised Tool for Assessing Risk of Bias in Randomised Trials. BMJ 2019, 366, l4898. [Google Scholar] [CrossRef]
- Hansen, E.J.; Simony, A.; Rousing, R.; Carreon, L.Y.; Tropp, H.; Andersen, M.Ø. Double Blind Placebo-Controlled Trial of Percutaneous Vertebroplasty (VOPE). Glob. Spine J. 2016, 6, s-0036. [Google Scholar] [CrossRef]
- Firanescu, C.E.; de Vries, J.; Lodder, P.; Venmans, A.; Schoemaker, M.C.; Smeets, A.J.; Donga, E.; Juttmann, J.R.; Klazen, C.A.H.; Elgersma, O.E.H.; et al. Vertebroplasty versus Sham Procedure for Painful Acute Osteoporotic Vertebral Compression Fractures (VERTOS IV): Randomised Sham Controlled Clinical Trial. BMJ 2018, 361, k1551. [Google Scholar] [CrossRef] [PubMed]
- Plot Digitizer. Free Online Tool. Available online: https://plotdigitizer.com/app (accessed on 25 August 2025).
- Yang, E.-Z.; Xu, J.-G.; Huang, G.-Z.; Xiao, W.-Z.; Liu, X.-K.; Zeng, B.-F.; Lian, X.-F. Percutaneous Vertebroplasty Versus Conservative Treatment in Aged Patients with Acute Osteoporotic Vertebral Compression Fractures: A Prospective Randomized Controlled Clinical Study. Spine 2016, 41, 653–660. [Google Scholar] [CrossRef]
- Higgins, J.P.T.; Thomas, J.; Chandler, J.; Cumpston, M.; Li, T.; Page, M.J.; Welch, V.A. (Eds.) Cochrane Handbook for Systematic Reviews of Interventions; Version 6.5; Cochrane: London, UK, 2024; Available online: www.cochrane.org/handbook (accessed on 25 August 2025).
- Voormolen, M.H.J.; Mali, W.P.T.M.; Lohle, P.N.M.; Fransen, H.; Lampmann, L.E.H.; Van Der Graaf, Y.; Juttmann, J.R.; Jansssens, X.; Verhaar, H.J.J. Percutaneous Vertebroplasty Compared with Optimal Pain Medication Treatment: Short-Term Clinical Outcome of Patients with Subacute or Chronic Painful Osteoporotic Vertebral Compression Fractures. The VERTOS Study. Am. J. Neuroradiol. 2007, 28, 555–560. [Google Scholar]
- Hozo, S.P.; Djulbegovic, B.; Hozo, I. Estimating the Mean and Variance from the Median, Range, and the Size of a Sample. BMC Med. Res. Methodol. 2005, 5, 13. [Google Scholar] [CrossRef]
- Klazen, C.A.H.; Lohle, P.N.M.; De Vries, J.; Jansen, F.H.; Tielbeek, A.V.; Blonk, M.C.; Venmans, A.; Van Rooij, W.J.J.; Schoemaker, M.C.; Juttmann, J.R.; et al. Vertebroplasty versus Conservative Treatment in Acute Osteoporotic Vertebral Compression Fractures (Vertos II): An Open-Label Randomised Trial. Lancet 2010, 376, 1085–1092. [Google Scholar] [CrossRef]
- Láinez Ramos-Bossini, A.J.; Gámez Martínez, A.; Luengo Gómez, D.; Valverde-López, F.; Melguizo, C.; Prados, J. Prevalence of Sarcopenia Determined by Computed Tomography in Pancreatic Cancer: A Systematic Review and Meta-Analysis of Observational Studies. Cancers 2024, 16, 3356. [Google Scholar] [CrossRef]
- Láinez Ramos-Bossini, A.J.; Gámez Martínez, A.; Luengo Gómez, D.; Valverde-López, F.; Morillo Gil, A.J.; González Flores, E.; Salmerón Ruiz, Á.; Jiménez Gutiérrez, P.M.; Melguizo, C.; Prados, J. Computed Tomography-Based Sarcopenia and Pancreatic Cancer Survival-A Comprehensive Meta-Analysis Exploring the Influence of Definition Criteria, Prevalence, and Treatment Intention. Cancers 2025, 17, 607. [Google Scholar] [CrossRef]
- Zuo, X.-H.; Zhu, X.-P.; Bao, H.-G.; Xu, C.-J.; Chen, H.; Gao, X.-Z.; Zhang, Q.-X. Network Meta-Analysis of Percutaneous Vertebroplasty, Percutaneous Kyphoplasty, Nerve Block, and Conservative Treatment for Nonsurgery Options of Acute/Subacute and Chronic Osteoporotic Vertebral Compression Fractures (OVCFs) in Short-Term and Long-Term Effects. Medicine 2018, 97, e11544. [Google Scholar] [CrossRef] [PubMed]
- Chen, K.; Gao, T.; Zhu, Y.; Lyu, F.; Jiang, J.; Zheng, C. Augmented Central Pain Processing Occurs after Osteoporotic Vertebral Compression Fractures and Is Associated with Residual Back Pain after Percutaneous Vertebroplasty. Asian Spine J. 2024, 18, 380–389. [Google Scholar] [CrossRef]
- Egger, M.; Davey Smith, G.; Schneider, M.; Minder, C. Bias in Meta-Analysis Detected by a Simple, Graphical Test. BMJ 1997, 315, 629–634. [Google Scholar] [CrossRef] [PubMed]
- R Core Team. R: A Language and Environment for Statistical Computing; R Foundation for Statistical Computing: Vienna, Austria, 2022. [Google Scholar]
- Balduzzi, S.; Rücker, G.; Schwarzer, G. How to Perform a Meta-Analysis with R: A Practical Tutorial. Evid. Based Ment. Health 2019, 22, 153–160. [Google Scholar] [CrossRef]
- Rousing, R.; Andersen, M.O.; Jespersen, S.M.; Thomsen, K.; Lauritsen, J. Percutaneous Vertebroplasty Compared to Conservative Treatment in Patients with Painful Acute or Subacute Osteoporotic Vertebral Fractures: Three-Months Follow-up in a Clinical Randomized Study. Spine 2009, 34, 1349–1354. [Google Scholar] [CrossRef] [PubMed]
- Chen, G.; Zhang, S.; Liu, Y.; Sun, R.; Zhao, X.; Luo, D. Percutaneous Vertebroplasty Compared to Conservative Treatment in Patients with Osteoporotic Vertebral Compression Fractures. J. Cervicodynia Lumbodynia 2010, 31, 323–326. [Google Scholar]
- Farrokhi, M.R.; Alibai, E.; Maghami, Z. Randomized Controlled Trial of Percutaneous Vertebroplasty versus Optimal Medical Management for the Relief of Pain and Disability in Acute Osteoporotic Vertebral Compression Fractures. J. Neurosurg. Spine 2011, 14, 561–569. [Google Scholar] [CrossRef]
- Blasco, J.; Martinez-Ferrer, A.; MacHo, J.; San Roman, L.; Pomés, J.; Carrasco, J.; Monegal, A.; Guañabens, N.; Peris, P. Effect of Vertebroplasty on Pain Relief, Quality of Life, and the Incidence of New Vertebral Fractures: A 12-Month Randomized Follow-up, Controlled Trial. J. Bone Miner. Res. 2012, 27, 1159–1166. [Google Scholar] [CrossRef]
- Chen, D.; An, Z.-Q.; Song, S.; Tang, J.-F.; Qin, H. Percutaneous Vertebroplasty Compared with Conservative Treatment in Patients with Chronic Painful Osteoporotic Spinal Fractures. J. Clin. Neurosci. 2014, 21, 473–477. [Google Scholar] [CrossRef] [PubMed]
- Chen, J.-P.; Qi, X.-W.; Li, S.-J.; Kuang, L.-P.; Yuan, X.-H.; Wang, G.-S.; Tan, W.-Y. Bone cement injection as vertebral augmentation therapy for osteoporotic vertebral compression fractures. Chin. J. Tissue Eng. Res. 2015, 19, 3292–3296. [Google Scholar] [CrossRef]
- Clark, W.; Bird, P.; Gonski, P.; Diamond, T.H.; Smerdely, P.; McNeil, H.P.; Schlaphoff, G.; Bryant, C.; Barnes, E.; Gebski, V. Safety and Efficacy of Vertebroplasty for Acute Painful Osteoporotic Fractures (VAPOUR): A Multicentre, Randomised, Double-Blind, Placebo-Controlled Trial. Lancet 2016, 388, 1408–1416. [Google Scholar] [CrossRef]
- Zhu, R.-S.; Kan, S.-L.; Ning, G.-Z.; Chen, L.-X.; Cao, Z.-G.; Jiang, Z.-H.; Zhang, X.-L.; Hu, W. Which Is the Best Treatment of Osteoporotic Vertebral Compression Fractures: Balloon Kyphoplasty, Percutaneous Vertebroplasty, or Non-Surgical Treatment? A Bayesian Network Meta-Analysis. Osteoporos. Int. 2019, 30, 287–298. [Google Scholar] [CrossRef]
- Sanli, I.; van Kuijk, S.M.J.; de Bie, R.A.; van Rhijn, L.W.; Willems, P.C. Percutaneous Cement Augmentation in the Treatment of Osteoporotic Vertebral Fractures (OVFs) in the Elderly: A Systematic Review. Eur. Spine J. 2020, 29, 1553–1572. [Google Scholar] [CrossRef]
- Andreão, F.F.; Borges, P.; Palavani, L.B.; Machinski, E.; Oliveira, L.B.; Ferreira, M.Y.; Batista, S.; Semione, G.; Neto, A.R.; Bertani, R.; et al. Percutaneous Vertebroplasty versus Nonoperative Treatment of Osteoporotic Vertebral Fractures: A Meta-Analysis of Randomized Controlled Trials. World Neurosurg. 2024, 190, 408–421.e5. [Google Scholar] [CrossRef]
- Jones, J.C.; Miller, J.A.; Sudarshana, D.M.; Thompson, N.R.; Benzel, E.C.; Mroz, T.E. Predictors of Favorable Quality of Life Outcome Following Kyphoplasty and Vertebroplasty. J. Neurosurg. Spine 2019, 31, 389–396. [Google Scholar] [CrossRef]
- Ebeling, P.R.; Akesson, K.; Bauer, D.C.; Buchbinder, R.; Eastell, R.; Fink, H.A.; Giangregorio, L.; Guanabens, N.; Kado, D.; Kallmes, D.; et al. The Efficacy and Safety of Vertebral Augmentation: A Second ASBMR Task Force Report. J. Bone Miner. Res. 2019, 34, 3–21. [Google Scholar] [CrossRef]
- Ruiz Santiago, F.; Bueno Caravaca, L.; Garrido Sanz, F.; Jiménez Gutiérrez, P.M.; Luengo Gómez, D.; Rivera Izquierdo, M.; Benítez, J.M.; Láinez Ramos-Bossini, A.J. Factors Influencing the Development of Metachronous Fractures in Patients with Osteoporotic Vertebral Fractures Treated with Conservative Management or Vertebroplasty. Diagnostics 2025, 15, 160. [Google Scholar] [CrossRef] [PubMed]
- Pron, G.; Hwang, M.; Nasralla, M.; Smith, R.; Cheung, A.; Murphy, K. Cost-Effectiveness and Willing-to-Pay Thresholds for Vertebral Augmentation of Osteoporotic Vertebral Fractures, What Are They Based on: A Systematic Review. BMJ Open 2023, 13, e062832. [Google Scholar] [CrossRef] [PubMed]
- Pron, G.; Hwang, M.; Smith, R.; Cheung, A.; Murphy, K. Cost-Effectiveness Studies of Vertebral Augmentation for Osteoporotic Vertebral Fractures: A Systematic Review. Spine J. 2022, 22, 1356–1371. [Google Scholar] [CrossRef]
- Tsoumakidou, G.; Too, C.W.; Koch, G.; Caudrelier, J.; Cazzato, R.L.; Garnon, J.; Gangi, A. CIRSE Guidelines on Percutaneous Vertebral Augmentation. Cardiovasc. Interv. Radiol. 2017, 40, 331–342. [Google Scholar] [CrossRef] [PubMed]
| Study | Group | N | Age | M/F Ratio | Symptoms Duration a | F-U b | Initial VAS | Initial RMDQ | Initial ODI | Initial QUALEFFO |
|---|---|---|---|---|---|---|---|---|---|---|
| Voormolen et al. (2007) [36] | PV | 18 | 72 (59–84) | 4/14 | 85 (47–138) | 2 W | 7.1 (5–9) | 15.7 (8–22) | - | 60 (37–86) |
| CT | 16 | 74 (55–88) | 2/14 | 76 (46–141) | 2 W | 7.6 (5–10) | 17.8 (9–24) | - | 67 (38–86) | |
| Rousing et al. (2009) [46] | PV | 25 | 80 (65–96) | 6/19 | 8.4 (3.7–13) | 12 | 7.5 (6.6–8.4) | - | - | - |
| CT | 24 | 80 (71–93) | 3/21 | 6.7 (2.1–11.4) | 12 | 8.8 (8.2–9.3) | - | - | - | |
| Kallmes et al. (2009) [22] | PV | 68 | 73.4 (9.4) | 15/53 | 16 (10.36) c W | 1 | 6.9 (2.0) | 16.6 (3.8) | - | - |
| Placebo | 63 | 74.3 (9.6) | 17/46 | 20 (8–38) c W | 1 | 7.2 (1.8) | 17.5 (4.1) | - | - | |
| Buchbinder et al. (2009) [21] | PV | 38 | 74.2 (14) | 7/31 | 9 (3.8–13) c W | 24 | 7.4 (2.1) | 17.3 (2.8) | - | 56.9 (13.4) |
| Placebo | 40 | 78.9 (9.5) | 9/31 | 9.5 (3–17) c W | 24 | 7.1 (2.3) | 17.3 (2.9) | - | 59.6 (17.1) | |
| Chen et al. (2010) [47] | PV | 18 | 77.5 (0.8) | 4/14 | <6 W | 3 | 7.8 (1.2) | - | - | - |
| CT | 22 | 76.3 (0.5) | 6/16 | <6 W | 3 | 8.1 (0.8) | - | - | - | |
| Klazen et al. (2010) [38] | PV | 101 | 75.2 (9.8) | 31/70 | 29.3 (17.1) | 12 | 7.8 (1.5) | 18.6 (3.6) | - | 58.7 (13.5) |
| CT | 101 | 75.4 (8.4) | 31/70 | 26.8 (16.0) | 12 | 7.5 (1.6) | 17.2 (4.2) | - | 54.7 (14.4) | |
| Farrokhi et al. (2011) [48] | PV | 40 | 72 (59–90) | 10/30 | 27 (4–50) c W | 36 | 8.4 (1.6) | - | 51.2 (2.2) | - |
| CT | 42 | 74 (55–87) | 12/30 | 30 (6–54) c W | 36 | 7.2 (1.7) | - | 47.1 (2.8) | - | |
| Blasco et al. (2012) [49] | PV | 64 | 71.3 (10) | 17/47 | 140.3 (96.1) | 12 | 7.21 (0.3) | - | - | 65.2 (2.2) |
| CT | 61 | 75.3 (8.5) | 11/50 | 143.1 (130.3) | 12 | 6.3 (0.4) | - | - | 59.2 (2.2) | |
| Chen et al. (2014) [50] | PV | 46 | 64.6 (9.1) | 14/32 | 7.1 (3) | 12 | 6.5 (0.9) | 18.6 (1.8) | 59.9 (2.2) | - |
| CT | 47 | 66.5 (9.1) | 13/30 | 6.8 (2.5) | 12 | 6.4 (0.9) | 16.7 (1.3) | 57.9 (1.9) | - | |
| Chen et al. (2015) [51] | PV | 42 | 67 (8.4) | 18/24 | - | 34.7 | 7.3 (1.0) | 48.8 (6.8) | - | |
| CT | 42 | 66.1 (8.7) | 19/23 | - | 34.7 | 7.5 (0.8) | 48.9 (7.3) | - | ||
| Hansen et al. (2016) [31] | PV | 22 | 70.6 (54–90) | 4/18 | 74.7 (4.6) | 12 | 5.3 (0.4) | - | - | - |
| Placebo | 24 | 69.3 (53–84) | 2/22 | 76.1 (4.4) | 12 | 4.6 (0.46) | - | - | - | |
| Yang et al. (2016) [34] | PV | 56 | 77.1 (6.0) | 20/36 | 5.5 (3.9) | 12 | 7.5 (1.1) | - | 80.2 (9.9) | 78.1 (8.1) |
| CT | 51 | 76.2 (5.6) | 18/33 | 5.6 (3.8) | 12 | 7.7 (1.1) | - | 81.5 (9.7) | 77.5 (8.6) | |
| Clark et al. (2016) [52] | PV | 61 | 80 (7) | 13/48 | 2.8 (1.6) W | 6 | 8.1 (1.8) | 19.5 (3.5) | - | 65.4 (11.4) |
| Placebo | 59 | 81 (7) | 19/40 | 2.4 (1.4) W | 6 | 8.2 (1.5) | 19.8 (3.7) | - | 67.7 (11.2) | |
| Firanescu et al. (2018) [32] | PV | 90 | 74.7 (10.7) | 23/67 | 43 (29–52) | 12 | 7.7 (1.4) | 18.0 (4.5) | - | 68.4 (17.1) |
| Placebo | 86 | 76.9 (8.1) | 20/66 | 36 (24–51) | 12 | 7.9 (1.6) | 17.8 (4.7) | - | 69.7 (17.9) | |
| Carli et al. (2023) [23] | PV | 40 | 69 (10) | 13/27 | 176 (43–907) | 12 | 7.6 (1.8) | 64.7 (20) | - | 61.8 (9.3) |
| Placebo | 40 | 71 (10) | 13/27 | 185 (68–1165) | 12 | 7.3 (1.5) | 63.4 (17.9) | - | 60.9 (8.8) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Láinez Ramos-Bossini, A.J.; Garrido Sanz, F.; Gea Becerra, M.; Melguizo Alonso, C.; Prados, J.; Ruiz Santiago, F.; Benítez, J.M. Efficacy of Percutaneous Vertebroplasty Versus Placebo and Conservative Treatment in Osteoporotic Vertebral Fractures: An Updated Systematic Review and Meta-Analysis of Randomized Clinical Trials. Diagnostics 2025, 15, 2684. https://doi.org/10.3390/diagnostics15212684
Láinez Ramos-Bossini AJ, Garrido Sanz F, Gea Becerra M, Melguizo Alonso C, Prados J, Ruiz Santiago F, Benítez JM. Efficacy of Percutaneous Vertebroplasty Versus Placebo and Conservative Treatment in Osteoporotic Vertebral Fractures: An Updated Systematic Review and Meta-Analysis of Randomized Clinical Trials. Diagnostics. 2025; 15(21):2684. https://doi.org/10.3390/diagnostics15212684
Chicago/Turabian StyleLáinez Ramos-Bossini, Antonio Jesús, Francisco Garrido Sanz, Marina Gea Becerra, Consolación Melguizo Alonso, José Prados, Fernando Ruiz Santiago, and José Manuel Benítez. 2025. "Efficacy of Percutaneous Vertebroplasty Versus Placebo and Conservative Treatment in Osteoporotic Vertebral Fractures: An Updated Systematic Review and Meta-Analysis of Randomized Clinical Trials" Diagnostics 15, no. 21: 2684. https://doi.org/10.3390/diagnostics15212684
APA StyleLáinez Ramos-Bossini, A. J., Garrido Sanz, F., Gea Becerra, M., Melguizo Alonso, C., Prados, J., Ruiz Santiago, F., & Benítez, J. M. (2025). Efficacy of Percutaneous Vertebroplasty Versus Placebo and Conservative Treatment in Osteoporotic Vertebral Fractures: An Updated Systematic Review and Meta-Analysis of Randomized Clinical Trials. Diagnostics, 15(21), 2684. https://doi.org/10.3390/diagnostics15212684








