Prevalence, Morphometric Characteristics of the Accessory Abductor Pollicis Longus Muscle and Clinical Implications: A Cadaveric Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Cadaveric Dissection
2.2. Morphometric Analysis
2.3. Statistical Analysis
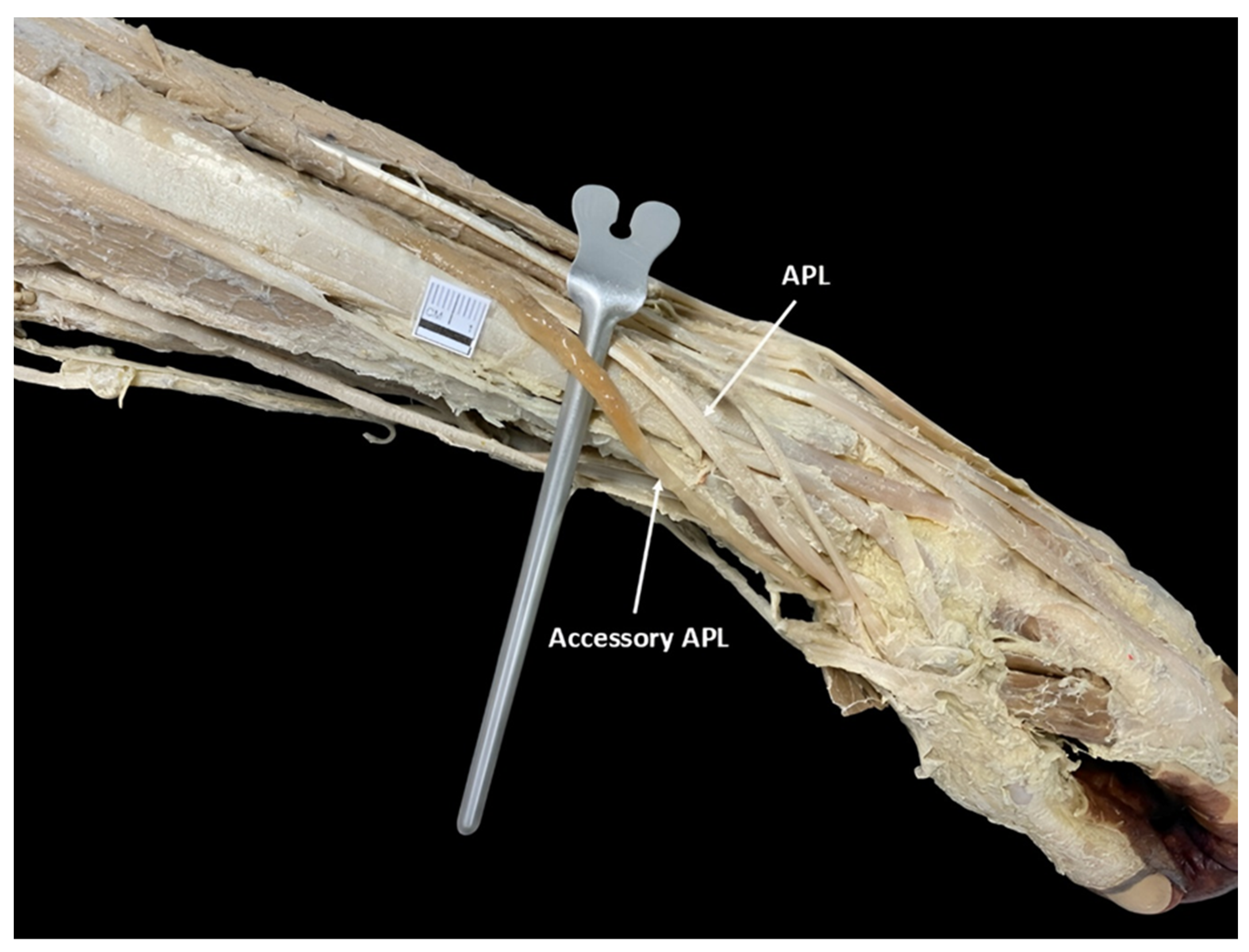
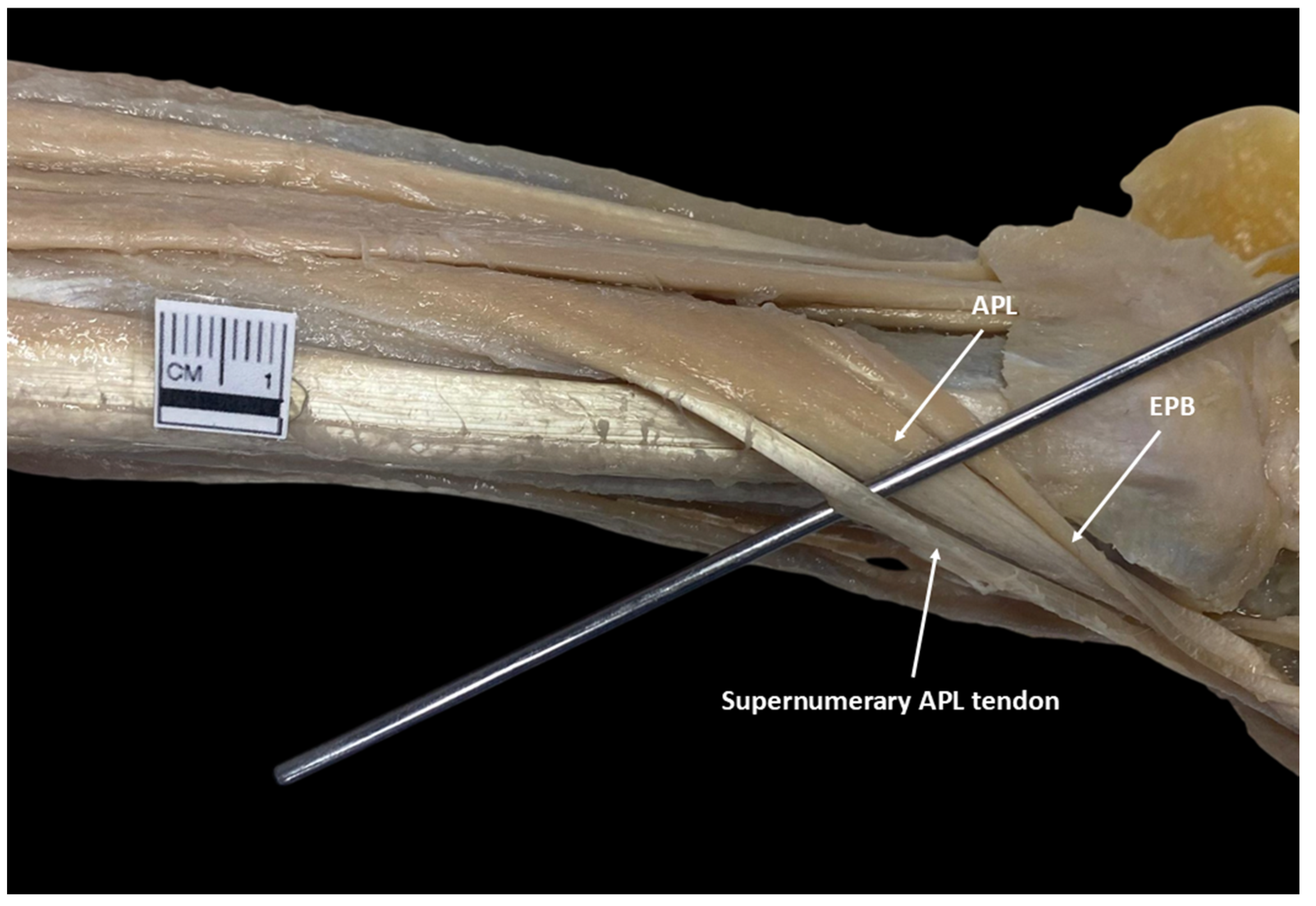
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| APL | Abductor pollicis longus |
| AAPL | Accessory abductor pollicis longus |
| DTL | Distal tendon length |
| ML | Muscle length |
| TML | Transverse muscle length |
| EBP | Extensor pollicis brevis |
References
- Standring, S. (Ed.) Gray’s Anatomy: The Anatomical Basis of Clinical Practice, 41st ed.; Elsevier: New York, NY, USA, 2015. [Google Scholar]
- Chang, E.Y.; Chung, K.C. Outcomes of trapeziectomy with a modified abductor pollicis longus suspension arthroplasty for the treatment of thumb carpometacarpal joint osteoarthritis. Plast. Reconstr. Surg. 2008, 122, 505–515. [Google Scholar] [CrossRef] [PubMed]
- Lee, H.J.; Kim, P.T.; Deslivia, M.F.; Jeon, I.H.; Lee, S.J.; Nam, S.J. Results of abductor pollicis longus suspension ligamentoplasty for treatment of advanced first carpometacarpal arthritis. Clin. Orthop. Surg. 2015, 7, 372–376. [Google Scholar] [CrossRef]
- Satria, O.; Wibowo, R.S.; Putra, G.U.; Fathurrahman, I. Suture suspension sling arthroplasty in thumb carpometacarpal joint arthritis: A case series. Int. J. Surg. Case Rep. 2023, 110, 108583. [Google Scholar] [CrossRef]
- Rab, M.; Gohritz, A.; Gohla, T.; Krimmer, H.; Lanz, U. Ergebnisse nach Resektions-Suspensions-Arthroplastik bei Rhizarthrose: Vergleich der Abductor pollicis longus-mit der Flexor carpi radialis-Sehnensuspension [Long-term results after resection arthroplasty in patients with arthrosis of the thumb carpometacarpal joint: Comparison of abductor pollicis longus and flexor carpi radialis tendon suspension]. Handchir. Mikrochir. Plast. Chir. 2006, 38, 98–103. [Google Scholar] [CrossRef] [PubMed]
- Bravo, E.; Barco, R.; Bullón, A. Anatomic study of the abductor pollicis longus: A source for grafting material of the hand. Clin. Orthop. Relat. Res. 2010, 468, 1305–1309. [Google Scholar] [CrossRef][Green Version]
- Hatipoğlu, M.Y.; Yapar, A.; Ergişi, Y.; Tokgöz, M.A.; Yapar, D.; Öztürk, A.M. What is the clinical and functional effect of performing suspension arthroplasty with abductor pollicis longus tendon slip to carpometacarpal joint osteoarthritis of the thumb? Jt. Dis. Relat. Surg. 2022, 33, 149–155. [Google Scholar] [CrossRef]
- Tomaszewski, K.A.; Henry, B.M.; Kumar Ramakrishnan, P.; Roy, J.; Vikse, J.; Loukas, M.; Tubbs, R.S.; Walocha, J.A. Development of the Anatomical Quality Assurance (AQUA) checklist: Guidelines for reporting original anatomical studies. Clin. Anat. 2017, 30, 14–20. [Google Scholar] [CrossRef]
- Fabrizio, P.A.; Clemente, F.R. A Variation in the Organization of Abductor Pollicis Longus. Clin. Anat. 1996, 9, 371–375. [Google Scholar] [CrossRef]
- Karauda, P.; Olewnik, Ł.; Podgórski, M.; Polguj, M.; Ruzik, K.; Szewczyk, B.; Topol, M. Anatomical Variations of the Abductor Pollicis Longus: A Pilot Study. Folia Morphol. 2020, 79, 817–822. [Google Scholar] [CrossRef]
- Prameela, M.D.; Prabhu, L.V.; Murlimanju, B.V.; Pai, M.M.; Rai, R.; Kumar, C.G. Morphological Variants of the Abductor Pollicis Longus and Extensor Pollicis Brevis Tendons: A Cadaveric Study. Muscles Ligaments Tendons J. 2022, 12, 72–78. [Google Scholar] [CrossRef]
- Kaur, A. Accessory Abductor Pollicis Longus: An Anatomical Case Report. J. Anat. Soc. India 2024, 73, 284–286. [Google Scholar] [CrossRef]
- Jaber, N.K.; Charrier, C.; Maouloud, N.; Legendre, O.; Sam, F. Multiple Musculotendinous Variations in the Limbs: A Cadaveric Case Report. Cureus 2025, 17, e77192. [Google Scholar] [CrossRef]
- García-Orozco, L.; Duque-Colorado, J.; Alarcón-Apablaza, J.; Roa, I.; Rojas, M. Striated Musculature: Embryonic and Fetal Development. Int. J. Morphol. 2024, 42, 341–347. [Google Scholar] [CrossRef]
- Besse, L.; Sheeba, C.J.; Holt, M.; Labuhn, M.; Wilde, S.; Feneck, E.; Bell, D.; Kucharska, A.; Logan, M.P.O. Individual Limb Muscle Bundles Are Formed through Progressive Steps Orchestrated by Adjacent Connective Tissue Cells during Primary Myogenesis. Cell Rep. 2020, 30, 3552–3565.e6. [Google Scholar] [CrossRef]
- Wilde, S.; Feneck, E.M.; Mohun, T.J.; Logan, M.P.O. 4D Formation of Human Embryonic Forelimb Musculature. Development 2021, 148, dev194746. [Google Scholar] [CrossRef]
- Deshmukh, V.; Talhar, S.; Muthiyan, G.; Kasat, P.; Chandrasekaran, K.; Sontakke, B. Insights with consensus on Abductor Pollicis Longus from the Central Indian population at Nagpur, Maharashtra. Bioinformation 2023, 19, 1111–1115. [Google Scholar] [CrossRef]
- Perruisseau-Carrier, A.; Artz, M.; Ta, P.; Seizeur, R.; Hu, W.; Le Nen, D. Feasibility of the Abductor Pollicis Longus Hemitendon Transfer for Thumb Opposition: An Anatomical Study. Orthop. Traumatol. Surg. Res. 2023, 109, 103548. [Google Scholar] [CrossRef]
- Opreanu, R.C.; Wechter, J.; Tabbaa, H.; Kepros, J.P.; Baulch, M.; Xie, Y.; Lackey, W.; Katranji, A. Anatomic Variations of the First Extensor Compartment and Abductor Pollicis Longus Tendon in Trapeziometacarpal Arthritis. Hand 2010, 5, 184–189. [Google Scholar] [CrossRef]
- White, A.C.; Byrd, J.J.; McCumber, T.L.; Snow, E.L. Prevalence, Evaluation, and Clinical Implications of a Reticular Tunnel Formed by Uncharacteristic Distal Fibers of the Abductor Pollicis Longus. Transl. Res. Anat. 2023, 34, 100279. [Google Scholar] [CrossRef]
- Marí-Gorreto, J.; San-Millán, M.; Carrera, A.; Tubbs, R.S.; Iwanaga, J.; Cateura, A.; Acquabona, L.; Reina, M.A.; Reina, F. The anatomy of the tendon of abductor pollicis longus and its morphological variations: An anatomical approach emphasizing the clinical relevance. Ann. Anat. 2023, 247, 152068. [Google Scholar] [CrossRef] [PubMed]
- Sheth, A.B.N.; Patra, A.; Mahajan, D. Anatomical variations and developmental insights of tendons in the first extensor compartment of the hand: Cadaveric study with surgical implications. Clin. Ter. 2024, 175, 26–33. [Google Scholar] [CrossRef]
- Rosas, S.; Mesa, C.; Mesa, F. The Abductor Pollicis Longus Tendon as an Alternative Graft in Hand Surgery. J. Hand Surg. Am. 2017, 42, e205–e208. [Google Scholar] [CrossRef]
- Guglielmetti, L.G.B.; Shimba, L.G.; do Santos, L.C.; Severino, F.R.; Severino, N.R.; de Moraes Barros Fucs, P.M.; de Paula Leite Cury, R. The Influence of Femoral Tunnel Length on Graft Rupture after Anterior Cruciate Ligament Reconstruction. J. Orthop. Traumatol. 2017, 18, 243–250. [Google Scholar] [CrossRef][Green Version]
- Bullón, A.; Bravo, E.; Zarbahsh, S.; Barco, R. Reconstruction after chronic extensor pollicis longus ruptures: A new technique. Clin. Orthop. Relat. Res. 2007, 462, 93–98. [Google Scholar] [CrossRef]
- Gulati, H.S.; Ray, B.; Sushma; D’Souza, A.S.; Kumar, N. Morphometry of the Deep Muscles of the Extensor Compartment of the Forearm and Related Variations. Eur. J. Anat. 2014, 18, 171–174. [Google Scholar]
- Duque-Colorado, J.; García-Orozco, L.; Riveros, A.; Del Sol, M. Scapular notch, spinoglenoid notch, and scapular dimensions: Implications on the safe zone of the suprascapular nerve. Anat. Cell Biol. 2025, 58, 54–60. [Google Scholar] [CrossRef] [PubMed]
- Duque-Colorado, J.; Alzate-Mejia, O.A.; del Sol, M. Morphometry of the Scapular Notch and Its Clinical Implication in Suprascapular Nerve Entrapment. Diagnostics 2025, 15, 346. [Google Scholar] [CrossRef] [PubMed]
- Iwanaga, J.; Singh, V.; Ohtsuka, A.; Hwang, Y.; Kim, H.J.; Moryś, J.; Ravi, K.S.; Ribatti, D.; Trainor, P.A.; Sañudo, J.R.; et al. Acknowledging the use of human cadaveric tissues in research papers: Recommendations from anatomical journal editors. Clin. Anat. 2021, 34, 2–4. [Google Scholar] [CrossRef]
- Iwanaga, J.; Kim, H.J.; Akita, K.; Logan, B.M.; Hutchings, R.T.; Ottone, N.; Nonaka, Y.; Anand, M.; Burns, D.; Singh, V.; et al. Ethical Use of Cadaveric Images in Anatomical Textbooks, Atlases, and Journals: A Consensus Response From Authors and Editors. Clin. Anat. 2025, 38, 222–225. [Google Scholar] [CrossRef] [PubMed]
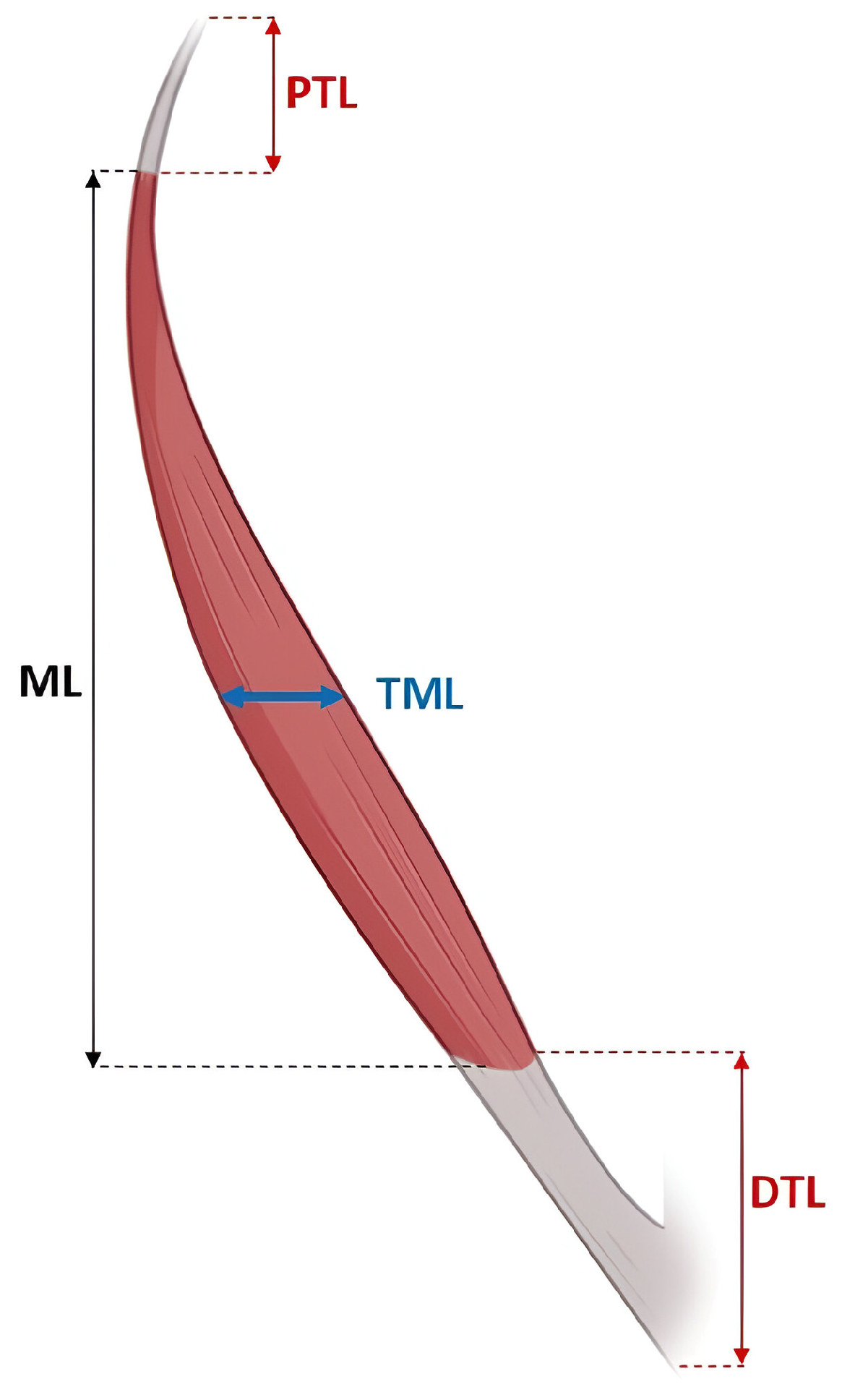
| Parameter | Minimum–Maximum (cm) | Mean ± SD (cm) |
|---|---|---|
| PTL | 0.68–1.41 | 1.20 ± 0.080 |
| DTL | 2.33–6.95 | 3.91 ± 0.52 |
| ML | 2.78–7.28 | 5.3 ± 0.45 |
| TML | 0.33–0.78 | 0.55 ± 0.056 |
| Authors | Population | Morphological Classification of APL | Prevalence (%) | Specimens Analyzed (%) |
|---|---|---|---|---|
| Fabrizio & Clemente [9] | North American | Digastric | 30 | 50 |
| Karauda et al. [10] | Polish | Biceps Multicaudal | 24 50 | 50 |
| Prameela et al. [11] | Indian | Multicaudal | 80.90 | 115 |
| Perruisseau-Carrier et al. [18] | French | Biceps | 73 | 11 |
| This study | Bolivian | Accessory muscle Multicaudal | 43.75 6.25 | 16 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Duque-Colorado, J.; Rodriguez-Torrez, V.H.; García-Orozco, L.; Algieri, R.D.; Ottone, N.E. Prevalence, Morphometric Characteristics of the Accessory Abductor Pollicis Longus Muscle and Clinical Implications: A Cadaveric Study. Diagnostics 2025, 15, 2455. https://doi.org/10.3390/diagnostics15192455
Duque-Colorado J, Rodriguez-Torrez VH, García-Orozco L, Algieri RD, Ottone NE. Prevalence, Morphometric Characteristics of the Accessory Abductor Pollicis Longus Muscle and Clinical Implications: A Cadaveric Study. Diagnostics. 2025; 15(19):2455. https://doi.org/10.3390/diagnostics15192455
Chicago/Turabian StyleDuque-Colorado, Jhonatan, Victor Hugo Rodriguez-Torrez, Laura García-Orozco, Rubén Daniel Algieri, and Nicolás E. Ottone. 2025. "Prevalence, Morphometric Characteristics of the Accessory Abductor Pollicis Longus Muscle and Clinical Implications: A Cadaveric Study" Diagnostics 15, no. 19: 2455. https://doi.org/10.3390/diagnostics15192455
APA StyleDuque-Colorado, J., Rodriguez-Torrez, V. H., García-Orozco, L., Algieri, R. D., & Ottone, N. E. (2025). Prevalence, Morphometric Characteristics of the Accessory Abductor Pollicis Longus Muscle and Clinical Implications: A Cadaveric Study. Diagnostics, 15(19), 2455. https://doi.org/10.3390/diagnostics15192455






