Volumetric Three-Dimensional Evaluation of the Pharyngeal Airway After Orthognathic Surgery in Patients with Skeletal Class III Malocclusion
Abstract
1. Introduction
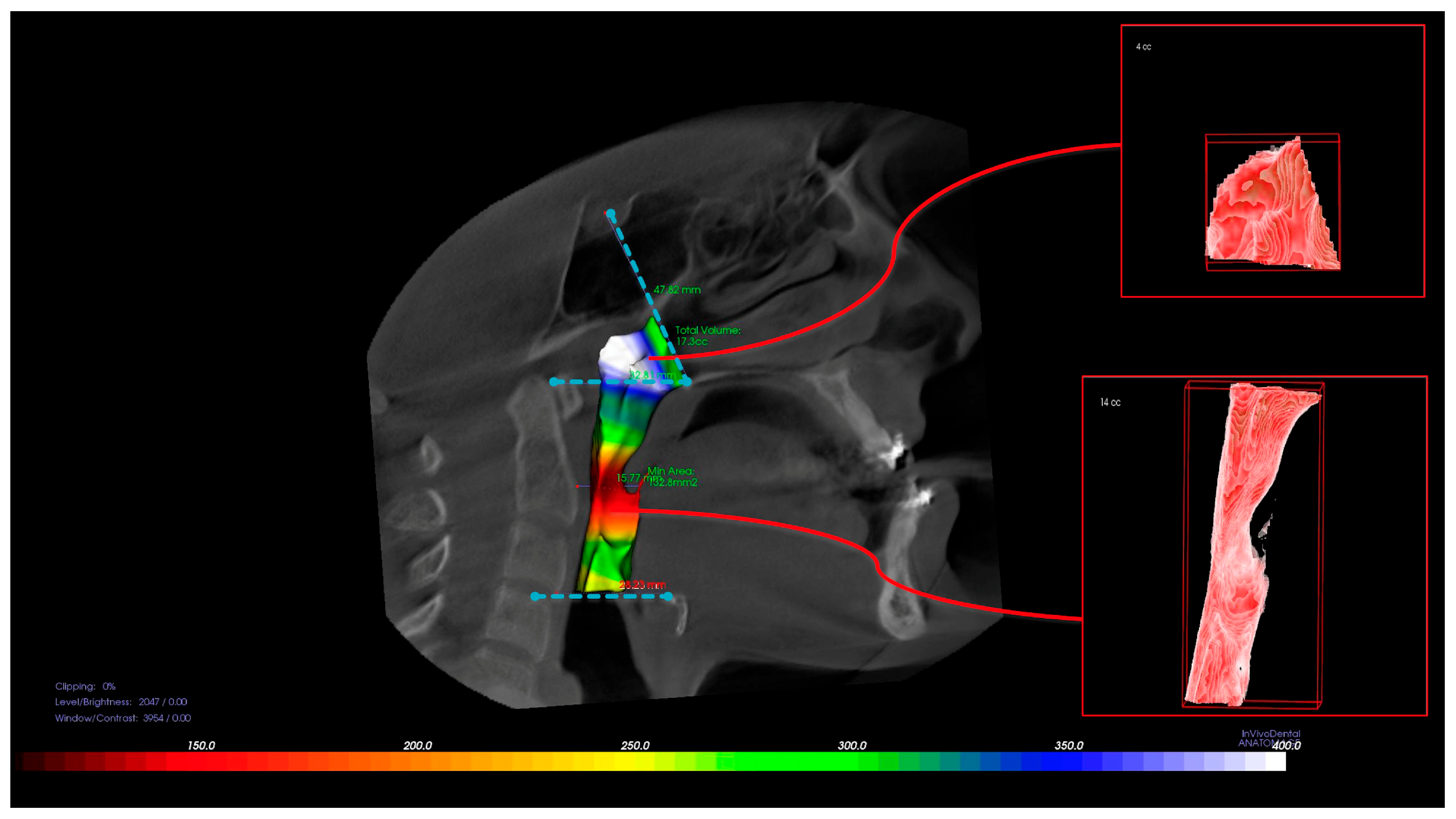
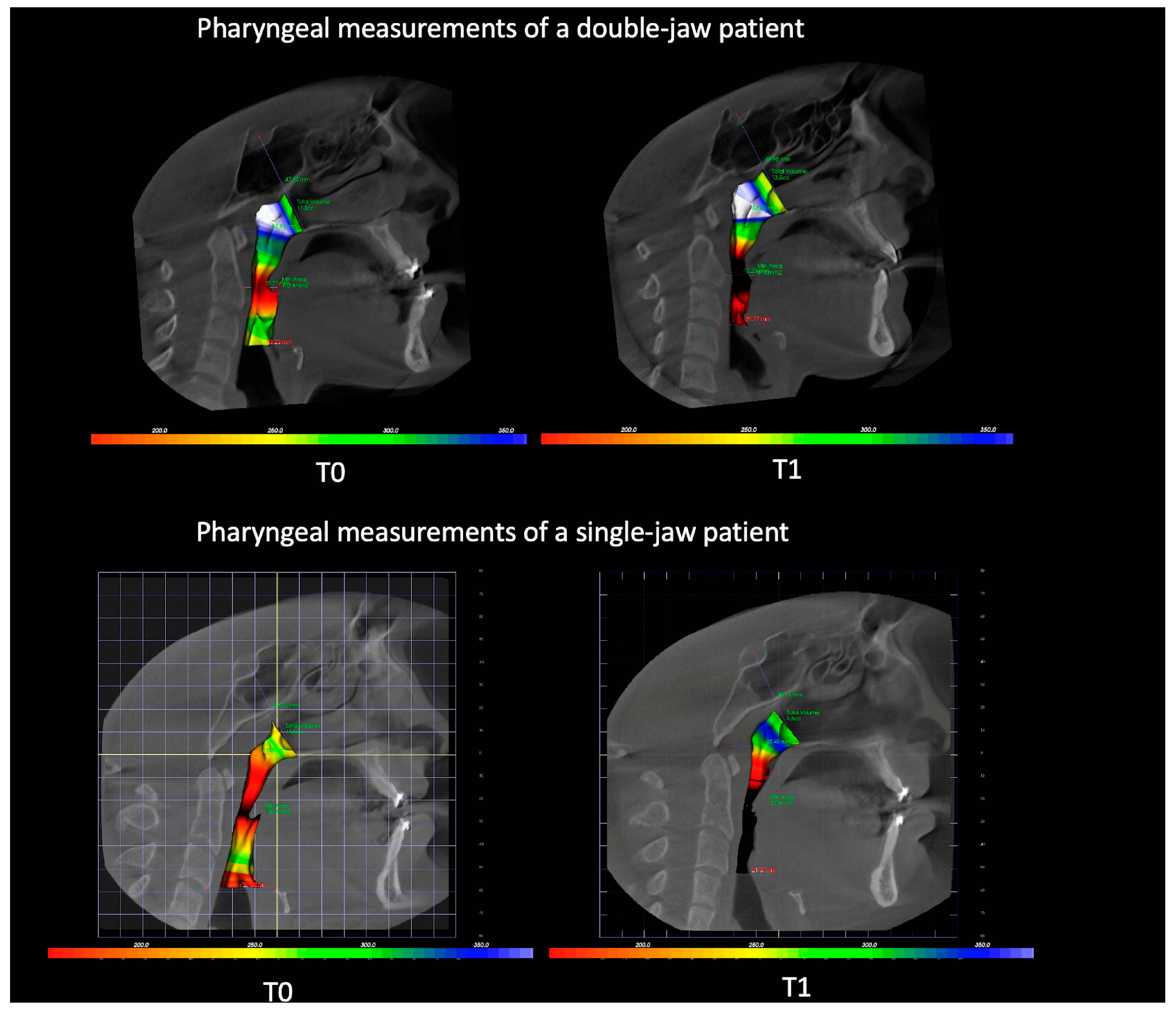
2. Materials and Methods
Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| CBCT | Cone-Beam Computed Tomography |
| OSA | Obstructive Sleep Apnea |
| PAS | Posterior Airway Space |
| 3D | Three-Dimensional |
| 2D | Two-Dimensional |
| NP | Nasopharynx |
| OP | Oropharynx |
| minAx | Most Constructed Area |
References
- Alhammadi, M.S.; Almashraqi, A.A.; Khadhi, A.H.; Arishi, K.A.; Alamir, A.A.; Beleges, E.M.; Halboub, E. Orthodontic camouflage versus orthodontic-orthognathic surgical treatment in borderline class III malocclusion: A systematic review. Clin. Oral Investig. 2022, 26, 6443–6455. [Google Scholar] [CrossRef] [PubMed]
- Woon, S.C.; Thiruvenkatachari, B. Early orthodontic treatment for Class III malocclusion: A systematic review and meta-analysis. Am. J. Orthod. Dentofac. Orthop. 2017, 151, 28–52. [Google Scholar] [CrossRef] [PubMed]
- Christovam, I.O.; Lisboa, C.O.; Ferreira, D.M.; Cury-Saramago, A.A.; Mattos, C.T. Upper airway dimensions in patients undergoing orthognathic surgery: A systematic review and meta-analysis. Int. J. Oral Maxillofac. Surg. 2016, 45, 460–471. [Google Scholar] [CrossRef] [PubMed]
- Grinberg, N.; Whitefield, S.; Kleinman, S.; Ianculovici, C.; Feldman, S.; Peleg, O. Posterior airway compromise following orthognathic surgery in skeletal class III patient—A systematic review and meta-analysis. Sleep Med. 2025, 129, 192–199. [Google Scholar] [CrossRef]
- Parsi, G.K.; Alsulaiman, A.A.; Kotak, B.; Mehra, P.; Will, L.A.; Motro, M. Volumetric changes of the upper airway following maxillary and mandibular advancement using cone beam computed tomography. Int. J. Oral Maxillofac. Surg. 2019, 48, 203–210. [Google Scholar] [CrossRef]
- Lye, K.W. Effect of orthognathic surgery on the posterior airway space (PAS). Ann. Acad. Med. Singap. 2008, 37, 677–682. [Google Scholar] [CrossRef]
- Park, S.B.; Kim, Y.I.; Son, W.S.; Hwang, D.S.; Cho, B.H. Cone-beam computed tomography evaluation of short- and long-term airway change and stability after orthognathic surgery in patients with Class III skeletal deformities: Bimaxillary surgery and mandibular setback surgery. Int. J. Oral Maxillofac. Surg. 2012, 41, 87–93. [Google Scholar] [CrossRef]
- Steegman, R.; Hogeveen, F.; Schoeman, A.; Ren, Y. Cone beam computed tomography volumetric airway changes after orthognathic surgery: A systematic review. Int. J. Oral Maxillofac. Surg. 2023, 52, 60–71. [Google Scholar] [CrossRef]
- Chang, M.K.; Sears, C.; Huang, J.C.; Miller, A.J.; Kushner, H.W.; Lee, J.S. Correlation of Airway Volume With Orthognathic Surgical Movement Using Cone-Beam Computed Tomography. J. Oral Maxillofac. Surg. 2015, 73, S67–S76. [Google Scholar] [CrossRef]
- Valls-Ontañón, A.; Arjooca, S.; Saavedra, O.; Giralt-Hernando, M.; Asensio-Salazar, J.; Haas, O.L., Jr.; Hernández-Alfaro, F. Does Aesthetic Osseous Genioplasty Impact Upper Airway Volume? Aesthetic Surg. J. 2023, 44, 354–362. [Google Scholar] [CrossRef]
- Park, S.-B.; Yoon, J.-K.; Kim, Y.-I.; Hwang, D.-S.; Cho, B.-H.; Son, W.-S. The evaluation of the nasal morphologic changes after bimaxillary surgery in skeletal class III maloccusion by using the superimposition of cone-beam computed tomography (CBCT) volumes. J. Craniomaxillofac. Surg. 2012, 40, e87–e92. [Google Scholar] [CrossRef] [PubMed]
- Chen, F.; Terada, K.; Hua, Y.; Saito, I. Effects of bimaxillary surgery and mandibular setback surgery on pharyngeal airway measurements in patients with Class III skeletal deformities. Am. J. Orthod. Dentofac. Orthop. 2007, 131, 372–377. [Google Scholar] [CrossRef]
- On, S.W.; Kim, H.J.; Cho, D.H.; Moon, Y.R.; Il Song, S. Silent Changes in Sleep Quality Following Mandibular Setback Surgery in Patients with Skeletal Class III Malocclusion: A Prospective Study. Sci. Rep. 2019, 9, 9737. [Google Scholar] [CrossRef] [PubMed]
- Holty, J.E.; Guilleminault, C. Surgical options for the treatment of obstructive sleep apnea. Med. Clin. N. Am. 2010, 94, 479–515. [Google Scholar] [CrossRef] [PubMed]
- Trevisiol, L.; Bersani, M.; Sanna, G.; Nocini, R.; D’Agostino, A. Posterior airways and orthognathic surgery: What really matters for successful long-term results? Am. J. Orthod. Dentofac. Orthop. 2022, 161, e486–e497. [Google Scholar] [CrossRef]
- Pellby, D.; Bengtsson, M. Changes in the upper airway volume after orthognathic surgery: Three-dimensional measurements in a supine body position. Int. J. Oral. Maxillofac. Surg. 2023, 52, 948–955. [Google Scholar] [CrossRef]
- Gonçales, E.S.; Rocha, J.F.; Gonçales, A.G.B.; Yaedú, R.Y.F.; Sant’Ana, E. Computerized cephalometric study of the pharyngeal airway space in patients submitted to orthognathic surgery. J. Maxillofac. Oral 2014, 13, 253–258. [Google Scholar] [CrossRef]
- Sears, C.R.; Miller, A.J.; Chang, M.K.; Huang, J.C.; Lee, J.S. Comparison of pharyngeal airway changes on plain radiography and cone-beam computed tomography after orthognathic surgery. J. Oral Maxillofac. Surg. 2011, 69, e385–e394. [Google Scholar] [CrossRef]
- Obelenis Ryan, D.P.; Bianchi, J.; Ignacio, J.; Wolford, L.M.; Goncalves, J.R. Cone-beam computed tomography airway measurements: Can we trust them? Am. J. Orthod. Dentofac. Orthop. 2019, 156, 53–60. [Google Scholar] [CrossRef]
- Lenza, M.G.; Lenza, M.M.; Dalstra, M.; Melsen, B.; Cattaneo, P.M. An analysis of different approaches to the assessment of upper airway morphology: A CBCT study. Orthod. Craniofacial Res. 2010, 13, 96–105. [Google Scholar] [CrossRef]
- Guven, O.; Saracoglu, U. Changes in pharyngeal airway space and hyoid bone positions after body ostectomies and sagittal split ramus osteotomies. J. Craniofacial Surg. 2005, 16, 23–30. [Google Scholar] [CrossRef] [PubMed]
- Hochban, W.; Schurmann, R.; Brandenburg, U.; Conradt, R. Mandibular setback for surgical correction of mandibular hyperplasia--does it provoke sleep-related breathing disorders? Int. J. Oral Maxillofac. Surg. 1996, 25, 333–338. [Google Scholar] [CrossRef]
- Hwang, S.; Chung, C.J.; Choi, Y.J.; Huh, J.K.; Kim, K.H. Changes of hyoid, tongue and pharyngeal airway after mandibular setback surgery by intraoral vertical ramus osteotomy. Angle Orthod. 2010, 80, 302–308. [Google Scholar] [CrossRef] [PubMed]
- Degerliyurt, K.; Ueki, K.; Hashiba, Y.; Marukawa, K.; Nakagawa, K.; Yamamoto, E. A comparative CT evaluation of pharyngeal airway changes in class III patients receiving bimaxillary surgery or mandibular setback surgery. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endodontology 2008, 105, 495–502. [Google Scholar] [CrossRef]
- Hatab, N.A.; Konstantinovic, V.S.; Mudrak, J.K. Pharyngeal airway changes after mono- and bimaxillary surgery in skeletal class III patients: Cone-beam computed tomography evaluation. J. Craniomaxillofac. Surg. 2015, 43, 491–496. [Google Scholar] [CrossRef] [PubMed]
- Hong, J.S.; Oh, K.M.; Kim, B.R.; Kim, Y.J.; Park, Y.H. Three-dimensional analysis of pharyngeal airway volume in adults with anterior position of the mandible. Am. J. Orthod. Dentofac. Orthop. 2011, 140, e161–e169. [Google Scholar] [CrossRef]
- Eggensperger, N.; Smolka, K.; Johner, A.; Rahal, A.; Thuer, U.; Iizuka, T. Long-term changes of hyoid bone and pharyngeal airway size following advancement of the mandible. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endodontology 2005, 99, 404–410. [Google Scholar] [CrossRef]
- Jakobsone, G.; Stenvik, A.; Espeland, L. The effect of maxillary advancement and impaction on the upper airway after bimaxillary surgery to correct Class III malocclusion. Am. J. Orthod. Dentofac. Orthop. 2011, 139, e369–e376. [Google Scholar] [CrossRef]
- Giap, H.-V.; Shin, J.W.; Chae, H.S.; Kim, Y.H.; Paeng, J.-Y.; Choi, H.W. Pharyngeal airway morphology in skeletal class III with mandibular asymmetry is improved after bimaxillary orthognathic surgery. J. Oral Maxillofac. Surg. 2021, 79, 1107–1121. [Google Scholar] [CrossRef]
- Mattos, C.T.; Vilani, G.N.; Sant’Anna, E.F.; Ruellas, A.C.; Maia, L.C. Effects of orthognathic surgery on oropharyngeal airway: A meta-analysis. Int. J. Oral Maxillofac. Surg. 2011, 40, 1347–1356. [Google Scholar] [CrossRef]
- Giralt-Hernando, M.; Valls-Ontanon, A.; Guijarro-Martinez, R.; Masia-Gridilla, J.; Hernandez-Alfaro, F. Impact of surgical maxillomandibular advancement upon pharyngeal airway volume and the apnoea-hypopnoea index in the treatment of obstructive sleep apnoea: Systematic review and meta-analysis. BMJ Open Respir. Res. 2019, 6, e000402. [Google Scholar] [CrossRef]
- Daluz, A.D.J.; da Silva, T.V.S.; Torres, B.O.; Costa, D.F.N.; Santos, L.A.M. Long-term airway evolution after orthognathic surgery: Systematic Review. J. Stomatol. Oral Maxillofac. Surg. 2022, 123, 191–198. [Google Scholar] [CrossRef] [PubMed]
- Agarwal, S.; Datana, S.; Sahoo, N.; Bhandari, S. Evaluation of airway dimensions following mandibular setback with surgery-first orthognathic versus conventional orthognathic approach. J. Maxillofac. Oral Surg. 2021, 20, 296–303. [Google Scholar] [CrossRef]
- Andrews, B.T.; Lakin, G.E.; Bradley, J.P.; Kawamoto, H.K., Jr. Orthognathic surgery for obstructive sleep apnea: Applying the principles to new horizons in craniofacial surgery. J. Craniofacial Surg. 2012, 23, 2028–2041. [Google Scholar] [CrossRef]
- Khaghaninejad, M.S.; Khojastehpour, L.; Danesteh, H.; Changizi, M.; Ahrari, F. Changes in the pharyngeal airway after different orthognathic procedures for correction of class III dysplasia. Maxillofac. Plast. Reconstr. Surg. 2022, 44, 23. [Google Scholar] [CrossRef] [PubMed]
- Francisco, I.; Travassos, R.; Baptista Paula, A.; Oliveiros, B.; Marques, F.; Prata Ribeiro, M.; McEvoy, M.; Santos, M.; Oliveira, C.; Marto, C.M. Evaluation of quality of life after orthognathic surgery in obstructive sleep apnea syndrome: A systematic review. Angle Orthod. 2025, 95, 104–125. [Google Scholar] [CrossRef]
- Lee, U.L.; Oh, H.; Min, S.K.; Shin, J.H.; Kang, Y.S.; Lee, W.W.; Han, Y.E.; Choi, Y.J.; Kim, H.J. The structural changes of upper airway and newly developed sleep breathing disorders after surgical treatment in class III malocclusion subjects. Medicine 2017, 96, e6873. [Google Scholar] [CrossRef] [PubMed]
- Abramson, Z.; Susarla, S.; Troulis, M.; Kaban, L. Age-related changes of the upper airway assessed by 3-dimensional computed tomography. J. Craniofacial Surg. 2009, 20 (Suppl. 1), 657–663. [Google Scholar] [CrossRef]
- Schendel, S.A.; Jacobson, R.; Khalessi, S. Airway growth and development: A computerized 3-dimensional analysis. J. Oral Maxillofac. Surg. 2012, 70, 2174–2183. [Google Scholar] [CrossRef]
- El, H.; Palomo, J.M. Measuring the airway in 3 dimensions: A reliability and accuracy study. Am. J. Orthod. Dentofac. Orthop. 2010, 137, S50.e1–S50.e9; discussion S50–S52. [Google Scholar] [CrossRef]
- Holmberg, H.; Linder-Aronson, S. Cephalometric radiographs as a means of evaluating the capacity of the nasal and nasopharyngeal airway. Am. J. Orthod. 1979, 76, 479–490. [Google Scholar] [CrossRef]
- Tselnik, M.; Pogrel, M.A. Assessment of the pharyngeal airway space after mandibular setback surgery. J. Oral Maxillofac. Surg. 2000, 58, 282–285; discussion 285–287. [Google Scholar] [CrossRef]
- Uesugi, T.; Kobayashi, T.; Hasebe, D.; Tanaka, R.; Ike, M.; Saito, C. Effects of orthognathic surgery on pharyngeal airway and respiratory function during sleep in patients with mandibular prognathism. Int. J. Oral Maxillofac. Surg. 2014, 43, 1082–1090. [Google Scholar] [CrossRef]
- He, J.; Wang, Y.; Hu, H.; Liao, Q.; Zhang, W.; Xiang, X.; Fan, X. Impact on the upper airway space of different types of orthognathic surgery for the correction of skeletal class III malocclusion: A systematic review and meta-analysis. Int. J. Surg. 2017, 38, 31–40. [Google Scholar] [CrossRef]
- Shin, J.-H.; Kim, M.-A.; Park, I.-Y.; Park, Y.-H. A 2-year follow-up of changes after bimaxillary surgery in patients with mandibular prognathism: 3-dimensional analysis of pharyngeal airway volume and hyoid bone position. Int. J. Oral Maxillofac. Surg. 2015, 73, 340.e1–340.e9. [Google Scholar] [CrossRef]
- Lee, S.-T.; Park, J.-H.; Kwon, T.-G. Influence of mandibular setback surgery on three-dimensional pharyngeal airway changes. Int. J. Oral Maxillofac. Surg. 2019, 48, 1057–1065. [Google Scholar] [CrossRef]
- An, J.H.; Park, S.-B.; Choi, Y.-K.; Lee, S.H.; Kim, K.B.; Kim, Y.-I. Cone-beam computed tomography evaluation of pharyngeal airway space changes after bimaxillary orthognathic surgery in patients with class III skeletal deformities: A 6-year follow-up study. Int. J. Oral Maxillofac. Surg. 2019, 77, 2534–2544. [Google Scholar] [CrossRef] [PubMed]
- Ali, S.A.; Marrapodi, M.M.; Shivakumar, G.C.; Shivakumar, S.; Hurkadle, J.; Cicciu, M.; Minervini, G. Efficacy of Orthognathic Surgery in OSAS Patients: A Systematic Review and Meta-Analysis. J. Oral Rehabil. 2025, 52, 554–565. [Google Scholar] [CrossRef] [PubMed]
- Kongsong, W.; Rochanavibhata, S.; Changsiripun, C.; Sinpitaksakul, P.; Chirakalwasan, N. Effects of mandibular setback surgery using the surgery-first approach versus conventional orthognathic approach on upper airway change and sleep quality. Head Face Med. 2025, 21, 37. [Google Scholar] [CrossRef]
- Scherer, J.; Sheats, R.; Phillips III, C. Class III bimaxillary orthognathic surgery and sleep disordered breathing outcomes. J. Dent. Sleep Med. 2015, 2, 157–162. [Google Scholar] [CrossRef]
- Chen, H.; Aarab, G.; de Ruiter, M.H.; de Lange, J.; Lobbezoo, F.; van der Stelt, P.F. Three-dimensional imaging of the upper airway anatomy in obstructive sleep apnea: A systematic review. Sleep Med. 2016, 21, 19–27. [Google Scholar] [CrossRef] [PubMed]
- Dos Santos, L.F.; Albright, D.A.; Dutra, V.; Bhamidipalli, S.S.; Stewart, K.T.; Polido, W.D. Is there a correlation between airway volume and maximum constriction area location in different dentofacial deformities? J. Oral Maxillofac. Surg. 2020, 78, 1415.e1–1415.e10. [Google Scholar] [CrossRef]
- Tso, H.H.; Lee, J.S.; Huang, J.C.; Maki, K.; Hatcher, D.; Miller, A.J. Evaluation of the human airway using cone-beam computerized tomography. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endodontology 2009, 108, 768–776. [Google Scholar] [CrossRef] [PubMed]
- Avrahami, E.; Englender, M. Relation between CT axial cross-sectional area of the oropharynx and obstructive sleep apnea syndrome in adults. AJNR Am. J. Neuroradiol. 1995, 16, 135–140. [Google Scholar] [PubMed]
- Abramson, Z.; Susarla, S.; August, M.; Troulis, M.; Kaban, L. Three-dimensional computed tomographic analysis of airway anatomy in patients with obstructive sleep apnea. J. Oral Maxillofac. Surg. 2010, 68, 354–362. [Google Scholar] [CrossRef]
- Partinen, M.; Guilleminault, C.; Quera-Salva, M.A.; Jamieson, A. Obstructive sleep apnea and cephalometric roentgenograms. The role of anatomic upper airway abnormalities in the definition of abnormal breathing during sleep. Chest 1988, 93, 1199–1205. [Google Scholar] [CrossRef]
- Li, Y.M.; Liu, J.L.; Zhao, J.L.; Dai, J.; Wang, L.; Chen, J.W. Morphological changes in the pharyngeal airway of female skeletal class III patients following bimaxillary surgery: A cone beam computed tomography evaluation. Int. J. Oral Maxillofac. Surg. 2014, 43, 862–867. [Google Scholar] [CrossRef]
- Gokce, S.M.; Gorgulu, S.; Gokce, H.S.; Bengi, A.O.; Karacayli, U.; Ors, F. Evaluation of pharyngeal airway space changes after bimaxillary orthognathic surgery with a 3-dimensional simulation and modeling program. Am. J. Orthod. Dentofac. Orthop. 2014, 146, 477–492. [Google Scholar] [CrossRef]
- Kang, N.E.; Lee, D.H.; In Seo, J.; Lee, J.K.; Song, S.I. Postoperative changes in the pharyngeal airway space through computed tomography evaluation after mandibular setback surgery in skeletal class III patients: 1-year follow-up. Maxillofac. Plast. Reconstr. Surg. 2021, 43, 31. [Google Scholar] [CrossRef]
- Kawamata, A.; Fujishita, M.; Ariji, Y.; Ariji, E. Three-dimensional computed tomographic evaluation of morphologic airway changes after mandibular setback osteotomy for prognathism. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endodontology 2000, 89, 278–287. [Google Scholar] [CrossRef]

| Amount of Movement (mm) | Maxilla | Mandible | p |
|---|---|---|---|
| Double jaw | 5.28 ± 2.07 | 7.84 ± 2.43 | 0.339 |
| Single jaw | ------- | 7.52 ± 1.2 |
| Double Jaw | Single Jaw | |||||||
|---|---|---|---|---|---|---|---|---|
| T1 | T2 | p | d | T1 | T2 | p | d | |
| Oropharynx volume (mm3) | 17,097 ± 5675 | 14,290 ± 5835 | 0.017 | 0.488 | 15,620 ± 5040 | 12,444 ± 4701 | 0.010 * | 0.652 |
| Nasopharynx volume (mm3) | 5316 ± 1948 | 6064 ± 1899 | 0.010 * | 0.389 | 4563 ± 2125 | 4693 ± 2201 | 0.551 | 0.06 |
| Total airway volume (mm3) | 25,741 ± 9195 | 22,164 ± 6262 | 0.075 | 0.455 | 20,452 ± 7754 | 16,846 ± 6529 | 0.010 * | 0.503 |
| PAS (mm) | 9.60 ± 4.17 | 6.43 ± 3.07 | 0.002 * | 0.866 | 9.68 ± 2.69 | 6.50 ± 2.55 | 0.000 * | 1.213 |
| minAx (mm2) | 189 (77.9–300) | 100 (36.9–236.8) | 0.001 * | -- | 168.02 ± 78.51 | 119.13 ± 75.93 | 0.000 * | 0.633 |
| Double Jaw | Single Jaw | p | |
|---|---|---|---|
| ∆OP (OP2 − OP1) | −2762 ± 3772 | −3408 ± 3343 | 0.674 |
| ∆NP (NP2 − NP1) | 707 ± 922 | −197 ± 1009 | 0.036 |
| ∆TOTAL (TOTAL2 − TOTAL1) | −2055 ± 4233 | −3605 ± 3823 | 0.375 |
| ∆PAS (PAS2 − PAS1) | −3.18 ± 2.9 | −3.17 ± 1.6 | 0.997 |
| ∆minAx (minAx2 − minAx1) | −71.8 (−172.8–175.72) | −44.3 (−81.9–17.1) | 0.239 |
| ∆minAx | ∆PAS | ∆TOTAL | ||
|---|---|---|---|---|
| ∆minAx | Correlation Coefficient | 1 | 0.427 * | 0.457 * |
| p | 0.042 | 0.029 | ||
| N | 23 | 23 | 23 | |
| ∆PAS | Correlation Coefficient | 0.427 * | 1 | 0.267 |
| p | 0.042 | 0.218 | ||
| N | 23 | 23 | 23 | |
| ∆TOTAL | Correlation Coefficient | 0.457 * | 0.267 | 1 |
| p | 0.029 | 0.218 | ||
| N | 23 | 23 | 23 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Oz, A.Z.; El, H.; Oz, A.A.; Palomo, J.M. Volumetric Three-Dimensional Evaluation of the Pharyngeal Airway After Orthognathic Surgery in Patients with Skeletal Class III Malocclusion. Diagnostics 2025, 15, 2217. https://doi.org/10.3390/diagnostics15172217
Oz AZ, El H, Oz AA, Palomo JM. Volumetric Three-Dimensional Evaluation of the Pharyngeal Airway After Orthognathic Surgery in Patients with Skeletal Class III Malocclusion. Diagnostics. 2025; 15(17):2217. https://doi.org/10.3390/diagnostics15172217
Chicago/Turabian StyleOz, Aslihan Zeynep, Hakan El, Abdullah Alper Oz, and Juan Martin Palomo. 2025. "Volumetric Three-Dimensional Evaluation of the Pharyngeal Airway After Orthognathic Surgery in Patients with Skeletal Class III Malocclusion" Diagnostics 15, no. 17: 2217. https://doi.org/10.3390/diagnostics15172217
APA StyleOz, A. Z., El, H., Oz, A. A., & Palomo, J. M. (2025). Volumetric Three-Dimensional Evaluation of the Pharyngeal Airway After Orthognathic Surgery in Patients with Skeletal Class III Malocclusion. Diagnostics, 15(17), 2217. https://doi.org/10.3390/diagnostics15172217









