Non-Invasive Dry Eye Disease Detection Using Infrared Thermography Images: A Proof-of-Concept Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Data Acquisition
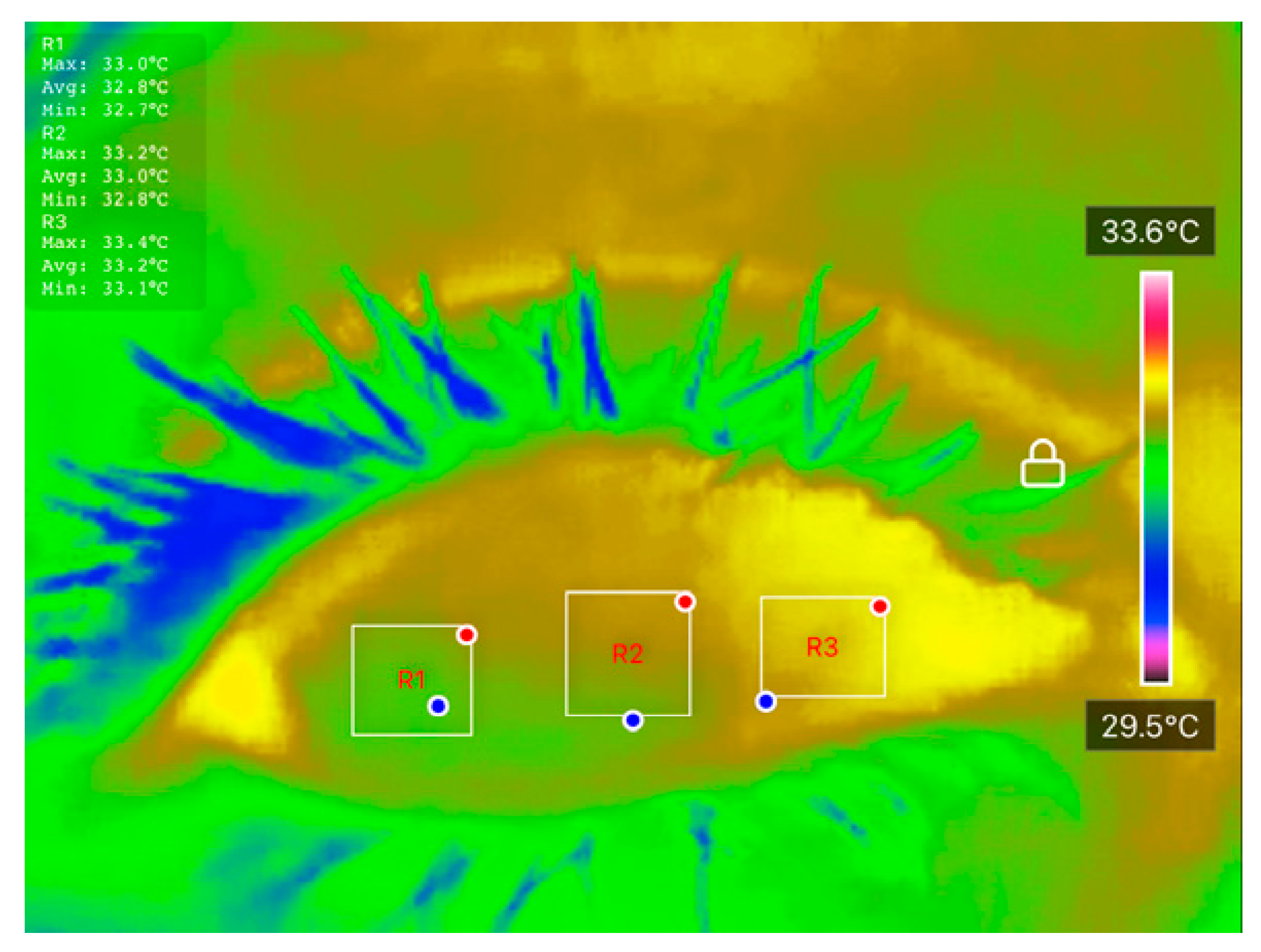
2.2. Preprocessing of DITI Data
2.3. Statistical Analysis
2.4. Machine Learning Classification
3. Results
3.1. DITI Dataset Processing and Analysis
3.2. Feature Selection and Correlation Analysis
3.3. Evaluation of Classification Performance Using Machine Learning
3.3.1. Support Vector Machine Classifier
3.3.2. k-Nearest Neighbours Classifier
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| DED | Dry Eye Disease |
| DITI | Digital Infrared Thermal Imaging |
| DL | Deep Learning |
| ML | Machine Learning |
| OST | Ocular Surface Temperature |
| NC | Nasal Cornea |
| CC | Center Cornea |
| TC | Temporal Cornea |
| TBUT | Tear Break Up Time |
| OSDI | Ocular Surface Disease Index |
| SVM | Support Vector Machine |
| k-NN | k-Nearest Neighbours |
References
- Findlay, Q.; Reid, K. Dry eye disease: When to treat and when to refer. Aust. Prescr. 2018, 41, 160–163. [Google Scholar] [CrossRef] [PubMed]
- Tsubota, K.; Yokoi, N.; Watanabe, H.; Dogru, M.; Kojima, T.; Yamada, M.; Kinoshita, S.; Kim, H.M.; Tchah, H.W.; Hyon, J.Y.; et al. A New Perspective on Dry Eye Classification: Proposal by the Asia Dry Eye Society. Eye Contact Lens 2020, 46, S2–S13. [Google Scholar] [CrossRef] [PubMed]
- Lemp, M.A. Report of the National Eye Institute/Industry workshop on Clinical Trials in Dry Eyes. CLAO J. 1995, 21, 221–232. [Google Scholar] [PubMed]
- Al-Mohtaseb, Z.; Schachter, S.; Lee, B.S.; Garlich, J.; Trattler, W. The relationship between dry eye disease and digital screen use. Clin. Ophthalmol. 2021, 15, 3811–3820. [Google Scholar] [CrossRef]
- Soifer, M.; Azar, N.S.; Mousa, H.M.; Perez, V.L. Ocular Surface Inflammatory Disorders (OSID): A Collective of Systemic Etiologies Which Cause or Amplify Dry Eye Syndrome. Front. Med. 2022, 9, 949202. [Google Scholar] [CrossRef]
- Baudouin, C.; Irkeç, M.; Messmer, E.M.; Benítez-del-Castillo, J.M.; Bonini, S.; Figueiredo, F.C.; Geerling, G.; Labetoulle, M.; Lemp, M.; Rolando, M.; et al. Clinical impact of inflammation in dry eye disease: Proceedings of the ODISSEY group meeting. Acta Ophthalmol. 2018, 96, 111–119. [Google Scholar] [CrossRef]
- Stern, M.E.; Pflugfelder, S.C. Inflammation in Dry Eye. Ocul. Surf. 2004, 2, 124–130. [Google Scholar] [CrossRef]
- Mohamed, H.B.; Abd El-Hamid, B.N.; Fathalla, D.; Fouad, E.A. Current trends in pharmaceutical treatment of dry eye disease: A review. Eur. J. Pharm. Sci. 2022, 175, 106206. [Google Scholar] [CrossRef]
- Wolffsohn, J.S.; Arita, R.; Chalmers, R.; Djalilian, A.; Dogru, M.; Dumbleton, K.; Gupta, P.K.; Karpecki, P.; Lazreg, S.; Pult, H.; et al. TFOS DEWS II Diagnostic Methodology report. Ocul. Surf. 2017, 15, 539–574. [Google Scholar] [CrossRef]
- Zhang, Q.; Wu, Y.; Song, Y.; Qin, G.; Yang, L.; Talwar, S.S.; Lin, T.; Talwar, G.D.S.; Zhang, H.; Xu, L.; et al. Screening Evaporative Dry Eyes Severity Using an Infrared Image. J. Ophthalmol. 2021, 2021, 8396503. [Google Scholar] [CrossRef]
- Kesztyüs, D.; Brucher, S.; Wilson, C.; Kesztyüs, T. Use of Infrared Thermography in Medical Diagnosis, Screening, and Disease Monitoring: A Scoping Review. Medicina 2023, 59, 2139. [Google Scholar] [CrossRef]
- Morgan, P.B.; Tullo, A.B.; Efron, N. Infrared thermography of the tear film in dry eye. Eye 1995, 9, 615–618. [Google Scholar] [CrossRef] [PubMed]
- Sudarshan, V.K.; Koh, J.E.W.; Acharya, U.R.; Tan, J.H.; Mookiah, M.R.K.; Chua, C.K.; Tong, L. Evaluation of Evaporative Dry Eye Disease Using Thermal Images of Ocular Surface Regions with DWT and Gabor Transform. In Application of Infrared to Biomedical Sciences; Springer: Singapore, 2017; pp. 359–375. [Google Scholar]
- Gulias-Cañizo, R.; Rodríguez-Malagón, M.E.; Botello-González, L.; Belden-Reyes, V.; Amparo, F.; Garza-Leon, M. Applications of Infrared Thermography in Ophthalmology. Life 2023, 13, 723. [Google Scholar] [CrossRef]
- Su, T.-Y.; Chang, S.-W. Normalized ocular surface temperature models for tear film characteristics and dry eye disease evaluation. Ocul. Surf. 2021, 19, 74–82. [Google Scholar] [CrossRef] [PubMed]
- Aljarousha, M.; Abd Rahman, A.A.; Badarudin, N.E.; Che Azemin, M.Z.; Awad, K. Prevalence and Risk Factors of Dry Eye Disease in Kuantan, Malaysia. Makara J. Health Res. 2018, 22, 27–33. [Google Scholar] [CrossRef]
- Kementerian Kesihatan Malaysia Petunjuk Kesihatan. 2024. Available online: https://www.moh.gov.my/moh/resources/Penerbitan/Penerbitan%20Utama/HEALTH%20INDICATOR/Petunjuk_Kesihatan_2024_-_latest.pdf (accessed on 24 July 2025).
- Gammoh, Y.; Morjaria, P.; Block, S.; Massie, J.; Hendicott, P. 2023 Global Survey of Optometry: Defining Variations of Practice, Regulation and Human Resources Between Countries. Clin. Optom. 2024, 16, 211–220. [Google Scholar] [CrossRef] [PubMed]
- Schiffman, R.M. Reliability and Validity of the Ocular Surface Disease Index. Arch. Ophthalmol. 2000, 118, 615. [Google Scholar] [CrossRef]
- Alsaqr, A.M. Remarks on the use of Pearson’s and Spearman’s correlation coefficients in assessing relationships in ophthalmic data. Afr. Vis. Eye Health 2021, 80, a612. [Google Scholar] [CrossRef]
- Su, T.Y.; Ho, W.T.; Lu, C.Y.; Chang, S.W.; Chiang, H.K. Correlations among ocular surface temperature difference value, the tear meniscus height, Schirmer’s test and fluorescein tear film break up time. Br. J. Ophthalmol. 2015, 99, 482–487. [Google Scholar] [CrossRef]
- Shah, A.M.; Galor, A. Impact of Ocular Surface Temperature on Tear Characteristics: Current Insights. Clin. Optom. 2021, 13, 51–62. [Google Scholar] [CrossRef]
- Ding, J.E.; Kim, Y.H.; Yi, S.M.; Graham, A.D.; Li, W.; Lin, M.C. Ocular surface cooling rate associated with tear film characteristics and the maximum interblink period. Sci. Rep. 2021, 11, 15030. [Google Scholar] [CrossRef] [PubMed]
- Abusharha, A. Analysis of Ocular Surface Temperature in Patients with Dry Eye. Med. J. Cairo Univ. 2021, 89, 2549–2553. [Google Scholar] [CrossRef]
- Deo, N.; Nagrale, P. Dry Eye Disease: An Overview of Its Risk Factors, Diagnosis, and Prevalence by Age, Sex, and Race. Cureus 2024, 16, e54028. [Google Scholar] [CrossRef]
- Wu, C.; Huang, Y.; Xu, B.; Li, B.; Zhuang, S.; Cao, G.; Hu, Y.; Gu, Z. Comparing the corneal temperature of dry eyes with that of normal eyes via high-resolution infrared thermography. Front. Med. 2025, 11, 1526165. [Google Scholar] [CrossRef]
- Abreau, K.; Callan, C.; Kottaiyan, R.; Zhang, A.; Yoon, G.; Aquavella, J.V.; Zavislan, J.; Hindman, H.B. Temperatures of the Ocular Surface, Lid, and Periorbital Regions of Sjögren’s, Evaporative, and Aqueous-Deficient Dry Eyes Relative to Normals. Ocul. Surf. 2016, 14, 64–73. [Google Scholar] [CrossRef]
- Su, T.Y.; Hwa, C.K.; Liu, P.H.; Wu, M.H.; Chang, D.O.; Su, P.F.; Chang, S.W.; Chiang, H.K. Noncontact detection of dry eye using a custom designed infrared thermal image system. J. Biomed. Opt. 2011, 16, 046009. [Google Scholar] [CrossRef]
- Acharya, U.R.; Tan, J.H.; Koh, J.E.W.; Sudarshan, V.K.; Yeo, S.; Too, C.L.; Chua, C.K.; Ng, E.Y.K.; Tong, L. Automated diagnosis of dry eye using infrared thermography images. Infrared Phys. Technol. 2015, 71, 263–271. [Google Scholar] [CrossRef]
- Sudarshan, V.K.; Koh, J.E.W.; Tan, J.H.; Hagiwara, Y.; Chua, K.C.; NG, E.Y.K.; Tong, L. Performance Evaluation of Dry Eye Detection System Using Higher-Order Spectra Features For Different Noise Levels in IR Thermal Images. J. Mech. Med. Biol. 2017, 17, 1740010. [Google Scholar] [CrossRef]






| 0 s | 1 s | 2 s | 3 s | 4 s |
|---|---|---|---|---|
 |  |  |  |  |
| NC = 33.2 °C CC = 33.0 °C TC = 32.8 °C | NC = 33.1 °C CC = 32.9 °C TC = 32.9 °C | NC = 32.9 °C CC = 32.9 °C TC = 32.9 °C | NC = 32.7 °C CC = 32.7 °C TC = 32.7 °C | NC = 32.7 °C CC = 32.7 °C TC = 32.7 °C |
| Parameters | Normal | DED | Shapiro-p |
|---|---|---|---|
| Number of eyes | 20 | 20 | - |
| Age (year) | 31.25 ± 17.57 | 25.63 ± 10.63 | <0.001 |
| Gender (female%, n) | 65% (13) | 85% (17) | - |
| TBUT (s) | 5.85 ± 1.14 | 2.37 ± 0.60 | <0.001 |
| OSDI score | 15.90 ± 8.48 | 37.43 ± 6.83 | 0.035 |
| Body temperature (°C) | 33.62 ± 0.92 | 33.77 ± 0.54 | <0.001 |
| Parameter | Normal | DED | |
|---|---|---|---|
| ) | NC | 0.58 ± 0.20 | 0.51 ± 0.18 |
| CC | 0.62 ± 0.22 | 0.52 ± 0.21 | |
| TC | 0.57 ± 0.24 | 0.49 ± 0.22 | |
| ) | NC | −0.071 ± 0.06 | −0.233 ± 0.05 |
| CC | −0.074 ± 0.05 | −0.228 ± 0.04 | |
| TC | −0.074 ± 0.06 | −0.217 ± 0.06 | |
| Parameter | Normal | DED | Shapiro-p | |
|---|---|---|---|---|
| NC | 33.99 ± 0.44 | 33.99 ± 0.41 | 0.075 | |
| Starting OST 0 s (°C) | CC | 33.83 ± 0.51 | 33.75 ± 0.45 | 0.515 |
| TC | 33.80 ± 0.52 | 33.77 ± 0.41 | 0.035 | |
| NC | 33.85 ± 0.46 | 33.68 ± 0.42 | 0.342 | |
| OST at 1 s (°C) | CC | 33.64 ± 0.50 | 33.42 ± 0.51 | 0.184 |
| TC | 33.68 ± 0.51 | 33.47 ± 0.45 | 0.479 | |
| NC | 33.79 ± 0.53 | 33.46 ± 0.40 | 0.589 | |
| OST at 2 s (°C) | CC | 33.60 ± 0.56 | 33.21 ± 0.46 | 0.539 |
| TC | 33.61 ± 0.56 | 33.29 ± 0.45 | 0.230 | |
| NC | 33.70 ± 0.53 | 33.26 ± 0.36 | 0.769 | |
| OST at 3 s (°C) | CC | 33.54 ± 0.57 | 33.02 ± 0.43 | 0.806 |
| TC | 33.55 ± 0.55 | 33.08 ± 0.44 | 0.337 | |
| NC | 33.71 ± 0.51 | 33.06 ± 0.39 | 0.852 | |
| OST at 4 s (°C) | CC | 33.53 ± 0.59 | 32.84 ± 0.45 | 0.253 |
| TC | 33.51 ± 0.59 | 32.90 ± 0.46 | 0.133 | |
| Main Features | t | p | |
|---|---|---|---|
| ) | NC | −1.109 | 0.275 |
| CC | −1.483 | 0.147 | |
| TC | −1.007 | 0.320 | |
| ) | NC | −0.004 | 0.997 |
| CC | −0.504 | 0.617 | |
| TC | −0.203 | 0.840 | |
| ) | NC | −9.034 | <0.001 |
| CC | −9.851 | <0.001 | |
| TC | −7.29 | <0.001 | |
| Secondary Features | t | p | |
| ) | NC | −1.165 | 0.251 |
| CC | −1.361 | 0.182 | |
| TC | −1.312 | 0.198 | |
| ) | NC | −2.165 | 0.037 |
| CC | −2.359 | 0.024 | |
| TC | −1.931 | 0.061 | |
| ) | NC | −2.988 | 0.005 |
| CC | −3.241 | 0.003 | |
| TC | −2.923 | 0.006 | |
| ) | NC | −4.423 | <0.001 |
| CC | −4.124 | <0.001 | |
| TC | −3.588 | <0.001 | |
| Kernel | Assessment | Top-3 Features | Top-5 Features | Top-10 Features | Average |
|---|---|---|---|---|---|
| Linear | Acc (%) | 86.49 | 90.54 | 89.19 | 88.74 |
| Sen (%) | 93.75 | 94.12 | 92.31 | 93.39 | |
| Spe (%) | 73.08 | 82.61 | 81.82 | 79.17 | |
| Err (%) | 13.51 | 9.46 | 10.81 | 11.26 | |
| Quadratic | Acc (%) | 90.54 | 89.19 | 91.89 | 90.54 |
| Sen (%) | 92.45 | 89.29 | 92.59 | 91.44 | |
| Spe (%) | 85.71 | 88.89 | 90.00 | 88.20 | |
| Err (%) | 9.46 | 10.81 | 8.11 | 9.46 | |
| Cubic | Acc (%) | 86.49 | 77.03 | 90.54 | 84.68 |
| Sen (%) | 90.38 | 85.71 | 92.45 | 89.52 | |
| Spe (%) | 77.27 | 60.00 | 85.71 | 74.33 | |
| Err (%) | 13.51 | 22.97 | 9.46 | 15.32 | |
| Fine Gaussian | Acc (%) | 87.84 | 87.84 | 77.03 | 84.23 |
| Sen (%) | 86.44 | 86.44 | 76.92 | 83.27 | |
| Spe (%) | 93.33 | 93.33 | 77.78 | 88.15 | |
| Err (%) | 12.16 | 12.16 | 22.97 | 15.77 | |
| Medium Gaussian | Acc (%) | 85.14 | 81.08 | 78.38 | 81.53 |
| Sen (%) | 83.61 | 79.69 | 77.27 | 80.19 | |
| Spe (%) | 92.31 | 90.00 | 87.50 | 89.94 | |
| Err (%) | 14.86 | 18.92 | 21.62 | 18.47 |
| Distance Technique | Assessment | k = 1 | k = 3 | k = 5 | Average |
|---|---|---|---|---|---|
| Euclidean | Acc (%) | 85.14 | 91.89 | 89.19 | 88.74 |
| Sen (%) | 88.68 | 92.59 | 87.93 | 89.73 | |
| Spe (%) | 76.19 | 90.00 | 93.75 | 86.65 | |
| Err (%) | 14.86 | 8.11 | 10.81 | 11.26 | |
| Chebyshev | Acc (%) | 85.14 | 86.49 | 86.49 | 86.04 |
| Sen (%) | 88.68 | 86.21 | 85.00 | 86.63 | |
| Spe (%) | 76.19 | 87.50 | 92.86 | 85.52 | |
| Err (%) | 14.86 | 13.51 | 13.51 | 13.96 | |
| Mahalanobis | Acc (%) | 82.43 | 87.84 | 87.84 | 86.04 |
| Sen (%) | 86.79 | 87.72 | 87.72 | 87.41 | |
| Spe (%) | 71.43 | 88.24 | 88.24 | 82.63 | |
| Err (%) | 17.57 | 12.16 | 12.16 | 13.96 |
| Classifier Method | Parameter/Kernel Type | Features | Accuracy (%) |
|---|---|---|---|
| k-NN | Euclidean + (k = 3) | Top-3 | 91.89 |
| SVM | Linear | Top-10 | 91.80 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ramlan, L.A.; Wan Zaki, W.M.D.; Mat Daud, M.; Mutalib, H.A. Non-Invasive Dry Eye Disease Detection Using Infrared Thermography Images: A Proof-of-Concept Study. Diagnostics 2025, 15, 2084. https://doi.org/10.3390/diagnostics15162084
Ramlan LA, Wan Zaki WMD, Mat Daud M, Mutalib HA. Non-Invasive Dry Eye Disease Detection Using Infrared Thermography Images: A Proof-of-Concept Study. Diagnostics. 2025; 15(16):2084. https://doi.org/10.3390/diagnostics15162084
Chicago/Turabian StyleRamlan, Laily Azyan, Wan Mimi Diyana Wan Zaki, Marizuana Mat Daud, and Haliza Abdul Mutalib. 2025. "Non-Invasive Dry Eye Disease Detection Using Infrared Thermography Images: A Proof-of-Concept Study" Diagnostics 15, no. 16: 2084. https://doi.org/10.3390/diagnostics15162084
APA StyleRamlan, L. A., Wan Zaki, W. M. D., Mat Daud, M., & Mutalib, H. A. (2025). Non-Invasive Dry Eye Disease Detection Using Infrared Thermography Images: A Proof-of-Concept Study. Diagnostics, 15(16), 2084. https://doi.org/10.3390/diagnostics15162084






