A Cone-Beam Computed Tomography Study of the Morphological and Morphometric Variations in the Mandibular Lingula and Its Clinical Implications
Abstract
1. Introduction
2. Materials and Methods
- Inclusion and exclusion criteria
- Malaysian subjects whose ethnicities were either Malay, Chinese or Indian;
- Age between 18 and 60 years old;
- Presence of first molars on both sides of the mandible.
- Subjects with poor quality CBCT with distortion of anatomical reference landmarks;
- Edentulous mandible;
- Presence of dentofacial deformities involving the mandible (i.e., syndromic patients);
- Presence of pathologic lesions such as cyst or tumour, mandibular fractures;
- Patients with a history or evidence of surgical intervention to the mandible.
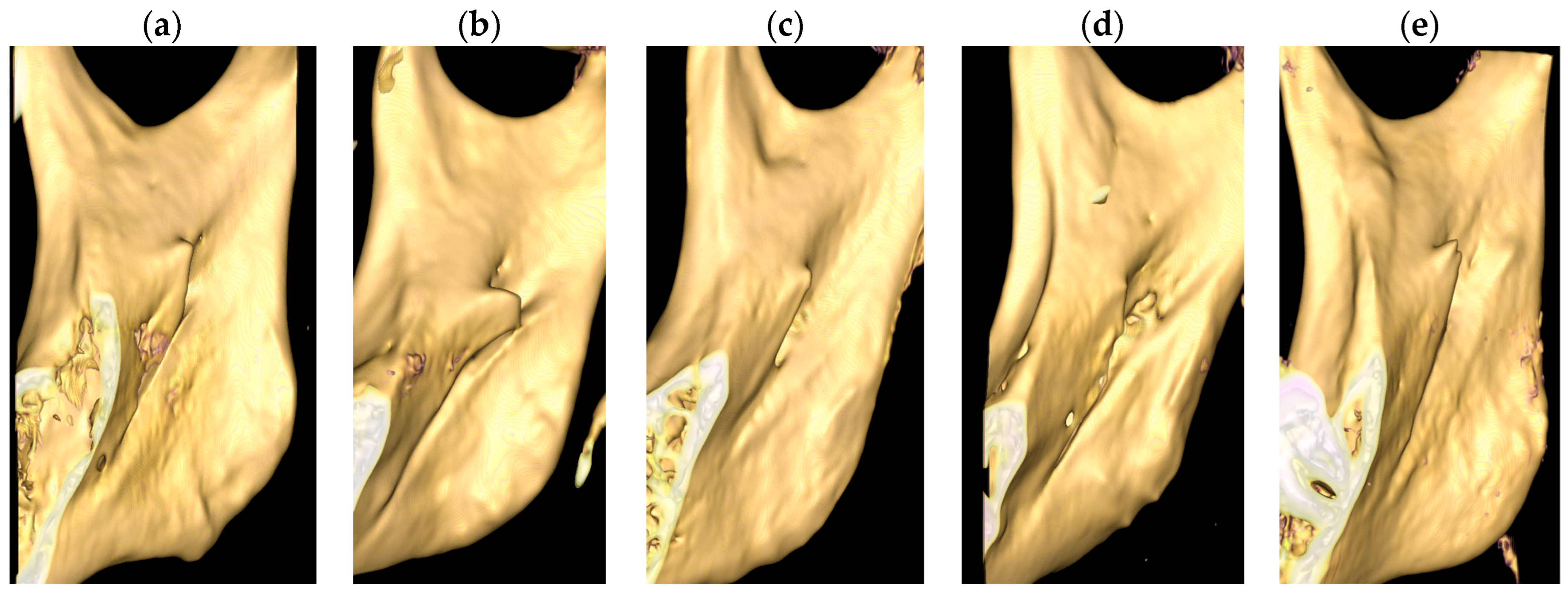
- Shape of lingula
- Triangular: Broad-based and pointed apex;
- Nodular: Rounded apex;
- Truncated: Flat projection with blunt upper margin;
- Assimilated: Completely incorporated into ramus of mandible;
- Others: M-shaped.
- Reference plane
- Reliability of measurement
- Statistical analysis
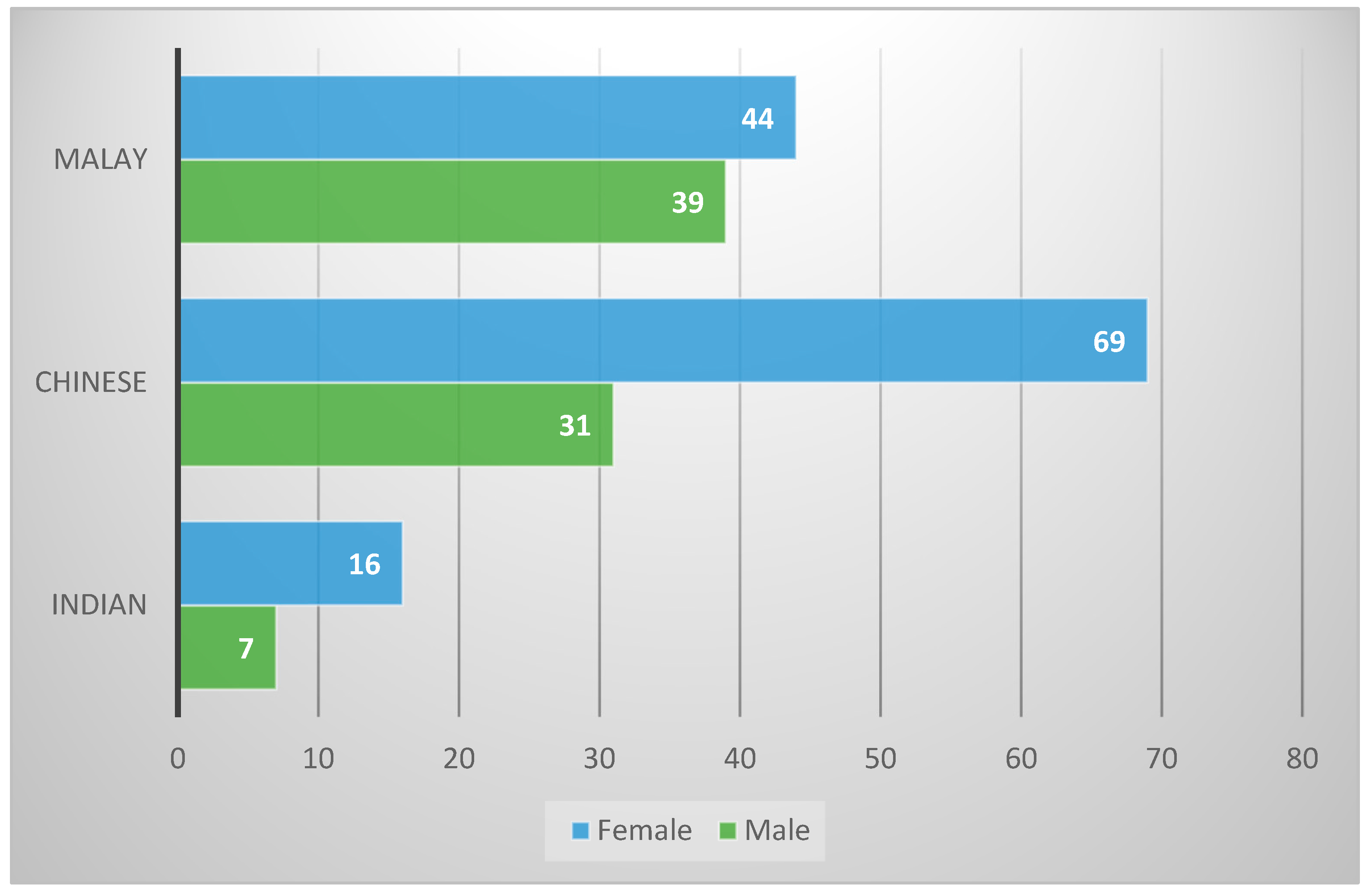
3. Results
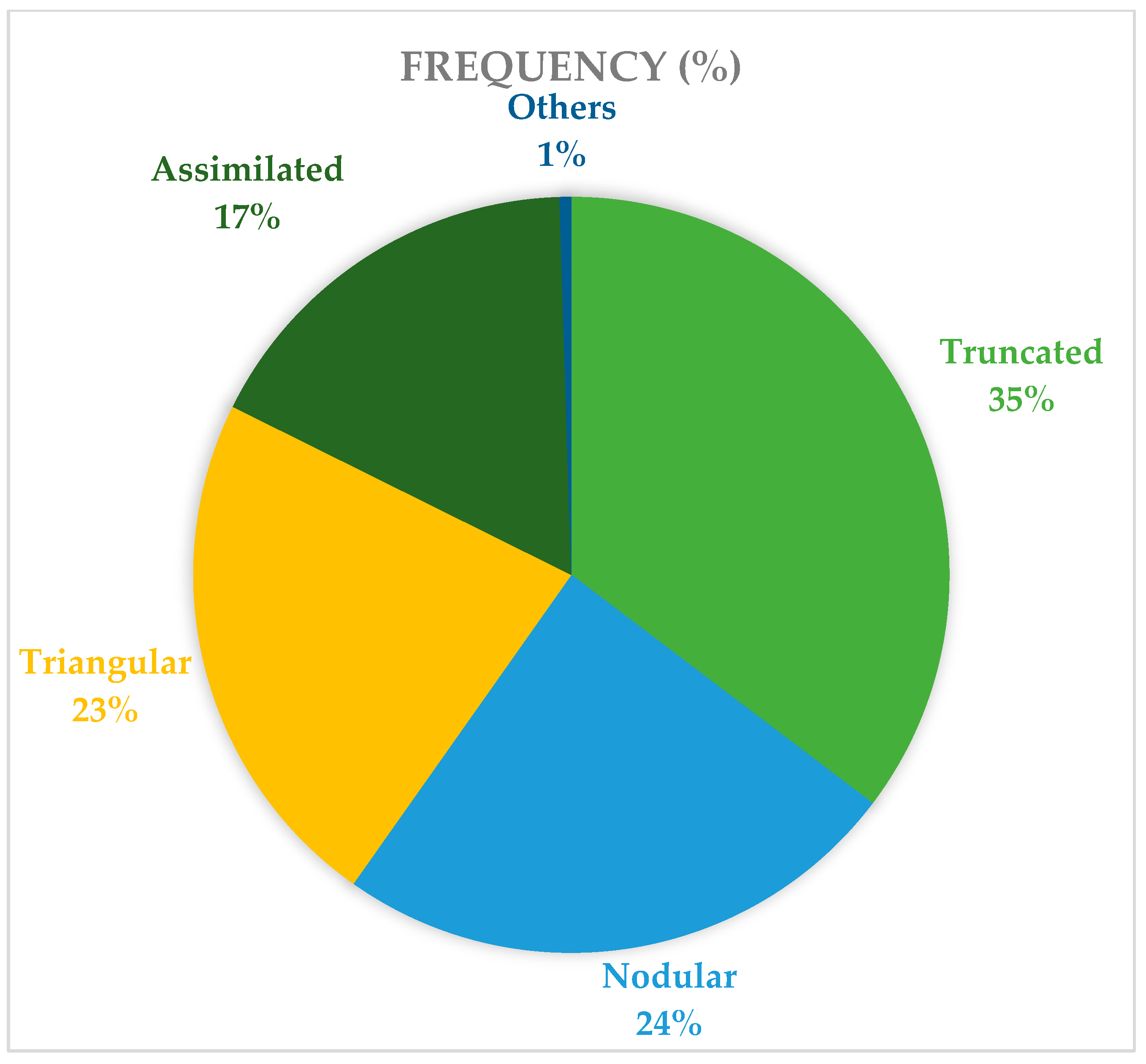
3.1. Shape of Lingula
3.2. Height of Lingula (HLI)
3.3. Distance of Lingula Tip to the Occlusal Plane (LiOP)
3.4. Distance of Lingula Tip to the Mandibular Second Molar (LiM2M)
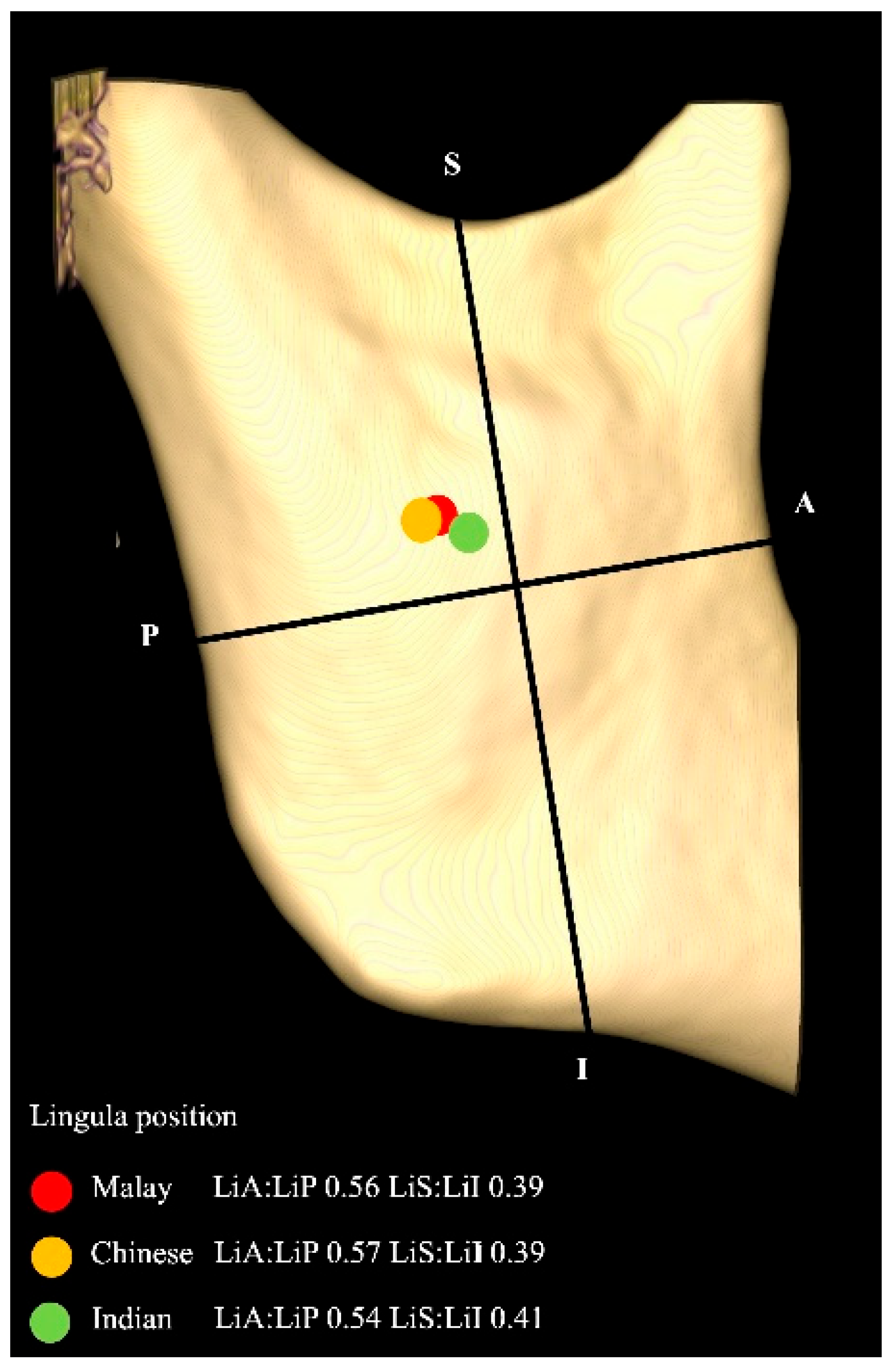
3.5. Distance of Lingula Tip to Anterior (LiA), Posterior (LiP), Superior (LiS), and Inferior (LiI) Borders of Ramus
4. Discussion
- Shape of Lingula
- HLi, LiOP, LiM2M
- LiA, LiP, LiS, LiI
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| CBCT | Cone-Beam Computed Tomograph |
| ML | Mandibular lingula |
| MF | Mandibular foramen |
| IAN | Inferior alveolar nerve |
References
- Jang, H.Y.; Han, S.J. Measurement of Mandibular Lingula Location Using Cone-Beam Computed Tomography and Internal Oblique Ridge-Guided Inferior Alveolar Nerve Block. J. Korean Assoc. Oral Maxillofac. Surg. 2019, 45, 158–166. [Google Scholar] [CrossRef] [PubMed]
- Hsu, K.J.; Lee, H.N.; Chen, C.M. Morphological Investigation of Mandibular Lingula: A Literature Review. J. Pers. Med. 2022, 12, 1015. [Google Scholar] [CrossRef]
- Monnazzi, M.S.; Passeri, L.A.; Gabrielli, M.F.R.; Bolini, P.D.A.; De Carvalho, W.R.S.; Da Costa Machado, H. Anatomic Study of the Mandibular Foramen, Lingula and Antilingula in Dry Mandibles, and Its Statistical Relationship between the True Lingula and the Antilingula. Int. J. Oral Maxillofac. Surg. 2012, 41, 74–78. [Google Scholar] [CrossRef] [PubMed]
- Nicholson, M.L. A Study of the Position of the Mandibular Foramen in the Adult Human Mandible. Anat. Rec. 1985, 212, 110–112. [Google Scholar] [CrossRef] [PubMed]
- Wong, M.K.; Jacobsen, P.L. Reasons for Local Anesthesia Failures. J. Am. Dent. Assoc. 1992, 123, 69–73. [Google Scholar] [CrossRef] [PubMed]
- Da Fontoura, R.A.; Vasconcellos, H.A.; Campos, A.E.S. Morphologic Basis for the Intraoral Vertical Ramus Osteotomy: Anatomic and Radiographic Localization of the Mandibular Foramen. J. Oral Maxillofac. Surg. 2002, 60, 660–665. [Google Scholar] [CrossRef]
- Lim, M.Y.; Lim, W.W.; Rajan, S.; Nambiar, P.; Ngeow, W.C. Age-Related Changes in the Location of the Mandibular and Mental Foramen in Children with Mongoloid Skeletal Pattern. Eur. Arch. Paediatr. Dent. 2015, 16, 397–407. [Google Scholar] [CrossRef]
- Srimani, P.; Goswami, B.; Mazumdar, S. Morphologic and Morphometric Analysis of Lingula in Localizing Mandibular Foramen and Its Surgical Importance (Cadaver India). Int. J. Anat. Radiol. Surg. 2017, 6, AO01–AO06. [Google Scholar]
- Madiraju, G.S.; Mohan, R. Morphological Analysis of the Mandibular Lingula and Its Relation to Antilingula Using Cone-Beam Computed Tomography in the Saudi Population. Diagnostics 2023, 13, 419. [Google Scholar] [CrossRef]
- Tengku Shaeran, T.A.; Shaari, R.; Abdul Rahman, S.; Alam, M.K.; Muhamad Husin, A. Morphometric Analysis of Prognathic and Non-Prognathic Mandibles in Relation to BSSO Sites Using CBCT. J. Oral Biol. Craniofac. Res. 2017, 7, 7–12. [Google Scholar] [CrossRef]
- Tuli, A.; Choudhry, R.; Choudhry, S.; Raheja, S.; Agarwal, S. Variation in Shape of the Lingula in the Adult Human Mandible. J. Anat. 2000, 197, 313–317. [Google Scholar] [CrossRef]
- Assis, F.P.; Sudhakar, A.S. Varying Shapes of Lingula and Its Prevalence in Dry Adult Human Mandible. Indian J. Clin. Anat. Physiol. 2019, 6, 224–228. [Google Scholar] [CrossRef]
- Varma, C.L.; Sameer, P.A. Morphological Variations of Lingula in South Indian Mandibles. Res. Rev. J. Med. Health Sci. 2013, 2, 31–34. [Google Scholar]
- Stipo, A.R.; Bertoglio, B.; Biehler-Gomez, L.; Cattaneo, C.; De Angelis, D. Morphological Analysis of Lingula Shape in a Modern Italian Cemeterial Population: Clinical and Forensic Considerations. Leg. Med. 2022, 55, 102027. [Google Scholar] [CrossRef]
- Ogut, E.; Yildirim, F.B. The Effects of Relationship Between the Mixed Typed of Lingula and Coronoid Process of the Mandible. Dokuz Eylül Üniversitesi Tıp Fakültesi Dergisi 2021, 35, 219–231. [Google Scholar] [CrossRef]
- Kositbowornchai, S.; Siritapetawee, M.; Damrongrungruang, T.; Khongkankong, W.; Chatrchaiwiwatana, S.; Khamanarong, K.; Chanthaooplee, T. Shape of the Lingula and Its Localization by Panoramic Radiograph versus Dry Mandibular Measurement. Surg. Radiol. Anat. 2007, 29, 689–694. [Google Scholar] [CrossRef]
- Jansisyanont, P.; Apinhasmit, W.; Chompoopong, S. Shape, Height, and Location of the Lingula for Sagittal Ramus Osteotomy in Thais. Clin. Anat. 2009, 22, 787–793. [Google Scholar] [CrossRef]
- Lopes, P.T.C.; Pereira, G.A.M.; Santos, A.M.P.V. Morphological analysis of the lingula in dry mandibles of individuals. South. Brazil J. Morphol. Sci. 2010, 27, 136–138. [Google Scholar]
- Samanta, P.; Kharb, P. Morphological Analysis of the Lingula in Dry Adult Human Mandibles of North Indian Population. J. Cranio-Maxillary Dis. 2012, 1, 7. [Google Scholar] [CrossRef]
- Nirmale, V.K.; Mane, U.W.; Sukre, S.B.; Diwan, C.V. Morphological features of human mandible. Int. J. Recent Trends Sci. Technol. 2012, 3, 38–43. [Google Scholar]
- Murlimanju, B.V.; Prabhu, L.V.; Pai, M.M.; Paul, M.T.; Saralaya, V.V.; Kumar, C.G. Morphological study of lingula of the mandibles in South Indian population. Morphol. Bull. De L’association Des Anat. 2012, 96, 16–20. [Google Scholar] [CrossRef]
- Smita, T. Variations in the Morphological appearance of lingula in dry adult human mandibles. Int. J. Cur. Res. Rev. 2013, 5, 41–45. [Google Scholar]
- Sekerci, A.E.; Cantekin, K.; Aydinbelge, M. Cone beam computed tomographic analysis of the shape, height, and location of the mandibular lingula in a population of children. Biomed Res Int. 2013, 2013, 825453. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Sekerci, A.E.; Sisman, Y. Cone-Beam Computed Tomography Analysis of the Shape, Height, and Location of the Mandibular Lingula. Surg. Radiol. Anat. 2014, 36, 155–162. [Google Scholar] [CrossRef]
- Padmavathi, G.; Varalakshmi, K.; Tiwari, S.; Roopashree, K. A Morphological and Morphometric Study of the Lingula in Dry Adult Human Mandibles of South Indian Origin and Its Clinical Significance. Int. J. Health Sci. Res. 2014, 4, 56–61. [Google Scholar]
- Sophia, M.M.; Anupriya, A.; Kalpana, R. A Morphometric and Morphological Study of Mandibular Lingula and Its Clinical Significance. Int. J. Med. Res. Rev. 2015, 3, 141–148. [Google Scholar] [CrossRef]
- Alves, N.; Deana, N.F. Morphological Study of the Lingula in Adult Human Mandibles of Brazilians Individuals and Clinical Implications. Biomed. Res. Int. 2015, 2015, 873751. [Google Scholar] [CrossRef]
- Senel, B.; Ozkan, A.; Altug, H.A. Morphological Evaluation of the Mandibular Lingula Using Cone-Beam Computed Tomography. Folia Morphol. 2015, 74, 497–502. [Google Scholar] [CrossRef]
- Lima, F.J.C.; Oliveira Neto, O.B.; Barbosa, F.T.; Sousa-Rodrigues, C.F. Location, Shape and Anatomic Relations of the Mandibular Foramen and the Mandibular Lingula: A Contribution to Surgical Procedures in the Ramus of the Mandible. Oral Maxillofac. Surg. 2016, 20, 177–182. [Google Scholar] [CrossRef]
- Jung, Y.H.; Cho, B.H.; Hwang, J.J. Location and Shape of the Mandibular Lingula: Comparison of Skeletal Class I and Class III Patients Using Panoramic Radiography and Cone-Beam Computed Tomography. Imaging Sci. Dent. 2018, 48, 185–190. [Google Scholar] [CrossRef]
- Modasiya, U.P.; Kanani, S.D. Study of the lingula in dry human mandibles and its clinical significance. Int. J. Anat. Res. 2018, 6, 5218–5221. [Google Scholar] [CrossRef]
- Asdullah, M.; Ansari, A.A.; Khan, M.H.; Salati, N.A.; Khawja, K.J.; Sachdev, A.S. Morphological variations of lingula and prevalence of accessory mandibular foramina in mandibles: A study. Natl. J. Maxillofac. Surg. 2018, 9, 129–133. [Google Scholar] [CrossRef]
- Akcay, H.; Kalabalık, F.; Tatar, B.; Ulu, M. Location of the mandibular lingula: Comparison of skeletal Class I and Class III patients in relation to ramus osteotomy using cone-beam computed tomography. J. Stomatol. Oral Maxillofac. Surg. 2019, 120, 504–508. [Google Scholar] [CrossRef] [PubMed]
- Soares, A.; Sampaio, C.; Sampaio, F.; Jesus, R.; Aguiar, M.; Junior, A.; Torres, T.; Neto, B.; Faria, M.; Bastos, L.; et al. Contribuição topográfica do forame e língula mandibular em procedimentos cirúrgicos no ramo da mandíbula. Rev. Bras. Odontol. 2019, 76, 1. [Google Scholar] [CrossRef]
- Özalp, Ö.; Salım, H.; Bilgin, B.; Öztürk, S.; Sarıkaya Doğan, M.; Göztepe, M.B.; Çalgüner, E.; Sindel, M.; Sindel, A. Morphologic and Morphometric Analysis of Mandibular Lingula. Anatomy 2020, 14, 16–221. [Google Scholar] [CrossRef]
- Elhassan, Y.H. Morphological Variations of the Mandibular Lingula: Clinical Implications for Surgical and Anesthetic Strategies in Adult Patients. Cureus 2025, 17, e79632. [Google Scholar] [CrossRef]
- Findik, Y.; Yildirim, D.; Baykul, T. Three-Dimensional Anatomic Analysis of the Lingula and Mandibular Foramen: A Cone Beam Computed Tomography Study. J. Craniofac. Surg. 2014, 25, 607–610. [Google Scholar] [CrossRef]
- Hsu, K.J.; Tseng, Y.C.; Liang, S.W.; Hsiao, S.Y.; Chen, C.M. Dimension and Location of the Mandibular Lingula: Comparisons of Gender and Skeletal Patterns Using Cone-Beam Computed Tomography. Biomed. Res. Int. 2020, 2020, 2571534. [Google Scholar] [CrossRef] [PubMed]
- Zhou, C.; Jeon, T.H.; Jun, S.H.; Kwon, J.J. Evaluation of Mandibular Lingula and Foramen Location Using 3-Dimensional Mandible Models Reconstructed by Cone-Beam Computed Tomography. Maxillofac. Plast. Reconstr. Surg. 2017, 39, 30. [Google Scholar] [CrossRef]
- Lupi, S.M.; Landini, J.; Olivieri, G.; Todaro, C.; Scribante, A.; Baena, R.R.Y. Correlation between the Mandibular Lingula Position and Some Anatomical Landmarks in Cone Beam Ct. Healthcare 2021, 9, 1747. [Google Scholar] [CrossRef]
- Sarna, K.; Sonigra, K.; Ngeow, W.C.; Guthua, S.; Opondo, F.; Tay, H.W. Variations of the Lingula and Mandibular Ramus in the Context of Sagittal Split Ramus Osteotomy: A Cone Beam Computed Tomography Study Supporting an Ethnic-Centric Approach to Orthognathic Surgery. Cureus 2024, 16, e67715. [Google Scholar] [CrossRef] [PubMed]
- Kim, H.J.; Lee, H.Y.; Chung, I.H.; Cha, I.H.; Yi, C.K. Mandibular Anatomy Related to Sagittal Split Ramus Osteotomy in Koreans. Yonsei Med. J. 1997, 38, 19–25. [Google Scholar] [CrossRef]
- Glądys, K.; Ostrowski, P.; Bonczar, M.; Kwiecińska, M.; Gliwa, J.; Nasser, A.; Możdżeń, K.; Trzeciak, M.; Gregorczyk-Maga, I.; Musiał, A.; et al. The Complete Anatomy of the Mandibular Lingula: A Meta-Analysis with Clinical Implications. Folia Morphol. 2023, 83, 531–540. [Google Scholar] [CrossRef]
- Hsu, K.J.; Chen, P.J.; Chen, H.S.; Lee, K.T.; Chen, C.M. Evaluation of Positions of Four Lingula Shapes for Mandibular Ramus Surgery. Front. Oral Health 2024, 5, 1521227. [Google Scholar] [CrossRef] [PubMed]
- Hunsuck, E.E. A Modified Intraoral Sagittal Splitting Technic for Correction of Mandibular Prognathism. J. Oral Surg. 1968, 26, 249–252. [Google Scholar]
- Choi, D.Y.; Hur, M.S. Anatomical Review of the Mandibular Lingula for Inferior Alveolar Nerve Block. Folia Morphol. 2021, 80, 786–791. [Google Scholar] [CrossRef] [PubMed]
- Zhao, K.; Zhang, B.; Hou, Y.; Miao, L.; Wang, R.; Yuan, H. Imaging Study on Relationship between the Location of Lingula and the Gonial Angle in a Chinese Population. Surg. Radiol. Anat. 2019, 41, 455–460. [Google Scholar] [CrossRef]
- Hayagreev, D.; Kodialbail, A.; Shetty, S.; Sujatha, S. Morphometric Variations of Mandibular Foramen and Lingula of Mandible with Gender and Age Using Cone Beam Computerised Tomography. Int. J. Curr. Res. Rev. 2021, 13, 29–35. [Google Scholar] [CrossRef]
- Rikhotso, R.; Munsamy, C. A Morphological Study of the Lingula in South Africans in Relation to Sagittal Split Osteotomy. S. Afr. Dent. J. 2017, 72, 408–412. [Google Scholar] [CrossRef]
- Dal Pont, G. Retromolar Osteotomy for the Correction of Prognathism. J. Oral Surg. Anesth. Hosp. Dent. Serv. 1961, 19, 42. [Google Scholar]
- Westermark, A.; Bystedt, H.; Von Konow, L. Inferior Alveolar Nerve Function after Sagittal Split Osteotomy of the Mandible: Correlation with Degree of Intraoperative Nerve Encounter and Other Variables in 496 Operations. Br. J. Oral Maxillofac. Surg. 1998, 36, 429–433. [Google Scholar] [CrossRef] [PubMed]
- Erzurumlu, U.Z.; Torul, Z.D. Three-Dimensional Evaluation of the Mandibular Lingula on Cone-Beam Computed Tomographic Images in The Turkish Population. J. Dent. Indones. 2022, 29, 179–186. [Google Scholar]

| Study | Population | Type of Study 1 | Method | No of Samples (Sides) | Gender 2 | Age 3 | Shape (n, %) | Most Prevalent | ||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Triangular | Truncated | Nodular | Assimilated | Others | ||||||||
| Tuli et al. (2000) [11] | Indian | DM | Direct visualization | 165 | 131 M; 34 F | NA | 226 (68.5%) | 52 (15.8%) | 36 (10.9%) | 16 (4.8%) | Triangular | |
| Kositbowornchai et al. (2007) [16] | Thai | DM | Digital calliper | 72 (144) | 52 M; 20 F | 27–87 | 24 (16.7%) | 68 (47.2%) | 33 (22.9%) | 19 (13.2%) | Truncated | |
| Jansisyanont et al. (2009) [17] | Thai | DM | Sliding callipers | 92 (184) | 58 M; 34 F | 18–83 | 55 (29.9%) | 85 (46.2%) | 36 (19.6%) | 8 (4.3%) | Truncated | |
| Lopes et al. (2010) [18] | South Brazilian | DM | Direct visualization | 80 | NA | NA | 66 (41.3%) | 58 (36.3%) | 17 (10.5%) | 19 (11.9%) | Triangular | |
| Samantha and Kharb (2012) [19] | North Indian | DM | Sliding calliper | 60 (120) | NA | NA | 54 (45.0%) | 36 (30.0%) | 23 (19.2%) | 7 (5.8%) | Triangular | |
| Nirmale et al. (2012) [20] | North Indian | DM | NA | 84 (168) | 62 M; 22 F | NA | 80 (47.6%) | 18 (10.7%) | 47 (28.0%) | 23 (13.7%) | Triangular | |
| Murlimanju et al. (2012) [21] | South Indian | DM | Direct visualization | 67 (134) | 37 M; 30 F | NA | 40 (29.9%) | 37 (27.6%) | 40 (29.9%) | 17 (12.6%) | Triangular and nodular | |
| Varma and Sameer (2013) [13] | South Indian | DM | NA | 193 (386) | NA | NA | 63 (16.3%) | 99 (25.7%) | 182 (47.2%) | 26 (6.7%) | 16 (4.1%) M-shaped | Nodular |
| Smita (2013) [22] | Indian | DM | NA | 50 (100) | NA | NA | 42 (42.0%) | 36 (36.0%) | 10 (10.0%) | 12 (12.0%) | Triangular | |
| Sekerci et al. (2013) [23] | Turkish Pediatric | CBCT | NNT software | 125 B; 144 G | 6–12 | 74 (13.8%) | 126 (23.4%) | 260 (48.3%) | 78 (14.5%) | Nodular | ||
| Sekerci and Sisman (2014) [24] | Turkish | CBCT | NA | 412 | 312 M; 199 F | NA | 116 (14.1%) | 264 (32.0%) | 422 (51.2%) | 22 (2.7%) | Nodular | |
| Padmavathi et al. (2014) [25] | South Indian | DM | Vernier calliper | 65 (130) | NA | NA | 38 (29.2%) | 44 (33.8%) | 25 (19.2%) | 23 (17.7%) | Truncated | |
| Sophia et al. (2015) [26] | South Indian | DM | NA | 50 (100) | UNK | UNK | 49 (49.0%) | 23 (23.0%) | 18 (18.0%) | 10 (10.0%) | Triangular | |
| Alves and Deana (2015) [27] | Brazilian | DM | NA | 132 (253) | 165 M; 88 F | NA | 59 (23.3%) | 124 (49.0%) | 67 (26.5%) | 3 (1.2%) | Truncated | |
| Senel et al. (2015) [28] | Turkish | CBCT | iCat vision | 126 | 35 M; 28 F | 25–70 (46) | 28 (22.2%) | 24 (19%) | 41 (32.5%) | 33 (26.2%) | Nodular | |
| Lima at el. (2016) [29] | Brazilian | DM | Calliper | 30 (60) | UNK | UNK | 11 (18.3%) | 29 (48.3%) | - | 2 (3.3%) | Rectangular 18 (30.0%) | Trapezoidal |
| Jung et al. (2018) [30] | Korea | CBCT | PaX-Zenith 3D system (VATECH Co.) | 347 (694) | 181 M; 166 F | 19–50 | 99 (14.3%) | 203 (29.3%) | 375 (54.0%) | 17 (2.4%) | Nodular | |
| Modasiya and Kanani (2018) [31] | North Indian | DM | Direct visualization | 90 (180) | NA | NA | 76 (42.2%) | 28 (15.5%) | 39 (21.7%) | 37 (20.6%) | Truncated | |
| Asdullah et al. (2018) [32] | Indian | DM | NA | 50 (100) | 25 M; 25 F | NA | 42 (42.0%) | 32 (32.0%) | 20 (20.0%) | 6 (6.0%) | Triangular | |
| Assis et al. (2019) [12] | South Indian | DM | Direct visualization | 50 (100) | NA | NA | 47 (47%) | 18 (18%) | 26 (26%) | 7 (7%) | M-shaped 2 (2%) | Triangular |
| Akcay et al. (2019) [33] | Turkish | CBCT | Mimics software | 60 (120) | 30 M; 30 F | NA | 24 (20.0%) | 26 (21.7%) | 54 (45.0%) | 16 (13.3%) | Nodular | |
| Soares et al. (2019) [34] | Brazilian | DM | Digital calliper | 77 | NA | NA | 35 (45.4%) | 33 (42.9%) | - | 9 (11.7%) | Triangular | |
| Ozalp et al. (2020) [35] | Turkish (Anatolian) | DM | Digital calliper | 50 | UNK | UNK | 42 (42.0%) | 28 (28.0%) | 30 (30.0%) | nil | Triangular | |
| Stipo et al. (2022) [14] | Italian | DM | Direct visualization | 235 (453) | 121 M; 14 F | 20-101 | 49 (10.8%) | 175 (38.6%) | 119 (26.3%) | 18 (4.0%) | Bridge 23 (5.1%) Mixed 69 (15.2%) | Truncated |
| Elhassan (2025) [36] | Saudi | DM | Digital calliper | 100 (200) | 80 M; 20 F | NA | 118 (59.0%) | 44 (22.0%) | 26 (13.0%) | 12 (6.0%) | Triangular | |
| Code | Definition |
|---|---|
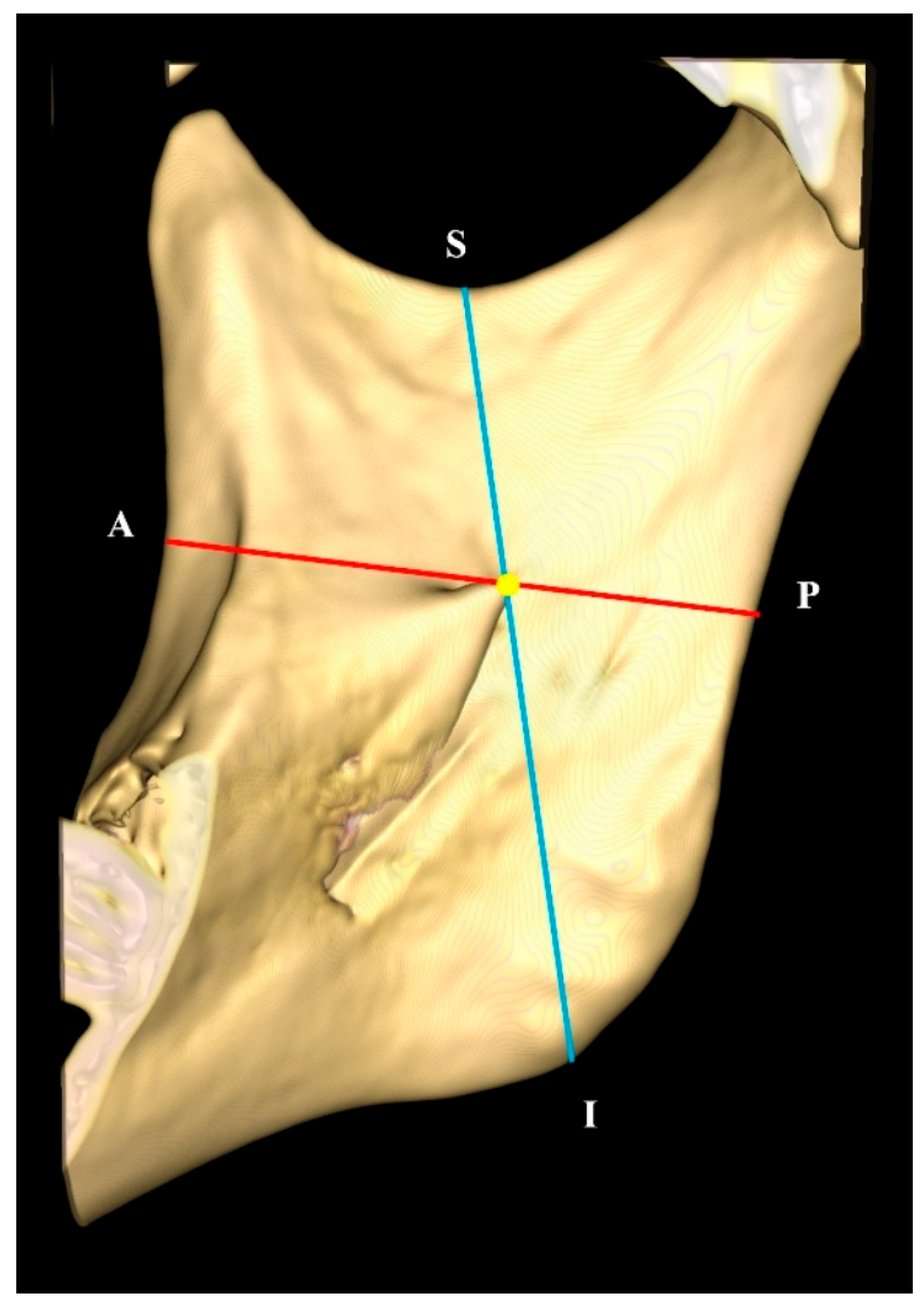
| OP | Formed by connecting the midpoint of both mandibular central incisors at the incisal edge and the mesiobuccal cusp of the mandibular first molars (Figure 2) |
| HLi | Distance of the lingula tip (Li) to the mandibular foramen opening, measured in a vertical line perpendicular to the OP, extending from the tip of the lingula to the lower border (most inferior part of the mandibular foramen opening for assimilated type) |
| LiOP | Distance of the lingula tip (Li) to the occlusal plane (OP), measured in a vertical line perpendicular to the OP |
| LiM2M | Distance of the lingula tip (Li) to the mandibular second molar (M2M) cementoenamel junction (CEJ) disto-lingual aspect |
| Code | Definition | Description |
|---|---|---|
| LiA | Distance of the lingula tip (Li) to the deepest point on the coronoid notch at the anterior border of ramus (A) | Shortest linear distance measured from the anatomical landmarks (irrespective of horizontal or vertical plane) |
| LiP | Distance of the lingula tip (Li) to the posterior border of ramus (P) | AP − LiA = LiP |
| LiS | Distance of the lingula tip (Li) to the deepest point of the sigmoid notch at the superior border of the ramus (S) | Shortest linear distance measured from the anatomical landmarks (irrespective of horizontal or vertical plane) |
| LiI | Distance of the lingula tip (Li) to the inferior border of the ramus | SI − LiS = LiI |
| AP | Distance from the anterior to posterior border of the ramus; also the antero-posterior diameter of the ramus | Straight line (red line) connecting a point on the deepest concavity of the anterior border of the ramus, passing through the tip of the lingula and extending to the posterior border of the ramus |
| SI | Distance from the superior to the inferior border of the ramus | Straight line (blue line) connecting a point on the deepest concavity of the sigmoid notch, passing through the tip of the lingula and extending to the inferior border of the ramus |
| LiA:LiP | Position of the lingula antero-posteriorly in the ramus of the mandible | Ratio of LiA over LiP for localization of the lingula |
| LiS:LiI | Position of the lingula supero-inferiorly in the ramus of the mandible | Ratio of LiS over LiI for localization of the lingula |
| Male | Female | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Total | Bilateral | Unilateral | Bilateral | Unilateral | Bilateral | Unilateral | ||||||||
| No. | % | No. | % | No. | % | No. | % | No. | % | No. | % | No. | % | |
| Triangular | 93 | 22.6% | 54 | 25.5% | 39 | 19.4% | 22 | 27.2% | 12 | 16.7% | 32 | 24.6% | 27 | 21.1% |
| Truncated | 146 | 35.4% | 65 | 30.7% | 81 | 40.3% | 25 | 30.9% | 38 | 52.8% | 40 | 30.8% | 43 | 33.6% |
| Nodular | 101 | 24.5% | 61 | 28.8% | 40 | 19.9% | 21 | 25.9% | 8 | 11.1% | 40 | 30.8% | 32 | 25.0% |
| Assimilated | 71 | 17.2% | 31 | 14.6% | 40 | 19.9% | 13 | 16.0% | 14 | 19.4% | 18 | 13.8% | 26 | 20.3% |
| Others | 1 | 0.2% | 0 | 0.0% | 1 | 0.5% | 0 | 0.0% | 1 | 1.4% | 0 | 0.0% | 0 | 0.0% |
| Total | 412 | 211 | 51.2% | 201 | 48.8% | 81 | 38.4% | 73 | 36.3% | 130 | 61.6% | 128 | 63.7% | |
| Height of Lingula in mm (SD), with 95% CI | ||||||
|---|---|---|---|---|---|---|
| Ethnic | Malay (n = 158) | Chinese (n = 192) | Indian (n = 43) | Overall (n = 393) | p-Value | |
| Sides | Left (n = 169) | 5.29 (1.28) | 5.35 (1.40) | 5.32 (1.46) | 5.33 (1.35) | 0.727 |
| 5.00–5.59 | 5.06–5.66 | 4.60–6.07 | 5.13–5.54 | |||
| Right (n = 172) | 5.24 (1.40) | 5.22 (1.36) | 4.58 (1.12) | 5.17 (1.36) | ||
| 4.91–5.59 | 4.94–5.52 | 4.05–5.15 | 4.97–5.41 | |||
| Gender | Male (n = 127) | 5.14 (1.48) | 5.37 (1.50) | 4.73 (1.39) | 5.23 (1.48) | 0.061 |
| 4.77–5.57 | 5.02–5.76 | 3.79–5.75 | 4.97–5.49 | |||
| Female (n = 214) | 5.36 (1.20) | 5.25 (1.32) | 5.03 (1.33) | 5.26 (1.28) | ||
| 5.08–5.63 | 5.01–5.49 | 4.45–5.62 | 5.09–5.43 | |||
| Total | 5.26 (1.33) | 5.29 (1.38) | 4.95 (1.33) | 5.25 (1.36) | ||
| 4.97–5.52 | 5.09–5.44 | 5.11–5.40 | 5.11–5.40 | |||
| Distance of Lingula to the Occlusal Plane in mm (SD), with 95% CI | ||||||
|---|---|---|---|---|---|---|
| Ethnic | Malay (n = 158) | Chinese (n = 192) | Indian (n = 43) | Overall (n = 393) | p-Value | |
| Sides | Left (n = 201) | 9.04 (3.45) | 8.85 (3.07) | 7.59 (2.37) | 8.79 (3.18) | 0.063 |
| 8.26–9.82 | 8.24–9.46 | 6.51–8.63 | 8.34–9.23 | |||
| Right (n = 198) | 8.38 (3.34) | 8.55 (3.69) | 7.02 (2.87) | 8.31 (3.49) | ||
| 7.68–9.17 | 7.83–9.36 | 5.78–8.24 | 7.83–8.83 | |||
| Gender | Male (n = 76) | 9.24 (3.46) | 9.53 (3.49) | 6.66 (1.77) | 9.13 (3.43) | 0.479 |
| 8.47–10.02 | 9.66–10.40 | 5.66–7.60 | 8.62–9.68 | |||
| Female (n = 124) | 8.21 (3.29) | 8.32 (3.29) | 7.58 (2.90) | 8.19 (3.24) | ||
| 7.53–9.03 | 7.72–8.90 | 6.54–8.74 | 7.79–8.61 | |||
| Total | 8.71 (3.40) | 8.70 (3.39) | 7.30 (2.62) | 8.55 (3.34) | ||
| 8.17–9.29 | 8.21–9.21 | 6.53–8.18 | 8.24–8.88 | |||
| Distance of Lingula to the Mandibular Second Molar in mm (SD), with 95% CI | ||||||
|---|---|---|---|---|---|---|
| Ethnic | Malay (n = 158) | Chinese (n = 192) | Indian (n = 43) | Overall (n = 393) | p-Value | |
| Sides | Left (n = 185) | 31.78 (3.22) | 31.55 (3.78) | 29.89 (2.47) | 31.45 (3.47) | 0.305 |
| 31.02–32.48 | 30.72–32.39 | 28.91–30.91 | 30.93–31.96 | |||
| Right (n = 181) | 31.92 (3.27) | 31.50 (3.81) | 29.85 (3.55) | 31.49 (3.59) | ||
| 31.21–32.65 | 30.71–32.37 | 28.38–31.24 | 30.97–32.03 | |||
| Gender | Male (n = 134) | 33.12 (3.20) | 32.96 (2.96) | 30.13 (3.26) | 32.75 (3.22) | 0.420 |
| 32.37–33.86 | 32.10–33.71 | 28.36–31.83 | 32.17–33.33 | |||
| Female (n = 232) | 30.77 (2.86) | 30.93 (3.94) | 29.74 (2.97) | 30.73 (3.49) | ||
| 30.19–31.44 | 30.24–31.59 | 28.64–30.88 | 30.29–31.18 | |||
| Total | 31.85 (3.24) | 31.53 (3.78) | 29.87 (3.03) | 31.47 (3.53) | ||
| 31.30–32.40 | 30.96–32.07 | 28.96–30.90 | 31.11–31.83 | |||
| Mean Distance of Lingula to the Anterior, Posterior, Superior, and Inferior Ramus Border in mm (SD), with 95% CI | |||||||
|---|---|---|---|---|---|---|---|
| Ethnic | Malay (M) | Chinese (C) | Indian (I) | p-Value | |||
| M vs. C | C vs. I | M vs. I | |||||
| LiA | Male | 17.65 (2.44) | 18.42 (2.44) | 15.83 (1.25) | |||
| 17.16–18.13 | 17.88–18.96 | 14.69–16.97 | |||||
| Female | 17.77 (1.68) | 18.28 (2.28) | 16.43 (1.96) | ||||
| 17.32–18.23 | 17.91–18.64 | 15.48–17.19 | |||||
| Total | 17.71 (2.07) | 18.32 (2.32) | 16.25 (1.78) | 0.022 * | <0.001 * | <0.001 * | |
| 17.40–18.03 | 18.00–18.64 | 15.72–16.87 | |||||
| LiP | Male | 15.22 (4.28) | 15.50 (3.40) | 16.03 (4.17) | |||
| 14.47–15.97 | 14.66–16.34 | 14.25–17.80 | |||||
| Female | 13.98 (2.53) | 14.01 (3.37) | 13.19 (2.30) | ||||
| 13.27–14.68 | 13.44–14.57 | 12.02–14.37 | |||||
| Total | 14.56 (3.51) | 14.47 (3.44) | 14.05 (3.22) | 0.964 | 0.733 | 0.64 | |
| 14.02–15.10 | 13.99–14.95 | 13.10–15.01 | |||||
| LiS | Male | 18.45 (3.01) | 17.60 (2.64) | 20.66 (4.95) | |||
| 17.80–19.11 | 16.87–18.34 | 19.12–22.10 | |||||
| Female | 17.86 (3.23) | 17.15 (2.51) | 17.08 (2.96) | ||||
| 17.25–18.47 | 16.66–17.64 | 16.06–18.10 | |||||
| Total | 18.14 (3.13) | 17.29 (2.55) | 18.17 (3.98) | 0.017 * | 0.161 | 0.988 | |
| 17.66–18.62 | 16.94–17.65 | 16.99–19.35 | |||||
| LiI | Male | 29.21 (4.63) | 29.42 (4.49) | 26.72 (4.66) | |||
| 28.30–30.12 | 28.40–30.44 | 24.57–28.87 | |||||
| Female | 26.53 (3.21) | 25.57 (4.15) | 25.07 (3.47) | ||||
| 25.67–27.39 | 24.89–26.26 | 23.65–26.49 | |||||
| Total | 27.79 (4.15) | 26.77 (4.61) | 25.57 (3.89) | 0.047 * | 0.175 | 0.004 * | |
| 27.15–28.42 | 26.13–27.41 | 24.42–26.73 | |||||
| Study | Population | Study Type—Instrument | Ref. Plane | Samples, n (Sides) | Gender | Age (Mean) | Lingula Measurements | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| LiA | LiP | LiS | LiI | LiM2M | LiOP | Hli | ||||||||
| Sophia et al. (2015) [26] | Indian | DM—NA | Mandibular base | 50 (100) | UNK | UNK | 17.11 ± 2.32 | 14.86 ± 2.54 | 18.71 ± 3.18 | 30.30 ± 5.11 | NA | NA | 7.45 ± 1.48 | |
| Senel et al. (2015) [28] | Turkish | CBCT—iCat | NA | 63 (126) | 35 M 28 F | 25–70 (46) | 18.5 ± 2.3 | 16.9 ± 3.5 | 18.1 ± 3.6 | 38.3 ± 5.3 | NA | NA | 7.8 ± 2.4 | |
| Lima at el. (2016) [29] | Brazilian | DM—calliper | NA | 30 | UNK | UNK | R | 18.68 ± 3.75 | 15.78 ± 2.08 | 16.64 ± 1.98 | 33.53 ± 5.23 | NA | NA | 7.88 ± 2.15 |
| L | 19.96 ± 3.58 | 15.81 ± 2.55 | 16.31 ± 2.58 | 33.87 ± 4.67 | NA | NA | 7.77 ± 2.01 | |||||||
| Alves and Deana (2015) [27] | Brazilian (Amerindian and Caucasian) | DM—digital calliper | NA | 132 (253) | 165 M 88 F | NA | 17.76 ± 2.69 | 15.28 ± 2.31 | 17.29 ± 2.57 | NA | 33.30 ± 4.14 | NA | 8.29 ± 1.99 | |
| Zhou et al. (2017) [39] | Korean | CBCT—OnDemand3 D® | Occlusal plane | 106 (121) | 51 M 55 F | 18–36 (26.8) | 18.2 ± 2.4 | 18.2 ± 1.7 | 15.7 ± 2.7 | 35.3 ± 3.3 | 31.0 ± 3.3 | 6.0 ± 2.9 | 10.1 ± 2.3 | |
| 18.3 ± 2.2 | 17.0 ± 1.8 | 15.5 ± 2.3 | 30.5 ± 2.8 | 28.1 ± 2.9 | 9.8 ± 2.1 | |||||||||
| Tengku Shaeran et al. (2017) [10] | Malaysian | CBCT—NA | NA | 51 | 21 M 30 F | 18–35 | C I | 15.00 ± 2.61 | NA | NA | NA | NA | NA | NA |
| C III | 12.48 ± 2.16 | NA | NA | NA | NA | NA | NA | |||||||
| Modasiya and Kanani (2018) [31] | North Indian | DM—vernier calliper | NA | 90 (180) | NA | NA | 16.62 ± 3.31 | 15.94 ± 1.63 | 16.05 ± 2.85 | 34.16 ± 2.96 | NA | 7.75 ± 1.81 | NA | |
| Akcay et al. (2019) [33] | Turkish | CBCT—mimics | Occlusal plane | 60 (120) | 16 M 14 F | 11.63 ± 1.67 | 16.18 ± 1.76 | 18.22 ± 2.81 | NA | NA | 9.01± 3.18 | NA | ||
| Zhao et al. (2019) [47] | Chinese | CBCT—NNT | Occlusal plane | 407 (814) | 201M 206 F | 20–35 | M | 16.53 | 16.9 | 16.67 | 34.74 | NA | 5.97 | NA |
| F | 16.77 | 16.42 | 16.22 | 32.37 | NA | 5.03 | NA | |||||||
| Jang et al. (2019) [1] | Korean | CBCT—Ez3D-I | Occlusal plane | 125 | 63 M 62 F | 15–56 | M | 14.99 ± 1.27 | NA | NA | NA | NA | 10.30 ± 2.33 | NA |
| F | 14.37 ± 1.55 | NA | NA | NA | NA | 7.37 ± 1.94 | NA | |||||||
| Ozalp et al. (2020) [35] | Turkish (Anatolian) | DM—digital calliper | NA | 50 | UNK | UNK | 16.86 ± 2.73 | 14.7 ± 1.6 | NA | NA | NA | NA | 11.92 ± 2.03 | |
| Hsu et al. (2020) [38] | Taiwanese | CBCT—NA | Frankfort horizontal plane | 72 (144) | 23 M 49 F | NA | 19.21 ± 3.02 | 15.22 ± 2.02 | 20.04 ± 3.16 | 31.20 ± 3.81 | NA | NA | 8.07 ± 2.39 | |
| Hayagreev et al. (2021) [48] | Indian | CBCT—Carestream; dicom software | NA | 100 | NA | <20; >20 | 16.1 ± 2.2 | 14.8 ± 2.1 | 16.3 ± 2.9 | 32.2 ± 4.0 | NA | NA | NA | |
| Lupi et al. (2021) [40] | Italian | CBCT—SimPlant Pro 18® | Occlusal plane | 111 (201) | 56 M 43 F | 18–88 (34.9) | 16.96 ± 2.40 | 15.28 ± 2.10 | 13.87 ± 3.69 | 31.20 ± 4.35 | 29.22 ± 3.98 | 11.22 ± 4.27 | NA | |
| Erzurumlu and Torul (2022) [52] | Turkish | CBCT—NA | Occlusal plane | 50 (100) | 19 M; 31 F | 18–56 (31.2) | 17.09 ± 2.11 | 15.46 ± 1.62 | 17.10 ± 2.57 | NA | NA | 9.55 ± 2.92 | NA | |
| Madiraju and Mohan (2023) [9] | Saudi | CBCT—i-CAT Vision software | NA | 125 (250) | 68 M; 57 F | 16–36 (24.2) | NA | NA | NA | NA | NA | NA | 7.73 ± 0.44 | |
| Hsu et al. (2024) [44] | Taiwanese | CBCT—RadiAnt | Frankfort horizontal plane | 90 (180) | 30 M; 60 F | NA | 18.88 ± 2.66 | 15.23 ± 2.02 | 19.59 ± 3.19 | 31.34 ± 3.92 | NA | NA | NA | |
| Present study | Malaysian | CBCT—Slicer | Occlusal plane | 206 (412) | 129 M; 77 F | 18–60 (33.3) | 17.84 ± 2.25 | 14.46 ± 3.44 | 17.73 ± 3.00 | 27.05 ± 4.40 | 31.47 ± 3.53 | 8.55 ± 3.34 | 5.25 ± 1.36 | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tay, H.W.; Ngeow, W.C. A Cone-Beam Computed Tomography Study of the Morphological and Morphometric Variations in the Mandibular Lingula and Its Clinical Implications. Diagnostics 2025, 15, 2071. https://doi.org/10.3390/diagnostics15162071
Tay HW, Ngeow WC. A Cone-Beam Computed Tomography Study of the Morphological and Morphometric Variations in the Mandibular Lingula and Its Clinical Implications. Diagnostics. 2025; 15(16):2071. https://doi.org/10.3390/diagnostics15162071
Chicago/Turabian StyleTay, Hui Wen, and Wei Cheong Ngeow. 2025. "A Cone-Beam Computed Tomography Study of the Morphological and Morphometric Variations in the Mandibular Lingula and Its Clinical Implications" Diagnostics 15, no. 16: 2071. https://doi.org/10.3390/diagnostics15162071
APA StyleTay, H. W., & Ngeow, W. C. (2025). A Cone-Beam Computed Tomography Study of the Morphological and Morphometric Variations in the Mandibular Lingula and Its Clinical Implications. Diagnostics, 15(16), 2071. https://doi.org/10.3390/diagnostics15162071






