Predictive Power of Baseline [18F]FDG PET/CT for Adverse Events in DLBCL Patients Undergoing CAR-T Cell Therapy
Abstract
1. Introduction
2. Materials and Methods
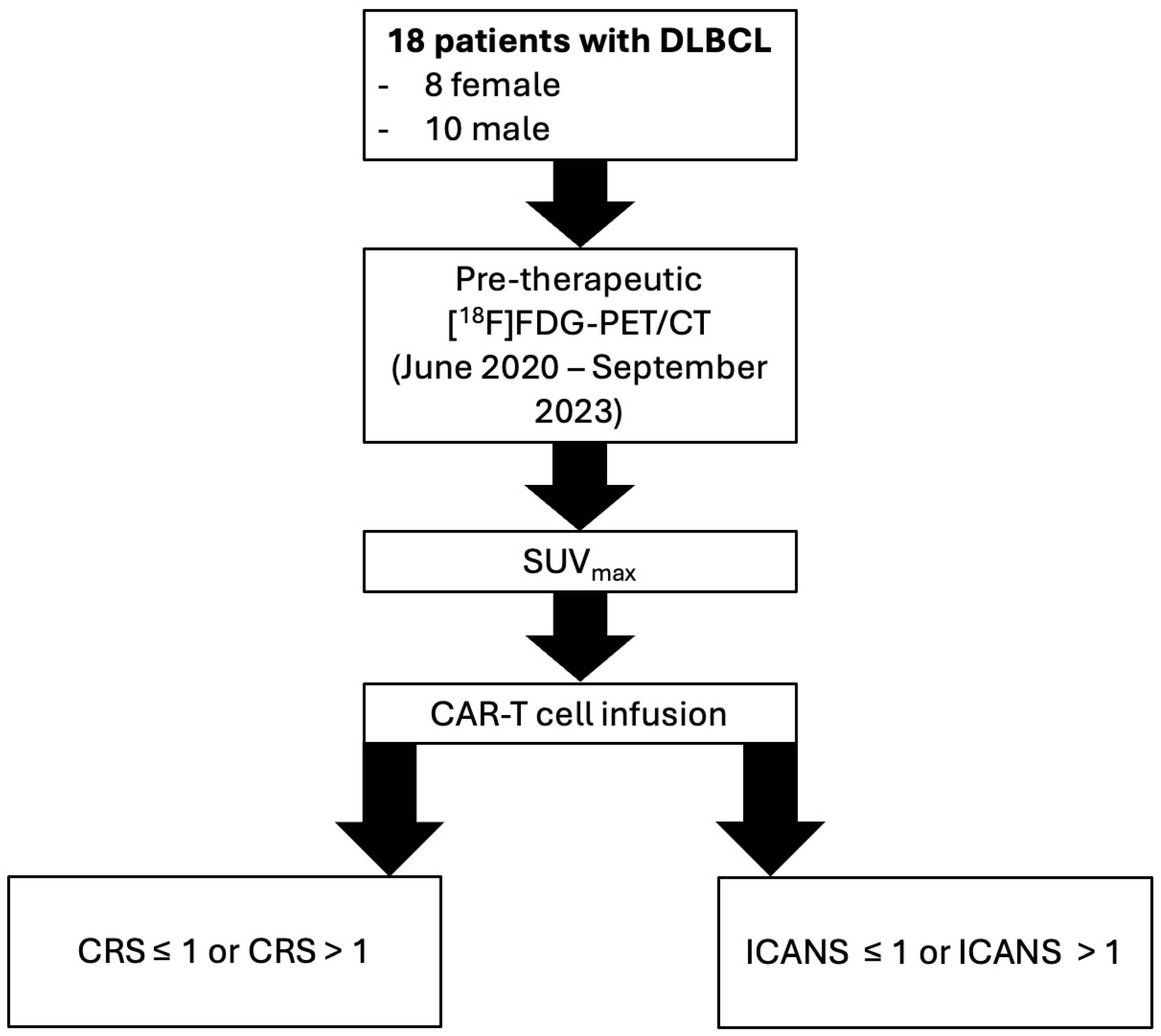
2.1. Patients
2.2. PET/CT Imaging
2.3. Image Analysis
2.4. Patients’ Demographics/Characteristics, Follow-Up and Clinical Data
2.5. Statistical Analysis
3. Results
3.1. Patient Characteristic and PET/CT Metabolic Parameters
3.2. SUVmax and Clinical Parameters
3.3. Prediction of Toxicity
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Miliotou, A.N.; Papadopoulou, L.C. CAR T-cell Therapy: A New Era in Cancer Immunotherapy. Curr. Pharm. Biotechnol. 2018, 19, 5–18. [Google Scholar] [CrossRef]
- Al-Mansour, M.; Al-Foheidi, M.; Ibrahim, E. Efficacy and safety of second-generation CAR T-cell therapy in diffuse large B-cell lymphoma: A meta-analysis. Mol. Clin. Oncol. 2020, 13, 33. [Google Scholar] [CrossRef]
- Derlin, T.; Schultze-Florey, C.; Werner, R.A.; Möhn, N.; Skripuletz, T.; David, S.; Beutel, G.; Eder, M.; Ross, T.L.; Bengel, F.M.; et al. 18F-FDG PET/CT of off-target lymphoid organs in CD19-targeting chimeric antigen receptor T-cell therapy for relapsed or refractory diffuse large B-cell lymphoma. Ann. Nucl. Med. 2021, 35, 132–138. [Google Scholar] [CrossRef]
- Neelapu, S.S.; Locke, F.L.; Bartlett, N.L.; Lekakis, L.J.; Miklos, D.B.; Jacobson, C.A.; Braunschweig, I.; Oluwole, O.O.; Siddiqi, T.; Lin, Y.; et al. Axicabtagene Ciloleucel CAR T-Cell Therapy in Refractory Large B-Cell Lymphoma. N. Engl. J. Med. 2017, 377, 2531–2544. [Google Scholar] [CrossRef]
- Elsawy, M.; Chavez, J.C.; Avivi, I.; Larouche, J.F.; Wannesson, L.; Cwynarski, K.; Osman, K.; Davison, K.; Rudzki, J.D.; Dahiya, S.; et al. Patient-reported outcomes in ZUMA-7, a phase 3 study of axicabtagene ciloleucel in second-line large B-cell lymphoma. Blood 2022, 140, 2248–2260. [Google Scholar] [CrossRef]
- Wang, J.; Galal, A. Can Fluorodeoxyglucose Positron Emission Tomography/Computed Tomography Predict Chimeric Antigen Receptor T Cell Adverse Effects? Biol. Blood Marrow Transpl. 2019, 25, e187–e188. [Google Scholar] [CrossRef] [PubMed]
- Ye, C.Y.; Zhao, L.N.; Wang, S.Y.; Cheng, H.; Chen, W.; Qi, K.M.; Wu, Q.Y.; Li, Z.Y.; Xu, K.L.; Cao, J. Analysis of Related Early Warning Indexes of Cytokine Release Syndrome in Multiple Myeloma Patients after CAR-T Treatment. Zhongguo Shi Yan Xue Ye Xue Za Zhi 2021, 29, 1203–1208. [Google Scholar] [PubMed]
- Vercellino, L.; de Jong, D.; di Blasi, R.; Kanoun, S.; Reshef, R.; Schwartz, L.H.; Dercle, L. Current and Future Role of Medical Imaging in Guiding the Management of Patients with Relapsed and Refractory Non-Hodgkin Lymphoma Treated with CAR T-Cell Therapy. Front. Oncol. 2021, 11, 664688. [Google Scholar] [CrossRef] [PubMed]
- Shouval, R.; Strouse, C.; Kim, S.; Oloyede, T.; Ahmed, S.; Awan, F.T.; Luan, D.; Bachanova, V.; Badar, T.; Bar, M.; et al. Cytokine Release Syndrome and Neurotoxicity Following CD19 CAR-T in B-Cell Lymphoma. Transpl. Cell Ther. 2025, 31, 419–433. [Google Scholar] [CrossRef]
- Rivera, A.M.; May, S.; Lei, M.; Qualls, S.; Bushey, K.; Rubin, D.B.; Barra, M.E. CAR T-Cell-Associated Neurotoxicity: Current Management and Emerging Treatment Strategies. Crit. Care Nurs. Q. 2020, 43, 191–204. [Google Scholar] [CrossRef]
- Wang, X.; He, X.; Zhang, T.; Liu, J.; Zhao, M. Latest updates on pathogenesis mechanisms and management strategies for cytokine release syndrome, neurotoxicity, and hemophagocytic lymphohistiocytosis related to CAR-T cell therapies. Ann. Hematol. 2025, 104, 3129–3151. [Google Scholar] [CrossRef]
- Tilly, H.; Gomes da Silva, M.; Vitolo, U.; Jack, A.; Meignan, M.; Lopez-Guillermo, A.; Walewski, J.; André, M.; Johnson, P.W.; Pfreundschuh, M.; et al. Diffuse large B-cell lymphoma (DLBCL): ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann. Oncol. 2015, 26 (Suppl. 5), v116–v125. [Google Scholar] [CrossRef]
- Goyal, H.; Jain, S. Applications of 18F-FDG PET/CT in Lymphoma and leukemia with focus on NCCN guidelines: A pictorial review. J. Nucl. Med. 2023, 64 (Suppl. 1), 1123. [Google Scholar]
- Marchal, E.; Palard-Novello, X.; Lhomme, F.; Meyer, M.E.; Manson, G.; Devillers, A.; Marolleau, J.P.; Houot, R.; Girard, A. Baseline [18F]FDG PET features are associated with survival and toxicity in patients treated with CAR T cells for large B cell lymphoma. Eur. J. Nucl. Med. Mol. Imaging 2024, 51, 481–489. [Google Scholar] [CrossRef]
- Mbakaza, O.; Vangu, M.W. 18F-FDG PET/CT Imaging: Normal Variants, Pitfalls, and Artifacts Musculoskeletal, Infection, and Inflammation. Front. Nucl. Med. 2022, 2, 847810. [Google Scholar] [CrossRef] [PubMed]
- Kirienko, M.; Gelardi, F.; Fiz, F.; Bauckneht, M.; Ninatti, G.; Pini, C.; Briganti, A.; Falconi, M.; Oyen, W.J.G.; van der Graaf, W.T.A.; et al. Personalised PET imaging in oncology: An umbrella review of meta-analyses to guide the appropriate radiopharmaceutical choice and indication. Eur. J. Nucl. Med. Mol. Imaging 2024, 52, 208–224. [Google Scholar] [CrossRef] [PubMed]
- Tomasik, J.; Avni, B.; Grisariu, S.; Elias, S.; Zimran, E.; Stepensky, P.; Basak, G.W. Endothelial Activation and Stress Index Score as a Prognostic Factor of Cytokine Release Syndrome in CAR-T Patients—A Retrospective Analysis of Multiple Myeloma and Large B-Cell Lymphoma Cohorts. Arch. Immunol. Ther. Exp. 2024, 72, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Korell, F.; Penack, O.; Mattie, M.; Schreck, N.; Benner, A.; Krzykalla, J.; Wang, Z.; Schmitt, M.; Bullinger, L.; Müller-Tidow, C.; et al. EASIX and Severe Endothelial Complications After CD19-Directed CAR-T Cell Therapy—A Cohort Study. Front. Immunol. 2022, 13, 877477. [Google Scholar] [CrossRef]
- World Medical Association. World Medical Association Declaration of Helsinki: Ethical principles for medical research involving human subjects. JAMA 2013, 310, 2191–2194. [Google Scholar] [CrossRef]
- Kuehl, H.; Veit, P.; Rosenbaum, S.J.; Bockisch, A.; Antoch, G. Can PET/CT replace separate diagnostic CT for cancer imaging? Optimizing CT protocols for imaging cancers of the chest and abdomen. J. Nucl. Med. 2007, 48 (Suppl. 1), 45S–57S. [Google Scholar]
- Cheson, B.D.; Fisher, R.I.; Barrington, S.F.; Cavalli, F.; Schwartz, L.H.; Zucca, E.; Lister, T.A. Recommendations for Initial Evaluation, Staging, and Response Assessment of Hodgkin and Non-Hodgkin Lymphoma: The Lugano Classification. J. Clin. Oncol. 2014, 32, 3059–3067. [Google Scholar] [CrossRef]
- Kinahan, P.E.; Fletcher, J.W. Positron emission tomography-computed tomography standardized uptake values in clinical practice and assessing response to therapy. Semin. Ultrasound CT MR 2010, 31, 496–505. [Google Scholar] [CrossRef]
- Massaro, A.; Cittadin, S.; Milan, E.; Tamiso, L.; Pavan, L.; Secchiero, C.; Rampin, L.; Grassetto, G.; Marzola, M.C.; Rubello, D. Reliability of SUVmax vs. SUVmean FDG PET/CT. J. Nucl. Med. 2009, 50 (Suppl. 2), 2121. [Google Scholar]
- Lee, D.W.; Santomasso, B.D.; Locke, F.L.; Ghobadi, A.; Turtle, C.J.; Brudno, J.N.; Maus, M.V.; Park, J.H.; Mead, E.; Pavletic, S.; et al. ASTCT Consensus Grading for Cytokine Release Syndrome and Neurologic Toxicity Associated with Immune Effector Cells. Biol. Blood Marrow Transpl. 2019, 25, 625–638. [Google Scholar] [CrossRef] [PubMed]
- Hong, R.; Tan Su Yin, E.; Wang, L.; Zhao, X.; Zhou, L.; Wang, G.; Zhang, M.; Zhao, H.; Wei, G.; Wang, Y.; et al. Tumor Burden Measured by 18F-FDG PET/CT in Predicting Efficacy and Adverse Effects of Chimeric Antigen Receptor T-Cell Therapy in Non-Hodgkin Lymphoma. Front. Oncol. 2021, 11, 713577. [Google Scholar] [CrossRef]
- Brudno, J.N.; Kochenderfer, J.N. Recent advances in CAR T-cell toxicity: Mechanisms, manifestations and management. Blood Rev. 2019, 34, 45–55. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.; Hu, Y.; Yang, S.; Wei, G.; Zhao, X.; Wu, W.; Zhang, Y.; Zhang, Y.; Chen, D.; Wu, Z.; et al. Role of Fluorodeoxyglucose Positron Emission Tomography/Computed Tomography in Predicting the Adverse Effects of Chimeric Antigen Receptor T Cell Therapy in Patients with Non-Hodgkin Lymphoma. Biol. Blood Marrow Transplant. 2019, 25, 1092–1098. [Google Scholar] [CrossRef] [PubMed]
- Al-Ibraheem, A.; Abdlkadir, A.S.; Lopci, E.; Allouzi, S.; Paez, D.; Alkuwari, M.; Makoseh, M.; Novruzov, F.; Usmani, S.; Al-Rabi, K.; et al. FDG-PET in Chimeric Antigen Receptor T-Cell (CAR T-Cell) Therapy Toxicity: A Systematic Review. Cancers 2024, 16, 1728. [Google Scholar] [CrossRef]
- Zhou, Y.; Li, J.; Zhang, X.; Jia, T.; Zhang, B.; Dai, N.; Sang, S.; Deng, S. Prognostic Value of Radiomic Features of 18F-FDG PET/CT in Patients with B-Cell Lymphoma Treated with CD19/CD22 Dual-Targeted Chimeric Antigen Receptor T Cells. Front. Oncol. 2022, 12, 834288. [Google Scholar] [CrossRef]
- Ababneh, H.S.; Ng, A.K.; Abramson, J.S.; Soumerai, J.D.; Takvorian, R.W.; Frigault, M.J.; Patel, C.G. Metabolic parameters predict survival and toxicity in chimeric antigen receptor T-cell therapy-treated relapsed/refractory large B-cell lymphoma. Hematol. Oncol. 2024, 42, e3231. [Google Scholar] [CrossRef]
- Gui, J.; Li, M.; Xu, J.; Zhang, X.; Mei, H.; Lan, X. [18F]FDG PET/CT for prognosis and toxicity prediction of diffuse large B-cell lymphoma patients with chimeric antigen receptor T-cell therapy. Eur. J. Nucl. Med. Mol. Imaging 2024, 51, 2308–2319. [Google Scholar] [CrossRef]
- Giavridis, T.; van der Stegen, S.J.C.; Eyquem, J.; Hamieh, M.; Piersigilli, A.; Sadelain, M. CAR T cell-induced cytokine release syndrome is mediated by macrophages and abated by IL-1 blockade. Nat. Med. 2018, 24, 731–738. [Google Scholar] [CrossRef]
- Norelli, M.; Camisa, B.; Barbiera, G.; Falcone, L.; Purevdorj, A.; Genua, M.; Sanvito, F.; Ponzoni, M.; Doglioni, C.; Cristofori, P.; et al. Monocyte-derived IL-1 and IL-6 are differentially required for cytokine-release syndrome and neurotoxicity due to CAR T cells. Nat. Med. 2018, 24, 739–748. [Google Scholar] [CrossRef]
- Pennisi, M.; Sanchez-Escamilla, M.; Flynn, J.R.; Shouval, R.; Alarcon Tomas, A.; Silverberg, M.L.; Batlevi, C.; Brentjens, R.J.; Dahi, P.B.; Devlin, S.M.; et al. Modified EASIX predicts severe cytokine release syndrome and neurotoxicity after chimeric antigen receptor T cells. Blood Adv. 2021, 5, 3397–3406. [Google Scholar] [CrossRef] [PubMed]
- Crispe, I.N. The liver as a lymphoid organ. Annu. Rev. Immunol. 2009, 27, 147–163. [Google Scholar] [CrossRef]
- Messmer, A.S.; Que, Y.-A.; Schankin, C.; Banz, Y.; Bacher, U.; Novak, U.; Pabst, T. CAR T-cell therapy and critical care. Wien. Klin. Wochenschr. 2021, 133, 1318–1325. [Google Scholar] [CrossRef] [PubMed]


| Grade CRS | 1 | 2 | 3 | 4 |
|---|---|---|---|---|
| Temperature | ≥38 °C | ≥38 °C | ≥38 °C | ≥38 °C |
| Degree of hypotension | Awakens spontaneously | Awakens to voice | Awakens only to tactile stimulations | Stupor or coma |
| Degree of hypoxia | None | Hypotension not requiring vasopressors | Hypotension requiring one vasopressor | Hypotension requiring multiple vasopressors |
| Motor findings | None | Hypoxia requiring low-dose O2 supplementation | Hypoxia requiring high-dose O2 supplementation | Hypoxia requiring positive-pressure O2 supplementation |
| Grade ICANS | 1 | 2 | 3 | 4 |
| ICE score | 7–9 | 3–6 | 0–2 | 0 |
| Depressed level of consciousness | Awakens spontaneously | Awakens to voice | Awakens only to tactile stimulations | Stupor or coma |
| Seizure | N/A | N/A | Any clinical seizure focal or generalized that resolves rapidly or nonconvulsive seizures on EEG that resolves with intervention | Life-threatening prolonged seizure (<5 min) or repetitive clinical or electrical seizures without return to baseline in between |
| Motor findings | N/A | N/A | Life-threatening prolonged seizure (<5 min) or repetitive clinical or electrical seizures without return to baseline in between | Deep focal motor weakness such as hemiparesis or paraparesis |
| Elevated ICP/cerebral edema | N/A | N/A | Focal/local edema on neuroimaging | Diffuse cerebral edema on neuroimaging; decerebrate or decorticate posturing; cranial nerve VI palsy; papilledema; or Cushing’s triad |
| Patients’ Demographics/Characteristics/Side Effects | Value | Percentage (%) |
|---|---|---|
| Number of Patients | n = 18 | 100 |
| Age in years | ||
| Mean ± SD | 60 ± 12 | |
| Gender | ||
| Female | n = 8/18 | 44 |
| Male | n = 10/18 | 56 |
| Initial Ann Arbor stage (AAS) | ||
| I | n = 2/18 | 11.1 |
| II | n = 1/18 | 5.6 |
| III | n = 5/18 | 27.8 |
| IV | n = 10/18 | 55.5 |
| Cytokine Release Syndrome (CRS) | ||
| no CRS | n = 2/18 | 11.1 |
| 1 | n = 10/18 | 55.5 |
| 2 | n = 4/18 | 22.2 |
| 3 | n = 1/18 | 5.6 |
| 4 | n = 1/18 | 5.6 |
| Immune Effector Cell-associated Neurotoxicity Syndrome (ICANS) | ||
| no ICANS | n = 14/18 | 77.7 |
| 1 | n = 0/18 | 0 |
| 2 | n = 2/18 | 11.1 |
| 3 | n = 1/18 | 5.6 |
| 4 | n = 1/18 | 5.6 |
| CRS ≤ 1 vs. CRS > 1 | ICANS ≤ 1 vs. ICANS > 1 | |
|---|---|---|
| Mann–Whitney U | 16.0 | 7.0 |
| Wilcoxon W | 94.0 | 112.0 |
| Z | −1.9 | −2.2 |
| p-value | 0.07 | 0.03 * |
| Mean SUVmax ± SD | 8.0 ± 6.4 vs. 17.4 ± 11.9 | 8.0 ± 5.7 vs. 22.5 ± 12 |
| Baseline Clinical Parameters and Adverse Events | Pre-Therapeutic SUVmax | ||
|---|---|---|---|
| r | p | Odds: SUVmax > 17 | |
| LDH | 0.5 CI: 0.04, 0.74 | 0.02 * | __ |
| IL-6 | 0.1 CI: −0.46, 0.48 | >0.05 | __ |
| CRP | 0.2 CI: −0.29, 0.61 | >0.05 | __ |
| mEASIX score | 0.3 CI: −0.19, 0.67 | >0.05 | __ |
| CRS | 0.5 CI: 0.04, 0.78 | 0.03 * | CRS > 1: p = 0.03 OR = 22 CI 2, 314 * |
| ICANS | 0.6 CI: 0.19, 0.83 | 0.01 * | ICANS > 1: p = 0.04 OR = 18 CI 1, 271 * |
| CRS | ICANS | |||
|---|---|---|---|---|
| r | p | r | p | |
| SUVmax spleen | 0.0 CI: −0.47, 0.47 | 0.91 | −0.2 CI: −0.62, 0.30 | 0.48 |
| SUVmax liver | 0.1 CI: −0.38, 0.54 | 0.64 | 0.1 CI: −0.38, 0.54 | 0.75 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Peters, H.A.; Novruzov, E.; Bärmann, B.-N.; Weiss, D.; Boschheidgen, M.; Ivan, V.L.; Liebers, N.; Fischer, J.; Mamlins, E.; Radujkovic, A.; et al. Predictive Power of Baseline [18F]FDG PET/CT for Adverse Events in DLBCL Patients Undergoing CAR-T Cell Therapy. Diagnostics 2025, 15, 2025. https://doi.org/10.3390/diagnostics15162025
Peters HA, Novruzov E, Bärmann B-N, Weiss D, Boschheidgen M, Ivan VL, Liebers N, Fischer J, Mamlins E, Radujkovic A, et al. Predictive Power of Baseline [18F]FDG PET/CT for Adverse Events in DLBCL Patients Undergoing CAR-T Cell Therapy. Diagnostics. 2025; 15(16):2025. https://doi.org/10.3390/diagnostics15162025
Chicago/Turabian StylePeters, Helena A., Emil Novruzov, Ben-Niklas Bärmann, Daniel Weiss, Matthias Boschheidgen, Vivien Lorena Ivan, Nora Liebers, Johannes Fischer, Eduards Mamlins, Aleksandar Radujkovic, and et al. 2025. "Predictive Power of Baseline [18F]FDG PET/CT for Adverse Events in DLBCL Patients Undergoing CAR-T Cell Therapy" Diagnostics 15, no. 16: 2025. https://doi.org/10.3390/diagnostics15162025
APA StylePeters, H. A., Novruzov, E., Bärmann, B.-N., Weiss, D., Boschheidgen, M., Ivan, V. L., Liebers, N., Fischer, J., Mamlins, E., Radujkovic, A., Kobbe, G., Kirchner, J., Minko, P., Nachtkamp, K., Jäger, P., Antke, C., Giesel, F. L., Dietrich, S., Antoch, G., & Jannusch, K. (2025). Predictive Power of Baseline [18F]FDG PET/CT for Adverse Events in DLBCL Patients Undergoing CAR-T Cell Therapy. Diagnostics, 15(16), 2025. https://doi.org/10.3390/diagnostics15162025








