Precision in Practice: Clinical Indication-Specific DRLs for Head CT for Advanced Personalised Dose Benchmarking
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Data Collection
2.2. CT Equipment
2.3. Protocol Parameters Based on Clinical Indications
2.4. Data Analysis
3. Results
3.1. Demographic and Clinical Indication Profile of CT Head Patients
3.2. Radiation Dose Parameters by Clinical Indication for CT Head Examinations
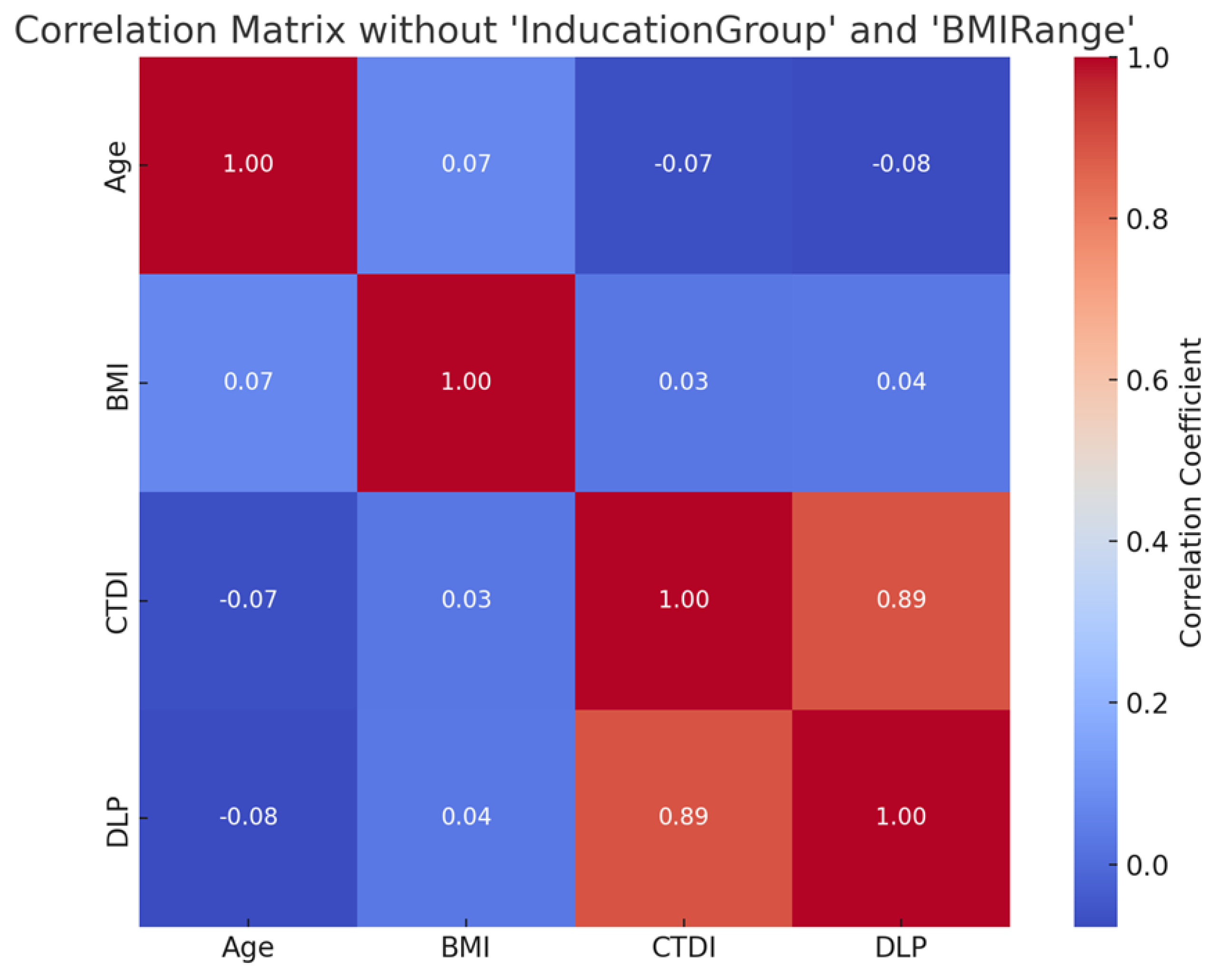
3.3. Correlation Analysis Between Patient and Dose Parameters
4. Discussion
5. Limitations
6. Conclusions
7. Recommendations
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| AEC | Automatic Exposure Control |
| ALARA | As Low As Reasonably Achievable |
| BMI | Body Mass Index |
| CTA | CT Angiography |
| CT | Computed Tomography |
| CTDIvol | Computed Tomography Dose Index Volume |
| DLP | Dose–Length Product |
| DRL | Diagnostic Reference Level |
| DRLCI | Diagnostic Reference Level based on Clinical Indication |
| EUCLID | European Study on Clinical Diagnostic Reference Levels |
| FOV | Field of View |
| GE | General Electric (as in GE Healthcare) |
| ICRP | International Commission on Radiological Protection |
| NDRL | National Diagnostic Reference Level |
| PACS | Picture Archiving and Communication System |
| RIS | Radiology Information System |
| SD | Standard Deviation |
References
- Abuzaid, M.M.; Elshami, W.; Tekin, H.O.; Sulieman, A.; Bradley, D.A. Comparison of radiation dose and image quality in head CT scans among multidetector CT scanners. Radiat. Prot. Dosim. 2021, 196, 10–16. [Google Scholar] [CrossRef] [PubMed]
- Abuzaid, M.M.; Elshami, W.; Sulieman, A.; Bradley, D. Cumulative radiation exposure, effective and organ dose estimation from multiple head CT scans in stroke patients. Radiat. Phys. Chem. 2022, 199, 110306. [Google Scholar] [CrossRef]
- Vañó, E.; Miller, D.L.; Martin, C.J.; Rehani, M.M.; Kang, K.; Rosenstein, M.; Ortiz-López, P.; Mattsson, S.; Padovani, R.; Rogers, A. ICRP Publication 135: Diagnostic Reference Levels in Medical Imaging. Ann. ICRP 2017, 46, 1–144. [Google Scholar] [CrossRef] [PubMed]
- Martin, C.J.; Vano, E. Diagnostic Reference Levels and Optimisation in Radiology: Where Do We Go from Here? J. Radiol. Prot. 2018, 38, E1–E4. [Google Scholar] [CrossRef] [PubMed]
- Steffensen, C.; Trypis, G.; Mander, G.T.W.; Munn, Z. Optimisation of Radiographic Acquisition Parameters for Direct Digital Radiography: A Systematic Review. Radiography 2021, 27, 663–672. [Google Scholar] [CrossRef] [PubMed]
- Aly, A.; Tsapaki, V.; Ahmed, A.Z.; Own, A.; Patro, S.; Al Naemi, H.; Kharita, M.H. Clinical diagnostic reference levels in neuroradiology based on clinical indication. Radiat. Prot. Dosim. 2024, 200, 755–762. [Google Scholar] [CrossRef] [PubMed]
- Tsapaki, V.; Triantopoulou, S. Does clinical indication play a role in CT radiation dose in pediatric patients? Phys. Med. 2016, 32, 209–210. [Google Scholar] [CrossRef]
- Paulo, G.; Damilakis, J.; Tsapaki, V.; Schegerer, A.A.; Repussard, J. Diagnostic reference levels based on clinical indications in computed tomography: A literature review. Insights Imaging 2020, 11, 96. [Google Scholar] [CrossRef] [PubMed]
- Lin, C.J.; Mok, G.S.P.; Tsai, M.F.; Tsai, W.T.; Yang, B.H.; Tu, C.Y.; Wu, T.H. National survey of radiation dose and image quality in adult CT head scans in Taiwan. PLoS ONE 2015, 10, e0131243. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Habib Geryes, B.; Hornbeck, A.; Jarrige, V.; Pierrat, N.; Ducou Le Pointe, H.; Dreuil, S. Patient dose evaluation in computed tomography: A French national study based on clinical indications. Phys. Med. 2019, 61, 18–27. [Google Scholar] [CrossRef] [PubMed]
- AlNaemi, H.; Tsapaki, V.; Omar, A.J.; AlKuwari, M.; AlObadli, A.; Alkhazzam, S.; Aly, A.; Kharita, M.H. Towards establishment of diagnostic reference levels based on clinical indication in the State of Qatar. Eur. J. Radiol. Open 2020, 7, 100282. [Google Scholar] [CrossRef] [PubMed]
- Ukoha, P.O.; Idigo, F.U.; Chukwudi Okeji, M.; Joseph, D.; Flavious, N.; Onwuzu, S.; Joseph Skam, D.; Elshami, W. Clinical indication diagnostic reference level (DRLCI) and post-optimization image quality for adult computed tomography examinations in Enugu, South Eastern Nigeria. Radiat. Phys. Chem. 2023, 206, 110728. [Google Scholar] [CrossRef]
- International Commission on Radiological Protection. The 2007 recommendations of the International Commission on Radiological Protection. Ann. ICRP 2007, 37, 1–332. [Google Scholar] [CrossRef]
- Vano, E.; Miller, D.L.; Martin, C.J.; Rehani, M.M.; Kang, K.; Rosenstein, M.; Ortiz-Lopez, P.; Mattsson, S.; Padovani, R.; Rogers, A.T. The New ICRP Recommendations on Diagnostic Reference Levels for Medical Imaging. In Proceedings of the European Congress of Radiology—EuroSafe Imaging, Vienna, Austria, 28 February–4 March 2018. [Google Scholar] [CrossRef]
- International Commission on Radiological Protection. Managing patient dose in multi-detector computed tomography. Ann. ICRP 2007, 37, 1–79. [Google Scholar] [CrossRef]
- Damilakis, J.; Frija, G.; Hierath, M.; Jaschke, W.; Mayerhofer-Sebera, U.; Paulo, G.; Repussard, J.; Schegerer, A.; Tsapaki, V.; Verius, M. EUCLID. European Study on Clinical Diagnostic Reference Levels for X-Ray Medical Imaging Deliverable 2.1: Report and Review on Existing Clinical DRLs; European Commission: Luxembourg, 2018. [Google Scholar]
- Hasan, N.; Rizk, C.; Babikir, E. National diagnostic reference levels based on clinical indications and patient size for adults’ computed tomography in the Kingdom of Bahrain. Radiat. Phys. Chem. 2022, 197, 110147. [Google Scholar] [CrossRef]
- Tsapaki, V.; Damilakis, J.; Paulo, G.; Schegerer, A.A.; Jaschke, W.; Frija, G. EuroSafe imaging diagnostic reference levels based on clinical indications: Results of a large-scale European survey. Eur. Radiol. 2021, 31, 4459–4469. [Google Scholar] [CrossRef] [PubMed]
- Abuzaid, M. Optimizing radiation dose in high-resolution chest CT: The impact of patient-specific factors and size-specific dose estimates. Diagnostics 2025, 15, 740. [Google Scholar] [CrossRef] [PubMed]
- Modlińska, S.; Rojek, M.; Bielówka, M.; Kufel, J. Establishing Local Diagnostic Reference Levels for Head Computed Tomography Examinations. Biomedicines 2024, 12, 2446. [Google Scholar] [CrossRef] [PubMed]
- Sakhnini, L. CT Radiation Dose Optimization and Reduction for Routine Head, Chest and Abdominal CT Examination. Radiol. Diagn. Imaging 2018, 2, 1–4. [Google Scholar] [CrossRef]
- Kumamaru, K.K.; Kogure, Y.; Suzuki, M.; Hori, M.; Nakanishi, A.; Kamagata, K.; Hagiwara, A.; Andica, C.; Ri, K.; Houshido, N.; et al. A strategy to optimize radiation exposure for non-contrast head CT: Comparison with the Japanese diagnostic reference levels. Jpn. J. Radiol. 2016, 34, 451–457. [Google Scholar] [CrossRef] [PubMed]
| Parameter | Head |
|---|---|
| Scan Type | Helical |
| Detector Rows | 32 |
| Pitch | 0.531 |
| Rotation Time (s) | 0.5 |
| Kilo Volt (kV) | 120 |
| Automatic Exposure Control Type | Smart mA |
| Milliampere (mA) Range (Manual mA) | 130–440 (210) |
| Slice Thickness (mm) /Interval (mm) | 5/5 |
| Scanning Length (mm) | 140–180 |
| Category | Variable | n (%) |
|---|---|---|
| Gender | Female | 168 (44.4%) |
| Male | 210 (55.6%) | |
| BMI Range | Healthy Weight (BMI * 18.5–24.9) | 155 (41.0) |
| Overweight (BMI 25–29.9) | 179 (47.4) | |
| Obesity (BMI ≥ 30) | 44 (11.6) | |
| Indications | Trauma | 102 (27.0) |
| Headache | 99 (26.2) | |
| Stroke | 99 (26.2) | |
| Seizure | 43 (11.4) | |
| Infection | 35 (9.3) |
| Clinical Indication | Dose | Mean ± SD | 75 Percentile |
|---|---|---|---|
| Headache | CTDI vol | 51.26 ± 5.36 | 54.07 |
| DLP | 1078.32 ± 176.24 | 1205.78 | |
| Infection | CTDI vol | 52.90 ± 5.57 | 54.15 |
| DLP | 1142.97 ± 127.71 | 1219.98 | |
| Seizure | CTDI vol | 51.88 ± 6.10 | 54.13 |
| DLP | 1099.97 ± 185.07 | 1212.66 | |
| Stroke | CTDI vol | 50.65 ± 5.28 | 54.07 |
| DLP | 1065.02 ± 194.73 | 1205.78 | |
| Trauma | CTDI vol | 50.58 ± 5.59 | 54.06 |
| DLP | 1052.52 ± 194.09 | 1205.74 |
| Clinical Indication | Study | CTDIvol (mGy) | DLP (mGy·cm) |
|---|---|---|---|
| Stroke | European Survey | 48 | 1386 |
| Nigeria | 43 | 879 | |
| Bahrain | 66 | 1152 | |
| Current Study | 54.07 | 1205.78 | |
| Trauma | Nigeria | 43 | 907 |
| Qatar | 51 | 1820 | |
| Bahrain | 66 | 1286 | |
| Current Study | 54.06 | 1205.74 | |
| Seizure | Nigeria | 28 | 995 |
| Current Study | 54.13 | 1212.66 | |
| Infection | Nigeria | 34 | 969 |
| Current Study | 54.15 | 1219.98 | |
| Headache | Bahrain | 67 | 1206 |
| Current Study | 54.07 | 1205.78 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Almuqbil, N.; Hamd, Z.Y.; Elshami, W.; Abuzaid, M. Precision in Practice: Clinical Indication-Specific DRLs for Head CT for Advanced Personalised Dose Benchmarking. Diagnostics 2025, 15, 1849. https://doi.org/10.3390/diagnostics15151849
Almuqbil N, Hamd ZY, Elshami W, Abuzaid M. Precision in Practice: Clinical Indication-Specific DRLs for Head CT for Advanced Personalised Dose Benchmarking. Diagnostics. 2025; 15(15):1849. https://doi.org/10.3390/diagnostics15151849
Chicago/Turabian StyleAlmuqbil, Nora, Zuhal Y. Hamd, Wiam Elshami, and Mohamed Abuzaid. 2025. "Precision in Practice: Clinical Indication-Specific DRLs for Head CT for Advanced Personalised Dose Benchmarking" Diagnostics 15, no. 15: 1849. https://doi.org/10.3390/diagnostics15151849
APA StyleAlmuqbil, N., Hamd, Z. Y., Elshami, W., & Abuzaid, M. (2025). Precision in Practice: Clinical Indication-Specific DRLs for Head CT for Advanced Personalised Dose Benchmarking. Diagnostics, 15(15), 1849. https://doi.org/10.3390/diagnostics15151849







