Evaluation of Maxillary Dentoalveolar Expansion with Clear Aligners: A Retrospective CBCT Study
Abstract
1. Introduction
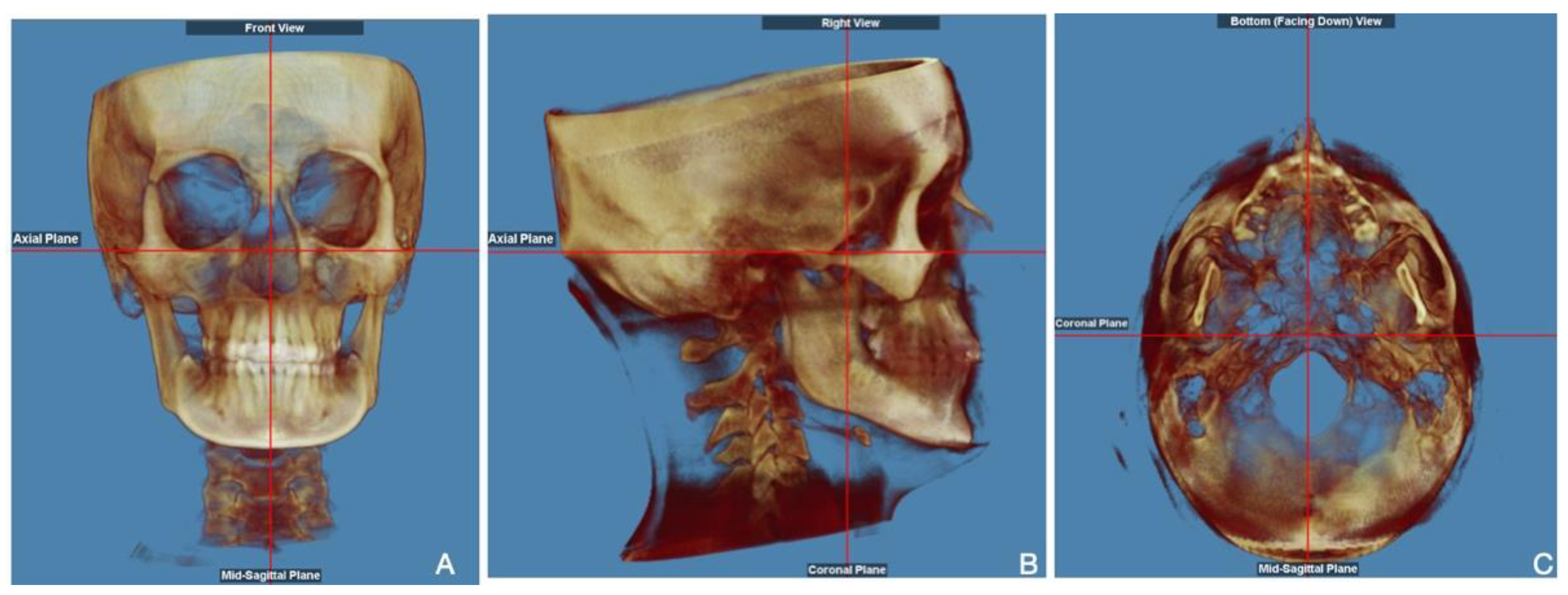
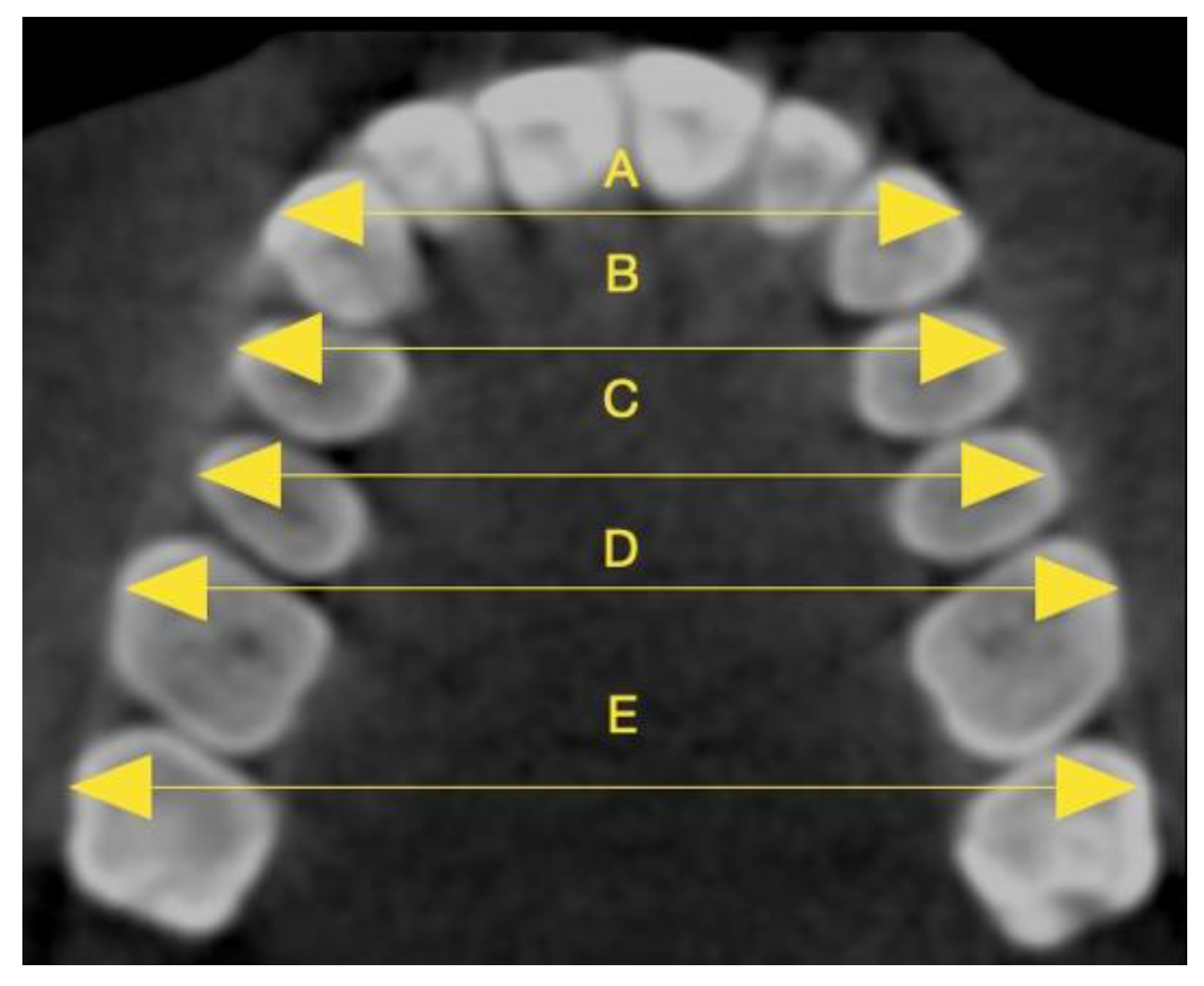
2. Materials and Methods
Statistical Analysis
3. Results
4. Discussion
5. Conclusions
- We obtained a significant increase in maxillary alveolar bone width, particularly in the buccal and palatal alveolar ridges.
- We observed an efficient transverse expansion at both apex and cusp levels from canines to second molars.
- The inter-apex and inter-cusp widths achieved at the end of therapy differed significantly in relation to tooth position. The interpremolar widths exhibited the most notable increase and the most effective variation in treatment response.
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- McNamara, J.A. Maxillary transverse deficiency. Am. J. Orthod. Dentofac. Orthop. 2000, 117, 567–570. [Google Scholar] [CrossRef] [PubMed]
- Srivastava, S.C.; Mahida, K.; Agarwal, C.; Chavda, R.M.; Patel, H.A. Longitudinal Stability of Rapid and Slow Maxillary Expansion: A Systematic Review. J. Contemp. Dent. Pract. 2020, 21, 1068–1072. [Google Scholar] [CrossRef]
- Wei, N.; Wang, C.; Zhang, Y.; Wei, Y.; Hu, W.; Yang, X.; Chung, K.H. The Influence of the Maxillary Posterior Region on Smile Aesthetics in a Chinese Cohort. Int. Dent. J. 2022, 72, 659–666. [Google Scholar] [CrossRef] [PubMed]
- Lacruz, R.S.; Bermúdez de Castro, J.M.; Martinón-Torres, M.; O’Higgins, P.; Paine, M.L.; Carbonell, E.; Arsuaga, J.L.; Bromage, T.G. Facial morphogenesis of the earliest europeans. PLoS ONE 2013, 6, e65199. [Google Scholar] [CrossRef]
- Festa, F.; D’Anastasio, R.; Benazzi, S.; Macrì, M. Three-Dimensional Analysis of the Maxillary Sinuses in Ancient Crania Dated to the V–VI Centuries BCE from Opi (Italy): Volumetric Measurements in Ancient Skulls from the Necropolis of Opi, Abruzzi, Italy. Diagnostics 2024, 14, 1683. [Google Scholar] [CrossRef] [PubMed]
- Huynh, T.; Kennedy, D.B.; Joondeph, D.R.; Bollen, A.M. Treatment response and stability of slow maxillary expansion using Haas, hyrax, and quad-helix appliances: A retrospective study. Am. J. Orthod. Dentofac. Orthop. 2009, 136, 331–339. [Google Scholar] [CrossRef] [PubMed]
- Andrucioli, M.C.D.; Matsumoto, M.A.N. Transverse maxillary deficiency: Treatment alternatives in face of early skeletal maturation. Dental Press J. Orthod. 2020, 25, 70–79. [Google Scholar] [CrossRef]
- Festa, F.; Festa, M.; Medori, S.; Perrella, G.; Valentini, P.; Bolino, G.; Macrì, M. Midpalatal Suture Maturation in Relation to Age, Sex, and Facial Skeletal Growth Patterns: A CBCT Study. Children 2024, 11, 1013. [Google Scholar] [CrossRef]
- Revankar, A.V.; Bhat, S.S.; Rozario, J.E. A comparison of the quadhelix and the nickel-titanium palatal expander in the treatment of narrow maxillary arches: A prospective clinical study. J. Orthod. Sci. 2023, 12, 8. [Google Scholar] [CrossRef]
- Perrotti, G.; Carrafiello, A.; Rossi, O.; Karanxha, L.; Baccaglione, G.; Del Fabbro, M. Clinical Use of Aligners Associated with Nuvola® OP System for Transverse Maxillary Deficiency: A Retrospective Study on 100 Patients. Int. J. Environ. Res. Public Health 2022, 19, 5751. [Google Scholar] [CrossRef]
- Robertson, L.; Kaur, H.; Fagundes, N.C.F.; Romanyk, D.; Major, P.; Flores Mir, C. Effectiveness of clear aligner therapy for orthodontic treatment: A systematic review. Orthod. Craniofac. Res. 2020, 23, 133–142. [Google Scholar] [CrossRef] [PubMed]
- Santucci, V.; Rossouw, P.E.; Michelogiannakis, D.; El-Baily, T.; Feng, C. Assessment of Posterior Dentoalveolar Expansion with Invisalign in Adult Patients. Int. J. Environ. Res. Public Health 2023, 20, 4318. [Google Scholar] [CrossRef] [PubMed]
- Weir, T. Clear aligners in orthodontic treatment. Aust. Dent. J. 2017, 62, 58–62. [Google Scholar] [CrossRef]
- Livas, C.; Pazhman, F.S.; Ilbeyli, Z.; Pandis, N. Perceived esthetics and value of clear aligner therapy systems: A survey among dental school instructors and undergraduate students. Dent. Press J. Orthod. 2023, 28, e232225. [Google Scholar] [CrossRef]
- Pacheco-Pereira, C.; Brandelli, J.; Flores-Mir, C. Patient satisfaction and quality of life changes after Invisalign treatment. Am. J. Orthod. Dentofac. Orthop. 2018, 153, 834–841. [Google Scholar] [CrossRef]
- Bastidas-Castillo, D.A.; Ramirez-Naranjo, P. Surgery first with clear aligners for a Class II patient: Case report and literature review. J. Stomatol. Oral Maxillofac. Surg. 2024, 125, 101672. [Google Scholar] [CrossRef]
- Nshimiyimana, E.; Ubuzima, P.; Mukeshimana, C.; Michelogiannakis, D.; Mbyayingabo, D.; Mugabo, E.; Gakunzi, D.; Ndanga, E.; Mazimpaka, P.; Habumugisha, J. Skeletal and dental open bite treatment using clear aligners and orthodontic miniscrew-anchored fixed appliances in permanent dentition: A systematic review. J. World Fed. Orthod. 2025, 14, 46–63. [Google Scholar] [CrossRef] [PubMed]
- Vaid, N.R.; Sabouni, W.; Wilmes, B.; Bichu, Y.M.; Thakkar, D.P.; Adel, S.M. Customized adjuncts with clear aligner therapy: “The Golden Circle Model” explained! J. World Fed. Orthod. 2022, 11, 216–225. [Google Scholar] [CrossRef]
- Kravitz, N.D.; Dalloul, B.; Zaid, Y.A.; Shah, C.; Vaid, N.R. What percentage of patients switch from Invisalign to braces? A retrospective study evaluating the conversion rate, number of refinement scans, and length of treatment. Am. J. Orthod. Dentofac. Orthop. 2023, 163, 526–530. [Google Scholar] [CrossRef]
- Bilello, G.; Fazio, M.; Amato, E.; Crivello, L.; Galvano, A.; Currò, G. Accuracy evaluation of orthodontic movements with aligners: A prospective observational study. Prog. Orthod. 2022, 23, 12. [Google Scholar] [CrossRef]
- D’Antò, V.; Bucci, R.; De Simone, V.; Ghislanzoni, L.H.; Michelotti, A.; Rongo, R. Evaluation of Tooth Movement Accuracy with Aligners: A Prospective Study. Materials 2022, 15, 2646. [Google Scholar] [CrossRef] [PubMed]
- Rocha, A.S.; Gonçalves, M.; Oliveira, A.C.; Azevedo, R.M.S.; Pinho, T. Efficiency and Predictability of Coronal Maxillary Expansion Repercussion with the Aligners System: A Retrospective Study. Dent. J. 2023, 11, 258. [Google Scholar] [CrossRef] [PubMed]
- Aragon, M.L.S.C.; Mendes Ribeiro, S.M.; Fernandes Fagundes, N.C.; Normando, D. Effectiveness of dental arch expansion in the orthodontic treatment with clear aligners: A scoping review. Eur. J. Orthod. 2024, 46, cjae059. [Google Scholar] [CrossRef]
- Gu, J.; Tang, J.S.; Skulski, B.; Fields, H.W., Jr.; Beck, F.M.; Firestone, A.R.; Kim, D.G.; Deguchi, T. Evaluation of Invisalign treatment effectiveness and efficiency compared with conventional fixed appliances using the Peer Assessment Rating index. Am. J. Orthod. Dentofac. Orthop. 2017, 151, 259–266. [Google Scholar] [CrossRef]
- Ke, Y.; Zhu, Y.; Zhu, M. A comparison of treatment effectiveness between clear aligner and fixed appliance therapies. BMC Oral Health 2019, 19, 24. [Google Scholar] [CrossRef]
- Bouchant, M.; Saade, A.; El Helou, M. Is maxillary arch expansion with Invisalign® efficient and predictable? A systematic review. Int. Orthod. 2023, 21, 100750. [Google Scholar] [CrossRef] [PubMed]
- Deregibus, A.; Tallone, L.; Rossini, G.; Parrini, S.; Piancino, M.; Castroflorio, T. Morphometric analysis of dental arch form changes in class II patients treated with clear aligners. J. Orofac. Orthop. 2020, 81, 229–238. [Google Scholar] [CrossRef]
- Vidal-Bernárdez, M.L.; Vilches-Arenas, Á.; Sonnemberg, B.; Solano-Reina, E.; Solano-Mendoza, B. Efficacy and predictability of maxillary and mandibular expansion with the Invisalign® system. J. Clin. Exp. Dent. 2021, 13, e669–e677. [Google Scholar] [CrossRef]
- Solano-Mendoza, B.; Sonnemberg, B.; Solano-Reina, E.; Iglesias-Linares, A. How effective is the Invisalign® system in expansion movement with Ex30′ aligners? Clin. Oral Investig. 2017, 21, 1475–1484. [Google Scholar] [CrossRef]
- Abdelkarim, A. Cone-Beam Computed Tomography in Orthodontics. Dent. J. 2019, 7, 89. [Google Scholar] [CrossRef]
- Tang, H.; Liu, S.; Shi, Y.; Wei, J.; Peng, J.; Feng, H. Automatic segmentation and landmark detection of 3D CBCT images using semi supervised learning for assisting orthognathic surgery planning. Sci. Rep. 2025, 15, 8814. [Google Scholar] [CrossRef] [PubMed]
- Zhou, N.; Guo, J. Efficiency of upper arch expansion with the Invisalign system. Angle Orthod. 2020, 90, 23–30. [Google Scholar] [CrossRef] [PubMed]
- Macrì, M.; Medori, S.; Varvara, G.; Festa, F. A Digital 3D Retrospective Study Evaluating the Efficacy of Root Control during Orthodontic Treatment with Clear Aligners. Appl. Sci. 2023, 13, 1540. [Google Scholar] [CrossRef]
- Feragalli, B.; Rampado, O.; Abate, C.; Macrì, M.; Festa, F.; Stromei, F.; Caputi, S.; Guglielmi, G. Cone beam computed tomography for dental and maxillofacial imaging: Technique improvement and low-dose protocols. Radiol. Med. 2017, 122, 581–588. [Google Scholar] [CrossRef] [PubMed]
- Verma, S.K.; Maheshwari, S.; Gautam, S.N.; Prabhat, K.; Kumar, S. Natural head position: Key position for radiographic and photographic analysis and research of craniofacial complex. J. Oral Biol. Craniofac. Res. 2012, 2, 46–49. [Google Scholar] [CrossRef]
- Tian, K.; Li, Q.; Wang, X.; Liu, X.; Wang, X.; Li, Z. Reproducibility of natural head position in normal Chinese people. Am. J. Orthod. Dentofac. Orthop. 2015, 148, 503–510. [Google Scholar] [CrossRef]
- Macrì, M.; Toniato, E.; Murmura, G.; Varvara, G.; Festa, F. Midpalatal Suture Density as a Function of Sex and Growth-Pattern-Related Variability via CBCT Evaluations of 392 Adolescents Treated with a Rapid Maxillary Expander Appliance. Appl. Sci. 2022, 12, 2221. [Google Scholar] [CrossRef]
- Morales-Burruezo, I.; Gandía-Franco, J.L.; Cobo, J.; Vela-Hernández, A.; Bellot-Arcís, C. Arch expansion with the Invisalign system: Efficacy and predictability. PLoS ONE 2020, 10, e0242979. [Google Scholar] [CrossRef]
- Galluccio, G.; De Stefano, A.A.; Horodynski, M.; Impellizzeri, A.; Guarnieri, R.; Barbato, E.; Di Carlo, S.; De Angelis, F. Efficacy and Accuracy of Maxillary Arch Expansion with Clear Aligner Treatment. Int. J. Environ. Res. Public Health 2023, 20, 4634. [Google Scholar] [CrossRef]
- Deng, L.; Guo, Y. Estrogen effects on orthodontic tooth movement and orthodontically-induced root resorption. Arch. Oral Biol. 2020, 118, 104840. [Google Scholar] [CrossRef]
- Krishnan, V.; Kuijpers-Jagtman, A.M.; Davidovitch, Z. Biological Mechanisms of Tooth Movement, 3rd ed.; Willey Blackwell: Hoboken, NJ, USA, 2022; pp. 100–116. ISBN 9781119608936. [Google Scholar]
- Rossini, G.; Parrini, S.; Castroflorio, T.; Deregibus, A.; Debernardi, C.L. Efficacy of clear aligners in controlling orthodontic tooth movement: A systematic review. Angle Orthod. 2015, 85, 881–889. [Google Scholar] [CrossRef]
- Houle, J.P.; Piedade, L.; Todescan, R., Jr.; Pinheiro, F.H. The predictability of transverse changes with Invisalign. Angle Orthod. 2017, 87, 19–24. [Google Scholar] [CrossRef] [PubMed]
- Lione, R.; Paoloni, V.; Bartolommei, L.; Gazzani, F.; Meuli, S.; Pavoni, C.; Cozza, P. Maxillary arch development with Invisalign system. Angle Orthod. 2021, 91, 433–440. [Google Scholar] [CrossRef]
- Bucur, S.M.; Moga, R.A.; Olteanu, C.D.; Bud, E.S.; Vlasa, A. A Retrospective Study Regarding the Efficacy of Nuvola® OP Clear Aligners in Maxillary Arch Expansion in Adult Patients. Diagnostics 2025, 15, 738. [Google Scholar] [CrossRef] [PubMed]
- D’Antò, V.; Valletta, R.; Di Mauro, L.; Riccitiello, F.; Kirlis, R.; Rongo, R. The Predictability of Transverse Changes in Patients Treated with Clear Aligners. Materials 2023, 16, 1910. [Google Scholar] [CrossRef] [PubMed]
- Ma, S.; Wang, Y. Clinical outcomes of arch expansion with Invisalign: A systematic review. BMC Oral Health 2023, 23, 587. [Google Scholar] [CrossRef]
- Kalekar, A.A.; Manchanda, J.; Chavan, S.; Bhad, W.A.; Atram, H.; Badu, P.; Tarde, P. Effectiveness of maxillary arch expansion using clear aligners in adult patients: A systematic review and meta-analysis. Aust. Orthod. J. 2024, 40, 111–129. [Google Scholar] [CrossRef]
- Riede, U.; Wai, S.; Neururer, S.; Reistenhofer, B.; Riede, G.; Besser, K.; Crismani, A. Maxillary expansion or contraction and occlusal contact adjustment: Effectiveness of current aligner treatment. Clin. Oral Investig. 2021, 25, 4671–4679. [Google Scholar] [CrossRef]
- Papadimitriou, A.; Mousoulea, S.; Gkantidis, N.; Kloukos, D. Clinical effectiveness of Invisalign® orthodontic treatment: A systematic review. Prog. Orthod. 2018, 28, 37. [Google Scholar] [CrossRef]
- Charalampakis, O.; Iliadi, A.; Ueno, H.; Oliver, D.R.; Kim, K.B. Accuracy of clear aligners: A retrospective study of patients who needed refinement. Am. J. Orthod. Dentofac. Orthop. 2018, 154, 47–54. [Google Scholar] [CrossRef]
- Ali, S.A.; Miethke, H.R. Invisalign, an innovative invisible orthodontic appliance to correct malocclusions: Advantages and limitations. Dent. Update 2012, 39, 258–260. [Google Scholar] [CrossRef] [PubMed]
- Castroflorio, T.; Sedran, A.; Parrini, S.; Garino, F.; Reverdito, M.; Capuozzo, R.; Mutinelli, S.; Grybauskas, S.; Vaitiekūnas, M.; Deregibus, A. Predictability of orthodontic tooth movement with aligners: Effect of treatment design. Prog. Orthod. 2023, 16, 2. [Google Scholar] [CrossRef]
- Nucera, R.; Dolci, C.; Bellocchio, A.M.; Costa, S.; Barbera, S.; Rustico, L.; Farronato, M.; Militi, A.; Portelli, M. Effects of Composite Attachments on Orthodontic Clear Aligners Therapy: A Systematic Review. Materials 2022, 15, 533. [Google Scholar] [CrossRef]
- Nogal-Coloma, A.; Yeste-Ojeda, F.; Rivero-Lesmes, J.C.; Martin, C. Predictability of Maxillary Dentoalveolar Expansion Using Clear Aligners in Different Types of Crossbites. Appl. Sci. 2023, 13, 2963. [Google Scholar] [CrossRef]
- Al-Nadawi, M.; Kravitz, N.D.; Hansa, I.; Makki, L.; Ferguson, D.J.; Vaid, N.R. Effect of clear aligner wear protocol on the efficacy of tooth movement. Angle Orthod. 2021, 91, 157–163. [Google Scholar] [CrossRef] [PubMed]
- O’Connor, J.; Weir, T.; Freer, E.; Kerr, B. Clinical expression of programmed maxillary buccal expansion and buccolingual crown inclination with Invisalign EX30 and SmartTrack aligners and the effect of 1-week vs. 2-week aligner change regimes: A retrospective cohort study. Korean J. Orthod. 2024, 54, 142–152. [Google Scholar] [CrossRef]
- Dudic, A.; Giannopoulou, C.; Leuzinger, M.; Kiliaridis, S. Detection of apical root resorption after orthodontic treatment by using panoramic radiography and cone-beam computed tomography of super-high resolution. Am. J. Orthod. Dentofac. Orthop. 2009, 135, 434–437. [Google Scholar] [CrossRef]
- Deng, Y.; Sun, Y.; Xu, T. Evaluation of root resorption after comprehensive orthodontic treatment using cone beam computed tomography (CBCT): A meta-analysis. BMC Oral Health 2018, 18, 116. [Google Scholar] [CrossRef]
- Mallya, S.M.; Lam, E.W.N. White and Pharoah’s Oral Radiology, 8th ed.; Mosby Inc.: St. Louis, MO, USA, 2018; pp. 377–435. ISBN 9780323543835. [Google Scholar]
- Venkatesh, E.; Elluru, S.V. Cone beam computed tomography: Basics and applications in dentistry. J. Istanb. Univ. Fac. Dent. 2017, 51, S102–S121. [Google Scholar] [CrossRef]
- Lombardo, L.; Palone, M.; Longo, M.; Arveda, N.; Nacucchi, M.; De Pascalis, F.; Spedicato, G.A.; Siciliani, G. MicroCT X-Ray Comparison of Aligner Gap and Thickness of Six Brands of Aligners: An in-Vitro Study. Prog. Orthod. 2020, 21, 12. [Google Scholar] [CrossRef]
- Chisari, J.R.; McGorray, S.P.; Nair, M.; Wheeler, T.T. Variables affecting orthodontic tooth movement with clear aligners. Am. J. Orthod. Dentofac. Orthop. 2014, 145, 82–91. [Google Scholar] [CrossRef] [PubMed]


| Maxillary Linear Width | T1-T0 (mm) (Mean ± SD) | T1-T0 Minimum–Maximum Values (mm) | T1-T0 (%) (Mean ± SD) | T1-T0 Minimum–Maximum Values (%) | p-Value |
|---|---|---|---|---|---|
| Alveolar bone | 0.09 ± 0.22 | 0–1.20 | 0.14 ± 0.39 | 0–2.04 | 0.009 * |
| Buccal alveolar ridge | 1.01 ± 0.38 | 0.30–2.80 | 1.80 ± 0.69 | 0.53 ± 5.03 | 2.83857 × 10−24 ** |
| Palatal alveolar ridge | 0.81 ± 0.37 | 0–1.30 | 2.24 ± 1.04 | 0–4.05 | 2.08145 × 10−20 ** |
| Inter-Apex Width | T1-T0 (mm) (Mean ± SD) | T1-T0 Minimum–Maximum Values (mm) | T1-T0 (%) (Mean ± SD) | T1-T0 Minimum–Maximum Values (%) | p-Value |
|---|---|---|---|---|---|
| Intercanine | 1.31 ± 0.73 | 0.10–2.50 | 4.39 ± 2.43 | 0.34–8.39 | 5.84596 × 10−17 ** |
| First interpremolar | 1.89 ± 0.39 | 0.7–2.6 | 5.18 ± 1.11 | 1.93–7.22 | 1.07006 × 10−35 ** |
| Second interpremolar | 1.48 ± 0.68 | 0.10–2.60 | 3.53 ± 1.63 | 0.24–6.15 | 2.33339 × 10−20 ** |
| First intermolar | 0.70 ± 0.26 | 0.10–1.20 | 1.40 ± 0.53 | 0.20–2.41 | 4.20634 × 10−24 ** |
| Second intermolar | 0.15 ± 0.09 | 0–0.40 | 0.29 ± 0.17 | 0–0.77 | 2.28014 × 10−16 ** |
| Inter-Cusp Width | T1-T0 (mm) (Mean ± SD) | T1-T0 Minimum–Maximum Values (mm) | T1-T0 (%) (Mean ± SD) | T1-T0 Minimum–Maximum Values (%) | p-Value |
|---|---|---|---|---|---|
| Intercanine | 2.32 ± 0.33 | 1.40–3.60 | 7.37 ± 1.11 | 4.18–11.76 | 2.39215 × 10−43 ** |
| First interpremolar | 3.44 ± 0.22 | 3.10–3.90 | 8.65 ± 0.60 | 7.71–10.13 | 1.1346 × 10−60 ** |
| Second interpremolar | 3.14 ± 0.27 | 2.70–3.60 | 6.94 ± 0.65 | 5.71–8.13 | 5.72304 × 10−54 ** |
| First intermolar | 2.60 ± 0.52 | 0.40–3.40 | 5.74 ± 1.19 | 0.90–7.64 | 1.4256 × 10−35 ** |
| Second intermolar | 0.70 ± 0.28 | 0.10–1.80 | 1.24 ± 0.51 | 0.18–3.24 | 1.2904 × 10−22 ** |
| Source | Sum of Squares | Degrees of Freedom | Mean Square | F | p-Value |
|---|---|---|---|---|---|
| Between groups | 94.1761567 | 4 | 23.5440392 | 95.36 | <0.001 |
| Within groups | 60.4889981 | 245 | 0.24689387 | ||
| Total | 154.665155 | 249 | 0.6211452 |
| Inter-Apex Width | Contrast | Standard Error | t Test | p-Value > |t| | [95% Confidence Interval] | |
|---|---|---|---|---|---|---|
| Tooth type | ||||||
| First premolar vs. canine | 0.586 | 0.0993768 | 5.90 | <0.001 | 0.3128924 | 0.8591075 |
| Second premolar vs. canine | 0.174 | 0.0993768 | 1.75 | 0.405 | 0.0991075 | 0.4471075 |
| First molar vs. canine | 0.61 | 0.0993768 | 6.14 | <0.001 | 0.8831075 | 0.3368925 |
| Second molar vs. canine | 1.158 | 0.0993768 | 11.65 | <0.001 | 1.431108 | 0.8848925 |
| Second premolar vs. first premolar | 0.412 | 0.0993768 | 4.15 | <0.001 | 0.6851075 | 0.1388924 |
| First molar vs. first premolar | 1.196 | 0.0993768 | 12.03 | <0.001 | 1.469108 | 0.9228924 |
| Second molar vs. first premolar | 1.744 | 0.0993768 | 17.55 | <0.001 | 2.017108 | 1.470892 |
| First molar vs. second premolar | 0.784 | 0.0993768 | 7.89 | <0.001 | 1.057108 | 0.5108924 |
| Second molar vs. second premolar | 1.332 | 0.0993768 | 13.40 | <0.001 | 1.605108 | 1.058892 |
| Second molar vs. first molar | 0.548 | 0.0993768 | 5.51 | <0.001 | 0.8211075 | 0.2748925 |
| Source | Sum of Squares | Degrees of Freedom | Mean Square | F | p-Value |
|---|---|---|---|---|---|
| Between groups | 227.96456 | 4 | 56.9911399 | 487.29 | <0.001 |
| Within groups | 28.6542002 | 245 | 0.116955919 | ||
| Total | 256.61876 | 249 | 1.03059743 |
| Inter-Cusp Width | Contrast | Standard Error | t Test | p-Value > |t| | [95% Confidence Interval] | |
|---|---|---|---|---|---|---|
| Tooth type | ||||||
| First premolar vs. canine | 1.118 | 0.0683976 | 16.35 | <0.001 | 0.9300295 | 1.30597 |
| Second premolar vs. canine | 0.82 | 0.0683976 | 11.99 | <0.001 | 0.6320295 | 1.00797 |
| First molar vs. canine | 0.276 | 0.0683976 | 4.04 | 0.001 | 0.0880295 | 0.4639705 |
| Second molar vs. canine | 1.622 | 0.0683976 | 23.71 | <0.001 | 1.80997 | 1.43403 |
| Second premolar vs. first premolar | 0.298 | 0.0683976 | 4.36 | <0.001 | 0.4859705 | 0.1100295 |
| First molar vs. first premolar | 0.842 | 0.0683976 | 12.31 | <0.001 | 1.02997 | 0.6540295 |
| Second molar vs. first premolar | 2.74 | 0.0683976 | 40.06 | <0.001 | 2.92797 | 2.55203 |
| First molar vs. second premolar | 0.544 | 0.0683976 | 7.95 | <0.001 | 0.7319705 | 0.3560295 |
| Second molar vs. second premolar | 2.442 | 0.0683976 | 35.70 | <0.001 | 2.62997 | 2.25403 |
| Second molar vs. first molar | 1.898 | 0.0683976 | 27.75 | <0.001 | 2.08597 | 1.71003 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Macrì, M.; Medori, S.; Festa, F. Evaluation of Maxillary Dentoalveolar Expansion with Clear Aligners: A Retrospective CBCT Study. Diagnostics 2025, 15, 1586. https://doi.org/10.3390/diagnostics15131586
Macrì M, Medori S, Festa F. Evaluation of Maxillary Dentoalveolar Expansion with Clear Aligners: A Retrospective CBCT Study. Diagnostics. 2025; 15(13):1586. https://doi.org/10.3390/diagnostics15131586
Chicago/Turabian StyleMacrì, Monica, Silvia Medori, and Felice Festa. 2025. "Evaluation of Maxillary Dentoalveolar Expansion with Clear Aligners: A Retrospective CBCT Study" Diagnostics 15, no. 13: 1586. https://doi.org/10.3390/diagnostics15131586
APA StyleMacrì, M., Medori, S., & Festa, F. (2025). Evaluation of Maxillary Dentoalveolar Expansion with Clear Aligners: A Retrospective CBCT Study. Diagnostics, 15(13), 1586. https://doi.org/10.3390/diagnostics15131586






