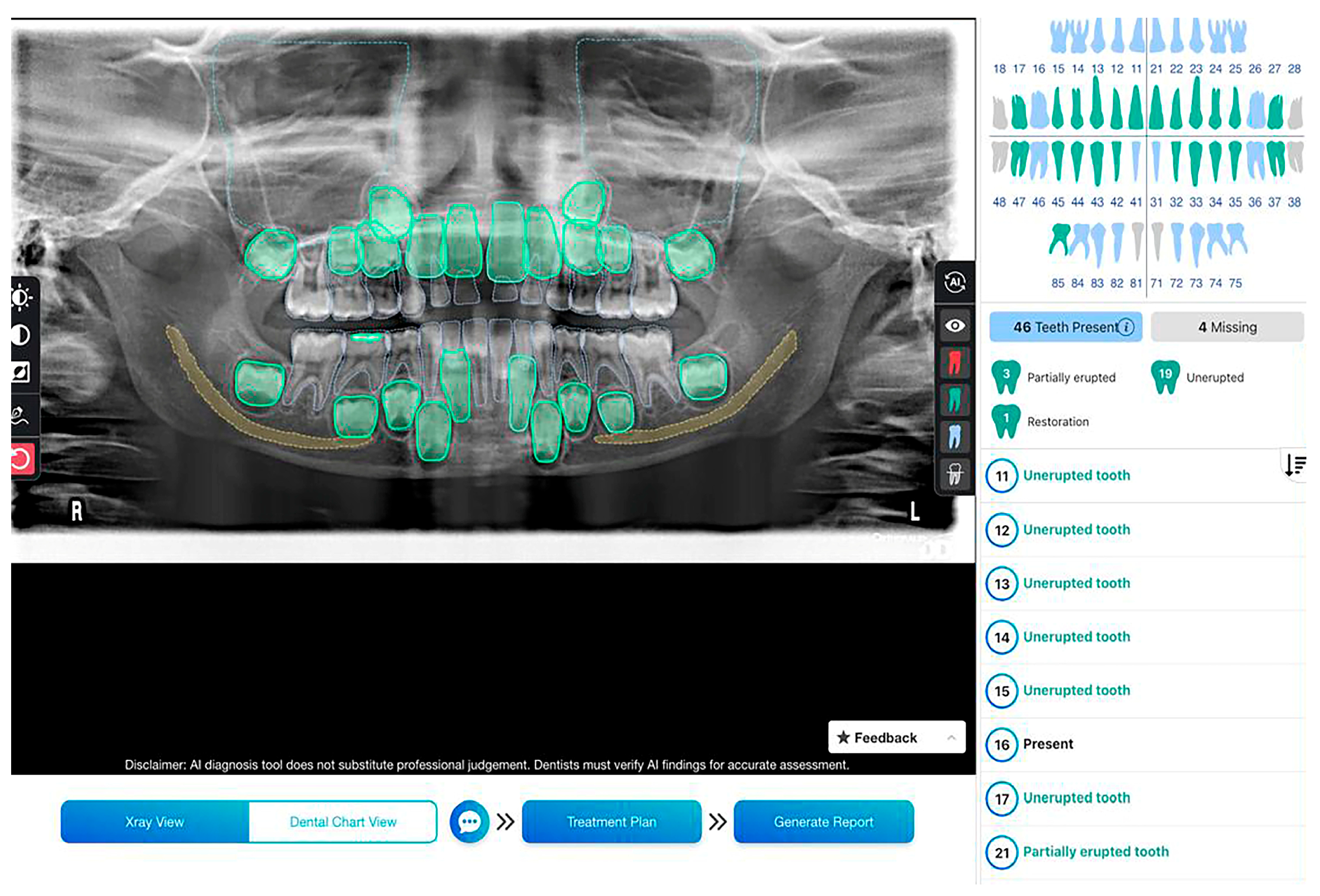
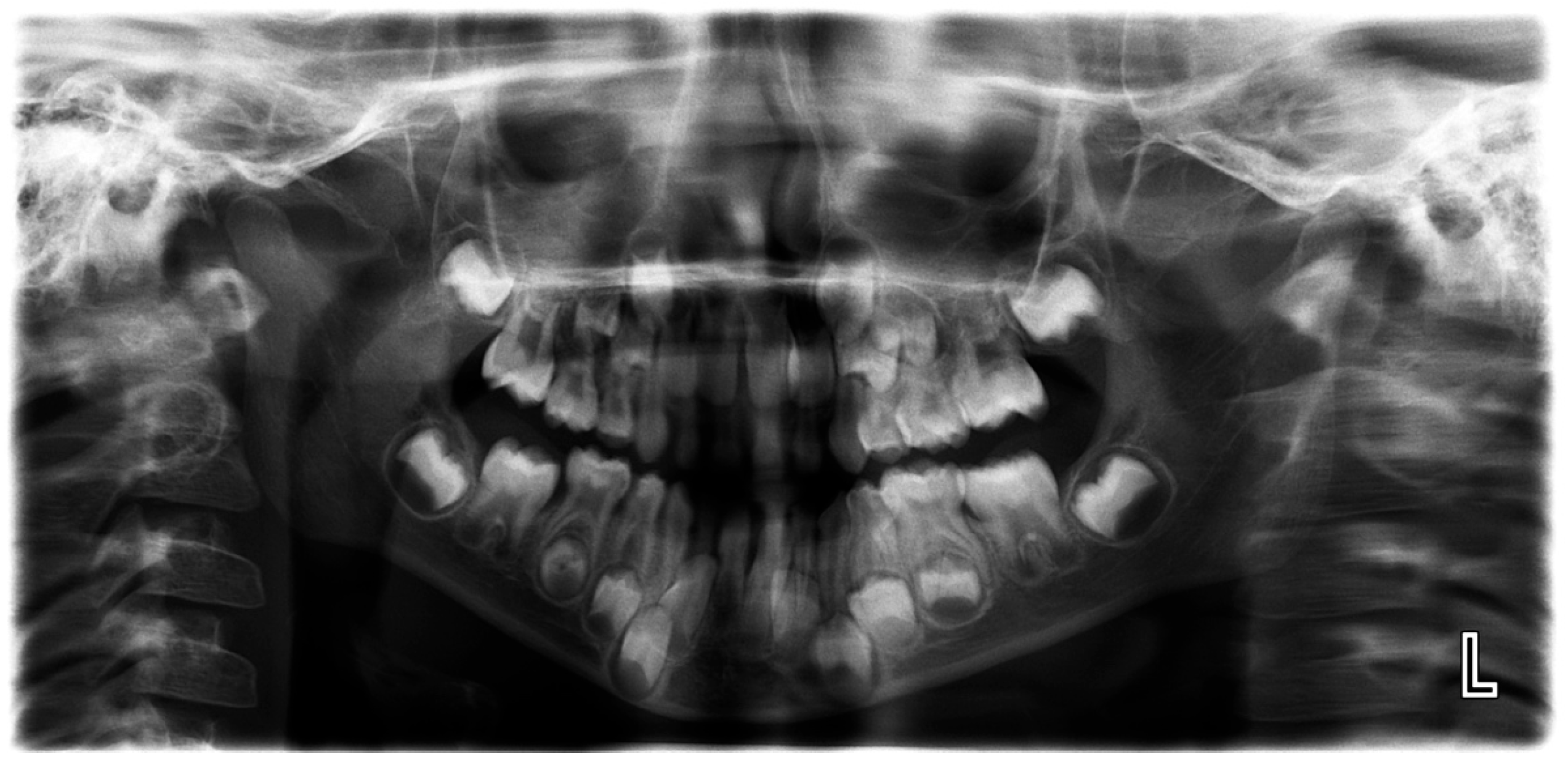
The Validation of an Artificial Intelligence-Based Software for the Detection and Numbering of Primary Teeth on Panoramic Radiographs
Abstract
1. Introduction
2. Materials and Methods
Statistical Analysis
3. Results
3.1. Upper Primary Anterior Teeth
3.2. Upper Primary Molars
3.3. Lower Primary Anterior Teeth
3.4. Lower Primary Molars
3.5. Overall Evaluation of Primary Teeth Detection
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Shan, T.; Tay, F.R.; Gu, L. Application of Artificial Intelligence in Dentistry. J. Dent. Res. 2021, 100, 232–244. [Google Scholar] [CrossRef]
- FDI World Dental Federation. Artificial intelligence in dentistry. Int. Dent. J. 2025, 75, 3–4. [Google Scholar] [CrossRef] [PubMed]
- Schwendicke, F.; Chaurasia, A.; Wiegand, T.; Uribe, S.E.; Fontana, M.; Akota, I.; Tryfonos, O.; Krois, J. Artificial intelligence for oral and dental healthcare: Core education curriculum. J. Dent. 2023, 128, 104363. [Google Scholar] [CrossRef] [PubMed]
- Schwendicke, F.; Samek, W.; Krois, J. Artificial Intelligence in Dentistry: Chances and Challenges. J. Dent. Res. 2020, 99, 769–774. [Google Scholar] [CrossRef] [PubMed]
- Evangelista, K.; de Freitas Silva, B.S.; Yamamoto-Silva, F.P.; Valladares-Neto, J.; Silva, M.A.G.; Soares Cevidanes, L.H.; de Luca Canto, G.; Massignan, C. Accuracy of artificial intelligence for tooth extraction decision-making in orthodontics: A systematic review and meta-analysis. Clin. Oral Investig. 2022, 26, 6893–6905. [Google Scholar] [CrossRef]
- Hwang, J.J.; Jung, Y.H.; Cho, B.H.; Heo, M.S. An overview of deep learning in the field of dentistry. Imaging Sci. Dent. 2019, 49, 1–7. [Google Scholar] [CrossRef]
- Krishna, A.B.; Tanveer, A.; Bhagirath, P.V.; Gannepalli, A. Role of artificial intelligence in diagnostic oral pathology—A modern approach. J. Oral Maxillofac. Pathol. 2020, 24, 152–156. [Google Scholar] [CrossRef]
- Revilla-León, M.; Gómez-Polo, M.; Vyas, S.; Barmak, B.A.; Galluci, G.O.; Att, W.; Krishnamurthy, V.R. Artificial intelligence applications in implant dentistry: A systematic review. J. Prosthet. Dent. 2023, 129, 293–300. [Google Scholar] [CrossRef]
- Rajinikanth, S.; Rajkumar, D.; Rajinikanth, A.; Anandhapandian, P. An overview of artificial intelligence based automated di-agnosis in paediatric dentistry. Front. Oral Health 2024, 5, 1482334. [Google Scholar] [CrossRef]
- Vishwanathaiah, S.; Fageeh, H.N.; Khanagar, S.B.; Maganur, P.C. Artificial Intelligence Its Uses and Application in Pediatric Dentistry: A Review. Biomedicines 2023, 11, 788. [Google Scholar] [CrossRef]
- Kosan, E.; Krois, J.; Wingenfeld, K.; Deuter, C.E.; Gaudin, R.; Schwendicke, F. Patients’ Perspectives on Artificial Intelligence in Dentistry: A Controlled Study. J. Clin. Med. 2022, 11, 2143. [Google Scholar] [CrossRef] [PubMed]
- Bahadir, H.S.; Keskin, N.B.; Çakmak, E.Ş.K.; Güneç, G.; Cesur Aydin, K.; Peker, F. Patients’ attitudes toward artificial intelli-gence in dentistry and their trust in dentists. Oral Radiol. 2025, 41, 52–59. [Google Scholar] [CrossRef] [PubMed]
- Patil, S.; Albogami, S.; Hosmani, J.; Mujoo, S.; Kamil, M.A.; Mansour, M.A.; Abdul, H.N.; Bhandi, S.; Ahmed, S.S.S.J. Artificial Intelligence in the Diagnosis of Oral Diseases: Applications and Pitfalls. Diagnostics 2022, 12, 1029. [Google Scholar] [CrossRef] [PubMed]
- Alessa, N. Application of Artificial Intelligence in Pediatric Dentistry: A Literature Review. J. Pharm. Bioallied Sci. 2024, 16 (Suppl. S3), S1938–S1940. [Google Scholar] [CrossRef]
- Anthonappa, R.P.; King, N.M.; Rabie, A.B.; Mallineni, S.K. Reliability of panoramic radiographs for identifying supernumerary teeth in children. Int. J. Paediatr. Dent. 2012, 22, 37–43. [Google Scholar] [CrossRef]
- Ahn, Y.; Hwang, J.J.; Jung, Y.H.; Jeong, T.; Shin, J. Automated Mesiodens Classification System Using Deep Learning on Pan-oramic Radiographs of Children. Diagnostics 2021, 11, 1477. [Google Scholar] [CrossRef]
- Reis, J.C.; Fraga, M.A.A.; DeAzevedo-Vaz, S.L.; Miotto, M.H.M.B.; Perreira, T.C.R. Alterations in Panoramic Radiographies in Children. RGO, Rev. Gaúch. Odontol. 2020, 68, e20200073. [Google Scholar] [CrossRef]
- Choi, J.W. Assessment of panoramic radiography as a national oral examination tool: Review of the literature. Imaging Sci. Dent. 2011, 41, 1–6. [Google Scholar] [CrossRef]
- Rozyło-Kalinowska, I. Panoramic radiography in dentistry. Clin. Dent. Rev. 2021, 5, 26. [Google Scholar] [CrossRef]
- Cohnen, M.; Kemper, J.; Möbes, O.; Pawelzik, J.; Mödder, U. Radiation dose in dental radiology. Eur. Radiol. 2002, 12, 634–637. [Google Scholar] [CrossRef]
- Bonny, T.; Al Nassan, W.; Obaideen, K.; Al Mallahi, M.N.; Mohammad, Y.; El-Damanhoury, H.M. Contemporary Role and Applications of Artificial Intelligence in Dentistry. F1000Research 2023, 12, 1179. [Google Scholar] [CrossRef] [PubMed]
- Ahmed, N.; Abbasi, M.S.; Zuberi, F.; Qamar, W.; Halim, M.S.B.; Maqsood, A.; Alam, M.K. Artificial Intelligence Techniques: Analysis, Application, and Outcome in Dentistry—A Systematic Review. Biomed. Res. Int. 2021, 2021, 9751564. [Google Scholar] [CrossRef] [PubMed]
- Revilla-León, M.; Gómez-Polo, M.; Vyas, S.; Barmak, A.B.; Özcan, M.; Att, W.; Krishnamurthy, V.R. Artificial intelligence applications in restorative dentistry: A systematic review. J. Prosthet. Dent. 2022, 128, 867–875. [Google Scholar] [CrossRef] [PubMed]
- Alharbi, S.S.; Alhasson, H.F. Exploring the Applications of Artificial Intelligence in Dental Image Detection: A Systematic Review. Diagnostics 2024, 14, 2442. [Google Scholar] [CrossRef]
- Ding, H.; Wu, J.; Zhao, W.; Matinlinna, J.P.; Burrow, M.F.; Tsoi, J.K.H. Artificial intelligence in dentistry—A review. Front. Dent. Med. 2023, 4, 1085251. [Google Scholar] [CrossRef]
- Mallineni, S.K.; Sethi, M.; Punugoti, D.; Kotha, S.B.; Alkhayal, Z.; Mubaraki, S.; Almotawah, F.N.; Kotha, S.L.; Sajja, R.; Nettam, V. Artificial Intelligence in Dentistry: A Descriptive Review. Bioengineering 2024, 11, 1267. [Google Scholar] [CrossRef]
- Alam, M.K.; Alftaikhah, S.A.A.; Issrani, R.; Ronsivalle, V.; Giudice, A.L.; Cicciù, M.; Minervini, G. Applications of artificial intelligence in the utilisation of imaging modalities in dentistry: A systematic review and meta-analysis of in-vitro studies. Heliyon 2024, 10, e24221. [Google Scholar] [CrossRef]
- Morch, C.M.; Atsu, S.; Cai, W.; Madathil, C.A.; Liu, X.; Mai, V.; Tamimi, F.; Dilhac, M.A.; Ducret, M. Artificial Intelligence and Ethics in Dentistry: A Scoping Review. J. Dent. Res. 2021, 100, 1452–1460. [Google Scholar] [CrossRef]
- Thorat, V.; Rao, P.; Joshi, N.; Talreja, P.; Shetty, A.R. Role of Artificial Intelligence (AI) in Patient Education and Communication in Dentistry. Cureus 2024, 16, e59799. [Google Scholar] [CrossRef]
- Jeyaraman, M.; Balaji, S.; Jeyaraman, N.; Yadav, S. Unraveling the Ethical Enigma: Artificial Intelligence in Healthcare. Cureus 2023, 15, e43262. [Google Scholar] [CrossRef]
- Leite, A.F.; Gerven, A.V.; Willems, H. Artificial intelligence-driven novel tool for tooth detection and segmentation on pano-ramic radiographs. Clin. Oral Investig. 2021, 25, 2257–2267. [Google Scholar] [CrossRef] [PubMed]
- Turosz, N.; Chęcińska, K.; Chęciński, M.; Sielski, M.; Sikora, M. Evaluation of Dental Panoramic Radiographs by Artificial Intelligence Compared to Human Reference: A Diagnostic Accuracy Study. J. Clin. Med. 2024, 13, 6859. [Google Scholar] [CrossRef] [PubMed]
- Güneç, H.G.; Ürkmez, E.Ş.; Danaci, A.; Dilmaç, E.; Onay, H.H.; Cesur Aydin, K. Comparison of artificial intelligence vs. junior dentists’ diagnostic performance based on caries and periapical infection detection on panoramic images. Quant. Imaging Med. Surg. 2023, 13, 7494–7503. [Google Scholar] [CrossRef] [PubMed]
- Jaiswal, M.; Sharma, M.; Khandnor, P. Deep learning models for classification of deciduous and permanent teeth from digital panoramic images. Cureus 2023, 15, e49937. [Google Scholar] [CrossRef]


| Sensitivity | The proportion of the testing method’s true positive results to the reference method’s all positive results. |
| Specificity | The proportion of the testing method’s true negative results to the reference method’s all negative results. |
| Positive Predictive Value (PPV) | The proportion of positive test results that are actually positive according to the reference method to total test positive results. |
| Negative Predictive Value (NPV) | The proportion of negative test results that are actually negative according to the reference method to total test negative results. |
| Test accuracy | The proportion of the number of true test results to all test results. |
| Kappa coefficient of agreement | Measures the degree of agreement accounting for the fact that the two methods may happen to agree on some cases by pure chance. |
| Tooth Number | Sensitivity | Specificity | PPV | NPV | Accuracy |
|---|---|---|---|---|---|
| 53 | 0.99 | 0.97 | 0.99 | 0.95 | 0.98 |
| 52 | 0.91 | 0.99 | 0.98 | 0.97 | 0.97 |
| 51 | 0.89 | 0.99 | 0.94 | 0.98 | 0.98 |
| 61 | 0.93 | 0.99 | 0.95 | 0.99 | 0.98 |
| 62 | 0.93 | 0.99 | 0.97 | 0.98 | 0.98 |
| 63 | 0.97 | 0.98 | 0.99 | 0.90 | 0.97 |
| Tooth Number | Sensitivity | Specificity | PPV | NPV | Accuracy |
|---|---|---|---|---|---|
| 55 | 0.99 | 0.98 | 1.00 | 0.96 | 0.99 |
| 54 | 0.98 | 0.97 | 0.98 | 0.97 | 0.98 |
| 64 | 0.97 | 0.99 | 0.99 | 0.96 | 0.98 |
| 65 | 0.98 | 0.98 | 0.99 | 0.94 | 0.98 |
| Tooth Number | Sensitivity | Specificity | PPV | NPV | Accuracy |
|---|---|---|---|---|---|
| 73 | 0.97 | 0.98 | 0.99 | 0.94 | 0.97 |
| 72 | 0.88 | 0.99 | 0.97 | 0.98 | 0.98 |
| 71 | 0.83 | 1.00 | 0.91 | 0.99 | 0.99 |
| 81 | 0.87 | 0.99 | 0.87 | 0.99 | 0.99 |
| 82 | 0.83 | 0.99 | 0.94 | 0.97 | 0.96 |
| 83 | 0.97 | 0.96 | 0.98 | 0.95 | 0.97 |
| Tooth Number | Sensitivity | Specificity | PPV | NPV | Accuracy |
|---|---|---|---|---|---|
| 75 | 0.98 | 0.98 | 0.99 | 0.96 | 0.98 |
| 74 | 0.97 | 0.98 | 0.99 | 0.95 | 0.97 |
| 84 | 0.99 | 0.98 | 0.99 | 0.98 | 0.98 |
| 85 | 0.99 | 1.00 | 1.00 | 0.96 | 0.99 |
| Tooth Number | Sensitivity | Specificity | PPV | NPV | Accuracy |
|---|---|---|---|---|---|
| Upper primary incisors | 0.92 | 0.99 | 0.97 | 0.98 | 0.98 |
| Upper primary canines | 0.98 | 0.97 | 0.99 | 0.92 | 0.98 |
| Upper primary molars | 0.98 | 0.98 | 0.99 | 0.96 | 0.98 |
| Lower primary incisors | 0.85 | 0.99 | 0.94 | 0.98 | 0.98 |
| Lower primary canines | 0.97 | 0.98 | 0.99 | 0.94 | 0.97 |
| Lower primary molars | 0.98 | 0.98 | 0.99 | 0.96 | 0.98 |
| All primary teeth | 0.97 | 0.99 | 0.99 | 0.97 | 0.98 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bakhsh, H.H.; Alomair, D.; AlShehri, N.A.; Alturki, A.U.; Allam, E.; ElKhateeb, S.M. The Validation of an Artificial Intelligence-Based Software for the Detection and Numbering of Primary Teeth on Panoramic Radiographs. Diagnostics 2025, 15, 1489. https://doi.org/10.3390/diagnostics15121489
Bakhsh HH, Alomair D, AlShehri NA, Alturki AU, Allam E, ElKhateeb SM. The Validation of an Artificial Intelligence-Based Software for the Detection and Numbering of Primary Teeth on Panoramic Radiographs. Diagnostics. 2025; 15(12):1489. https://doi.org/10.3390/diagnostics15121489
Chicago/Turabian StyleBakhsh, Heba H., Dur Alomair, Nada Ahmed AlShehri, Alia U. Alturki, Eman Allam, and Sara M. ElKhateeb. 2025. "The Validation of an Artificial Intelligence-Based Software for the Detection and Numbering of Primary Teeth on Panoramic Radiographs" Diagnostics 15, no. 12: 1489. https://doi.org/10.3390/diagnostics15121489
APA StyleBakhsh, H. H., Alomair, D., AlShehri, N. A., Alturki, A. U., Allam, E., & ElKhateeb, S. M. (2025). The Validation of an Artificial Intelligence-Based Software for the Detection and Numbering of Primary Teeth on Panoramic Radiographs. Diagnostics, 15(12), 1489. https://doi.org/10.3390/diagnostics15121489






