Cone Beam Computed Tomography in Oral Cancer: A Scoping Review
Abstract
1. Introduction
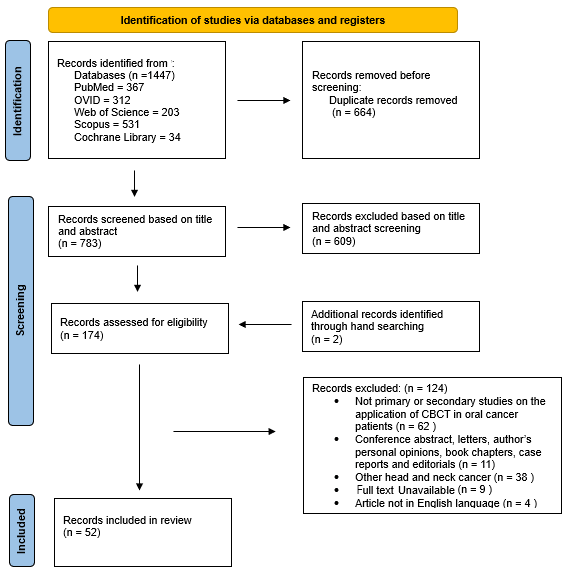
2. Materials and Methods
2.1. Protocol and Registration
2.2. Research Question
2.3. Identification of Relevant Studies
2.4. Study Selection
2.5. Data Extraction
3. Results
3.1. Imaging in Radiotherapy Treatment
3.2. Bone Invasion Assessment
3.3. Intraoperative Surgical Guidance
3.4. Complication Assessment
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| CBCT | Cone beam computed tomography |
| OPG | Orthopantomogram |
| MRI | Magnetic resonance imaging |
| TMJ | Temporomandibular joint |
| CT | Computed tomography |
| IGRT | Image-guided radiation therapy |
| SPECT | Single-photon emission CT |
| ART | Adaptive radiation therapy |
| LINAC | Linear accelerator |
| EPIDs | Electronic portal imaging devices |
| CAS | Computer-assisted surgery |
| ORN | Osteoradionecrosis |
References
- Mozzo, P.; Procacci, C.; Tacconi, A.; Martini, P.T.; Andreis, I.A. A new volumetric CT machine for dental imaging based on the cone-beam technique: Preliminary results. Eur. Radiol. 1998, 8, 1558–1564. [Google Scholar] [CrossRef] [PubMed]
- Lam, M.; Critchley, S.; Zhang, A.; Monsour, P. Current trends in the adoption and education of cone beam computed tomography and panoramic radiography machines across Australia. Dentomaxillofac. Radiol. 2021, 50, 20200380. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Scarfe, W.C.; Farman, A.G. What is cone-beam CT and how does it work? Dent. Clin. N. Am. 2008, 52, 707–730. [Google Scholar] [CrossRef] [PubMed]
- Bray, F.; Ferlay, J.; Soerjomataram, I.; Siegel, R.L.; Torre, L.A.; Jemal, A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J. Clin. 2018, 68, 394–424. [Google Scholar] [CrossRef]
- Güneri, P.; Epstein, J.B. Late stage diagnosis of oral cancer: Components and possible solutions. Oral Oncol. 2014, 50, 1131–1136. [Google Scholar] [CrossRef] [PubMed]
- Köhler, H.F.; Mehanna, H.; Shah, J.P.; Sanabria, A.; Fagan, J.; Kuriakose, M.A.; Rene Leemans, C.; O’Sullivan, B.; Krishnan, S.; Kowalski, L.P. Comparison of different guidelines for oral cancer. Eur. Arch. Otorhinolaryngol. 2021, 278, 2961–2973. [Google Scholar] [CrossRef] [PubMed]
- Zanoni, D.K.; Montero, P.H.; Migliacci, J.C.; Shah, J.P.; Wong, R.J.; Ganly, I.; Patel, S.G. Survival outcomes after treatment of cancer of the oral cavity (1985–2015). Oral Oncol. 2019, 90, 115–121. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Nasseh, I.; Al-Rawi, W. Cone Beam Computed Tomography. Dent. Clin. N. Am. 2018, 62, 361–391. [Google Scholar] [CrossRef] [PubMed]
- Kamburoğlu, K. Use of dentomaxillofacial cone beam computed tomography in dentistry. World J. Radiol. 2015, 7, 128–130. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Scarfe, W.C.; Toghyani, S.; Azevedo, B. Imaging of Benign Odontogenic Lesions. Radiol. Clin. N. Am. 2018, 56, 45–62. [Google Scholar] [CrossRef] [PubMed]
- Luo, J.; You, M.; Zheng, G.; Xu, L. Cone beam computed tomography signs of desmoplastic ameloblastoma: Review of 7 cases. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. 2014, 118, e126–e133. [Google Scholar] [CrossRef] [PubMed]
- Treister, N.S.; Friedland, B.; Woo, S.B. Use of cone-beam computerized tomography for evaluation of bisphosphonate-associated osteonecrosis of the jaws. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 2010, 109, 753–764. [Google Scholar] [CrossRef] [PubMed]
- Peters, M.D.J.; Marnie, C.; Tricco, A.C.; Pollock, D.; Munn, Z.; Alexander, L.; McInerney, P.; Godfrey, C.M.; Khalil, H. Updated methodological guidance for the conduct of scoping reviews. JBI Evid. Synth. 2020, 18, 2119–2126. [Google Scholar] [CrossRef] [PubMed]
- Lip and Oral Cavity Cancer Treatment (PDQ®). Available online: https://www.cancer.gov/types/head-and-neck/hp/adult/lip-mouth-treatment-pdq (accessed on 5 March 2024).
- Cheung, J.; Aubry, J.F.; Yom, S.S.; Gottschalk, A.R.; Celi, J.C.; Pouliot, J. Dose Recalculation and the Dose-Guided Radiation Therapy (DGRT) Process Using Megavoltage Cone-Beam CT. Int. J. Radiat. Oncol. Biol. Phys. 2009, 74, 583–592. [Google Scholar] [CrossRef]
- Den, R.B.; Doemer, A.; Kubicek, G.; Bednarz, G.; Galvin, J.M.; Keane, W.M.; Xiao, Y.; Machtay, M. Daily image guidance with cone-beam computed tomography for head-and-neck cancer intensity-modulated radiotherapy: A prospective study. Int. J. Radiat. Oncol. Biol. Phys. 2010, 76, 1353–1359. [Google Scholar] [CrossRef]
- Yan, D.; Liang, J. Expected treatment dose construction and adaptive inverse planning optimization: Implementation for offline head and neck cancer adaptive radiotherapy. Med. Phys. 2013, 40, 021719. [Google Scholar] [CrossRef]
- Hermans, B.C.M.; Persoon, L.C.G.G.; Podesta, M.; Hoebers, F.J.P.; Verhaegen, F.; Troost, E.G.C. Weekly kilovoltage cone-beam computed tomography for detection of dose discrepancies during (chemo)radiotherapy for head and neck cancer. Acta Oncol. 2015, 54, 1483–1489. [Google Scholar] [CrossRef]
- Hvid, C.A.; Elstrøm, U.V.; Jensen, K.; Alber, M.; Grau, C. Accuracy of software-assisted contour propagation from planning CT to cone beam CT in head and neck radiotherapy. Acta Oncol. 2016, 55, 1324–1330. [Google Scholar] [CrossRef]
- Hofmaier, J.; Haehnle, J.; Kurz, C.; Landry, G.; Maihoefer, C.; Schüttrumpf, L.; Süss, P.; Teichert, K.; Söhn, M.; Spahr, N.; et al. Multi-criterial patient positioning based on dose recalculation on scatter-corrected CBCT images. Radiother. Oncol. 2017, 125, 464–469. [Google Scholar] [CrossRef]
- Norfadilah, M.N.; Ahmad, R.; Heng, S.P.; Lam, K.S.; Radzi, A.; John, L.S.H. Immobilisation precision in VMAT for oral cancer patients. J. Phys. Conf. Ser. 2017, 851, 012025. [Google Scholar] [CrossRef]
- Brivio, D.; Hu, Y.D.; Margalit, D.N.; Zygmanski, P. Selection of head and neck cancer patients for adaptive replanning of radiation treatment using kV-CBCT. Biomed. Phys. Eng. Express 2018, 4, 055009. [Google Scholar] [CrossRef]
- McCulloch, M.M.; Lee, C.; Rosen, B.S.; Kamp, J.D.; Lockhart, C.M.; Lee, J.Y.; Polan, D.F.; Hawkins, P.G.; Anderson, C.J.R.; Heukelom, J.; et al. Predictive Models to Determine Clinically Relevant Deviations in Delivered Dose for Head and Neck Cancer. Pract. Radiat. Oncol. 2019, 9, e422–e431. [Google Scholar] [CrossRef] [PubMed]
- Wei, W.; Ioannides, P.J.; Sehgal, V.; Daroui, P. Quantifying the impact of optical surface guidance in the treatment of cancers of the head and neck. J. Appl. Clin. Med. Phys. 2020, 21, 73–82. [Google Scholar] [CrossRef]
- Hague, C.; Aznar, M.; Dong, L.; Fotouhi-Ghiam, A.; Lee, L.W.; Li, T.; Lin, A.; Lowe, M.; Lukens, J.N.; McPartlin, A.; et al. Inter-fraction robustness of intensity-modulated proton therapy in the post-operative treatment of oropharyngeal and oral cavity squamous cell carcinomas. Br. J. Radiol. 2020, 93, 20190638. [Google Scholar] [CrossRef]
- Figen, M.; Çolpan Öksüz, D.; Duman, E.; Prestwich, R.; Dyker, K.; Cardale, K.; Ramasamy, S.; Murray, P.; Şen, M. Radiotherapy for Head and Neck Cancer: Evaluation of Triggered Adaptive Replanning in Routine Practice. Front. Oncol. 2020, 10, 579917. [Google Scholar] [CrossRef]
- Morgan, H.E.; Wang, K.; Dohopolski, M.; Liang, X.; Folkert, M.R.; Sher, D.J.; Wang, J. Exploratory ensemble interpretable model for predicting local failure in head and neck cancer: The additive benefit of CT and intra-treatment cone-beam computed tomography features. Quant. Imaging Med. Surg. 2021, 11, 4781–4796. [Google Scholar] [CrossRef]
- De Ornelas, M.; Xu, Y.; Padgett, K.; Schmidt, R.M.; Butkus, M.; Diwanji, T.; Luciani, G.; Lambiase, J.; Samuels, S.; Samuels, M.; et al. CBCT-Based Adaptive Assessment Workflow for Intensity Modulated Proton Therapy for Head and Neck Cancer. Int. J. Part. Ther. 2021, 7, 29–41. [Google Scholar] [CrossRef]
- Kanehira, T.; van Kranen, S.; Jansen, T.; Hamming-Vrieze, O.; Al-Mamgani, A.; Sonke, J.J. Comparisons of normal tissue complication probability models derived from planned and delivered dose for head and neck cancer patients. Radiother. Oncol. 2021, 164, 209–215. [Google Scholar] [CrossRef]
- Shinde, P.; Jadhav, A.; Gupta, K.K.; Dhoble, S. Quantification Of 6D Inter-Fraction Tumour Localisation Errors in Tongue And Prostate Cancer Using Daily Kv-CBCT For 1000 OMRT And VMAT Treatment Fractions. Radiat. Prot. Dosim. 2022, 198, 1265–1281. [Google Scholar] [CrossRef]
- Rachi, T.; Ariji, T.; Takahashi, S. Development of Machine-Learning Prediction Programs for Delivering Adaptive Radiation Therapy with Tumor Geometry and Body Shape Changes in Head and Neck Volumetric Modulated Arc Therapy. Adv. Radiat. Oncol. 2023, 8, 101172. [Google Scholar] [CrossRef]
- All, S.; Zhong, X.; Choi, B.; Kim, J.S.; Zhuang, T.; Avkshtol, V.; Sher, D.; Lin, M.H.; Moon, D.H. In Silico Analysis of Adjuvant Head and Neck Online Adaptive Radiation Therapy. Adv. Radiat. Oncol. 2023, 9, 101319. [Google Scholar] [CrossRef] [PubMed]
- Sharma, G.; Razeghi Kondelaji, M.H.; Sharma, G.P.; Hansen, C.; Parchur, A.K.; Shafiee, S.; Jagtap, J.M.; Fish, B.; Bergom, C.; Paulson, E.; et al. X-ray and MR Contrast Bearing Nanoparticles Enhance the Therapeutic Response of Image-Guided Radiation Therapy for Oral Cancer. Technol. Cancer Res. Treat. 2023, 22, 15330338231189593. [Google Scholar] [CrossRef] [PubMed]
- Jung, S.; Kim, B.; Lee, S.Y.; Chang, W.I.; Son, J.; Park, J.M.; Choi, C.H.; Lee, J.H.; Wu, H.G.; Kim, J.I.; et al. Novel tongue-positioning device to reduce tongue motions during radiation therapy for head and neck cancer: Geometric and dosimetric evaluation. PLoS ONE 2023, 18, e0291712. [Google Scholar] [CrossRef]
- Bobić, M.; Lalonde, A.; Nesteruk, K.P.; Lee, H.; Nenoff, L.; Gorissen, B.L.; Bertolet, A.; Busse, P.M.; Chan, A.W.; Winey, B.A.; et al. Large anatomical changes in head-and-neck cancers—A dosimetric comparison of online and offline adaptive proton therapy. Clin. Transl. Radiat. Oncol. 2023, 40, 100625. [Google Scholar] [CrossRef] [PubMed]
- Jain, V.; Soni, T.P.; Singh, D.K.; Patni, N.; Jakhotia, N.; Gupta, A.K.; Gupta, T.C.; Singhal, H. A prospective study to assess and quantify the setup errors with cone-beam computed tomography in head-and-neck cancer image-guided radiotherapy treatment. J. Cancer Res. Ther. 2022, 19, 783–787. [Google Scholar] [CrossRef]
- Håkansson, K.; Giannoulis, E.; Lindegaard, A.; Friborg, J.; Vogelius, I. CBCT-based online adaptive radiotherapy for head and neck cancer—Dosimetric evaluation of first clinical experience. Acta Oncol. 2023, 62, 1369–1374. [Google Scholar] [CrossRef]
- Mail, N.; Alshamrani, K.M.; Lodhi, R.N.; Khawandanh, E.; Saleem, A.; Khan, B.; Alghamdi, M.; Nadershah, M.; Althaqafy, M.S.; Subahi, A.; et al. Evaluation of positioning accuracy in head-and-neck cancer treatment: A cone beam computed tomography assessment of three immobilization devices with volumetric modulated arc therapy. J. Biol. Methods 2024, 11, e99010025. [Google Scholar] [CrossRef]
- Blumenfeld, P.; Arbit, E.; Den, R.; Salhab, A.; Falick Michaeli, T.; Wygoda, M.; Hillman, Y.; Pfeffer, R.M.; Fang, M.; Misrati, Y.; et al. Real world clinical experience using daily intelligence-assisted online adaptive radiotherapy for head and neck cancer. Radiat. Oncol. 2024, 19, 43. [Google Scholar] [CrossRef]
- Momin, M.A.; Okochi, K.; Watanabe, H.; Imaizumi, A.; Omura, K.; Amagasa, T.; Okada, N.; Ohbayashi, N.; Kurabayashi, T. Diagnostic accuracy of cone-beam CT in the assessment of mandibular invasion of lower gingival carcinoma: Comparison with conventional panoramic radiography. Eur. J. Radiol. 2009, 72, 75–81. [Google Scholar] [CrossRef]
- Hendrikx, A.W.; Maal, T.; Dieleman, F.; Van Cann, E.M.; Merkx, M.A. Cone-beam CT in the assessment of mandibular invasion by oral squamous cell carcinoma: Results of the preliminary study. Int. J. Oral Maxillofac. Surg. 2010, 39, 436–439. [Google Scholar] [CrossRef]
- Dreiseidler, T.; Alarabi, N.; Ritter, L.; Rothamel, D.; Scheer, M.; Zöller, J.E.; Mischkowski, R.A. A comparison of multislice computerized tomography, cone-beam computerized tomography, and single photon emission computerized tomography for the assessment of bone invasion by oral malignancies. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 2011, 112, 367–374. [Google Scholar] [CrossRef] [PubMed]
- Uribe, S.; Rojas, L.; Rosas, C. Accuracy of imaging methods for detection of bone tissue invasion in patients with oral squamous cell carcinoma. Dentomaxillofac. Radiol. 2013, 42, 20120346. [Google Scholar] [CrossRef] [PubMed]
- Hakim, S.G.; Wieker, H.; Trenkle, T.; Sieg, P.; Konitzer, J.; Holl-Ulrich, K.; Jacobsen, H.C. Imaging of mandible invasion by oral squamous cell carcinoma using computed tomography, cone-beam computed tomography and bone scintigraphy with SPECT. Clin. Oral Investig. 2014, 18, 961–967. [Google Scholar] [CrossRef]
- Linz, C.; Müller-Richter, U.D.; Buck, A.K.; Mottok, A.; Ritter, C.; Schneider, P.; Metzen, D.; Heuschmann, P.; Malzahn, U.; Kübler, A.C.; et al. Performance of cone beam computed tomography in comparison to conventional imaging techniques for the detection of bone invasion in oral cancer. J. Oral Maxillofac. Surg. 2015, 44, 8–15. [Google Scholar] [CrossRef]
- Czerwonka, L.; Bissada, E.; Goldstein, D.P.; Wood, R.E.; Lam, E.W.; Yu, E.; Lazinski, D.; Irish, J.C. High-resolution cone-beam computed tomography for assessment of bone invasion in oral cancer: Comparison with conventional computed tomography. Head Neck 2017, 39, 2016–2020. [Google Scholar] [CrossRef]
- Bombeccari, G.P.; Candotto, V.; Gianni, A.B.; Carinci, F.; Spadari, F. Accuracy of the Cone Beam Computed Tomography in the Detection of Bone Invasion in Patients with Oral Cancer: A Systematic Review. Eurasian J. Med. 2019, 51, 298–306. [Google Scholar] [CrossRef]
- Qiao, X.; Liu, W.; Cao, Y.; Miao, C.; Yang, W.; Su, N.; Ye, L.; Li, L.; Li, C. Performance of different imaging techniques in the diagnosis of head and neck cancer mandibular invasion: A systematic review and meta-analysis. Oral Oncol. 2018, 86, 150–164. [Google Scholar] [CrossRef]
- Shree, S.; Ramesh, K.; Sadaksharam, J. CBCT-based active contour segmentation of bone invasion in oral squamous cell carcinoma—A preliminary retrospective study. J. Ind. Acad. Oral Med. Radiol. 2020, 32, 140. [Google Scholar] [CrossRef]
- Abhinaya, L.M.; Arvind, M.; Rajendran, D. Evaluation of Osseous Changes in Oral Carcinoma—2D Vs 3D Imaging. Int. J. Cur. Res. Rev. 2020, 12, S95–S100. [Google Scholar] [CrossRef]
- Wang, Z.; Zhang, S.; Pu, Y.; Wang, Y.; Lin, Z.; Wang, Z. Accuracy of cone-beam computed tomography for the evaluation of mandible invasion by oral squamous cell carcinoma. BMC Oral Health 2021, 21, 226. [Google Scholar] [CrossRef]
- Shenoy, P.; Archana, P.; Chatra, L.; Veena, K.; Prabhu, R.V.; Shetty, P. Evaluation of Patterns of Mandibular Bone Invasion in CBCT of Patients with Oral Squamous Cell Carcinoma. J. Ind. Acad. Oral Med. Radiol. 2022, 34, 300–303. [Google Scholar] [CrossRef]
- Slieker, F.J.B.; Van Gemert, J.T.M.; Seydani, M.G.; Farsai, S.; Breimer, G.E.; Forouzanfar, T.; de Bree, R.; Rosenberg, A.J.W.P.; Van Cann, E.M. Value of cone beam computed tomography for detecting bone invasion in squamous cell carcinoma of the maxilla. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. 2022, 134, 102–109. [Google Scholar] [CrossRef] [PubMed]
- Straub, A.; Linz, C.; Lapa, C.; Hartmann, S.; Kübler, A.C.; Müller-Richter, U.D.A.; Faber, J.; Bley, T.; Brumberg, J.; Kertels, O.; et al. Performance of cone-beam computed tomography (CBCT) in comparison to conventional computed tomography (CT) and magnetic resonance imaging (MRI) for the detection of bone invasion in oral squamous cell cancer (OSCC): A prospective study. BMC Oral Health 2024, 24, 341. [Google Scholar] [CrossRef]
- Neal, T.W.; Wahidi, J.; Williams, F.C.; Schlieve, T.; Donepudi, J.; Kim, R.Y. The utility of cone-beam computed tomography and multislice computed tomography scan for the evaluation of invasion versus erosion by mandibular squamous cell carcinoma as viewed on medical PACS. Proc. Bayl. Univ. Med. Cent. 2024, 37, 396–400. [Google Scholar] [CrossRef]
- Daly, M.J.; Muhanna, N.; Chan, H.; Wilson, B.C.; Irish, J.C.; Jaffray, D.A. A surgical navigation system for non-contact diffuse optical tomography and intraoperative cone-beam CT. Proc. SPIE 2014, 8937, 893703. [Google Scholar] [CrossRef]
- Weijs, W.L.; Coppen, C.; Schreurs, R.; Vreeken, R.D.; Verhulst, A.C.; Merkx, M.A.; Bergé, S.J.; Maal, T.J. Accuracy of virtually 3D planned resection templates in mandibular reconstruction. J. Craniomaxillofac. Surg. 2016, 44, 1828–1832. [Google Scholar] [CrossRef]
- Ivashchenko, O.; Pouw, B.; de Witt, J.K.; Koudounarakis, E.; Nijkamp, J.; van Veen, R.L.P.; Ruers, T.J.M.; Karakullukcu, B.M. Intraoperative verification of resection margins of maxillary malignancies by cone-beam computed tomography. Br. J. Oral Maxillofac. Surg. 2019, 57, 174–181. [Google Scholar] [CrossRef]
- Muhanna, N.; Chan, H.H.L.; Douglas, C.M.; Daly, M.J.; Jaidka, A.; Eu, D.; Bernstein, J.; Townson, J.L.; Irish, J.C. Sentinel lymph node mapping using ICG fluorescence and cone beam CT—A feasibility study in a rabbit model of oral cancer. BMC Med. Imaging 2020, 20, 106. [Google Scholar] [CrossRef]
- Steybe, D.; Russe, M.F.; Ludwig, U.; Sprave, T.; Vach, K.; Semper-Hogg, W.; Schmelzeisen, R.; Voss, P.J.; Poxleitner, P. Intraoperative marking of the tumour resection surface for improved radiation therapy planning in head and neck cancer: Preclinical evaluation of a novel liquid fiducial marker. Dentomaxillofac. Radiol. 2021, 50, 20200290. [Google Scholar] [CrossRef]
- Polfliet, M.; Hendriks, M.S.; Guyader, J.M.; Ten Hove, I.; Mast, H.; Vandemeulebroucke, J.; van der Lugt, A.; Wolvius, E.B.; Klein, S. Registration of magnetic resonance and computed tomography images in patients with oral squamous cell carcinoma for three-dimensional virtual planning of mandibular resection and reconstruction. Int. J. Oral Maxillofac. Surg. 2021, 50, 1386–1393. [Google Scholar] [CrossRef]
- Agbaje, J.O.; Jacobs, R.; Michiels, K.; Abu-Ta’a, M.; van Steenberghe, D. Bone healing after dental extractions in irradiated patients: A pilot study on a novel technique for volume assessment of healing tooth sockets. Clin. Oral Investig. 2009, 13, 257–261. [Google Scholar] [CrossRef] [PubMed]
- Al-Saleh, M.A.; Punithakumar, K.; Lagravere, M.; Boulanger, P.; Jaremko, J.L.; Wolfaardt, J.; Major, P.W.; Seikaly, H. Three-dimensional morphological changes of the temporomandibular joint and functional effects after mandibulotomy. J. Otolaryngol. Head Neck Surg. 2017, 46, 8. [Google Scholar] [CrossRef] [PubMed]
- Rosen, B.S.; Hawkins, P.G.; Polan, D.F.; Balter, J.M.; Brock, K.K.; Kamp, J.D.; Lockhart, C.M.; Eisbruch, A.; Mierzwa, M.L.; Ten Haken, R.K.; et al. Early Changes in Serial CBCT-Measured Parotid Gland Biomarkers Predict Chronic Xerostomia After Head and Neck Radiation Therapy. Int. J. Radiat. Oncol. Biol. Phys. 2018, 102, 1319–1329. [Google Scholar] [CrossRef] [PubMed]
- Brauner, E.; Musio, D.; Mezi, S.; Ciolfi, A.; Maghella, F.; Cassoni, A.; De Angelis, F.; Guarino, G.; Romeo, U.; Tenore, G.; et al. Implant placement in oral squamous cells carcinoma patients treated with chemoradiotherapy: “Sapienza Head and Neck Unit” clinical recommendations. Eur. Rev. Med. Pharmacol. Sci. 2019, 23, 9923–9930. [Google Scholar] [CrossRef]
- Dohopolski, M.; Wang, K.; Morgan, H.; Sher, D.; Wang, J. Use of deep learning to predict the need for aggressive nutritional supplementation during head and neck radiotherapy. Radiother. Oncol. 2022, 171, 129–138. [Google Scholar] [CrossRef]
- Tyndall, D.A.; Price, J.B.; Tetradis, S.; Ganz, S.D.; Hildebolt, C.; Scarfe, W.C. American Academy of Oral and Maxillofacial Radiology. Position statement of the American Academy of Oral and Maxillofacial Radiology on selection criteria for the use of radiology in dental implantology with emphasis on cone beam computed tomography. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. 2012, 113, 817–826. [Google Scholar] [CrossRef]
- Hidalgo-Rivas, J.A.; Theodorakou, C.; Carmichael, F.; Murray, B.; Payne, M.; Horner, K. Use of cone beam CT in children and young people in three United Kingdom dental hospitals. Int. J. Paediatr. Dent. 2014, 24, 336–348. [Google Scholar] [CrossRef]
- Peters, C.I.; Peters, O.A. CBCT: The New Standard of Care?—American Association of Endodontists. American Association of Endodontists. Available online: https://www.aae.org/specialty/cbct-new-standard-care/ (accessed on 8 May 2025).
- van Herk, M.; Jaffray, D.; Betgen, A.; Remeijer, P.; Sonke, J.; Smitsmans, M.; Zijp, L.; Lebesque, J. First clinical experience with cone-beam CT guided radiation therapy; evaluation of dose and geometric accuracy. Int. J. Radiat. Oncol. Biol. Phys. 2004, 60, S196. [Google Scholar] [CrossRef]
- Jaffray, D.A.; Siewerdsen, J.H. Cone-beam computed tomography with a flat-panel imager: Initial performance characterization. Med. Phys. 2000, 27, 1311–1323. [Google Scholar] [CrossRef]
- Yap, L.M.; Jamalludin, Z.; Ng, A.H.; Ung, N.M. A multi-center survey on adaptive radiation therapy for head and neck cancer in Malaysia. Phys. Eng. Sci. Med. 2023, 46, 1331–1340. [Google Scholar] [CrossRef]
- Lee, V.S.; SchettIno, G.; Nisbet, A. UK adaptive radiotherapy practices for head and neck cancer patients. BJR Open 2020, 2, 20200051. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Dohopolski, M.; Choi, B.; Meng, B.; Visak, J.; Zhong, X.; Kim, J.S.; Inam, E.; Avkshtol, V.; Moon, D.H.; Sher, D.J.; et al. Dosimetric Impact of Simulated Daily Adaptive Radiotherapy with Significantly Reduced Setup Margins in the Definitive Treatment of Head and Neck Cancer. Int. J. Radiat. Oncol. Biol. Phys. 2022, 114, e590. [Google Scholar] [CrossRef]
- Assouline, S.L.; Meyer, C.; Weber, E.; Chatelain, B.; Barrabe, A.; Sigaux, N.; Louvrier, A. How useful is intraoperative cone beam computed tomography in maxillofacial surgery? An overview of the current literature. Int. J. Oral Maxillofac. Surg. 2021, 50, 198–204. [Google Scholar] [CrossRef]
- Schepers, R.H.; Kraeima, J.; Vissink, A.; Lahoda, L.U.; Roodenburg, J.L.; Reintsema, H.; Raghoebar, G.M.; Witjes, M.J. Accuracy of secondary maxillofacial reconstruction with prefabricated fibula grafts using 3D planning and guided reconstruction. J. Craniomaxillofac Surg. 2016, 44, 392–399. [Google Scholar] [CrossRef]
- Van Baar, G.J.C.; Forouzanfar, T.; Liberton, N.P.T.J.; Winters, H.A.H.; Leusink, F.K.J. Accuracy of computer-assisted surgery in mandibular reconstruction: A systematic review. Oral Oncol. 2018, 84, 52–60. [Google Scholar] [CrossRef]
| Inclusion criteria |
|
| Exclusion criteria |
|
| Indication | Number of Articles | Highest Level of Evidence | Citation Received (up to April 2025) | Citation per Article | Date of First Publication on Topic | Publications Number Since 2020 |
|---|---|---|---|---|---|---|
| Imaging in radiation treatment | 25 | Case–control | 483 citations | 19.3 | 2009 | 16 |
| Bone invasion assessment | 16 | Systematic review | 334 citations | 20.9 | 2009 | 7 |
| Intraoperative surgical guidance | 6 | Prospective observational study | 60 citations | 10 | 2014 | 3 |
| Complication assessment | 5 | Prospective observational study | 96 citations | 19.2 | 2009 | 1 |
| Author | Title | Year | Study Design | Objective of Study | Citations |
|---|---|---|---|---|---|
| Cheung et al. [15] | Dose recalculation and the Dose-Guided Radiation Therapy (DGRT) process using megavoltage cone-beam CT | 2009 | PS | To demonstrate the process of performing dose recalculation on megavoltage CBCT images | 41 |
| Den et al. [16] | Daily Image Guidance With Cone-Beam Computed Tomography for Head-and-Neck Cancer Intensity-Modulated Radiotherapy: A Prospective Study | 2010 | PS | To report on the use of daily kilovoltage CBCT to evaluate the inter-fraction and residual error motion of patients undergoing intensity-modulated radiotherapy for head and neck cancer | 219 |
| Yan et al. [17] | Expected treatment dose construction and adaptive inverse planning optimization: Implementation for offline head and neck cancer adaptive radiotherapy | 2013 | RS | To evaluate expected treatment dose for adaptive inverse planning optimization and evaluate it on head and neck cancer adaptive treatment modification using daily CBCT images | 23 |
| Hermans et al. [18] | Weekly kilovoltage cone-beam computed tomography for detection of dose discrepancies during (chemo)radiotherapy for head and neck cancer | 2015 | RS | To evaluate discrepancies between planned and actually delivered radiation doses in head and neck patients and identify predictive factors using weekly CBCT images | 9 |
| Hvid et al. [19] | Accuracy of software-assisted contour propagation from planning CT to cone beam CT in head and neck radiotherapy | 2016 | RS | To determine the accuracy of automated contours compared to manually corrected contours using daily CBCT images | 23 |
| Hofmaier et al. [20] | Multi-criterial patient positioning based on dose recalculation on scatter-corrected CBCT images | 2017 | RS | To evaluate the feasibility and potential advantages of dose-guided patient positioning based on dose recalculation on scatter-corrected CBCT images | 19 |
| Norfadilah et al. [21] | Immobilisation precision in VMAT for oral cancer patients | 2017 | PS | To evaluate the positioning reproducibility of immobilization devices during oral cancer radiotherapy by using CBCT images | 2 |
| Brivio et al. [22] | Selection of head and neck cancer patients for adaptive re-planning of radiation treatment using kV-CBCT | 2018 | RS | To develop a CBCT-based method for the selection of head and neck cancer patients that may require adaptive re-planning | 5 |
| McCulloch et al. [23] | Predictive Models to Determine Clinically Relevant Deviations in Delivered Dose for Head and Neck Cancer | 2019 | RS | To develop a predictive model based on the radiation delivered dose deviations assessed by CBCT | 17 |
| Wei et al. [24] | Quantifying the impact of optical surface guidance in the treatment of cancers of the head and neck | 2020 | RS | To assess the setup accuracy and time for surface-guided radiation therapy using CBCT to verify patient positioning | 10 |
| Hague et al. [25] | Inter-fraction robustness of intensity-modulated proton therapy in the post-operative treatment of oropharyngeal and oral cavity squamous cell carcinomas | 2020 | RS | To evaluate the robustness of an inter-fraction multifield optimized with the use of CBCT in regard to radiation clinical target volume coverage | 15 |
| Figen et al. [26] | Radiotherapy for Head and Neck Cancer: Evaluation of Triggered Adaptive Re-planning in Routine Practice | 2020 | RS | To evaluate the rate of re-planning and determine the factors for a re-plan by assessing anatomical changes with CBCT | 32 |
| Morgan et al. [27] | Exploratory ensemble interpretable model for predicting local failure in head and neck cancer: the additive benefit of CT and intra-treatment cone-beam computed tomography features | 2021 | CCS | To analyse local failure in head and neck cancer using images from CT and CBCT to develop a model for predicting local failure | 16 |
| De Ornelas et al. [28] | CBCT-Based Adaptive Assessment Workflow for Intensity Modulated Proton Therapy for Head and Neck Cancer | 2021 | RS | To explore CBCT use in calculating the proton dose for adaptive radiotherapy in intensity-modulated proton therapy for head and neck cancer | 15 |
| Kanehira et al. [29] | Comparisons of normal tissue complication probability models derived from planned and delivered dose for head and neck cancer patients | 2021 | RS | To compare planned radiation dosage with the delivered dose as estimated from daily CBCT images | 2 |
| Shinde et al. [30] | Quantification of 6D inter-fraction tumour localisation errors in tongue and prostate cancer using daily KV-CBCT for 1000 IMRT and VMAT treatment fractions | 2022 | RS | To evaluate the use of CBCT in minimizing tumour localization errors | 0 |
| Rachi et al. [31] | Development of Machine-Learning Prediction Programs for Delivering Adaptive Radiation Therapy With Tumor Geometry and Body Shape Changes in Head and Neck Volumetric Modulated Arc Therapy | 2023 | RS | To use CBCT to identify objective indicators for cases needing adaptive radiation therapy and develop machine-learning prediction programs | 1 |
| All et al. [32] | In Silico Analysis of Adjuvant Head and Neck Online Adaptive Radiation Therapy | 2024 | PS | To evaluate the benefits of single versus weekly adaptive radiation therapy in head and neck cancer by assessing planning target volume changes using CBCT | 0 |
| Sharma et al. [33] | X-ray and MR Contrast Bearing Nanoparticles Enhance the Therapeutic Response of Image-Guided Radiation Therapy for Oral Cancer | 2023 | AS | To demonstrate the use of theranostic nanoparticles in image-guided radiation therapy planning, utilizing CBCT for tumour delineation and radiation beam arrangement | 4 |
| Jung et al. [34] | Novel tongue-positioning device to reduce tongue motions during radiation therapy for head and neck cancer: Geometric and dosimetric evaluation | 2023 | PS | To verify the position of the tongue during radiation therapy for oral cancer | 0 |
| Bobic et al. [35] | Large anatomical changes in head-and-neck cancers—A dosimetric comparison of online and offline adaptive proton therapy | 2023 | RS | To evaluate an online adaptive workflow intensity-modulated proton therapy versus full offline re-planning with CBCT used to assess anatomical changes | 17 |
| Jain et al. [36] | A prospective study to assess and quantify the setup errors with cone-beam computed tomography in head-and-neck cancer image-guided radiotherapy treatment | 2023 | PS | To assess and quantify the setup errors with CBCT in head and neck cancer image-guided radiotherapy treatment | 3 |
| Håkansson et al. [37] | CBCT-based online adaptive radiotherapy for head and neck cancer-dosimetric evaluation of first clinical experience | 2023 | PS | To assess the dosimetric difference between the daily adapted plans and the original plan with daily CBCT | 5 |
| Mail et al. [38] | Evaluation of positioning accuracy in head-and-neck cancer treatment: A cone beam computed tomography assessment of three immobilization devices with volumetric modulated arc therapy | 2024 | RS | To assess the precision and repeatability of the daily patient positioning for three immobilization devices used for patients undergoing radiation using CBCT | 0 |
| Blumenfeld et al. [39] | Real world clinical experience using daily intelligence-assisted online adaptive radiotherapy for head and neck cancer | 2024 | PS | To evaluate the initial clinical experience of daily adaptive radiotherapy for patients with head and neck cancer using an online adaptive platform with intelligence-assisted workflows with daily CBCT | 5 |
| Authors | Title | Year | Study Design | Objective of Study | Citations |
|---|---|---|---|---|---|
| Momin et al. [40] | Diagnostic accuracy of cone-beam CT in the assessment of mandibular invasion of lower gingival carcinoma: Comparison with conventional panoramic radiography | 2009 | RS | To compare the diagnostic accuracy of CBCT versus panoramic radiography in assessing mandibular invasion by oral cancer | 47 |
| Hendrikx et al. [41] | Cone-beam CT in the assessment of mandibular invasion by oral squamous cell carcinoma: results of the preliminary study. | 2010 | RS | To compare the diagnostic value of CBCT in assessing mandibular invasion by oral cancer with panoramic radiography, MRI, and histological examination | 59 |
| Dreiseidler et al. [42] | A comparison of multislice computerized tomography, cone-beam computerized tomography, and single photon emission computerized tomography for the assessment of bone invasion by oral malignancies | 2011 | PS | To compare the performance of CBCT with conventional CT and SPECT in the detection of bone invasion from oral cancer | 41 |
| Uribe et al. [43] | Accuracy of imaging methods for detection of bone tissue invasion in patients with oral squamous cell carcinoma | 2013 | SR | To examine the available evidence on the diagnostic accuracy of imaging methods for the detection of mandibular bone tissue invasion by squamous cell carcinoma | 71 |
| Hakim et al. [44] | Imaging of mandible invasion by oral squamous cell carcinoma using computed tomography, cone-beam computed tomography and bone scintigraphy with SPECT | 2014 | CCS | To compare the performances in detecting bone invasion of the mandible in oral cancer between CT, CBCT, and bone scintigraphy with SPECT | 28 |
| Linz et al. [45] | Performance of cone beam computed tomography in comparison to conventional imaging techniques for the detection of bone invasion in oral cancer | 2015 | RS | To compare the performance of CBCT with OPG radiographs, conventional CT, MRI, and SPECT in the detection of bone invasion from oral cancer | 26 |
| Czerwonka et al. [46] | High-resolution cone-beam computed tomography for assessment of bone invasion in oral cancer: Comparison with conventional computed tomography | 2017 | PS | To compare the sensitivity and specificity to detect mandibular invasion with conventional CT among patients with oral cancer | 12 |
| Bombeccari et al. [47] | Accuracy of the Cone Beam Computed Tomography in the Detection of Bone Invasion in Patients with Oral Cancer: A Systematic Review | 2019 | SR | To examine the available evidence on the accuracy of CBCT compared with other imaging techniques to detect the degree of invasion of the bone tissue in oral cancer | 16 |
| Qiao et al. [48] | Performance of different imaging techniques in the diagnosis of head and neck cancer mandibular invasion: A systematic review and meta-analysis | 2018 | SR | To examine the available evidence on the diagnostic efficacy of the different imaging techniques for mandibular invasion by head and neck cancer | 18 |
| Shree et al. [49] | CBCT-based active contour segmentation of bone invasion in oral squamous cell carcinoma—A preliminary retrospective study | 2020 | RS | To compare the volumetric analysis by manual and semiautomatic active contour segmentation in oral cancer with frank mandibular bone invasion | 0 |
| Abhinaya et al. [50] | Evaluation of osseous changes in oral carcinoma-2D versus 3D imaging | 2020 | RS | To compare osseous changes using OPG radiographs and CBCT in oral cancer cases | 0 |
| Wang et al. 2021 [51] | Accuracy of cone-beam computed tomography for the evaluation of mandible invasion by oral squamous cell carcinoma | 2021 | ELS | To evaluate the accuracy of CBCT to detect mandibular erosion or invasion with spiral CT among patients with oral cancer | 6 |
| Shenoy et al. [52] | Evaluation of patterns of mandibular bone invasion in CBCT of patients with oral squamous cell carcinoma: A descriptive study | 2022 | RS | To evaluate the patterns of mandibular invasion of oral cancer in CBCT images | 0 |
| Slieker et al. [53] | Value of cone beam computed tomography for detecting bone invasion in squamous cell carcinoma of the maxilla | 2022 | RS | To determine the diagnostic value of CBCT in detecting bone invasion in cancer of the maxilla | 4 |
| Straub et al. [54] | Performance of cone-beam computed tomography (CBCT) in comparison to conventional computed tomography (CT) and magnetic resonance imaging (MRI) for the detection of bone invasion in oral squamous cell cancer (OSCC): a prospective study | 2024 | PS | To compare the ability to detect bone erosion or invasion with conventional CT and MRI among patients with oral cancer | 5 |
| Neal et al. [55] | The utility of cone-beam computed tomography and multislice computed tomography scan for the evaluation of invasion versus erosion by mandibular squamous cell carcinoma as viewed on medical PACS | 2024 | RS | To compare the utility for detecting mandibular erosion or invasion with conventional CT among patients with oral cancer | 1 |
| Author | Title | Year | Study Design | Objective of Study | Citations |
|---|---|---|---|---|---|
| Daly et al. [56] | A surgical navigation system for non-contact diffuse optical tomography and intraoperative cone-beam CT | 2014 | ELS | To assess the feasibility of a non-contact diffuse optical tomography system for multimodal imaging with intraoperative CBCT during minimally invasive cancer surgery | 5 |
| Weijs et al. [57] | Accuracy of virtually 3D planned resection templates in mandibular reconstruction | 2016 | PS | To evaluate the accuracy of prefabricated surgical resection templates using CBCT used in mandibular segmental resections | 37 |
| Ivashchenko et al. [58] | Intraoperative verification of resection margins of maxillary malignancies by cone-beam computed tomography | 2019 | PS | To assess the feasibility of intraoperative imaging during maxillectomy to verify the planned resection margins | 5 |
| Muhanna et al. [59] | Sentinel lymph node mapping using ICG fluorescence and cone beam CT—a feasibility study in a rabbit model of oral cancer | 2020 | AS | To assess the technical feasibility of intraoperative indocyanine green (ICG)-based near-infrared (NIR) fluorescence imaging and CBCT for sentinel lymph node identification during head and neck surgery | 8 |
| Steybe et al. [60] | Intraoperative marking of the tumour resection surface for improved radiation therapy planning in head and neck cancer: preclinical evaluation of a novel liquid fiducial marker | 2020 | AS | To assess the feasibility of using CBCT as part of intraoperative marking of the tumour resection surface in oral cancer patients | 3 |
| Polfliet et al. [61] | Registration of magnetic resonance and computed tomography images in patients with oral squamous cell carcinoma for three-dimensional virtual planning of mandibular resection and reconstruction | 2021 | RS | To evaluate an automated method to perform image registration of MRI and CBCT to be integrated for the virtual planning of mandibular resection margins in oral cancer | 2 |
| Author | Title | Year | Study Design | Objective of Study | Citations |
|---|---|---|---|---|---|
| Agbaje et al. [62] | Bone healing after dental extractions in irradiated patients: a pilot study on a novel technique for volume assessment of healing tooth sockets | 2009 | PS | To assess socket healing following extraction in irradiated jaws | 22 |
| Al-Saleh et al. [63] | Three-dimensional morphological changes of the temporomandibular joint and functional effects after mandibulotomy | 2017 | PS | To assess TMJ morphological changes following mandibulotomy compared to the transoral approach | 12 |
| Rosen et al. [64] | Early Changes in Serial CBCT-Measured Parotid Gland Biomarkers Predict Chronic Xerostomia After Head and Neck Radiation Therapy | 2018 | RS | To assess the applicability of serial CBCT images to predict the occurrence of chronic xerostomia | 47 |
| Brauner et al. [65] | Implant placement in oral squamous cells carcinoma patients treated with chemoradiotherapy: “Sapienza Head and Neck Unit” clinical recommendations | 2019 | PS | To prevent the occurrence of osteoradionecrosis following dental implant by blending radiation dosimetry planning CT scan with CBCT | 4 |
| Dohopolski et al. [66] | Use of deep learning to predict the need for aggressive nutritional supplementation during head and neck radiotherapy | 2022 | RS | To assess the use of CBCT as an adjunct to predict the need for aggressive nutrition supplementation to prevent malnutrition | 11 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mohd Nizar, M.A.; Nabil, S. Cone Beam Computed Tomography in Oral Cancer: A Scoping Review. Diagnostics 2025, 15, 1378. https://doi.org/10.3390/diagnostics15111378
Mohd Nizar MA, Nabil S. Cone Beam Computed Tomography in Oral Cancer: A Scoping Review. Diagnostics. 2025; 15(11):1378. https://doi.org/10.3390/diagnostics15111378
Chicago/Turabian StyleMohd Nizar, Muhammad Aiman, and Syed Nabil. 2025. "Cone Beam Computed Tomography in Oral Cancer: A Scoping Review" Diagnostics 15, no. 11: 1378. https://doi.org/10.3390/diagnostics15111378
APA StyleMohd Nizar, M. A., & Nabil, S. (2025). Cone Beam Computed Tomography in Oral Cancer: A Scoping Review. Diagnostics, 15(11), 1378. https://doi.org/10.3390/diagnostics15111378






